Professional Documents
Culture Documents
Policies and Procedures Manual Tube Feeding (Nasogastic)
Uploaded by
Derick RanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Policies and Procedures Manual Tube Feeding (Nasogastic)
Uploaded by
Derick RanaCopyright:
Available Formats
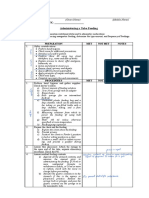
POLICIES AND PROCEDURES MANUAL
TUBE FEEDING (NASOGASTIC)
DOCUMENT CONTOL REVISION NO. EFFECTIVITY DATE PAGE
NO. *** ***
*** REVIEW DUE
***
***
SUBJECTS: TUBE FEEDING (NASOGASTRIC)
1. EQUIPMENT:
1. Feeding ordered by physician
2. 50ml of water
3. Absorbent pad
4. Gavage bag with tubing and flow regulator clam (if a gavage bag is
unavailable, us a bulb syringe or a catheter tip syringe)
5. 50ml syringe
6. Stethoscope
7. Gloves
8. Basin
9. Suction source
10. I.V. standard
2. PREPERATION OF EQUIPMENT:
A. After obtaining from the pharmacy, the unopened cans of formula may be
stored and are to be administered at room temperature. Hot formula may
coagulate formula proteins and clog tubing. Heat may change the
chemical composition of the formula. It may burn or irritate gastric
mucosa. Chilling the formula is avoided because it increases viscosity of
the liquid, which may clog the tube. Cold formula may also cause
vasoconstriction, which reduces the flow of gastric digestive secretions,
which may cause cramping, nausea, vomiting and distention.
B. Wash hands
C. Close the gavage-tubing clamp and pour the appropriate amount of
formula into the gavage bag. Squeeze the drip chamber and fill half way.
Remove the cap from the distal end of the tubing. Open the clamp and
run the formula through the length of tubing and clamp the tubing.
D. All air in tubing is removed so that it does not enter the
Individual’s stomach and cause distention and discomfort.
3. PROCEDURE:
NOTE: if Individual shows any signs of respiratory distress discontinue
feeding immediately and re-assess placement of feeding tube and
Individual status.
POLICIES AND PROCEDURES MANUAL
TUBE FEEDING (NASOGASTIC)
DOCUMENT CONTOL REVISION NO. EFFECTIVITY DATE PAGE
NO. *** ***
*** REVIEW DUE
***
***
NURSING ACTION RATIONAL- PRECAUTIONS
A. Approach and identify Individual. A. To gain Individual confidence and
Explain the procedure and provide lessen anxiety and embarrassment.
privacy Assure Individual’s identity
B. Wash hands B. To avoid cross contamination
C. Bring assembled equipment to C. The equipment need not be sterile.
Individual’s room maintaining a clean Since the stomach is not a sterile
technique. cavity, however, clean technique is
necessary
D. Elevate the head of the Individual’s D. Prevent aspiration of feeding by
bed to semi-fowlers or high position gastroesophageal reflex and to aid
unless contraindicated digestion
E. Place towel or Chux on Individual’s E. Protect Individual’s gown from
chest spillage
F. Put on disposable gloves F. Prevent cross contamination
G. remove cap or plug from distal end G. To check tube patency and
of feeding tube and use syringe to position. To be sure it has not become
inject 10-15 ml of air through the tube displaced. Listen for hissing or gurgling
while auscultating the Individual’s sound (air passing through the
stomach with a stethoscope stomach)
H. Aspirate stomach contents H. Confirm proper position and
patency of the tube
I. Re-install the aspirated stomach I. To prevent the loss of electrolytes ad
contents into the stomach gastric juices
J. NEVER GIVE A FEEDING UNLESS J. Administering a tube feeding
YOU ARE SURE THE TUBE IS through a misplaced tube can cause
PROPERLY POSITIONED IN formula to enter the lungs leading to
INDIVIDUAL’S STOMACH suffocation and death
K. Gavage Bag Feeding K. To prevent air from entering
a) Connect the gavage stomach. Prevents sudden stomach
feeding bag tubing to the distention, which can cause nausea,
feeding tube. Depending vomiting, cramps, or diarrhea. Maintain
on the type of tube used tube patency by removing excess
you may need an adapter sticky formula, which could occlude the
to connect the two tubes. nasogastric tube. To prevent air from
b) Open the regulator clamp entering the stomach causing gastric
on the gavage bag tubing distention.
and adjust the flow rate.
c) Initially administer feeding
slowly & increase rate as
tolerated.
d) After administering the
appropriate amount of
feeding flush the tubing
POLICIES AND PROCEDURES MANUAL
TUBE FEEDING (NASOGASTIC)
DOCUMENT CONTOL REVISION NO. EFFECTIVITY DATE PAGE
NO. *** ***
*** REVIEW DUE
***
***
with about 100ml of water
e) Close the regulator clamp
on the gavage bag
tubing.
L. Catheter Tip Syringe L. Prevent excess air form entering the
f) Attach the syringe to the stomach, causing gastric distention and
feeding tube discomfort. Prevent air from entering
g) Fill the syringe with stomach. NOTE: No more than 500 cc
formula and allow formula of fluid is given at one time.
to flow through. The
height at which you hold
the syringe will determine
flow rate. When the
syringe is ¾ empty, pour
more formula into it.
h) Disconnect the syringe
from the feeding tube and
plug off nasogastric tube
M. “Kangaroo Pump” Place amount of
formula in Kangaroo Pump gavage
bag. Check patency of tube following
N.P. 328. Set up pump to rate as
ordered by Physician.
N. Observe Individual & respiration
throughout the procedure
O. Cover the end of the feeding tube O. To prevent leakage and tube
with its plug or cap. Then release the contamination
tubing or clamp on the tubing. Secure
tubing.
P. Leave the Individual in semi- or P. To prevent gastroesophageal reflux
high-fowlers position for at least 30 and to aid digestion. To prevent
minutes aspiration and suffocation.
Q. Rinse all re-usable equipment with Q. To prevent bacterial growth
warm water and store in a brown paper
bag labeled with the Individual’s name.
R. Change feeding/equipment every R. to prevent bacterial growth
24 hours
S. Wash hands S. To prevent infection
SPECIAL CONSIDERATION RATIONAL-PRECAUTIONS
A. When ready to administer, shake A. Agitation corrects separation, which
the can well immediately before could alter the content of the planed
opening. Once opened, dispense the feeding and potentially clog the tube.
prescribed volume and discard any Immediate use and discard ensures the
unused formula. formula is not a vehicle for microbial
contamination/growth.
POLICIES AND PROCEDURES MANUAL
TUBE FEEDING (NASOGASTIC)
DOCUMENT CONTOL REVISION NO. EFFECTIVITY DATE PAGE
NO. *** ***
*** REVIEW DUE
***
***
B. Aspirate stomach contents 2 or 3 B. a) To verify adequate gastric
hours emptying and decrease vomiting
and aspiration .
b) To maintain acid-base balance.
c) The nutritionist will be able to
calculate the caloric intake
accurately by knowing the amount
of feeding returned.
C. During continuous feeding, assess C. Distention may cause nausea,
the Individual frequently for abdominal vomiting and is uncomfortable.
distention.
D. If diarrhea occurs, notify the D. Diarrhea is the most common
physician so that the underlying cause complication. Common causes are: too
can be determined and corrected, e.g., high infusion rate or volume, lack of
alternating the prescribed medications, fiber, altered gastrointestinal flora (e.g.
changing the formula and/or due to medication or contamination),
administration rate/volume, switching to hypoalbuminemia, or hyperosmolar
a fiber containing formula, solutions (Isotonic formulas are best
administering antidiarrheal medication, tolerated.)
or correcting a low serum albumin. Also
ensure that proper infection control and
equipment practices are being
followed.
E. If constipation occurs, notify the E. Irregular bowel movements can
physician so that the underlying cause result from the low fiber content of the
can be determined and corrected , e.g., formula, inadequate fluids, medication
altering the formula, adding fluids, or lack of activity. The feeding should
ordering a bulk forming laxative, be stopped and evaluated if obstruction
increasing Individual activity, or is suspected.
changing a medication.
F. Assess hydration and increase fluid F. Dehydration may cause
intake as necessary if fluids are not constipation
contraindicated.
G. Drugs may be administered through G. Avoid need for discomfort of I.M.
the feeding tube, except for enteric- Injections
coated drugs. Crush tablets or open
and dilute capsules in water prior to
administering. Flush the tubing with
water after administering drugs.
H. Monitor blood glucose to assess H. To determine response nutritional
glucose tolerance. Also monitor serum support.
electrolytes and other blood studies as
ordered by the physician.
POLICIES AND PROCEDURES MANUAL
TUBE FEEDING (NASOGASTIC)
DOCUMENT CONTOL REVISION NO. EFFECTIVITY DATE PAGE
NO. *** ***
*** REVIEW DUE
***
***
4. DOCUMENTATION:
A. Document the feeding on the Medication Administration Record (MAR)
including:
1. The time the food product was opened & administered
2. The amount and type of formula given
3. The amount of water given
4. The time(s) that the tubing was changed
B. Record total I. & O. don the Intake and Output flow sheet
C. Record amount of residual feeding aspirated and returned on the IDN’s.
D. In the IDN’s record the placement and patency of the tube, the amount of
residual feeding (if any), the Individual’s reaction to and the tolerance of
feeding, including any cramping, diarrhea or abdominal distention. Also
note the results of blood tests.
REFERENCE: Nutrition Care Manual Feeding and Liquid Supplements
You might also like
- NGT ProcedureDocument5 pagesNGT ProcedureFrances MercadoNo ratings yet
- Differential DiagnosisDocument1 pageDifferential Diagnosisririz b100% (1)
- Lesson Plan in Science 4 - LajieDocument10 pagesLesson Plan in Science 4 - LajieMar JenNo ratings yet
- Policies and Procedures Manual Tube FeedingDocument4 pagesPolicies and Procedures Manual Tube FeedingDerick RanaNo ratings yet
- Administering Tube FeedingDocument2 pagesAdministering Tube FeedingAlecsandra CabridoNo ratings yet
- Feeding Via Gastric GavageDocument3 pagesFeeding Via Gastric Gavageneleh gray0% (1)
- Tube FeedingDocument6 pagesTube FeedingKyla Shain GallegoNo ratings yet
- Tube Feeding (GavageDocument2 pagesTube Feeding (GavageevergrayelleNo ratings yet
- ) Administering Nasogastric Tube or Orogastric Tube FeedingDocument6 pages) Administering Nasogastric Tube or Orogastric Tube FeedingJohn Pearl FernandezNo ratings yet
- Skill 21 (1) ..Management of Gastrointestinal SuctionDocument1 pageSkill 21 (1) ..Management of Gastrointestinal SuctionnetsquadNo ratings yet
- NGT DemoDocument5 pagesNGT Demoeliza luisNo ratings yet
- PRS NGTDocument7 pagesPRS NGTMika Marielle TrincheraNo ratings yet
- Nasogastric Tube InsertionDocument8 pagesNasogastric Tube InsertionMayaPopbozhikovaNo ratings yet
- Nasogastric Tube FeedingDocument2 pagesNasogastric Tube FeedingKathrina Mendoza HembradorNo ratings yet
- NGTDocument5 pagesNGTElla CerenioNo ratings yet
- Sarasota Memorial Hospital Nursing Procedure Title: Date: Reviewed: Pages: Issued For: ResponsibilityDocument5 pagesSarasota Memorial Hospital Nursing Procedure Title: Date: Reviewed: Pages: Issued For: Responsibilitybalab2311No ratings yet
- IV InsertionDocument9 pagesIV InsertionSharmaine Grace FlorigNo ratings yet
- Nasogastric Tube Feeding Definition:: University of Eastern PhilippinesDocument2 pagesNasogastric Tube Feeding Definition:: University of Eastern PhilippinesJerika Shane MañosoNo ratings yet
- Nursing Procedure: Golden Gate Colleges College of NursingDocument9 pagesNursing Procedure: Golden Gate Colleges College of NursingJohn Paul Richard Mindanao100% (1)
- NGT and Colostomy Care ChecklistDocument8 pagesNGT and Colostomy Care ChecklistJurac AzilanaNo ratings yet
- NCM 321 RLE Procedural Checklist 2Document33 pagesNCM 321 RLE Procedural Checklist 2Eryl Franz HerreraNo ratings yet
- Nasogastric Tube - Enema ProceduresDocument3 pagesNasogastric Tube - Enema ProceduresJOSHUA DICHOSONo ratings yet
- Nasogastric Tube FeedingDocument2 pagesNasogastric Tube FeedingCelline Isabelle ReyesNo ratings yet
- NGT Feeding RemovingDocument2 pagesNGT Feeding RemovingMaria Carmela RoblesNo ratings yet
- Skill 24 (1) ..Administration of A Bolus FeedingDocument2 pagesSkill 24 (1) ..Administration of A Bolus FeedingnetsquadNo ratings yet
- Demo Bladder IrrigationDocument4 pagesDemo Bladder IrrigationTopeshwar TpkNo ratings yet
- Lavage Assisting With Gastric IntubationDocument3 pagesLavage Assisting With Gastric IntubationLea Jean Lobrigo OleaNo ratings yet
- NGT Feeding: by Group 2Document25 pagesNGT Feeding: by Group 2karl montano100% (1)
- Assisting in Gastric LavageDocument5 pagesAssisting in Gastric LavageJannen Casas100% (1)
- Naso Gastric Tube Insertion and RemovalDocument5 pagesNaso Gastric Tube Insertion and RemovalPia Mae BuayaNo ratings yet
- Medical Surgical Nursing: Gracious Colleg of Nursing Abhanpur Raipur (C.G.)Document9 pagesMedical Surgical Nursing: Gracious Colleg of Nursing Abhanpur Raipur (C.G.)Topeshwar TpkNo ratings yet
- Trach SuctionDocument3 pagesTrach SuctionKey Charyeth AlbanoNo ratings yet
- NGT InsertionDocument4 pagesNGT InsertionAngela Joy AmparadoNo ratings yet
- NGT NCM-116 ChecklistDocument9 pagesNGT NCM-116 ChecklistclaribelleNo ratings yet
- NCM 116 ChecklistsDocument11 pagesNCM 116 ChecklistsJoy DamoNo ratings yet
- Mabini Colleges Fundamentals of Nursing Gastric Gavage B. Continuous Drip Method EquipmentDocument2 pagesMabini Colleges Fundamentals of Nursing Gastric Gavage B. Continuous Drip Method EquipmentLea Jean Lobrigo OleaNo ratings yet
- Cebu City Medical Center-College of NursingDocument5 pagesCebu City Medical Center-College of NursingJimnah Rhodrick BontilaoNo ratings yet
- Nasogastric & Gavage - NsoDocument5 pagesNasogastric & Gavage - NsojamesNo ratings yet
- Identify Any Deficiencies, Excesses or Problems With DeliveryDocument3 pagesIdentify Any Deficiencies, Excesses or Problems With DeliveryWenalyn Grace Abella LlavanNo ratings yet
- Learning Activity N3A & N3BDocument3 pagesLearning Activity N3A & N3BMikaela JosonNo ratings yet
- Module 3 Nursing Skills Procedure On GI, Endo-Metab Concept (A)Document18 pagesModule 3 Nursing Skills Procedure On GI, Endo-Metab Concept (A)Nashebah A. BatuganNo ratings yet
- NGT Insertion Directly From CanvasDocument6 pagesNGT Insertion Directly From CanvasRico Delgado of WorldbexNo ratings yet
- Respiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANDocument32 pagesRespiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANKun KandaNo ratings yet
- Nasogastric Tube A. DefinitionDocument5 pagesNasogastric Tube A. Definitionkarl montanoNo ratings yet
- Fundamentals BulletsDocument12 pagesFundamentals Bulletsmaya reyesNo ratings yet
- Insertion of A Nasogastric TubeDocument3 pagesInsertion of A Nasogastric TubeJames Andre P. MoralesNo ratings yet
- Bladder IrrigationDocument14 pagesBladder IrrigationsandhyaNo ratings yet
- New NGT Checklist EditedDocument7 pagesNew NGT Checklist EditedRhona Marie AcuñaNo ratings yet
- Tube FeedingDocument50 pagesTube FeedingHari Priya TangiralaNo ratings yet
- Health Care Procedures - Nutrition and EliminationDocument11 pagesHealth Care Procedures - Nutrition and EliminationRS BuenavistaNo ratings yet
- PowerpointDocument78 pagesPowerpointMiNa SUy FullNo ratings yet
- Gavage FedingDocument9 pagesGavage FedingGeetha ReddyNo ratings yet
- Nasogastric Tube (Assissting in Indertion, Feeding) .ProcedureDocument4 pagesNasogastric Tube (Assissting in Indertion, Feeding) .ProcedureJeonoh FloridaNo ratings yet
- Nasogastric Tube FeedingDocument19 pagesNasogastric Tube FeedingMicah Alexis CandelarioNo ratings yet
- NGT PowerpointDocument19 pagesNGT Powerpointسانو روديلNo ratings yet
- Changing Fecal Pouching Colostomy)Document48 pagesChanging Fecal Pouching Colostomy)Champola Pola Camille BernardoNo ratings yet
- Pediatric Procedures PDFDocument6 pagesPediatric Procedures PDFSanjida Mithila100% (1)
- Peg Feeding RationaleDocument3 pagesPeg Feeding RationaleAlyzza Dagoy100% (1)
- NGT FeedingDocument74 pagesNGT FeedingGoddy Manzano100% (1)
- NGT Feeding ChecklistDocument4 pagesNGT Feeding ChecklistCee Sanchez100% (6)
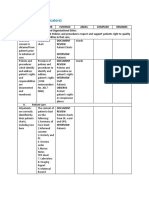
- Diabetes Mellitus: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument12 pagesDiabetes Mellitus: Assessment Diagnosis Planning Intervention Rationale EvaluationDerick RanaNo ratings yet
- Letter of ProfessionalismDocument1 pageLetter of ProfessionalismDerick RanaNo ratings yet
- Smith L (2017) Nursing Times 113: 12, 20-23Document59 pagesSmith L (2017) Nursing Times 113: 12, 20-23Derick RanaNo ratings yet
- Ic-01-048 Infection Control in Pediatric Intensive Care UnitDocument6 pagesIc-01-048 Infection Control in Pediatric Intensive Care UnitDerick RanaNo ratings yet
- Ic-01-047 Infection Control in Operating RoomDocument13 pagesIc-01-047 Infection Control in Operating RoomDerick RanaNo ratings yet
- Diabetes Nursing EducationDocument4 pagesDiabetes Nursing EducationDerick RanaNo ratings yet
- Diabetes Group ReportDocument34 pagesDiabetes Group ReportDerick RanaNo ratings yet
- Ic-01-040 Infection Control in Dental ClinicDocument11 pagesIc-01-040 Infection Control in Dental ClinicDerick RanaNo ratings yet
- Ic-01-049 Infection Control in Clinical EngineeringDocument4 pagesIc-01-049 Infection Control in Clinical EngineeringDerick RanaNo ratings yet
- Ic-01-041 Infection Control in DialysisDocument15 pagesIc-01-041 Infection Control in DialysisDerick RanaNo ratings yet
- Recruitment Checklist: Security Forces Hospital ProgramDocument4 pagesRecruitment Checklist: Security Forces Hospital ProgramDerick RanaNo ratings yet
- Ic-01-042 Infection Control in Emergency RoomDocument13 pagesIc-01-042 Infection Control in Emergency RoomDerick RanaNo ratings yet
- Policies and Procedures Manual Infection Control in General Nursing UnitDocument9 pagesPolicies and Procedures Manual Infection Control in General Nursing UnitDerick RanaNo ratings yet
- Ic-01-039 Infection Control in Adult Intensive Care UnitDocument7 pagesIc-01-039 Infection Control in Adult Intensive Care UnitDerick RanaNo ratings yet
- DEMENTIA Citical ExamDocument4 pagesDEMENTIA Citical ExamDerick RanaNo ratings yet
- Smith L (2017) Nursing Times 113: 12, 20-23Document59 pagesSmith L (2017) Nursing Times 113: 12, 20-23Derick RanaNo ratings yet
- Critical Care Notes BookDocument142 pagesCritical Care Notes BookDerick RanaNo ratings yet
- Ohhc Clean CatchDocument5 pagesOhhc Clean CatchDerick RanaNo ratings yet
- Emergency NursingDocument5 pagesEmergency NursingDerick RanaNo ratings yet
- NX Service Admin Practicum Packet-1Document12 pagesNX Service Admin Practicum Packet-1Derick RanaNo ratings yet
- Ohhc Laboratory ProceduresDocument3 pagesOhhc Laboratory ProceduresDerick RanaNo ratings yet
- Job Description: 1.1 Professional, Ethical and LegalDocument11 pagesJob Description: 1.1 Professional, Ethical and LegalDerick RanaNo ratings yet
- DOH Standards (Indicators)Document2 pagesDOH Standards (Indicators)Derick RanaNo ratings yet
- Ohhc Obtaining Stool Specimens For Laboratory AnalysisDocument8 pagesOhhc Obtaining Stool Specimens For Laboratory AnalysisDerick RanaNo ratings yet
- Presenting Complaint: ConstipationDocument5 pagesPresenting Complaint: ConstipationmiranaNo ratings yet
- Higado 1Document86 pagesHigado 1Carlos CuadrosNo ratings yet
- Liver DiseasesDocument114 pagesLiver DiseasesDayang Feineliza Samman BahjinNo ratings yet
- Prof. Barmawi KULIAH 5 AMOEBIASISDocument43 pagesProf. Barmawi KULIAH 5 AMOEBIASISTommy HardiantoNo ratings yet
- Operative Procedures in Surgical Gastroenterology Volume IIDocument275 pagesOperative Procedures in Surgical Gastroenterology Volume IIsalah subbahNo ratings yet
- Case Study Presented by Group 22 BSN 206: In-Depth View On CholecystectomyDocument46 pagesCase Study Presented by Group 22 BSN 206: In-Depth View On CholecystectomyAjiMary M. DomingoNo ratings yet
- Salivary Secretion: Chapter OutlineDocument9 pagesSalivary Secretion: Chapter OutlineJoshika MahendranNo ratings yet
- 7985 - Jadwal GIS 1920Document12 pages7985 - Jadwal GIS 1920amelia rahayuNo ratings yet
- Quiz 5 NDocument16 pagesQuiz 5 NabezareljvenNo ratings yet
- Git GutDocument4 pagesGit GutAngelica Murillo Ang-AngcoNo ratings yet
- CASE STUDY #2 Digestive System (Acute Pancreatitis)Document3 pagesCASE STUDY #2 Digestive System (Acute Pancreatitis)Lerma PagcaliwanganNo ratings yet
- Colonoscopy LandmarkDocument4 pagesColonoscopy LandmarkSueNo ratings yet
- What's The Difference Between Gastric and Duodenal Ulcers?Document6 pagesWhat's The Difference Between Gastric and Duodenal Ulcers?Anonymous cDy4bZMMNo ratings yet
- Final: Gluconeogenesis - When The Liver and KidneysDocument43 pagesFinal: Gluconeogenesis - When The Liver and KidneysRashid DayaoNo ratings yet
- Peritoneum 2022Document86 pagesPeritoneum 2022Tayyib KhanNo ratings yet
- Digestive System PowerpointDocument19 pagesDigestive System Powerpointapi-277974939No ratings yet
- Science CH - 2 - Jantuon Main PoshanDocument19 pagesScience CH - 2 - Jantuon Main PoshanVijay TrivediNo ratings yet
- Peptic Ulcer DiseaseDocument18 pagesPeptic Ulcer DiseaseAESTHETIC PHOTONo ratings yet
- Konsensus Konstipasi 2010Document8 pagesKonsensus Konstipasi 2010Lidya Ayu LestariNo ratings yet
- Motility Disorders of The GITDocument57 pagesMotility Disorders of The GITMahmoud AjinehNo ratings yet
- Digestive SystemDocument4 pagesDigestive SystemJM MatiasNo ratings yet
- PBL 5.2 (Git 1)Document46 pagesPBL 5.2 (Git 1)aiman mazlanNo ratings yet
- Assessment and Management of Patients With Biliary DisordersDocument18 pagesAssessment and Management of Patients With Biliary DisordersBheru LalNo ratings yet
- Acute Pancreatitis 2023Document25 pagesAcute Pancreatitis 2023raphael chidiebereNo ratings yet
- Important SlidesDocument5 pagesImportant Slidesgeert.schalkNo ratings yet
- Chronic Constipation in Rome 4 Era The Indian PerspectiveDocument11 pagesChronic Constipation in Rome 4 Era The Indian PerspectiveAbulHasan Idrus IstarNo ratings yet
- NCP2 FinalDocument2 pagesNCP2 FinallinlynNo ratings yet
- CH 06Document19 pagesCH 06cyberyeung0% (1)