Professional Documents
Culture Documents
ACEIII
Uploaded by
Ingrid IturrietaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ACEIII
Uploaded by
Ingrid IturrietaCopyright:
Available Formats
International Psychogeriatrics: page 1 of 9 © International Psychogeriatric Association 2016
doi:10.1017/S1041610216001496
Addenbrooke’s cognitive examination III: diagnostic utility for
mild cognitive impairment and dementia and correlation with
standardized neuropsychological tests
...........................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................................
Jordi A. Matias-Guiu, Ana Cortés-Martínez, Maria Valles-Salgado, Teresa Rognoni,
Marta Fernández-Matarrubia, Teresa Moreno-Ramos and Jorge Matías-Guiu
Department of Neurology, Hospital Clínico San Carlos, San Carlos Institute for Health Research (IdISSC), Universidad Complutense de Madrid, Madrid,
Spain
ABSTRACT
Background: Addenbrooke’s Cognitive Examination III (ACE-III) is a screening test that was recently
validated for diagnosing dementia. Since it assesses attention, language, memory, fluency, and visuospatial
function separately, it may also be useful for general neuropsychological assessments. The aim of this study
was to analyze the tool’s ability to detect early stages of Alzheimer’s disease and to examine the correlation
between ACE-III scores and scores on standardized neuropsychological tests.
Methods: Our study included 200 participants categorized as follows: 25 healthy controls, 48 individuals with
subjective memory complaints, 47 patients with amnestic mild cognitive impairment and 47 mild Alzheimer’s
disease, and 33 patients with other neurodegenerative diseases.
Results: The ACE-III memory and language domains were highly correlated with the neuropsychological
tests specific to those domains (Pearson correlation coefficient of 0.806 for total delayed recall on the Free
and Cued Selective Reminding Test vs. 0.744 on the Boston Naming Test). ACE-III scores discriminated
between controls and patients with amnestic mild cognitive impairment (AUC: 0.906), and between controls
and patients with mild Alzheimer’s disease (AUC: 0.978).
Conclusion: Our results suggest that ACE-III is a useful neuropsychological test for assessing the cognitive
domains of attention, language, memory, and visuospatial function. It also enables detection of Alzheimer’s
disease in early stages.
Key words: Addenbrooke’s cognitive examination, cognitive screening, dementia, neuropsychological assessment, Alzheimer’s disease
Introduction studies has reported a good diagnostic ability to
discriminate between healthy people and patients
Addenbrooke’s Cognitive Examination (ACE) has with dementia.
been validated in several languages and possesses However, we need cognitive tools that are able
good diagnostic and psychometric properties for to detect neurodegenerative diseases, and especially
diagnosing Alzheimer’s disease (AD) and other AD, at earlier stages. Relatively few studies have
types of dementia (Mathuranath et al., 2000). The evaluated the utility of ACE for diagnosing mild
third version of this test, ACE-III, was recently cognitive impairment (MCI) (Crawford et al.,
developed and validated in English and in Spanish 2012; Larner and Mitchell, 2014; Menon et al.,
(Hsieh et al., 2013; Matías-Guiu et al., 2015; 2014). The ACE-III total score and scores of its five
Matías-Guiu et al., 2016a). Each of these validation cognitive domains (attention, memory, language,
verbal fluency, and visuospatial abilities) make it
potentially useful for detecting neurodegenerative
Correspondence should be addressed to: Jordi A. Matias-Guiu, Department of
Neurology, Hospital Clinico San Carlos, San Carlos Institute for Health
diseases in early stages and establishing a cognitive
Research (IdISSC), Universidad Complutense, Calle Profesor Martin Lagos profile that may aid in differential diagnosis
S/N, 28040, Madrid, Spain. Phone: +34676933312, +34913303511. Email: (Matías-Guiu et al., 2016b).
jordimatiasguiu@hotmail.com, jordi.matias-guiu@salud.madrid.org. Received
24 Apr 2016; revision requested 16 May 2016; revised version received 31 Jul
Our hypothesis was that ACE-III may be
2016; accepted 19 Aug 2016. useful to establish a cognitive profile and for the
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
2 J. A. Matias-Guiu et al.
assessment of early stages of AD. The purpose of Furthermore, a group of 25 healthy controls
the present study is two-fold. First, we assessed (group 5) was recruited among healthy volunteers
the correlation between ACE-III domains and the and patients’ relatives. These were participants
neuropsychological tests specific to each cognitive presenting no neurological or systemic diseases
function in order to establish the ability of the potentially affecting cognitive function, no current
ACE-III to detect cognitive deficit affecting specific psychiatric disorders, and no history of abusing al-
domains. Second, we studied the diagnostic ability cohol or other substances. Healthy controls had no
of the ACE-III in patients with MCI and mild AD. cognitive and no functional impairment, according
to the Mini-Mental State Examination (MMSE)
adjusted for age and education > 24 (Blesa et al.,
2001), a global Clinical Dementia Rating equal
Methods to 0, a Functional Activities Questionnaire (FAQ)
of 0 (Pfeffer et al. 1982; Morris, 1993), absence
Study design
of depression according to Hamilton Depression
We conducted a prospective cross-sectional study scale (Hamilton, 1960), and absence of subjective
validating the ability of the ACE-III to detect memory or cognitive complaints.
deficits in the cognitive domains of attention,
memory, language, and visuospatial abilities. This
Neuropsychological assessment
research project was approved by the ethics
committee at our hospital. All patients were evaluated by two neuro-
logists specialized in cognitive neurology and
by structural neuroimaging. Neuropsychologists
Study sample administered the MMSE and ACE-III (Spanish
The study included 175 consecutively recruited version, available from www.neura.edu.au/frontier/
patients who visited our center between May 2014 research/test-downloads).
and November 2015 due to cognitive symptoms. Patients also completed a neuropsychological
Patients included in this study were different from assessment protocol including several tests from
those that participated in the previous work of NEURONORMA, a normative data project con-
validation of ACE-III in Spain (Matías-Guiu et al., ducted in Spain (Peña-Casanova et al., 2009).
2015). This project is similar to Mayo’s Older Americans
The inclusion criteria were being aged 50 Normative Studies (MOANS) in the USA. The
years or older and having sufficient physical tests included in our study were as follows: memory
capability and auditory and visual acuity for the span (forward and backward digit spans), the Corsi
neuropsychological assessment. block-tapping test, Trail Making Test (TMT),
Patients were classified in four groups according Symbol Digit Modalities Test (SDMT), Boston
to the results from the diagnostic study: Naming Test (BNT), Visual Object and Space
Perception Battery (VOSP; subtests for object
decision, progressive silhouettes, position discrim-
1. Individuals with subjective memory complaints ination, and number location), Judgement of
but with no objective cognitive impairment. We Line Orientation (JLO), Tower of London-Drexel
included patients reporting symptoms of memory loss University, Free and Cued Selective Reminding
but whose neuropsychological tests did not indicate Test (FCSRT), Rey–Osterrieth Complex Figure
cognitive impairment. Thus, age- and education- Test (copy and memory), and Stroop Color–Word
adjusted scores were above the percentile 11–18 Interference Test. Following the NEURONORMA
(scaled score 7 or higher). Other cognitive or authors’ recommendations, a scaled score ≤ 5
behavioral symptoms were not allowed in this group.
(percentile ≤ 5) was considered deficient. We
2 and 3. Patients with AD. We included all patients
meeting diagnostic criteria for amnestic mild cognitive
also assessed participants’ functional status using
impairment (aMCI; global Clinical Dementia Rating: the Functional Activities Questionnaire (Pfeffer
0.5) (group 2) and mild AD (global Clinical Dementia et al., 1982) and the Clinical Dementia Rating
Rating: 1) (group 3) (Morris, 1993; McKhann et al., scale (Morris, 1993). The diagnostic groups were
2011). created based on results from functional and
4. Patients with other causes of cognitive decline neurological assessments and scores on the battery
(other types of dementia). This group included of tests listed above.
patients with other neurodegenerative diseases (be-
havioral variant of frontotemporal dementia, primary
progressive aphasia, and atypical parkinsonism)
Statistical analysis
(Litvan et al., 1996; McKeith et al., 2005; Gorno- The statistical analysis was conducted using SPSS
Tempini et al., 2011; Rascovsky et al., 2011). Statistics 20.0 by IBM® and MedCalc® 16.4.3.
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
ACE-III for mild cognitive impairment and dementia 3
Kolmogorov–Smirnov test was used to determine p < 0.0001), and a medium correlation with the
normality. We calculated the Pearson correlation copy task of the Rey–Osterrieth complex figure (r
coefficient between ACE-III total and cognitive = 0.461, p value < 0.0001), VOSP-object decision
domain scores and specific neuropsychological (r = 0.348, p value < 0.0001), VOSP-position
test results. All participants were included in the discrimination (r = 0.407, p value < 0.0001),
correlation analyses. The α level of significance and with JLO (r = 0.498, p value < 0.0001).
was set at 0.05; p values < 0.05 were considered The correlation between ACE-III visuospatial and
statistically significant and led to rejection of the VOSP-progressive silhouettes was small (r = –
null hypothesis. These values are indicated with an 0.233, p value = 0.0005).
asterisk (*). p values lower than 0.01 are marked The ACE-III attention domain showed a
with two asterisks (**). medium correlation with the following tests:
We also estimated receiver operating charac- verbal span backward, visuospatial span forward,
teristic curves (ROC) for discriminating between visuospatial span backward, TMT part A, TMT
groups. The gold standard was the neuro- part B, SDMT, ROCF copy accuracy, FCSRT,
psychological study conducted by applying the ROCF memory, Stroop test, VOSP-number loca-
NEURONORMA test battery and comparing tion, and JLO. The correlation with the Tower of
results to the normative data obtained by that London was small. None of the tests showed a large
project (Peña-Casanova et al., 2009). In the ROC correlation with the ACE-III attention domain.
curve analysis, the control group and the group Regarding the ACE-III fluency domain, it showed
with subjective memory complaints were combined a large correlation with SDMT (r = 0.522, p <
in order to estimate the area under the curve 0.0001), BNT (r = 0.549, p < 0.0001), FCSRT
(AUC) used to discriminate non-pathological from total free recall (r = 0.550, p < 0.0001), and Stroop
pathological groups, and only participants aged 65 part B (r = 0.645, p < 0.0001) and part C (r
years or more were selected to avoid differences = 0.543, p < 0.0001), and it showed a medium
in age between groups. The ROC curves were correlation with verbal span backward, TMT
compared using the method proposed by DeLong part B, the other scores of the FCSRT, ROCF
et al. (1988). memory, Stroop part A, and Tower of London total
moves score. Table S1 (available as supplementary
material attached to the electronic version of
Results this paper at www.journals.cambridge.org/jid_IPG)
shows the correlations of ACE-III and its domains
Mean age was 71.94 ± 8.67, 116 of the participants with other tests.
were women (58%), and the mean duration of Furthermore, the correlation between ACE-
formal schooling was 9.77 ± 5.02 years. Of all III (total score) and MMSE was 0.820 (p <
participants included in the study, 25 were healthy 0.0001). The ACE-III (total score) showed a large
controls, 48 had subjective memory complaints, 47 correlation mainly with BNT (r = 0.687, p <
had aMCI, 47 had AD, and 33 had other types 0.0001) and with the FCSRT (especially with total
of dementia (12 with primary progressive aphasia, recall, r = 0.694, p value < 0.0001, and delayed
11 with the behavioral variant of frontotemporal total recall, r = 0.691, p value < 0.0001). The
dementia, and 10 with atypical Parkinsonism). The correlation was lower but still large or medium
demographic distribution and ACE-III scores of with verbal span forward, verbal span backward,
each group are shown in Table 1. The mean scores Corsi’s test forward, Corsi’s test backward, TMT
of the other cognitive tests are provided in Table 2. part A, TMT part B, SDMT, ROCF memory at
3 and 30 minutes, Stroop test, JLO, and VOSP
Correlation between ACE-III cognitive (Table S1).
domains and neuropsychological tests For the memory domain, the AUC discrim-
The ACE-III memory domain was very largely inating deficient scores (scaled score ≤ 5) from
correlated with the FCSRT (r = 0.806 for total normal scores (scaled score ≥ 6) on the FCSRT
recall, p value < 0.0001 and r = 0.806 for (delayed total recall) was 0.902. The language
total delayed recall, p value < 0.0001) and also domain AUC for detecting deficient scores on the
correlated with recall at 30 minutes on the Rey– BNT was 0.909. The AUC of the attention domain
Osterrieth Complex Figure Test (r = 0.554, p for detecting a TMT-B/TMT-A ratio of at least
value < 0.0001). The language domain was highly 3 (suggestive of executive dysfunction) was 0.667,
correlated with the BNT score (r = 0.744, p and for detecting impairment in Tower of London
value < 0.0001). Visuospatial domain has a large (correct moves), the AUC obtained was of 0.799.
correlation with SDMT (r = 0.549, p value < The AUC of the visuospatial domain was 0.780
0.0001) and VOSP-number location (r = 0.501, to detect impairment in JLO, 0.797 in ROCF
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
4 J. A. Matias-Guiu et al.
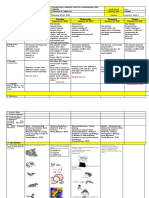
Table 1. Clinical and demographic characteristics of diagnostic groups
SUBJECTIVE
M E M O RY
CO N T RO L S CO M P L A I N T S aM C I , C D R A D, C D R 1 OT H E R T OTA L
(N = 25) (N = 48) 0.5 (N = 47) (N = 47) (N = 33) (N = 200)
............................................................................................................................................................................................................................................................................................................................
Women, n (%) 17 (8.5%) 22 (11%) 26 (13%) 37 (18.5%) 14 (7%) 116 (58%)
Age (years) 65.76 ± 10.16 67.44 ± 8.18 75.85 ± 6.32 75.00 ± 7.25 73.24 ± 7.82 71.94 ± 8.67
Education 12.40 ± 4.99 10.46 ± 5.77 9.68 ± 4.50 7.17 ± 3.23 10.61 ± 5.31 9.77 ± 5.02
(years)
Total MMSE 28.76 ± 1.67 27.67 ± 2.63 24.47 ± 3.22 20.17 ± 4.23 23.36 ± 4.57 24.58 ± 4.61
score
ACE-III (total) 89.44 ± 8.66 83.06 ± 11.80 66.26 ± 10.84 50.94 ± 11.43 60.18 ± 16.00 68.59 ± 18.23
ACE-III 16.48 ± 1.55 15.85 ± 2.50 13.78 ± 2.34 10.76 ± 3.14 12.72 ± 4.22 13.73 ± 3.53
attention
ACE-III 22.48 ± 3.40 19.62 ± 4.21 12.02 ± 3.37 8.63 ± 3.07 12.48 ± 6.03 14.43 ± 6.38
memory
ACE-III 24.24 ± 2.00 22.95 ± 3.35 20.25 ± 4.28 16.38 ± 5.26 18.09 ± 5.42 20.13 ± 5.15
language
ACE-III fluency 16.48 ± 1.55 15.85 ± 2.50 13.78 ± 2.34 10.76 ± 3.14 12.72 ± 4.22 13.73 ± 3.53
ACE-III 14.64 ± 1.22 13.81 ± 2.04 12.00 ± 2.24 10.00 ± 2.85 11.69 ± 3.30 12.24 ± 2.92
visuospatial
Table 2. Main neuropsychological scores
SUBJECTIVE
M E M O RY
CO N T RO L S CO M P L A I N T S aMCI, CDR A D, C D R 1 OT H E R
(N = 25) (N = 48) 0.5 (N = 47) (N = 47) (N = 33)
............................................................................................................................................................................................................................................................................................................................
Verbal span forward 11.37 ± 3.17 11.69 ± 2.26 10.83 ± 3.15 9.96 ± 3.17 9.91 ± 3.41
Verbal span backward 11.29 ± 2.69 11.35 ± 2.68 10.34 ± 2.90 9.26 ± 2.65 8.85 ± 3.31
Corsi forward 11.08 ± 2.56 10.27 ± 2.53 9.11 ± 2.48 8.11 ± 3.23 8.39 ± 3.09
Corsi backward 10.96 ± 3.0 10.23 ± 2.70 9.11 ± 2.64 7.77 ± 2.90 8.48 ± 3.68
TMT-A 9.92 ± 2.0 8.12 ± 2.40 7.46 ± 3.07 5.61 ± 2.38 5.20 ± 4.52
TMT-B 9.42 ± 1.50 8.17 ± 2.42 7.10 ± 2.74 3.25 ± 2.09 4.52 ± 2.43
SDMT 9.79 ± 1.81 8.79 ± 2.04 7.62 ± 3.46 4.48 ± 2.37 5.31 ± 2.72
BNT 10.42 ± 2.14 9.57 ± 2.58 7.06 ± 2.93 5.11 ± 2.68 5.74 ± 3.32
VOSP-object decision 10.83 ± 3.14 10.54 ± 2.44 9.43 ± 2.24 7.53 ± 3.07 9.41 ± 2.53
VOSP-progressive silhouettes 10.67 ± 2.54 10.22 ± 2.47 10.40 ± 2.59 7.96 ± 3.61 10.39 ± 3.46
VOSP-discrimination position 13.92 ± 5.03 12.93 ± 5.68 9.96 ± 5.52 8.40 ± 5.32 10.09 ± 5.53
VOSP-number Location 12.71 ± 4.00 13.07 ± 5.00 9.55 ± 3.77 8.14 ± 4.12 9.29 ± 5.13
JLO 9.86 ± 2.88 9.23 ± 3.23 8.15 ± 2.83 5.05 ± 3.39 7.00 ± 4.32
ToL (correct moves) 10.25 ± 3.71 11.24 ± 2.89 8.78 ± 3.56 5.42 ± 3.98 6.50 ± 3.91
FCSRT total recall 9.83 ± 2.74 8.97 ± 2.89 2.76 ± 1.43 2.70 ± 1.86 4.60 ± 3.57
FCSRT delayed total recall 11.92 ± 3.90 10.44 ± 2.92 3.21 ± 1.66 2.96 ± 1.21 5.52 ± 4.00
ROCF copy accuracy 10.58 ± 2.97 9.48 ± 2.87 7.28 ± 2.29 6.25 ± 2.91 6.45 ± 3.40
ROCF memory (30 minutes) 10.46 ± 2.28 9.81 ± 2.29 5.58 ± 2.69 3.61 ± 2.13 6.50 ± 2.78
Stroop A 10.79 ± 2.16 9.61 ± 2.07 8.80 ± 2.38 7.42 ± 2.50 6.48 ± 2.72
Stroop B 10.25 ± 2.04 9.11 ± 2.28 8.29 ± 2.94 6.45 ± 2.29 4.79 ± 2.62
Stroop C 9.42 ± 2.33 8.98 ± 2.68 8.67 ± 3.14 6.34 ± 2.83 5.79 ± 2.98
(copy), 0.729 in VOSP-discrimination of position, between patient groups. The control group
and 0.777 in VOSP-number location. included participants from groups 1 and 5 (healthy
participants and those with subjective memory
complaints, respectively); participants older than
ACE-III: discriminant ability between groups 65 years were selected to limit age differences
We estimated the ROC curves for the ACE-III between the control group and the patient groups.
and domain scores that were able to discriminate In the group of patients with objective cognitive
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
ACE-III for mild cognitive impairment and dementia 5
Figure 1(a). (Colour online) (a) ROC curves for discriminating between controls and patients with aMCI (CDR 0.5) using ACE-III, ACE-III
cognitive domains, and the MMSE. (b) ROC curves for discriminating between controls and patients with mild AD (CDR 1) using ACE-III,
ACE-III cognitive domains, and the MMSE. (c) ROC curves for discriminating between patients with aMCI (CDR 0.5) and those with mild
AD (CDR 1) using ACE-III, ACE-III cognitive domains, and the MMSE.
impairment suggestive of AD (aMCI and mild the memory domain, and 0.928 for the MMSE
AD), the AUC was 0.891 for ACE-III (total (Figure 1b). The optimal cut-off point for ACE-
score) and 0.942 for the memory domain, while III (total score) was 63/64 with a sensitivity and
the AUC for the MMSE was smaller at 0.853. a specificity of 93.6% and 94.9%, respectively.
Using the DeLong method, pairwise comparison of For the memory domain, the optimal cut-off point
ROC curves was performed. There were significant was 13/14, with a sensitivity of 95.7% and a
differences between the AUC of memory domain specificity of 89.7%. There were no significant
and MMSE (p = 0.007) and ACE-III-total score (p differences among the AUC of ACE-III (total
= 0.01), but not between ACE-III-total score and score), the memory domain, and MMSE, although
MMSE (p = 0.14). a trend toward statistical significance was observed
For discrimination between patients with aMCI between the AUC of the MMSE and memory
(CDR 0.5) and healthy participants with subjective domain (p = 0.06) and between MMSE and
memory complaints, the AUC was 0.817 for ACE- ACE-III (total score) (p = 0.09). Regarding
III (total score), 0.906 for the memory domain, discrimination between patients with aMCI (CDR
and 0.778 for the MMSE (Figure 1a). The optimal 0.5) and those with mild AD (CDR 1), the AUC
cut-off point for ACE-III (total score) was 73/74, was 0.852 for ACE-III (total score), 0.786 for
with a sensitivity of 76.6% and a specificity of the memory domain, and 0.789 for the MMSE
75%. For the memory domain, the optimal cut- (Figure 1c), with no differences between the AUC
off point was 15/16, with a sensitivity of 87.2% (p > 0.05).
and a specificity of 80%. There were significant Last, we analyzed the tool’s ability to discrim-
differences between the AUC of memory domain inate between controls and patients with other
and MMSE (p = 0.005) and ACE-total score (p neurodegenerative diseases. The AUC was 0.850
= 0.003), but not between ACE-III (total score) for ACE-III (total score), 0.816 for the memory
and MMSE (p = 0.30). The AUC discriminating domain, 0.870 for verbal fluency, and 0.805 for the
controls from patients with mild AD (CDR 1) MMSE, although there were no differences in AUC
was 0.966 for ACE-III (total score), 0.978 for between the different scores.
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
6 J. A. Matias-Guiu et al.
Figure 1(b). Continue
Figure 1(c). Continue
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
ACE-III for mild cognitive impairment and dementia 7
Discussion the MMSE. The diagnostic ability of ACE-III was
also high in early stages of AD, especially in the
The present study indicates that ACE-III is a group with aMCI. The memory domain exhibited
useful tool that can assist in the diagnosis of the highest scores on the test, showing an AUC of
aMCI and mild AD. The correlation coefficients 0.906 for diagnosis of the group with aMCI. This
obtained between each ACE-III domain and domain also demonstrated the greatest diagnostic
neuropsychological tests specific to those cognitive ability for the group scoring 1 on the CDR and
domains suggest that ACE-III is a useful screening for patients with suspected AD (CDR 0.5 and 1).
instrument contributing in detection of alterations Memory domain scores were therefore most sensit-
in some cognitive functions. ive for diagnosis, as their sensitivity and specificity
The memory domain was highly correlated with values show. However, the total ACE-III score
the FCSRT; this correlation confirms the finding showed the highest discriminant ability between
of Hsieh et al. (2013) who observed a large CDR scores of 0.5 and 1, which suggests that this
correlation between the memory domain and the score is the most appropriate indicator for patient
Rey Auditory Verbal Learning Test (0.59). The follow-up. This may be explained by the typical
correlation with the FCSRT was also stronger course of cognitive decline in AD: During the first
than that observed between the Montreal Cognitive stage (CDR 0.5), it presents memory impairment
Assessment and several other memory tests (Lam only, while in the second stage (CDR 1) other cog-
et al., 2013). The high correlation with the nitive functions are affected (language, executive
FCSRT is very interesting since that test has function, etc.). In addition, this finding supports
demonstrated its high sensitivity for diagnosing the idea that the usefulness of certain scores
prodromal AD and for stratifying the risk of or domains depends on their clinical application
progression to dementia (Sarazin et al., 2007). We (screening for dementia, screening in early stages,
also observed a marked correlation between the differential diagnosis, etc.) (Matías-Guiu and
language domain and the BNT (r = 0.744), which Fernández-Bobadilla, 2014; Hsieh et al., 2015).
suggests that ACE-III may be useful for cognitive The cut-off point of ACE-III for detecting mild
disorders presenting with language impairment, AD (CDR 1) was 63/64, which is similar to the
whether isolated or not, such as primary progressive cut-off point established by a previous validation
aphasia and AD (Leyton et al., 2010; Matías- study conducted in our setting (Matías-Guiu et al.,
Guiu et al., 2014). The attention domain displayed 2015); 73/74 is the cut-off point for aMCI. While
moderate correlations with tests related to attention these cut-off points are lower than those reported
and executive function: Memory span, the Corsi by other validation studies of English-language
block test, TMT, SDMT, and Stroop Color–Word versions of ACE-R and ACE-III, they resemble
Interference Test. These results are similar to those those reported for populations culturally closer to
reported by Hsieh et al. (2013) who found a our own, such as the Italian population (Pigliautile
correlation of 0.42 between the attention domain et al., 2011). Differences in cut-off points may also
score and the Digit Span Test. This correlation be linked to age and education differences between
is lower than correlations with other domains, patients (Jubb and Evans, 2015). Considering the
a fact that may be due to including orientation effect of these factors on test scores, normative data
within the attention domain as well as the multiple may be more useful than cut-off points.
dimensions of the attention and the executive In the group of patients with other neuro-
function. Similarly, the correlation between verbal degenerative diseases, the verbal fluency domain
fluency scores and executive tests was moderate, and total ACE-III score were shown to have
and visuospatial domain scores, VOSP, and JLO the highest discriminant ability from controls.
were also moderately correlated. There are several This may have been the case because this
reasons that probably explain why this correlation group included patients with language impairment
was not stronger. The visuospatial domain involves (primary progressive aphasia) and/or executive
not only visuospatial tasks, but also constructional dysfunction (frontotemporal dementia, atypical
praxis, which is influenced by visuospatial abilities parkinsonism) but with relatively well-preserved
as well as other factors, such as executive function. memory. In any case, this group is smaller and, to a
In addition, education has a significant impact certain extent, more heterogeneous; further studies
on constructional praxis, which may limit the are necessary to evaluate the usefulness of ACE-III
correlation between tests. in these patients, as well as in differential diagnosis
One of the most relevant finding of our study of neurodegenerative diseases (Elamin et al., 2015).
was that the ACE-III discriminates well between Our study has some limitations. First, in some
groups, in fact this test and specifically the memory analyses, we have combined the groups’ healthy
domain showed greater discriminant ability than controls and subjective memory loss, as well as
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
8 J. A. Matias-Guiu et al.
aMCI and AD. Although it is a controversial issue, Funding
subjective memory complaints might be a very early
symptom of a neurodegenerative disorders (Pedro None.
et al., 2016). Furthermore, not all patients with
aMCI go on to develop AD. Due to the selection
criteria and the comprehensive neuropsychological Supplementary material
protocol used in this study (including FCSRT,
which has been specifically recommended for the To view supplementary material for this
early diagnosis of AD), we think that it is unlikely article, please visit http://dx.doi.org/10.1017/
that patients with subjective memory complaints S1041610216001496
included were at risk of AD, while most patients
with aMCI were, in fact, at high risk of developing
AD. However, further studies evaluating the role References
of ACE-III in the prediction of progression of
aMCI and preclinical stages of AD would be very Blesa, R. et al. (2001). Clinical validity of the “mini-mental
informative. Another limitation was the fact that state” for Spanish speaking communities. Neuropsychologia,
AD patients were slightly less educated and older 39, 1150–1157.
Crawford, S., Whitnall, L., Robertson, J. and Evans, J. J.
than the control group. To reduce the effect of
(2012). A systematic review of the accuracy and clinical
this limitation, we estimated partial correlations, utility of the Addenbrooke’s cognitive examination and the
correcting for age and years of education as Addenbrooke’s cognitive examination-revised in the
confounding variables. diagnosis of dementia. International Journal of Geriatric
In conclusion, our results suggest that ACE- Psychiatry, 27, 659–669.
III is a useful tool for early diagnosis of AD and DeLong, E. R., DeLong, D. M. and Clarke-Pearson,
assessment of cognitive function, and they support D. L. (1988). Comparing the areas under two or more
using ACE-III as both a screening tool and a means correlated receiver operating characteristic curves: a
of describing cognitive profiles. nonparametric approach. Biometrics, 44, 837–844.
Elamin, M., Holloway, G., Bak, T. H. and Pal, S. (2015).
The utility of the Addenbrooke’s cognitive examination
version three in early-onset dementia. Dementia and
Geriatric Cognitive Disorders, 41, 9–15.
Conflict of interest Gorno-Tempini, M. L. et al. (2011). Classification of
primary progressive aphasia and its variants. Neurology, 76,
None. 1006–1114.
Hamilton, M. (1960). A rating scale for depression. Journal of
Neurology, Neurosurgery, and Psychiatry, 23, 56–62.
Hsieh, S. et al. (2015). The mini-Addenbrooke’s cognitive
examination: a new assessment tool for dementia. Dementia
Description of authors’ role and Geriatric Cognitive Disorders, 39, 1–11.
Jordi A. Matías-Guiu: Study concept and design, Hsieh, S., Schubert, S., Hoon, C., Mioshi, E. and
interpretation of data, statistical analysis, writing Hodges, J. R. (2013). Validation of the Addenbrooke’s
cognitive examination III in frontotemporal dementia and
the manuscript, final approval of the manu-
Alzheimer’s disease. Dementia and Geriatric Cognitive
script. Ana Cortés-Martínez: Acquisition of data, Disorders, 36, 242–250.
statistical analysis, writing of the manuscript, Jubb, M. and Evans, J. J. (2015). An investigation of the
final approval of the manuscript. María Valles- utility of the Addenbrooke’s cognitive examination III in
Salgado: Acquisition of data, literature search, the early detection of dementia in memory clinic patients
critical revision of the manuscript for important aged over 75 years. Dementia and Geriatric Cognitive
intellectual content, final approval of the ma- Disorders, 40, 222–232.
nuscript. Teresa Rognoni: Acquisition of data, Lam, B. et al. (2013). Criterion and convergent validity of
literature search, final approval of the manuscript. the montreal cognitive assessment with screening and
Marta Fernández-Matarrubia: Interpretation of standardized neuropsychological testing. Journal of the
data, literature search, final approval of the American Geriatrics Society, 61, 2181–2185.
Larner, A. and Mitchell, A. J. (2014). A meta-analysis of
manuscript. Teresa Moreno-Ramos: Acquisition
the accuracy of the Addenbrooke’s cognitive examination
of data, critical revision of the manuscript for (ACE) and the Addenbrooke’s cognitive
important intellectual content, final approval of examination-revised (ACE-R) in the detection of dementia.
the manuscript. Jorge Matías-Guiu: Study concept International Psychogeriatrics, 26, 555–563.
and design, literature search, acquisition of data, Leyton, C. E., Hornberger, M., Mioshi, E. and Hodges,
interpretation of data, study supervision, final J. R. (2010). Application of Addenbrooke’s cognitive
approval of the manuscript. examination to diagnosis and monitoring of progressive
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
ACE-III for mild cognitive impairment and dementia 9
primary aphasia. Dementia and Geriatric Cognitive Disorders, the National Institute on Aging-Alzheimer’s
29, 504–509. association workgroups on diagnostic guidelines for
Litvan, I. et al. (1996). Clinical research criteria for the Alzheimer’s disease. Alzheimer’s & Dementia, 7, 263–
diagnosis of progressive supranuclear palsy 269.
(Steele-Ricardson-Olszewski syndrome): report of the Menon, R., Lekha, V., Justus, S., Sarma, P. and
NINS-SPSP international workshop. Neurology, 47, 1–9. Mathuranath, P. (2014). A pilot study on utility of
Mathuranath, P. S., Nestor, P. J., Berrios, G. E., Malayalam version of Addenbrooke’s cognitive examination
Rakowicz, W. and Hodges, J. R. (2000). A brief in detection of amnestic mild cognitive impairment: a
cognitive test battery to differentiate Alzheimer’s disease critical insight into utility of learning and recall measures.
and frontotemporal dementia. Neurology, 55, Annals of Indian Academy of Neurology, 17, 420–425.
1613–1620. Morris, J. C. (1993). The clinical dementia rating (CDR):
Matias-Guiu, J. A. et al. (2014). Evaluation of the new current version and scoring rules. Neurology, 43,
consensus criteria for the diagnosis of primary progressive 2412–2414.
aphasia using fluorodeoxyglucose positron emission Pedro, M. C., Mercedes, M. P., Ramón, L. H. and Borja,
tomography. Dementia and Geriatric Cognitive Disorders, 38, M. R. (2016). Subjective memory complaints in elderly:
147–152. relationship with health status, multimorbidity,
Matías-Guiu, J. A. and Fernández-Bobadilla, R. (2014). medications, and use of services in a population-based
Validation of the Spanish-language version of study. International Psychogeriatrics. Epub ahead of print.
Mini-Addenbrooke’s cognitive examination as a dementia doi: 10.1017/S104161021600106X.
screening tool. Neurología. doi:10.1016/j.nrl.2014.10.005. Peña-Casanova, J. et al. (2009). Spanish multicenter
Matías-Guiu, J. A., Fernández-Bobadilla, R. and normative studies (NEURONORMA project): methods
Cortés-Martínez, A. (2016a). Addenbrooke’s Cognitive and sample characteristics. Archives of Clinical
Examination III: a neuropsychological test useful to screen Neuropsychology, 24, 307–319.
and obtain a cognitive profile. Neurología. Epub ahead of Pfeffer, R. I., Kurosaki, T. T., Harrah, C. H. Jr.,
print. doi: 10.1016/j.nrl.2016.06.014. Chance, J. M. and Filos, S. (1982). Measurement of
Matías-Guiu, J. A. et al. (2016b). Normative data for the functional activities in older adults in the community. The
Spanish version of the Addenbrooke’s cognitive Journal of Gerontology, 37, 323–329.
examination III. Dementia and Geriatric Cognitive Disorders, Pigliautile, M. et al. (2011). Validation study of the Italian
41, 243–250. Addenbrooke’s cognitive examination revised in a
Matías-Guiu, J. A. et al. (2015). Validation of the Spanish young-old and old-old population. Dementia and Geriatric
version of Addenbrooke’s cognitive examination III for Cognitive Disorders, 32, 301–307.
diagnosing dementia. Neurología, 30, 545–551. Rascovsky, K. et al. (2011). Sensitivity of revised diagnostic
McKeith, I. G. et al. (2005). Diagnosis and management of criteria for the behavioral variant of frontotemporal
dementia with Lewy bodies: third report of the DLB dementia. Brain, 134, 2456–2477.
consortium. Neurology, 65, 1863–1872. Sarazin, M. et al. (2007). Amnestic syndrome of the medial
McKhann, G. et al. (2011). The diagnosis of dementia temporal type identifies prodromal AD: a longitudinal
due to Alzheimer’s disease: recommendations from study. Neurology, 69, 1859–1867.
3676 :DD 53 4 697 9 5 7 ,: 7C7 2 7 CD . 9/ 9 0 3D C 4 75D D D:7 ,3 4 697 , 7 D7 C C7 3 3 34 7 3D
:DD 53 4 697 95 7 D7 C :DD 6H 6 9 1
You might also like
- Cognitive Screening Toolls For Identification of Dementia in Illiterature and Low - EducatedDocument33 pagesCognitive Screening Toolls For Identification of Dementia in Illiterature and Low - EducatedFlor BassoNo ratings yet
- Neuropsychological Rehabilitation: Principles and ApplicationsFrom EverandNeuropsychological Rehabilitation: Principles and ApplicationsJamuna RajeswaranRating: 5 out of 5 stars5/5 (1)
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author Manuscriptlaura4dapNo ratings yet
- An H Et Al, Large Intracranial Volume Accelerates Conversion To Dementia, 2016Document10 pagesAn H Et Al, Large Intracranial Volume Accelerates Conversion To Dementia, 2016henryfv2010No ratings yet
- JoernalDocument7 pagesJoernalyennaputriNo ratings yet
- Construct Validity of The Visual Cognitive Assessment Test (VCAT) - A Cross-Cultural Language-Neutral Cognitive Screening ToolDocument9 pagesConstruct Validity of The Visual Cognitive Assessment Test (VCAT) - A Cross-Cultural Language-Neutral Cognitive Screening ToolKAN NIMITPRASERTNo ratings yet
- Neuropsicologia Del MilenioDocument7 pagesNeuropsicologia Del MilenioJorge Gabriel Aguilar BrionesNo ratings yet
- Blen Now 2016Document7 pagesBlen Now 2016AmandaNo ratings yet
- Assessing-and-Diagnosing-Abnormality - 2Document6 pagesAssessing-and-Diagnosing-Abnormality - 2janeclou villasNo ratings yet
- SM 270309 BSXDocument10 pagesSM 270309 BSXCarolina MalheiroNo ratings yet
- A Comparative Review On Sleep Stage Classification MethodsDocument19 pagesA Comparative Review On Sleep Stage Classification MethodsVy Tô Nguyễn TườngNo ratings yet
- JNNP 2012 303926Document5 pagesJNNP 2012 303926Brew-sam ABNo ratings yet
- Evaluación PsiconeurológicaDocument11 pagesEvaluación PsiconeurológicaFormación Continua PoliestudiosNo ratings yet
- Attention and Executive Functions in Microsurgically Treated Patients After Subarachnoid HemorrhageDocument6 pagesAttention and Executive Functions in Microsurgically Treated Patients After Subarachnoid HemorrhageDURRAH FARARESANo ratings yet
- JsjsjjsjsDocument10 pagesJsjsjjsjsdavoklok123No ratings yet
- The e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsDocument10 pagesThe e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsFaiz KunNo ratings yet
- Beck's Depression ScaleDocument7 pagesBeck's Depression ScaleVitalia Putri PradanaNo ratings yet
- Assessment For Apraxia in Mild Cognitive Impairment and Alzheimer's DiseaseDocument6 pagesAssessment For Apraxia in Mild Cognitive Impairment and Alzheimer's DiseaseIvonne Ramon SuarezNo ratings yet
- Singh (2016) Neuropsychological Rehab of Patients With Traumatic Brain InjuryDocument19 pagesSingh (2016) Neuropsychological Rehab of Patients With Traumatic Brain InjuryInês CorreiaNo ratings yet
- 1 s2.0 S2173580819300173 MainDocument11 pages1 s2.0 S2173580819300173 MainIsayah Cuevas CoronelNo ratings yet
- Elderly Musicterapy Dementia PDFDocument11 pagesElderly Musicterapy Dementia PDFVictorvikkNo ratings yet
- Decisional Capacity To Consent To Treatment and Research in Patients Affected by Mild Cognitive Impairment A Systematic Review and Meta AnalysisDocument14 pagesDecisional Capacity To Consent To Treatment and Research in Patients Affected by Mild Cognitive Impairment A Systematic Review and Meta AnalysisJulio DelgadoNo ratings yet
- PGIMS ApprovedDocument8 pagesPGIMS ApprovedJes NongtduNo ratings yet
- Alzheimer S Dementia - 2022 - Kahali - COGNITO Computerized Assessment of Adult Information Processing NormativeDocument10 pagesAlzheimer S Dementia - 2022 - Kahali - COGNITO Computerized Assessment of Adult Information Processing Normativespurthi_16No ratings yet
- Neuroimagen y TartamudezDocument40 pagesNeuroimagen y TartamudezSofia Zuñiga RamosNo ratings yet
- The Brief Assessment of Cognition in Schizophrenia. Normative Data For The Italian PopulationDocument9 pagesThe Brief Assessment of Cognition in Schizophrenia. Normative Data For The Italian PopulationMAGALYNo ratings yet
- Chilean Version of The INECO Frontal Screening (IFS-Ch) - Psychometric Properties and Diagnostic AccuDocument9 pagesChilean Version of The INECO Frontal Screening (IFS-Ch) - Psychometric Properties and Diagnostic AccuValentina VillarroelNo ratings yet
- Effectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Document2 pagesEffectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Zalinah Mohd YusofNo ratings yet
- Eye Tracking Metrics To Screen and Assess Cognitive Impairment in Patients With Neurological DisordersDocument8 pagesEye Tracking Metrics To Screen and Assess Cognitive Impairment in Patients With Neurological DisordersSyed Abdul Qadir GilaniNo ratings yet
- Neuropsychological Assessment Dementia: State of The Art: BRHNG, JohansodDocument5 pagesNeuropsychological Assessment Dementia: State of The Art: BRHNG, JohansodJose Alonso Aguilar ValeraNo ratings yet
- A Systematic Review of Sensory-Based Autism PDFDocument13 pagesA Systematic Review of Sensory-Based Autism PDFMH AmoueiNo ratings yet
- Neurobiology of AgingDocument5 pagesNeurobiology of AgingcoconitaNo ratings yet
- Arbula 2020Document7 pagesArbula 2020Fabíola ManoNo ratings yet
- BaixadosDocument14 pagesBaixadosLanna RegoNo ratings yet
- Beaunieux 2011Document12 pagesBeaunieux 2011Jose Alonso Aguilar ValeraNo ratings yet
- 1 s2.0 S187620181300004XDocument6 pages1 s2.0 S187620181300004Xfunny guyNo ratings yet
- Using Temporal Orientation, Category Uency, and Word Recall For Detecting Cognitive Impairment: The 10-Point Cognitive Screener (10-CS)Document10 pagesUsing Temporal Orientation, Category Uency, and Word Recall For Detecting Cognitive Impairment: The 10-Point Cognitive Screener (10-CS)Camila VelosoNo ratings yet
- Analysis of Central Mechanism of Cognitive Training On Cognitive Impairment After Stroke: Resting-State Functional Magnetic Resonance Imaging StudyDocument10 pagesAnalysis of Central Mechanism of Cognitive Training On Cognitive Impairment After Stroke: Resting-State Functional Magnetic Resonance Imaging StudyLara Perez MurciaNo ratings yet
- Guia Demencia DCLDocument10 pagesGuia Demencia DCLmaricellap31No ratings yet
- Acw 018Document11 pagesAcw 018otakualafugaNo ratings yet
- EEG Based EmotionsDocument19 pagesEEG Based EmotionsAna Rita SerraNo ratings yet
- Neuropsychological Abnormalities in A Patient Diagnosed With Frontoparietal MeningiomaDocument4 pagesNeuropsychological Abnormalities in A Patient Diagnosed With Frontoparietal MeningiomaJhoan CaicedoNo ratings yet
- Artigo Arvore de DecisaoDocument10 pagesArtigo Arvore de DecisaoMayara MiyaharaNo ratings yet
- Neuropsych LogyDocument13 pagesNeuropsych LogyJulian Lloyd D. GasparNo ratings yet
- Neuropsychological AssessmentDocument10 pagesNeuropsychological AssessmentVanessa PalomaNo ratings yet
- 7 Luijtelaar11Document27 pages7 Luijtelaar11Fariz SyafiruddinNo ratings yet
- Working Memory RehabilitationDocument7 pagesWorking Memory RehabilitationKaterina ChatzNo ratings yet
- Granholm 2004Document6 pagesGranholm 2004Rob KorényiNo ratings yet
- Cognitive Remediation For Brain Injury and - Marvin H PoddDocument173 pagesCognitive Remediation For Brain Injury and - Marvin H PoddGheorghe Șarcani100% (1)
- Neuropsychological Assessment in Children: Jornal de PediatriaDocument6 pagesNeuropsychological Assessment in Children: Jornal de PediatriaBenja MoranNo ratings yet
- Cognitive Training in AutismDocument23 pagesCognitive Training in AutismdepisapiNo ratings yet
- Geriatric NursingDocument7 pagesGeriatric NursingHumberto HumbertoNo ratings yet
- CERAD Test Performances in Amnestic Mild Cognitive Impairment and Alzheimer's DiseaseDocument9 pagesCERAD Test Performances in Amnestic Mild Cognitive Impairment and Alzheimer's DiseaseConsultorio Psicológico YumboNo ratings yet
- Brain Imaging Genetics in ADHDDocument41 pagesBrain Imaging Genetics in ADHDEsmeraldaNo ratings yet
- Alz Dem Diag Ass Dis Mo - 2020 - Allegri - Prognostic Value of ATN Alzheimer Biomarkers 60 Month Follow Up ResultsDocument8 pagesAlz Dem Diag Ass Dis Mo - 2020 - Allegri - Prognostic Value of ATN Alzheimer Biomarkers 60 Month Follow Up Resultsk6fqcwfczfNo ratings yet
- Brain Disorders & Therapy: Are Mental Disorders Brain Diseases and What Does This Mean?Document5 pagesBrain Disorders & Therapy: Are Mental Disorders Brain Diseases and What Does This Mean?CharpapathNo ratings yet
- Neuronorma ViejosDocument11 pagesNeuronorma ViejosDavidNo ratings yet
- Collins Et Al., (2020) - A-Systematic-Review-Of-The-Prevalence-Of-Depression-Anxiety-And-Apathy-In-Frontotemporal-Dementia-Atypical-And-Young-Onset-Alzheimers-Disease-And-Inherited-DementiaDocument20 pagesCollins Et Al., (2020) - A-Systematic-Review-Of-The-Prevalence-Of-Depression-Anxiety-And-Apathy-In-Frontotemporal-Dementia-Atypical-And-Young-Onset-Alzheimers-Disease-And-Inherited-DementiaRealidades InfinitasNo ratings yet
- Psychometric Properties of The Spanish Version of The Clinical Outcomes in Routine Evaluation - Outcome MeasureDocument10 pagesPsychometric Properties of The Spanish Version of The Clinical Outcomes in Routine Evaluation - Outcome MeasureSilvana AcostaNo ratings yet
- 2008 Kolb & Kolb-Armstrong-Ch03 Handbook MLE&D PROOFSDocument28 pages2008 Kolb & Kolb-Armstrong-Ch03 Handbook MLE&D PROOFSERick SOnNo ratings yet
- Direct Method SummaryDocument2 pagesDirect Method SummaryMohammad naser KintozNo ratings yet
- Learning How To Learn: Implications For Non Traditional Adult StudentsDocument8 pagesLearning How To Learn: Implications For Non Traditional Adult StudentsurielNo ratings yet
- Models of Decision MakingDocument22 pagesModels of Decision MakingMohid AhmadNo ratings yet
- Analysis of High School Students Critical Thinking Ability To Solve Social Science ProblemsDocument13 pagesAnalysis of High School Students Critical Thinking Ability To Solve Social Science ProblemsGlobal Research and Development ServicesNo ratings yet
- Lesson Plan AdjectiveDocument7 pagesLesson Plan AdjectiveRoganda SiraitNo ratings yet
- DLL MAPEH 3rd-Quarter Week-2Document10 pagesDLL MAPEH 3rd-Quarter Week-2Clarissa Flores Madlao MendozaNo ratings yet
- Eng111-Purposive-Communication-Adapted CoursepackDocument150 pagesEng111-Purposive-Communication-Adapted CoursepackDensio100% (2)
- Unit 5 - I Am Special - Year 2 Listening and Speaking (Mixed Abilities)Document7 pagesUnit 5 - I Am Special - Year 2 Listening and Speaking (Mixed Abilities)Nur Syaheela Binti ZamriNo ratings yet
- DLP DRAFT FORMAT (Editable)Document7 pagesDLP DRAFT FORMAT (Editable)Velarde, Claire R.No ratings yet
- THE CAUSALITY O-WPS OfficeDocument56 pagesTHE CAUSALITY O-WPS Officenasser aplalNo ratings yet
- Activity 3 Light and ColourDocument4 pagesActivity 3 Light and Colourapi-545623990No ratings yet
- Topic 1 Problem Solving WAJ3105Document29 pagesTopic 1 Problem Solving WAJ3105Dzulkifli SulaimanNo ratings yet
- A COURSE MODULE in Eng322 Module 1 Lesson 2aDocument9 pagesA COURSE MODULE in Eng322 Module 1 Lesson 2aerickson hernanNo ratings yet
- Lesson Plan Functions of CommunicationDocument3 pagesLesson Plan Functions of CommunicationMarnie Godienes100% (2)
- Presentation On Reading SkillsDocument43 pagesPresentation On Reading SkillsSehar KhanNo ratings yet
- Developmental and Social FactorsDocument19 pagesDevelopmental and Social FactorsMercy AbaretaNo ratings yet
- Rubrics For Concept MapDocument1 pageRubrics For Concept MapEmyren ApuyaNo ratings yet
- Stephen Krashen's Theory of Second Language AcquisitionDocument16 pagesStephen Krashen's Theory of Second Language AcquisitionBelenVettese100% (5)
- Psycholinguistic Models of Speech Production in Bilingualism and MultilingualismDocument22 pagesPsycholinguistic Models of Speech Production in Bilingualism and Multilingualismkhadidja BOUTOUILNo ratings yet
- Table FinkDocument2 pagesTable FinkNadin NomanNo ratings yet
- ConclusionDocument4 pagesConclusionapi-284384069No ratings yet
- Mindset Questionnaire, TECDocument6 pagesMindset Questionnaire, TECRiya RaneNo ratings yet
- Focus: The Hidden Driver of ExcellenceDocument9 pagesFocus: The Hidden Driver of ExcellencelectavaresNo ratings yet
- Aptitude TestDocument12 pagesAptitude Testsushila napitNo ratings yet
- Commentary For Lesson PlanDocument2 pagesCommentary For Lesson PlanHariz SaveGaza100% (2)
- Lessons Discussed in The Personality Development Subject) : The Issues (Communication Breakdown)Document5 pagesLessons Discussed in The Personality Development Subject) : The Issues (Communication Breakdown)Arianne SagumNo ratings yet
- Basketball Student Teacher EvaluationDocument2 pagesBasketball Student Teacher Evaluationapi-302941656No ratings yet
- Lesson Reflection 3Document3 pagesLesson Reflection 3Fatima ObaidNo ratings yet
- Language-Learner Computer Interactions: Theory, Methodology and CALL ApplicationsDocument275 pagesLanguage-Learner Computer Interactions: Theory, Methodology and CALL ApplicationsAndrea EscalanteNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (26)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (516)