Professional Documents
Culture Documents
Dental Complications and Management of Patients On Bisphosphonate Therapy A Review Article
Uploaded by
yomiboyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental Complications and Management of Patients On Bisphosphonate Therapy A Review Article
Uploaded by
yomiboyCopyright:
Available Formats
j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0
Available online at www.sciencedirect.com
journal homepage: www.elsevier.com/locate/jobcr
Review Article
Dental complications and management of patients on
bisphosphonate therapy: A review article
Sandeep Kalra a, Veena Jain b,*
a
Research Officer, Department of Prosthodontics, Center for Dental Education and Research, All India Institute of Medical Sciences (AIIMS),
New Delhi 110029, India
b
Additional Professor, Department of Prosthodontics, Center for Dental Education and Research, All India Institute of Medical Sciences
(AIIMS), New Delhi 110029, India
article info abstract
Article history: Bisphosphonates are group of drugs that inhibit bone resorption and are used to treat a
Received 3 October 2012 range of pathologies including Paget’s disease, osteoporosis, multiple myeloma and
Accepted 1 November 2012 metastasis associated with breast or prostate cancer. The most common complication in
patients on bisphosphonate therapy is osteonecrosis of jaw (ONJ) which can occur after any
Keywords: surgical dental procedure and the risk for the development of osteonecrosis of jaw is higher
Bisphosphonates in patients receiving intravenous bisphosphonate therapy than in patients receiving oral
Osteonecrosis of jaw bisphosphonate therapy. Typical presentation is in the form of non-extraction socket,
Dental implants presence of exposed bone, gingival swelling or purulent discharge, when local debridement
and antibiotics are ineffective.
At present, there is no effective treatment for bisphosphonate induced osteonecrosis, so
prevention is extremely important. Maximum precautions should be taken in patients who
are at the risk of development of ONJ especially when any dental surgical procedure like
extractions, retrograde apicoectomies, periodontal surgery and implant placement is
contemplated. Dentists and oral or maxillofacial surgeon must keep up to date with the
latest approaches or guidelines to prevention and the risk factors, particularly when
treating patients who are on bisphosphonates, or who will be taking bisphosphonates.
Copyright ª 2012, Craniofacial Research Foundation. All rights reserved.
1. Introduction There are 2 types of bisphosphonates: nitrogen containing
and non-nitrogen containing. Those containing nitrogen in
Bisphosphonates are the group of drugs that inhibit bone their structure are more potent and accumulate in maximum
resorption and are used to treat metabolic diseases like oste- concentration in the matrix and osteoclasts.3
oporosis, Paget’s disease, hypercalcaemia of malignancy and There are two modes of administration of bisphospho-
multiple myeloma.1 The nuclear structure of bisphosphonates nates: intravenously (IV) and orally. There is lot of difference
consists of 2 phosphate group joined by single carbon atom.2 in potency with both modes as with oral administration only
* Corresponding author. Tel.: þ91 (0) 9868187441.
E-mail address: jainveena1@gmail.com (V. Jain).
2212-4268/$ e see front matter Copyright ª 2012, Craniofacial Research Foundation. All rights reserved.
http://dx.doi.org/10.1016/j.jobcr.2012.11.001
26 j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0
1% of the dose is absorbed by gastrointestinal tract whereas administered. Non-nitrogen containing bisphosphonates act
with IV mode more than 50% of the dose administered is bio by interacting with ATP in osteoclast forming ATP analogues
available, which makes IV dose more potent.4,5 Intravenous that induces osteoclast apoptosis. Nitrogen containing
bisphosphonates are used to reduce bone pain, Paget’s dis- bisphosphonates inhibit farnesyl pyrophosphate synthase
ease, hypercalcaemia of malignancy, myeloma. Oral (FPPS), a key enzyme in mevalonic acid pathway, in osteo-
bisphosphonates are mainly used for treatment of osteopo- clast which prevents the production of proteins essential for
rosis, osteogenesis imperfecta. their survival and function. Inhibition of this enzyme also
The main mechanism of their action is explained by the leads to accumulation of isopentyl disphosphonate (IPP)
fact that bisphosphonates have a high affinity for bone min- which is incorporated into an analogue of ATP that can
erals and bind strongly to hydroxyapatite resulting in selective induce osteoclast apoptosis. So due to their action on the
uptake to the target organ and high local concentration in osteoclast the bone healing and remodelling is affected in the
bone, particularly at the sites of active bone remodelling. They area that has been traumatized or surgically treated. This
act by inhibiting the osteoclast differentiation, reducing their leads to non-resorption of the necrotic bone which further
activity, and inducing osteoclast apoptosis.6 affects the blood supply of that area leading to osteonecrosis
Although bisphosphonates have been proved beneficial for of jaw.10
many metabolic bone diseases but due to their action on Now since the jaws have a greater blood supply than other
osteoclast, they impair bone healing and remodelling and this bones and a faster turnover rate related to their daily activity
has resulted in increased risk of development of osteonecrosis and presence of teeth, bisphosphonates are highly concen-
of jaw (ONJ) following surgical dental procedures like extrac- trated in jaws.11 Due to chronic invasive dental disease and
tion or implant placement.7 The basic mechanism of devel- treatments, thin mucosa over bone, this anatomic concen-
opment of osteonecrosis is that due to osteoclastic inhibition tration of bisphosphonates causes this condition to be man-
necrotic bone cannot be resorbed by the osteoclast during ifested exclusively in jaws.
normal course of healing and the necrotic bone which re-
mains, affects the blood supply to the area. So, the ONJ be-
2.2. Clinical presentation of bisphosphonate associated
comes the major dental complication in patients on
osteonecrosis of jaw
bisphosphonate therapy. The risk of developing ONJ increases
with the duration the patient has been taking the drugs. The
Osteonecrosis of jaw is also known as avascular necrosis of
patients receiving IV bisphosphonates are at more risk for
bone or osteochondritis dissecans. It leads to bone pain, loss
development of ONJ then those getting oral bisphosphonates.8
of bone function and bone destruction resulting in impair-
So it becomes important to identify the patients who are, or
ment of blood supply. It usually presents as area of exposed
will be placed on bisphosphonate therapy so that appropriate
bone along with soft tissue swelling, purulent discharge,
precautions or management can be done prior to any dental
loosening of teeth and the lesion do not respond to local
procedure.
debridement and antibiotics.12,13 Lesion develops around
This article focuses on presenting the incidence of osteo-
sharp bony area or previous surgical site including extraction,
necrosis of jaw after surgical dental procedure in patients
retrograde apicoectomies, periodontal surgery and dental
under bisphosphonate therapy and the management of such
implant surgery. There also may be feeling of numbness,
patients.
heaviness or dyesthesia of jaw. However, lesion may remain
asymptomatic for weeks or months. Occasionally, pain in
jaws may be the only symptom without any evidence of
2. Complications in patients on
radiological abnormality. The lesion may also become sec-
bisphosphonate therapy
ondary infected with actinomyces.14
The most common complication in patients on bisphospho-
nate therapy is osteonecrosis of jaw which occurs after any 2.3. Risk factors for bisphosphonate induced
surgical dental procedure. Although, spontaneous cases of osteonecrosis of jaw (ONJ)
osteonecrosis have been reported but in majority of cases
(68.8%), patients had a history of dental disease or treatment.8 2.3.1. Bisphosphonate exposure
According to the information currently available, risk for Risk of developing osteonecrosis with intake of bisphospho-
developing bisphosphonate associated osteonecrosis of jaw is nate depends upon the individual bisphosphonate potency,
higher in patients on IV bisphosphonate therapy than the the mode of administration and the cumulative dose.15,16
patients on oral bisphosphonates as orally they are poorly Among various bisphosphonates IV administered are
absorbed.8,9 more potent than orally administered bisphosphonates. In IV
administered bisphosphonates, Zolendronate is the most
2.1. Pathophysiology of osteonecrosis potent bisphosphonate because of its high mineral binding
affinity and FPPS enzyme inhibition whereas pamidronate is
As stated earlier bisphosphonates have high affinity for bone less potent.17e20 Orally administered bisphosphonates
minerals and bind strongly to hydroxyapatite which results include etidronate, risedronate, tiludronate, alendronate.
in high concentration at the site of active bone remodelling. Most cases of bisphosphonate induced ONJ have been re-
They further act to induce osteoclast apoptosis.6 The mode of ported with alendronic acid which is also used most widely
their action depends on the type of bisphosphonate worldwide.
j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0 27
The cumulative dose of bisphosphonate is also considered
to be an important factor in development of ONJ and is 3. Management of patients on
determined by the dose, frequency of administration, dura- bisphosphonate therapy
tion of therapy and half life of drug.
The action of bisphosphonate that is of concern to dentist is
2.3.2. History of dental disease that they destroy osteoclast and without osteoclast there
A history of dental disease, including invasive dental pro- cannot be bone healing which is very important for surgical
cedures, dental trauma and periodontal disease are important dental procedures like extraction or implant placement. So
risk factors for development of ONJ in association with management of patients on bisphosphonate therapy prior to
bisphosphonates. any surgical procedure becomes important.
A number of studies have identified dental extractions as
significant risk factors. Other dental procedures that have
3.1. Guidelines for management of patient on
been implicated in development of ONJ include bony exos-
bisphosphonate therapy (preventive measures)11,12,32,33
tosis, intubation induced trauma and dental implants.11,21 The
use of dentures and the presence of inflammatory dental
1. All patients should be asked about the current or past use of
disease such as periodontal disease, dental abscesses and
bisphosphonate drugs and the mode of administration
poor dental hygiene have also been identified as risk
because IV bisphosphonate have a longer half life and pa-
factors.19,21,22
tients on IV mode are at more risk for development of ONJ
than patients on oral bisphosphonate.
2.3.3. Jaw anatomy
2. Patients yet to start with bisphosphonate therapy should be
ONJ occurs twice as frequently in mandible than in maxilla
first examined for requirement of any surgical dental pro-
and areas with thin mucosa such as torus mandibularis and
cedures prior to the therapy, if the risk factors allows.
mylohyoid ridge.11,18,23
Hopeless teeth should be removed. Subgingival scaling
2.3.4. Malignant disease should be performed. Poorly fitting dentures should be
Duration of malignant disease, duration of bone metastasis replaced to avoid soft tissue trauma. Comprehensive
and type of cancer may be associated with increased risk of treatment should be performed to minimize the need for
ONJ development.21 ONJ predominantly occurs in breast can- future dental treatment.
cer, multiple myeloma and prostate cancer.24 3. For patients who have already started with the therapy, any
elective procedures should be avoided if possible to avoid
2.3.5. Concomitant treatment the risk of bisphosphonate induced osteonecrosis of jaw.
Patients on additional chemotherapy and corticosteroids Root canal treatment should be done rather than dental
which is common in such patients are at higher risk for extraction when possible.
developing ONJ.23,25 4. Patient should be routinely examined radio graphically for
osteonecrosis and baseline data should be recorded for the
2.3.6. Age, sex and race patient. Certain laboratory test may help to monitor
Old patients and female patients are at increased risk of markers of bone turnover and can help in diagnosis and
developing ONJ. Caucasians patients may be at higher risk of risk assessment of developing bisphosphonate associated
developing ONJ.23 osteonecrosis. Bisphosphonates reduces the level of CTx
(C-telopeptides) which are fragment of collagen released
2.3.7. Genetic factors during remodelling and skeleton turnover. So by assessing
Single nucleotide polymorphism of the cytochrome P450 the serum CTx levels risk assessment can be done34
CYP2C8 gene have been identified as a possible risk factor for (Table 1).
the development of ONJ in multiple myeloma patient 4. Patients should be educated about the importance of good
receiving Zolendronate and pamidronate treatment.26 Matrix oral hygiene, regular dental check-ups and also about the
metalloproteinase 2 has also been hypothesized as candidate symptoms of osteonecrosis of jaw so that patient can report
gene for an increased risk of bisphosphonate induced ONJ.27 early if the symptoms develop.
5. Patients in which dental extractions are unavoidable
2.3.8. Smoking should be first consulted with the prescriber of
Smoking is also possible risk factor for developing ONJ in pa- bisphosphonate therapy for possible temporary
tients on bisphosphonate therapy.21,28
2.3.9. Co-morbid condition
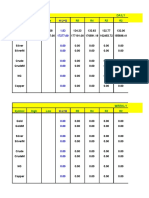
Low haemoglobin levels,23 low serum calcium and secondary Table 1 e CTx serum value and risk factors for
hyperparathyroidism,29 renal dialysis,23 diabetes30 and osteonecrosis.
obesity28 are possible risk factors for ONJ in cancer patients. CTx serum value (pg/ml) Risk for osteonecrosis
Other co-morbid conditions like hypertension, hyper-
lipidaemia, hypercholestrolaemia, rheumatoid arthritis and 300e600 (normal) None
150e299 None to minimal
diabetes may possibly contribute to risk of developing factors
101e149 Moderate
ONJ in patients receiving bisphosphonates for non-cancer <100 High
indications.31
28 j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0
Table 2 e Staging and management of osteonecrosis.
Stage Characterized by Treatment
Stage I Asymptomatic detection of exposed bone without soft tissue Managed conservatively. Daily irrigation, oral antimicrobials
infection rinses (0.12% chlorhexidine rinses)
Follow up every 3 months
If patient is wearing dentures then they should be properly
adjusted to avoid further trauma and should be removed in
night
Stage II Presence of symptoms around the area of exposed bone Culture directed antimicrobial therapy- long term
secondary to soft tissue swelling or bone infection Analgesics
Minor bone debridement to reduce sharp edges
Stage III Presence of pathological fracture Requires surgical debridement/resection to reduce volume of
Exposed bone associated with soft tissue infection, which is not necrotic bone
manageable with antibiotics alone Analgesics
Culture directed antibiotics-IV or oral
Oral antimicrobial rinses
interruption of drug if beneficial. Extraction should be done
as atraumatically as possible and flap raising should be 4. Dental implants and bisphosphonate
avoided. Sterile technique has to be followed. Patient therapy
should be kept on chlorhexidine mouthwash twice daily for
two months and postoperatively 2 month follow up should Implant placement in patients on bisphosphonate therapy
be done. In some cases it has been recommended to do root predisposes them to development of osteonecrosis of jaw. So
canal of the teeth followed by coronal amputation and prior to planning implants in such patients it is important to
leave the roots.35 identify the type of bisphosphonate (oral or intravenous) they
are taking. Various studies have been done to identify the
incidence of osteonecrosis in patients on bisphosphonate
3.2. Management of patients who have developed ONJ therapy (Table 3):
From the various studies it has been seen that patients on
1. If ONJ is suspected then panoramic radiography is recom- oral bisphosphonate therapy do not always result in osteo-
mended to determine the extent of necrosis and the posi- necrosis of jaw but it also depends on the duration of the
tion of sequestrum or osteomyelitis. therapy. The American association of oral and maxillofacial
2. Microbial cultures from the associated soft tissue surgeons do not contraindicate the dental implant placement
swelling or purulent discharge should be done to identify in patients taking oral bisphosphonates for fewer than three
any superinfection and the appropriate antimicrobial years prior to surgery provide that they do not present with
therapy. other risk factors such as medication with steroids or advance
3. Any additional dental trauma should be avoided as it may age. If the patient has been taking medicine for more than 3
further delay wound healing. years it has been recommended to stop the medicine for at
4. ONJ should be properly characterized and staging should be least 3 months before carrying out any surgical procedure and
done so that appropriate treatment can be done (Table 2).12 once the healing is complete the drug can be taken.
Table 3 e Recent studies showed the incidence of osteonecrosis in patients on bisphosphonate therapy.
Author Year Sample No. Of Bisphosph–onate Mode of Incidence of
implants therapy duration administration osteonecrosis
Marx11 2005 119 cases of osteonecrosis e 3 Oral 4 cases of osteonecrosis
in patients treated with deriving from implants
oral bisphosphonates
Jeffcoat36 2006 25 patients 102 25 (for 3 years on average) Oral No case of osteonecrosis
Wang37 2007 1 5 1 (for more than ten years) Oral 1
Marx38 2007 30 cases of osteonecrosis e 30 Oral 2 deriving from implant
in patients treated with placement
oral bisphosponates
Fugazzotto39 2007 61 169 61 (3 year average) Oral Torus exposure around on
post extraction implant
which closed
spontaneously after four
weeks
Grant40 2008 115 468 89 (33 for more than 3 Oral None
years)
j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0 29
jaws: risk factors, recognition, prevention and treatment.
5. Conclusion J Oral Maxillofac Surg. 2005;63:1567e1575.
12. Mehrotra B, Ruggiero SL. Bisphosphonate complications
Since the introduction of bisphosphonates they have been including osteonecrosis of the jaw. Hematology Am Soc Hematol
used to treat multiple bone disorders and cancers. In routine Educ Program; 2006::356e360.
13. Migiliorati CA, Casiglia J, Jacobsen PL, Siegel MA, Woo S-K.
dental practice clinicians come across many patients who are
Managing the care of patients with bisphosphonate-
receiving bisphosphonates as part of their therapy. Most
associated osteonecrosis. J Am Dent Assoc.
commonly postmenopausal female patient who are receiving 2005;136:1658e1668.
bisphosphonates as a treatment for osteoporosis which is very 14. Chun YH, Foster BL, Lukasavage PA. Bisphosphonate
common for their age group, are encountered. These patients modulates cementoblast behaviour in vitro. J Periodontol.
are at increased risk of developing ONJ when any dental 2005;76:1890e1900.
treatment is done or patient is suffering from dental disease. 15. Badros A, Weikel D, Salama A, et al. Osteonecrosis of the jaw
in multiple myeloma patients: clinical features and risk
So it becomes important to identify such patients and follow a
factors. J Clin Oncol. 2006;24(6):945e952.
suggested protocol to avoid complications. It is also important 16. Bannias A, Kastritis E, Bannia C, et al. Osteonecrosis of the
to identify various risk factors for the patient who might jaw in cancer after treatment with bisphosphonates:
develop bisphosphonate induced ONJ prior to any dental incidence and risk factors. J Clin Oncol. 2005;23:8580e8587.
procedure. 17. Dimopoulos M, Kastritis E, Amagnostopoulos A, et al.
Osteonecrosis of the jaw in patients with multiple myeloma
treated with bisphosphonates: evidence of increased risk
after treatment with zoledronic acid. Hematologica.
Conflicts of interest 2006;91:968e971.
18. Woo SB, Hell Stein JW, Kalmar JR. Systematic review:
All authors have none to declare. bisphosphonates and osteonecrosis of the jaw. Ann Intern
Med. 2006;144:753e761.
19. Durie BG, Katz M, Crowley J. Osteonecrosis of the jaw and
bisphosphonates. N Engl J Med. 2005;353:99e102.
references 20. Corso A, Varettoni M, Zappasodi P, et al. A different schedule
of zoledronic acid can reduce the risk of the osteonecrosis of
the jaw in patients with multiple myeloma. Leukemia.
1. Montoya-Carralero JM, Parra-Mino P, Ramı́rez-Fernández P, 2007;21:1545e1548.
Morata-Murcia IM, Mompeán-Gambı́n Mdel C, Calvo- 21. Hoff AO, Toth BB, Altundag K, et al. Frequency and risk
Guirado JL. Dental implants in patients treated with oral factors associated with osteonecrosis of the jaw in cancer
bisphosphonates: a bibliographic review. Med Oral Patol Oral patients treated with intravenous bisphosphonates. J Bone
Cir Bucal. 2010;15(1):e65ee69. Miner Res. 2008;23:826e836.
2. Serra MP, Llorca CS, Donat FJ. Oral implants in patients 22. Kyrgidis A, Vahtsevanos K, Koloutsos G, et al. Bisphosphonate
receiving bisphosphonates: a review and update. Med Oral related osteonecrosis of the jaws: risk factors in breast cancer
Patol Oral Cir Bucal. 2008;13:e755ee760. patients. A case control study. J Clin Oncol. 2008;26:4634e4638.
3. Russell RGG, Watts NB, Ebetino FH, Rogers MJ. Mechanisms of 23. Jadu F, Lee L, Pharoah M, Reece D, Wang L. A retrospective
action of bisphosphonates: similarities and differences and study assessing the incidence, risk factors and comorbidities
their potential influence on clinical efficacy. Osteoporos Int. of pamidronate-related necrosis of the jaws in multiple
2008;19:733e759. myeloma patients. Ann Oncol. 2007;18:2015e2019.
4. Ezra A, Golomb G. Administration routes and delivery 24. Abu-Id MH, Warnke PH, Gottschalk J, et al. “Bis-phossy
systems of bisphosphonates for the treatment of bone jaws”dhigh and low risk factors for bisphosphonate-induced
resorption. Adv Drug Deliv Rev. 2000;42:175e179. osteonecrosis of the jaw. J Craniomaxillofac Surg.
5. Berenson JR, Rosen L, Vesico R, et al. Pharmacokinetics of 2008;36:95e103.
pamidronate disodium in patients with cancer with normal 25. Zervas K, Verrou E, Teleioudis Z, et al. Incidence, risk factors
or impaired renal function. J Clin Pharmacol. 1997;37:285e290. and management of osteonecrosis of the jaw in patients with
6. Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism multiple myeloma: a single-centre experience in 303 patients.
of action and role in clinical practice. Mayo Clin Proc. Br J Haematol. 2006;134:620e623.
2008;83:1032e1045. 26. Sarasquete ME, Garcı́a-Sanz R, Marı́n L, et al. Bisphosphonate-
7. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. related osteonecrosis of the jaw is associated with
Osteonecrosis of the jaws associated with the use of polymorphisms of the cytochrome P450 CYP2C8 in multiple
bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. myeloma: a genome-wide single nucleotide polymorphism
2004;62:527e534. analysis. Blood. 2008;112(7):2709e2712.
8. King AE, Umland EM. Osteonecrosis of the jaw in patients 27. Lehrer S, Montazem André, Ramanathan Lakshmi, et al.
receiving intravenous or oral bisphosphonates. Bisphosphonate-Induced osteonecrosis of the jaws, bone
Pharmacotherapy. 2008;28:667e677. markers, and a hypothesized candidate gene. J Oral Maxillofac
9. Ruggiero SL. Bisphosphonate-related osteonecrosis of the Surg. 2009;67(1):159e161.
jaws. Compend Contin Educ Dent. 2008;29:96e98. 100-102, 104- 28. Wessel JH, Dodson TB, Zavras AI. Zoledronate, smoking,
105. and obesity are strong risk factors for osteonecrosis of the
10. Russell RGG, Xia Z, Dunford JE, et al. Bisphosphonates.An jaw: a case-control study. J Oral Maxillofac Surg.
update on mechanisms of action and how these relate to 2008;66:625e631.
clinical efficacy. In: Zaidi M, ed. Skeletal Biology and Medicine. 29. Ardine M, Generali D, Donadio M, et al. Could the long-term
Ann N Y Acad Sci. 2007;1117:209e257. persistence of low serum calcium levels and high serum
11. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate parathyroid hormone levels during bisphosphonate
induced exposed bone (osteonecrosis/osteoporosis) of the treatment predispose metastatic breast cancer patients to
30 j o u r n a l o f o r a l b i o l o g y a n d c r a n i o f a c i a l r e s e a r c h 3 ( 2 0 1 3 ) 2 5 e3 0
undergo osteonecrosis of the jaw? Ann Oncol. osteonecrosis of the jaws. Available at: http://www.aae.org/
2006;17:1336e1337. dentalpro/guidelines.htm. Accessed on 14.08.2006.
30. Khamaisi M, Regev E, Yarom N, et al. Possible association 36. Jeffcoat MK. Safety of oral bisphosphonates: controlled
between diabetes and bisphosphonate-related jaw studies on alveolar bone. Int J Oral Maxillofac Implants.
osteonecrosis. J Clin Endocrinol Metab. 2007;92(3):1172e1175. 2006;21:349e353.
Epub 2006 Dec 19. 37. Wang HL, Weber D, McCauley LK. Effect of long term oral
31. Hess LM, Jeter JM, Benham-Hutchins M, Alberts DS. Factors bisphosphonates on implant wound healing: literature
associated with osteonecrosis of the jaw among review and a case report. J Periodontol. 2007;78:584e594.
bisphosphonate users. Am J Med. 2008;121:475e483. 38. Marx RE, Cillo Jr JE, Ulloa JJ. Oral bisphosphonate induced
32. Damata K, Gralow J, Hoff A, et al. Recommendation for osteonecrosis: risk factors, prediction of risk using serum CTX
Prevention, Diagnosis and Treatment of Osteonecrosis of Jaws testing, prevention and treatment. J Oral Maxillofac Surg.
(Expert Panel). Novartis Pharmaceuticals; 2004. 2007;65:2397e2410.
33. Ruggiero S, Gralow J, Marx RE, et al. Practical guidelines for 39. Fugazzoto PA, Lightwood WS, Jaffin R, Kumar A. Implant
prevention, diagnosis and treatment of osteonecrosis of jaw placement with or without simultaneous tooth extraction in
in patient with cancer. J Oncol Pract. 2006;2:7e14. patients taking oral bisphosphonates: postoperative healing,
34. Greenspan SI, Rosen HN, Parker RA. Early changes in serum early follow-up, and the incidence of complications in two
N-telopeptide and C- telopeptide cross linked collagen type I private practices. J Periodontol. 2007;78:1664e1669.
predict long term response to alendronate therapy in elderly 40. Grant BT, Amenedo C, Freeman K, Kraut RA. Outcomes of
women. J Clin Endocrinol Metab. 2000;85:3357e3540. placing dental implants in patients taking oral
35. American Association of Endodontists Position Statement. bisphosphonates: a review of 115 cases. J Oral Maxillofac Surg.
Endodontic implications of bisphosphonate-associated 2008;66:223e230.
You might also like
- The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone ReconstructionFrom EverandThe Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone ReconstructionRating: 4 out of 5 stars4/5 (1)
- BISPHOSPHONATESDocument18 pagesBISPHOSPHONATEShumaNo ratings yet
- Thirunavukarasu 2015Document4 pagesThirunavukarasu 2015James Alexander Toruño GordonNo ratings yet
- Bisphosonatesstatement PDFDocument4 pagesBisphosonatesstatement PDFiulian tigauNo ratings yet
- Manejo de Pacientes Con BisfosfonatosDocument6 pagesManejo de Pacientes Con Bisfosfonatosmaria alejandra alarconNo ratings yet
- The Dental Implication of Bisphosphonates RJNDocument10 pagesThe Dental Implication of Bisphosphonates RJNmaxfaxNo ratings yet
- Bisphosphonate and Dental Implant (Power Point) (FINAL)Document30 pagesBisphosphonate and Dental Implant (Power Point) (FINAL)Shehab RehanyNo ratings yet
- BifosfonatDocument2 pagesBifosfonatHusnul Khatimah ImaduddinNo ratings yet
- Medoralv15 I1 p65Document5 pagesMedoralv15 I1 p65Guilherme GuerraNo ratings yet
- Tooth Socket HealingDocument16 pagesTooth Socket HealingluisNo ratings yet
- The Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementDocument11 pagesThe Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementHemil Dario Rosales MolinaNo ratings yet
- BRONJ (Bisphosphonates-Related Osteonecrosis of The Jaw)Document3 pagesBRONJ (Bisphosphonates-Related Osteonecrosis of The Jaw)drfarazNo ratings yet
- BRONJinDentalImplantPatientsGossAustralia PDFDocument7 pagesBRONJinDentalImplantPatientsGossAustralia PDFJing XueNo ratings yet
- Bisphosphonates Marx OMS ClinicsDocument12 pagesBisphosphonates Marx OMS ClinicsDeb SNo ratings yet
- BisphosphonateDocument33 pagesBisphosphonatelavate amol bhimraoNo ratings yet
- Katz 2005Document4 pagesKatz 2005Leonardo AmaralNo ratings yet
- Articulo Bifosfonato en InglesDocument6 pagesArticulo Bifosfonato en InglesLeidy Marín SantanaNo ratings yet
- BifosfonatosyortodonciaDocument8 pagesBifosfonatosyortodonciavivigaitanNo ratings yet
- Understanding Bisphosphonates and Osteonecrosis of The JawDocument9 pagesUnderstanding Bisphosphonates and Osteonecrosis of The JawGabriela OlateNo ratings yet
- Using Bisphosphonates Safely and OptimallyDocument2 pagesUsing Bisphosphonates Safely and OptimallyPablo IgnacioNo ratings yet
- Articol Acidul ZoledronicDocument13 pagesArticol Acidul ZoledronicAndreea GorbanescuNo ratings yet
- Bisphosphonates and ONJ Risk FactorsDocument2 pagesBisphosphonates and ONJ Risk FactorsJames SandersNo ratings yet
- Drug-Induced Osteonecrosis of The JawDocument7 pagesDrug-Induced Osteonecrosis of The Jawbucomaxilofacial.hfiNo ratings yet
- Iglesias-Linares Et Al. (2010)Document9 pagesIglesias-Linares Et Al. (2010)Laís C. PoletoNo ratings yet
- OsteonecrosisDocument6 pagesOsteonecrosisJaneth Dinorah Rodríguez CanoNo ratings yet
- Bisphosphonate-Associated Osteonecrosis of The Jaw: A Literature Review and Clinical Practice GuidelinesDocument12 pagesBisphosphonate-Associated Osteonecrosis of The Jaw: A Literature Review and Clinical Practice GuidelinesIrma Noor FitriastariNo ratings yet
- BiphosphonatesDocument14 pagesBiphosphonatesadrianajg.drNo ratings yet
- Dental Extractions and Bisphosphonates: The Assess-Ment, Consent and Management, A Proposed AlgorithmDocument6 pagesDental Extractions and Bisphosphonates: The Assess-Ment, Consent and Management, A Proposed Algorithmdent12No ratings yet
- Bi Pos PhonateDocument24 pagesBi Pos PhonateBudhiNo ratings yet
- Katz 2005Document4 pagesKatz 2005Leonardo AmaralNo ratings yet
- Bisphosphonate induced osteonecrosisDocument3 pagesBisphosphonate induced osteonecrosisZohair AlamNo ratings yet
- PicnoDocument4 pagesPicnoCaio GonçalvesNo ratings yet
- Self-Healing Lesion of Bisphosphonate Induced Osteonecrosis of Maxilla in An Osteoporotic Patient: A Case ReportDocument17 pagesSelf-Healing Lesion of Bisphosphonate Induced Osteonecrosis of Maxilla in An Osteoporotic Patient: A Case ReportYahul MazfarNo ratings yet
- Case Report BisphospanateDocument3 pagesCase Report BisphospanatedoctorniravNo ratings yet
- 732-Article Text-1301-1-10-20230406Document6 pages732-Article Text-1301-1-10-20230406Meiky eka SaputraNo ratings yet
- BifosfonatosDocument6 pagesBifosfonatosAna Paulina Marquez LizarragaNo ratings yet
- Overview of Bisphosphonate Use in Children FinalDocument2 pagesOverview of Bisphosphonate Use in Children FinalAko KareemNo ratings yet
- Jper 0584Document11 pagesJper 0584LoredanaNo ratings yet
- Paget's disease presenting with root resorptionDocument4 pagesPaget's disease presenting with root resorptionNurani AtikasariNo ratings yet
- Yuh 2014Document10 pagesYuh 2014Celyne DavoglioNo ratings yet
- Pathogenesis ONMAM - final bueno para desconocimiento de bronjDocument10 pagesPathogenesis ONMAM - final bueno para desconocimiento de bronjJose IgnacioNo ratings yet
- NSW Health BiphosphoanteDocument31 pagesNSW Health BiphosphoanteChaiNo ratings yet
- Is Dental Implant Placement Compatible in Patients Treated With BiphosphonatesDocument5 pagesIs Dental Implant Placement Compatible in Patients Treated With BiphosphonatesosiglesiNo ratings yet
- Osteonecrosis of The Jaw (ONJ) : Division of Oral Medicine and DentistryDocument2 pagesOsteonecrosis of The Jaw (ONJ) : Division of Oral Medicine and DentistrySyeda Nasra ShahNo ratings yet
- Sonnykalangi,+40 +ok+ (6) +Nidia+Limarga+550-555+doiDocument6 pagesSonnykalangi,+40 +ok+ (6) +Nidia+Limarga+550-555+doialif kausarNo ratings yet
- Aipg 2016Document115 pagesAipg 2016Gowri ShankarNo ratings yet
- Extreme Root Resorption Associated With Induced Tooth Movement - A Protocol For Clinical ManagementDocument8 pagesExtreme Root Resorption Associated With Induced Tooth Movement - A Protocol For Clinical Managementcarmen espinozaNo ratings yet
- Ozono 3Document3 pagesOzono 3aramirezp09No ratings yet
- Bisphosphonate-Related Osteonecrosis of The Jaws: A Comprehensive ReviewDocument10 pagesBisphosphonate-Related Osteonecrosis of The Jaws: A Comprehensive Reviewiulian tigauNo ratings yet
- Bisphosphonates: - Bisphosphonates (Also Called Diphosphonates) Are A Class of Drugs That Prevent The Loss of Bone MassDocument3 pagesBisphosphonates: - Bisphosphonates (Also Called Diphosphonates) Are A Class of Drugs That Prevent The Loss of Bone Massglaire927No ratings yet
- Freeman Hospital, Newcastle Upon Tyne, United KingdomDocument21 pagesFreeman Hospital, Newcastle Upon Tyne, United KingdomcozcozNo ratings yet
- Medication Related Osteonecrosis of The JawDocument26 pagesMedication Related Osteonecrosis of The Jawapi-265532519100% (1)
- Papillon Lefevre PublishedDocument6 pagesPapillon Lefevre PublishedAIRA BIANCA B. MANALANGNo ratings yet
- A Actynomices Deceulaer2014Document8 pagesA Actynomices Deceulaer2014Popescu MariaNo ratings yet
- Procedure For The Infusion of Biphosphonate Drugs in Clinical Oncology OutpatientsDocument12 pagesProcedure For The Infusion of Biphosphonate Drugs in Clinical Oncology OutpatientsJyothsna S ReddyNo ratings yet
- Oral Osteonecrosis Induced by Drugs in A Multiple Myeloma PatientDocument4 pagesOral Osteonecrosis Induced by Drugs in A Multiple Myeloma Patientbraily_cardenasNo ratings yet
- Fibrin Rich in Leukocytes and Platelets L PRF and Bisphosphonate Induced Osteonecrosis We Need To Advertise NowDocument7 pagesFibrin Rich in Leukocytes and Platelets L PRF and Bisphosphonate Induced Osteonecrosis We Need To Advertise NowEditor IJTSRDNo ratings yet
- Sarathy 2005Document5 pagesSarathy 2005Leonardo AmaralNo ratings yet
- Bone Turnover Markers To Monitor Oral Bisphosphonate TherapyDocument6 pagesBone Turnover Markers To Monitor Oral Bisphosphonate Therapyhossein kasiriNo ratings yet
- Art - 3A10.1007 - 2Fs12105 007 0033 2Document9 pagesArt - 3A10.1007 - 2Fs12105 007 0033 2Isteicy CortezNo ratings yet
- Development and Validation of A Predictive Model For Incident Type 2 Diabetes in Middle-Aged Mexican Adults The Metabolic Syndrome CohortDocument10 pagesDevelopment and Validation of A Predictive Model For Incident Type 2 Diabetes in Middle-Aged Mexican Adults The Metabolic Syndrome CohortyomiboyNo ratings yet
- Genetic Instability and Oral CancerDocument6 pagesGenetic Instability and Oral CanceryomiboyNo ratings yet
- Development and Validation of A Predictive Model For Incident Type 2 Diabetes in Middle-Aged Mexican Adults The Metabolic Syndrome CohortDocument10 pagesDevelopment and Validation of A Predictive Model For Incident Type 2 Diabetes in Middle-Aged Mexican Adults The Metabolic Syndrome CohortyomiboyNo ratings yet
- Bisphosphonates and Their Clinical Implications in Endodontic TherapyDocument8 pagesBisphosphonates and Their Clinical Implications in Endodontic TherapyyomiboyNo ratings yet
- Clinical Impact of Bisphosphonates in Root Canal TherapyDocument7 pagesClinical Impact of Bisphosphonates in Root Canal TherapyyomiboyNo ratings yet
- Obesity and Periodontitis A Link PDFDocument4 pagesObesity and Periodontitis A Link PDFyomiboyNo ratings yet
- New Classification For Periodontal Diseases 2017 PDFDocument367 pagesNew Classification For Periodontal Diseases 2017 PDFblokolbNo ratings yet
- Severe Periodontitis Is Associated With Insulin Resistance in Non-Abdominal Obese AdultsDocument9 pagesSevere Periodontitis Is Associated With Insulin Resistance in Non-Abdominal Obese AdultsyomiboyNo ratings yet
- Relationship Between Obesity, Glucose Tolerance, and Periodontal Disease in Japanese Women: The Hisayama StudyDocument8 pagesRelationship Between Obesity, Glucose Tolerance, and Periodontal Disease in Japanese Women: The Hisayama StudyyomiboyNo ratings yet
- Severe Periodontitis Is Associated With Insulin Resistance in Non-Abdominal Obese AdultsDocument9 pagesSevere Periodontitis Is Associated With Insulin Resistance in Non-Abdominal Obese AdultsyomiboyNo ratings yet
- Depression and Inflamatory Periodontal Disease Considerations - An Interdisciplinary ApproachDocument8 pagesDepression and Inflamatory Periodontal Disease Considerations - An Interdisciplinary ApproachyomiboyNo ratings yet
- Microbiology Past, Present & Future.Document13 pagesMicrobiology Past, Present & Future.yomiboyNo ratings yet
- Adiposity Measurements and Non-Surgical Periodontal Therapy Outcomes.Document8 pagesAdiposity Measurements and Non-Surgical Periodontal Therapy Outcomes.yomiboyNo ratings yet
- Association Between Type 2 Diabetes Mellitus and Anthropometric Measurements - A Case Control Study in South IndiaDocument7 pagesAssociation Between Type 2 Diabetes Mellitus and Anthropometric Measurements - A Case Control Study in South IndiayomiboyNo ratings yet
- Skugor TreatmentofdiabetesmellitusDocument5 pagesSkugor TreatmentofdiabetesmellitusyomiboyNo ratings yet
- Periodontal InfectionDocument8 pagesPeriodontal InfectionAmelyahNo ratings yet
- Cirugía EndodonticaDocument23 pagesCirugía Endodonticajaimerendon0978No ratings yet
- V 19 N 2 A 05Document5 pagesV 19 N 2 A 05akhileshrajanNo ratings yet
- Armitage 1999 PDFDocument6 pagesArmitage 1999 PDFnydiacastillom2268No ratings yet
- Increased Physical Activity Reduces Prevalence of PeriodontitisDocument8 pagesIncreased Physical Activity Reduces Prevalence of PeriodontitisyomiboyNo ratings yet
- V 19 N 2 A 05Document5 pagesV 19 N 2 A 05akhileshrajanNo ratings yet
- Association Between Dental Prosthesis and Periodontal Disease in A Rural Brazilian CommunityDocument6 pagesAssociation Between Dental Prosthesis and Periodontal Disease in A Rural Brazilian CommunityyomiboyNo ratings yet
- Genetic Instability and Oral CancerDocument6 pagesGenetic Instability and Oral CanceryomiboyNo ratings yet
- Diabesity and Periodontal Disease Relationship and ManagementDocument5 pagesDiabesity and Periodontal Disease Relationship and ManagementyomiboyNo ratings yet
- Wisdom Tooth-Complications in ExtractionDocument4 pagesWisdom Tooth-Complications in ExtractionyomiboyNo ratings yet
- P 1 OpeDocument1 pageP 1 OpeyomiboyNo ratings yet
- V 19 N 2 A 05Document5 pagesV 19 N 2 A 05akhileshrajanNo ratings yet
- 2.factory Price - Alarm Accessories-Complete 20150325Document15 pages2.factory Price - Alarm Accessories-Complete 20150325FREE BUSINESS INTELLIGENCENo ratings yet
- Pengaruh Ukuran Potongan Kopra Dalam Proses Pengeringan: Effect of The Copra Cut Size in The Drying ProcessDocument5 pagesPengaruh Ukuran Potongan Kopra Dalam Proses Pengeringan: Effect of The Copra Cut Size in The Drying ProcessAlexia Desi Ratnasari Loi 1841100210No ratings yet
- Papers Traducir CompletoDocument12 pagesPapers Traducir CompletoJuan Jesus Barreda TalaveraNo ratings yet
- Pathology AIIMSDocument26 pagesPathology AIIMSvkNo ratings yet
- Rational Choice TheoryDocument6 pagesRational Choice TheoryMaria Theresa HerbolingoNo ratings yet
- Radio Frequency Field - Bioeffects & SafetyDocument37 pagesRadio Frequency Field - Bioeffects & SafetyAmel AntonyNo ratings yet
- D754te3 VMDocument37 pagesD754te3 VMGurpreet SinghNo ratings yet
- Symbol High Low R5 R4 R3 R2: DailyDocument8 pagesSymbol High Low R5 R4 R3 R2: Daily257597 rmp.mech.16No ratings yet
- Production Chemistry and Flow Assurance SimulationDocument21 pagesProduction Chemistry and Flow Assurance SimulationWael Badri100% (1)
- Work Permit Renewal Application FormDocument2 pagesWork Permit Renewal Application FormyamojodnabNo ratings yet
- Population Ecology: Aecc-I +3 1 YearDocument32 pagesPopulation Ecology: Aecc-I +3 1 YearAnita kumari SahuNo ratings yet
- Scope Management Plan TemplateDocument10 pagesScope Management Plan TemplateAlessandro Rota100% (1)
- World Bank ReportDocument14 pagesWorld Bank Reportaditya_erankiNo ratings yet
- Ats, TT, Tig: Anti Tetanus Serum, Tetanus Toxoid, Tetanus Immuno-GlobulinDocument15 pagesAts, TT, Tig: Anti Tetanus Serum, Tetanus Toxoid, Tetanus Immuno-Globulinjisoo100% (2)
- Accessibility POC: October 26, 2017Document7 pagesAccessibility POC: October 26, 2017Ramesh BodukaniNo ratings yet
- General Psychology Mid Term ExamDocument2 pagesGeneral Psychology Mid Term Examapi-534780597No ratings yet
- GAD Accomplishment ReportDocument1 pageGAD Accomplishment ReportRenante Naga100% (6)
- Order - Judgement Query Coram WiseDocument13 pagesOrder - Judgement Query Coram Wisesatish_CJNo ratings yet
- Pharmaceutical Microbiology - B.pharmDocument383 pagesPharmaceutical Microbiology - B.pharmkeyurNo ratings yet
- Effect of Non-Newtonian Fluids On The Performance of Plate Type Heat ExchangerDocument4 pagesEffect of Non-Newtonian Fluids On The Performance of Plate Type Heat Exchangerdeepika snehiNo ratings yet
- Aiesha Edward Resume2Document2 pagesAiesha Edward Resume2api-491571342No ratings yet
- A Project Report: Maya Engineering WorksDocument2 pagesA Project Report: Maya Engineering WorksVishwendra SinghNo ratings yet
- Comparing Food with Comparative AdjectivesDocument4 pagesComparing Food with Comparative AdjectivesLuisito GonzalezNo ratings yet
- Fosfomycin: Review and Use Criteria BackgroundDocument12 pagesFosfomycin: Review and Use Criteria BackgroundAbu Azzam Al-Hadi100% (1)
- SEN Code of Practice 2001Document148 pagesSEN Code of Practice 2001Matt GrantNo ratings yet
- Johnson Et Al.2006. Felidae PhylogenyDocument6 pagesJohnson Et Al.2006. Felidae Phylogenyaspergillus_jallNo ratings yet
- Ramial Chipped Wood - A Basic Tool For Regenerating SoilsDocument15 pagesRamial Chipped Wood - A Basic Tool For Regenerating SoilsmrmiscNo ratings yet
- Pre-Final Exam in Audit 2-3Document5 pagesPre-Final Exam in Audit 2-3Shr BnNo ratings yet
- Cambridge BiologyDocument78 pagesCambridge BiologyBraweet SapkotaNo ratings yet
- Sprocket Asa 180Document1 pageSprocket Asa 180jhampolrosalesNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (18)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Secure Love: Create a Relationship That Lasts a LifetimeFrom EverandSecure Love: Create a Relationship That Lasts a LifetimeRating: 5 out of 5 stars5/5 (18)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)