Professional Documents
Culture Documents
Becker
Uploaded by
Gunther MirandaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Becker
Uploaded by
Gunther MirandaCopyright:
Available Formats
Ultrasound Obstet Gynecol 2001; 17: 496 – 501
The relevance of placental location at 20–23 gestational
BlackwellArticle
Original Science, Ltd
weeks for prediction of placenta previa at delivery:
evaluation of 8650 cases
R. H. BECKER, R. VONK, B. C. MENDE, V. RAGOSCH and M. ENTEZAMI
Free University of Berlin, University Hospital Benjamin Franklin, Department of Obstetrics and Gynecology, Berlin, Germany
K E Y W O R D S: Placenta previa, Prenatal diagnosis, Second trimester, Ultrasound
ABSTRACT INTRODUCTION
Objective To determine the correlation between placental Placenta previa is a rare but dangerous, sometimes fatal, con-
position at 20–23 weeks and incidence of birth complications dition: it increases maternal, fetal and neonatal morbidity
caused by placental position. and mortality1–3. During pregnancy, placenta previa is one of
Subjects and methods In an ongoing prospective study, the leading causes of third-trimester bleeding4. At delivery,
placental position was determined by transabdominal sono- women with placenta previa have an increased risk of abruptio
graphy as part of anomaly scanning at 20 –23 gestational placentae, Cesarean delivery, fetal malpresentation and post-
weeks, followed by transvaginal sonography in uncertain or partum hemorrhage5. In the United States between 1979 and
suspicious situations. Examination was performed in 9532 1986, 44 maternal deaths were related to placenta previa as an
cases; feedback was obtained from 8650 patients (90.7%). underlying disease, mainly because of bleeding and dissem-
inated intravascular coagulation5.
Results Transabdominal sonography was followed by To prevent severe complications, the accurate and timely
transvaginal scan in 363 of 8650 cases (4.2%). In 8551 cases diagnosis of placenta previa is indispensable. Unfortunately,
(98.9%), we found normal placental position, with the location of placental position produces a diagnostic dilemma:
placenta not reaching the internal os and a Cesarean section on one hand it would be advantageous to be informed about
rate of 17.1% (1458/8551). The incidence of ‘low placental a dangerous placental position as early as possible; on the
position’, with the placenta reaching the internal os was other hand, it is well known that the incidence of so called
0.66% (57/8650), with a Cesarean section rate of 21% (12/ placenta previa decreases with advancing gestational age,
57). In 0.49% (42/8650) of cases, the placenta overlapped especially during the second trimester. Many cases of placenta
the internal os at 20 –23 weeks; Cesarean section because of previa diagnosed during the early second trimester have an
placenta previa or bleeding was performed in 28 of 8650 outcome of normal delivery6. Therefore too early assessment
cases (0.32%). Vaginal delivery was possible in 43% of cases of placental position results in unnecessary patient anxiety7,8.
(13/30), when the overlap did not exceed 25 mm. If the Our aim was to determine the accuracy of placental location
overlap exceeded 25 mm (12 cases), no vaginal delivery was at a 20–23-week anomaly scan in predicting complications
reported. There was no reported case of placenta previa related to placental position at delivery.
missed at the 20–23-week scan.
Conclusion At 20 –23 weeks, a combination of routine
SUBJECTS AND METHODS
transabdominal and indication-based transvaginal loca-
tion of placental position is a powerful tool in predicting In an ongoing prospective study beginning in September
placenta previa at delivery. The advantage of determining 1992, the position of the placenta was registered in 9532 non-
placental position at this stage of pregnancy is a low false- selected consecutive patients undergoing anomaly scanning
positive rate compared to at earlier stages of pregnancy. We at 20–23 gestational weeks in our institution, which serves
conclude that an overlapping placenta at 20 –23 weeks has as one of the referral centers of Berlin. We received feed-
the consequence of a high probability of placenta previa at back concerning the outcome of pregnancies in 8650 cases
delivery. An overlap of 25 mm or more at 20 –23 weeks (91.9%); evaluation was done for these 8650 patients only.
seems to be incompatible with later vaginal delivery. The study group included 255 sets of twins, 19 sets of triplets
Correspondence: Dr R. Becker, Free University of Berlin, University Klinikum Benjamin Franklin, Kurfürstendamm 199, 10719 Berlin, Germany
(e-mail: bedaktari@t-online.de)
Received 8-3-00, Revised 14-12-00, Accepted 9-3-01
496 O RIGIN AL PAPER
Placenta previa Becker et al.
and 1 set of quadruplets. Each multiple pregnancy was located by abdominal scan with a normally filled bladder,
counted as one case. We included only pregnancies with a followed by transvaginal scan in uncertain or suspicious sit-
duration of more than 24 weeks; pregnancies terminated uations (n = 363, 4.2%). For evaluation, observations were
because of malformations were excluded from evaluation. divided into three groups:
Most of the patients were delivered in one of the several Group I: ‘normal’ position of placenta: the lower margin
hospitals of the city or the surrounding area. Feedback of of the placenta did not reach the internal os;
information concerning details of delivery including com- Group II: ‘low position’ of placenta: the lower margin of
plications was achieved by return of a form handed out to the the placenta reached the internal cervical os but did not
patient after examination; if omitted, information was overlap (Figure 1);
obtained by telephone contact in most cases with the patient. Group III: ‘overlapping placenta’: the lower margin of the
In 1998 and 1999, this was performed in 958 of 2333 cases placenta overlapped the internal os (Figure 2).
(41%); we therefore estimate the rate of spontaneous return When an overlapping placenta was suspected, the patient
of information in our whole study group to be around 50%. and her physician were informed, and follow up was recom-
The mean age of the patients was 31.1 (15 –46) years. The mended at 28 weeks. Calculations were performed using SAS
mean gestational age was 21.6 weeks. Examinations were (SAS, Heidelberg, Germany). Exact Clopper–Pearson confidence
performed with an Acuson 128 XP10 (Mountain View, CA, intervals were used for the proportions.
USA) ultrasound machine. Transabdominal scans were per-
formed with 4- and 5-MHz probes and transvaginal scans
RESULTS
with 7- or 8.5-MHz probes. Experience of the participating
physicians at the beginning of the study was more than The frequency of different classes of placental position is
2 years of exclusive sonographic work. The placenta was listed in Table 1. The correlation of gestational age and fre-
quency of ‘low’ or ‘overlapping’ placenta is presented in
Table 2. An overview of the frequency of Cesarean sections
in correlation to position of placenta at 20–23 weeks is
shown in Table 3. The frequency of Cesarean section in the
whole study group was 17.3% (1499/8650). Patients with
‘normal placental position’ (Group I) were delivered by
Cesarean section with a frequency of 17.1% (1458/8551). In
‘low position’ (Group II), the frequency was 21% (12/57);
this frequency was not statistically different from that of Group
I (P = 0.38, Fisher’s exact test). In 42 patients we found a
placenta overlapping the internal os containing one set of
twins (Group III). We had occasion to perform follow-up
examinations in 22 of these cases. In six of 22 cases, placental
position had normalized in later phases of pregnancy, all of
Table 1 Placental position at 20–23 weeks
Figure 1 Low position of placenta of uterine anterior wall, visualized by
transvaginal sonography with an 8.5-MHz probe. P, placenta; FH, fetal Placental position n (%) 95% confidence interval
head, large arrow, internal cervical os; small arrows, cervical channel.
‘Normal’ (Group I) 8551 (98.90) 98.61–99.07%
‘Low’ (Group II) 57 (0.66) 0.50–0.85%
‘Overlapping’ (Group III) 42 (0.49) 0.35–0.66%
> 0–10 mm 14 (0.16) 0.09–0.27%
11–24 mm 16 (0.19) 0.11–0.30%
≥ 25 mm 12 (0.14) 0.07–0.24%
Percentages are based upon the total population (n = 8650).
Table 2 Gestational age and placental extension
Placenta extended to or over
the internal cervical os
Gestational age
(weeks) n n Proportion (%)
20 + 0 to 20 + 6 661 11 1.66
21 + 0 to 21 + 6 3613 44 1.22
Figure 2 Placenta overlapping the internal cervical os by 16.6 mm, 22 + 0 to 22 + 6 3381 35 1.04
visualized by transvaginal sonography at 21 + 1 weeks with a 7-MHz 23 + 0 to 23 + 6 995 9 0.90
probe. P, placenta; large arrow, internal cervical os; small arrows, Overall 8650 99 1.14
cervical channel.
Ultrasound in Obstetrics and Gynecology 497
Placenta previa Becker et al.
them with an overlap less than 25 mm; 5 of these were delivered There was neither fetal nor maternal death in Group III.
vaginally; one was by Cesarean section because of malpres- One patient with a history of Cesarean section and an overlap
entation. The patient with the greatest amount of overlap and of posterior wall placenta of more than 50 mm experienced
normal delivery had an overlap of 20 mm. The frequency of massive hemorrhage during Cesarean section at 39 weeks
Cesarean section was 69% (29/42) including the one case of and underwent hysterectomy because of placenta increta. In
Cesarean section because of malpresentation (overlap 10 mm another patient, using color Doppler sonography we detected
at 22 + 6 weeks; no overlap at 26 + 6 weeks). In all other overlapping placenta in combination with velamentous inser-
cases, Cesarean section was performed because of placenta tion with an arterial umbilical vessel on the surface of the
previa according to the decision of the responsible physician, overlapping part of the placenta (Figures 4 and 5); she under-
nine of them because of vaginal bleeding between 31 and 39 went emergency Cesarean section following vaginal bleeding
gestational weeks. All patients with an overlap of 25 mm or at home at 32 + 4 weeks. One patient presented with a vas
more delivered by Cesarean section. In patients with pla- previum detected at 23 + 0 gestational weeks (Figure 6); she
centa overlapping less than 25 mm (n = 30), the frequency was admitted to hospital at 30 weeks and delivered by emer-
of Cesarean section because of placenta previa in the sub- gency Cesarean section following vaginal bleeding at 32 + 5
group of 1–10 mm overlap was 43% (6/14) compared to gestational weeks. In all cases, outcome for mother and child
62.5% (10/16) in the subgroup of 11–24 mm (P = 0.46, was favorable and all of the pregnancies of this group had a
Fisher’s exact test). The correlation between degree of duration of at least 31 weeks (Table 4).
placental overlap and sensitivity for Cesarean section
because of placenta previa in Group III (28/42, 67%) is
DISCUSSION
shown in Figure 3. An overview of the duration of pregnancies
in the three groups of different placental position is given in Placenta previa at delivery is a rare condition. Frequencies
Table 4. reported at birth range from 0.14%9 to 0.75%10 with a mean
of 0.38%1,5,8–16. An overview of frequencies of placenta pre-
Table 3 Cesarean section in relation to placental position at 20– via is given in Table 5. In our study group, the incidence of
23 weeks placenta previa at delivery with the consequence of Cesarean
section was 0.32% (28/8650; 95% confidence interval
95% confidence11
Placental position n (%) interval (%)
Table 4 Duration of pregnancy in relation to placental position at 20–
‘Normal’ (Group I) 1458/8551 (17.10) (16.26 –17.87) 23 weeks
‘Low’ (Group II) 12/57 (21.05) (11.38 –33.89)
‘Overlapping’ (Group III) *29/42 (69.05) (52.91–82.39) Duration of pregnancy (weeks)
> 0 –10 mm *7/14 (50.00) (23.04 –76.96)
11–24 mm 10/16 (62.50) (35.44 –84.80) Placental position n Median Range
≥ 25 mm 12/12 (100.00) (73.54 –100.00)
Overall 1499/8650 (17.33) (16.54 –18.14) ‘Normal’ (Group I) 8551 39.0 24–43
‘Low’ (Group II) 57 39.0 32–42
Percentages are based on the total number of patients in the group. ‘Overlapping’ (Group III) 42 38.0 31–41
*Includes one case of Cesarean section because of fetal malpresentation Overall 8650 39.0 24–43
with overlapping placenta at 22 weeks and normal placental position at
control sonography.
Figure 4 Placenta overlapping the internal os at 25 + 6 gestational weeks
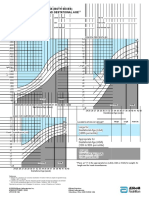
Figure 3 Receiver operating characteristic (ROC) curve for Cesarean visualized by transabdominal scan, with a 4-MHz probe. Overlap was
section due to persistence of placenta previa depending upon the degree detected at 20 + 6 gestational weeks, with an arterial vas previum
of overlap over the internal os in group III. (Group III consisted of 42 (umbilical artery) on the surface of the overlapping part of the placenta
patients; 28 of these had a Cesarean section because of placenta previa.) continuing as insertio velamentosa. X, insertion of the umbilical cord at
Area under curve (overlap) is 0.786 (standard error, 0.069). The dashed the ventral uterine wall; large arrow, internal cervical os; small arrows,
line represents: Sensitivity = 1 – Specificity. cervical channel.
498 Ultrasound in Obstetrics and Gynecology
Placenta previa Becker et al.
ranges, 0.22–0.47%) which lies close below the mean of pub- by the patients according to the information they had received
lished data. The differences of incidence in different study from their physicians in charge. In our opinion this seemed
groups may be due to the higher amount of high-risk preg- to be sufficiently reliable but may bear a small risk of incorrect
nancies in patients of referral hospitals as well as racial and information. With an incidence of 0.32% in our study group
genetic differences. Also, factors like confusing abruption with and 0.38% as the mean of incidence of more than 500 000
placenta previa, quality of outcome information or size of patients (Table 5) our assessment of placenta previa most prob-
study group may be of importance. ably does not include a large amount of incorrect information.
A crucial point in evaluation is the verification of placenta During pregnancy, the frequency of so-called ‘placenta
previa at delivery. In our study group, this was performed by previa’ decreases with increasing gestational age due to an
the responsible physician in the different hospitals of the city. effect described as ‘placental migration’17, caused by the fact
In nine cases, patients were delivered by Cesarean section in that the placenta-free uterine wall grows faster than the placenta-
acute clinical situations of bleeding following the diagnosis of covered area11. This effect was observed in our study group
placenta previa by previous sonograms. In one case, Cesar- with the frequency of ‘low’ or ‘overlapping’ placenta decreasing
ean section was performed because of malpresentation of the from 1.66% at week 20 to 0.90% at week 23 (Table 2).
fetus in a situation where ‘overlapping’ placenta had normal- The consequence of this effect is a higher amount of false-
ized; this case was counted as non-persistence. In 19 cases of positive cases of diagnosis of ‘placenta previa’ in earlier
Cesarean section following overlapping placenta at the 20– phases of pregnancy.
23-week scan, the information of a Cesarean section having An overview of the reported incidence and regression rate
been carried out because of placenta previa was given to us of so-called ‘placenta previa’ is given in Table 6. Incidence
at the time of scan decreased from 2.4% at 12–16 weeks11
to 0.48% at 20–23 weeks, depending on the definition of
‘placenta previa’. Parallel to this effect, the persistence rate
of ‘placenta previa’ until delivery increased from 6.4% at
12–16 weeks11 to 67% at 20–23 weeks.
Before introduction of transvaginal sonography, diagnosis
of placenta previa was difficult and had to rely on indirect
signs16. Since the introduction of transvaginal sonography,
this method has become the gold standard for the diagnosis
of placenta previa in all phases of pregnancy18,19. Performed
accurately, it seems to pose no threat to the pregnancy18–21.
In our study group, one patient with an overlap of 16 mm
reported bleeding in the evening after vaginal examination.
This was possibly due to abruption of the overlapping part
of the placenta following contractions induced by trans-
vaginal sonography; after 8 days in hospital, her pregnancy
Figure 5 Transvaginal sonography (7-MHz probe) of the same situation went on to 40 weeks and ended in a spontaneous delivery.
as in Figure 4 (In Figure 4, fetal head moved to lateral part of amniotic It is still unclear whether accurate diagnosis of placenta
cavity.) with pulsed Doppler of the vas praevium. P, placenta; FH, fetal previa is possible only by routine application of transvaginal
head; large arrow, internal cervical os; small arrows, cervical channel.
sonography9,11. Our experience with the use of transvaginal
sonography only in uncertain or suspicious situations, which
Table 5 Incidence of placenta previa at delivery
Incidence
Time span Study group (n) n %
Taipale et al. 19989 1995–96 3696 5 0.14
Taipale et al. 199711 1993–94 6428 10 0.16
Lauria et al. 199612 > 2910 5 0.17
Taylor et al. 199413 1984–87 278 933 917 0.33
Crane et al. 19991 1988–95 92 983 305 0.33
McClure and 0.47
Dornan 19908 1986 1490 7
Iyasu et al. 19935 1979–86 0.48
Frederiksen et al. 199914 1976–97 93 384 514 0.55
Figure 6 Vasa praevia at 23 + 0 gestational weeks visualized by Williams et al. 199115 1977–80 12 420 69 0.56
transvaginal scan with an 8.5-MHz probe: low position of placenta of Rizos et al. 197916 1972–77 1098 6 0.58
uterine anterior wall with the umbilical cord overlapping the internal os Sherman et al. 199210 1990 8410 63 0.75
and continuing on the posterior wall as insertio velamentosa. P, placenta; All 501 752 1901 0.38
FH, fetal head; arrows, cervical channel.
Ultrasound in Obstetrics and Gynecology 499
Placenta previa Becker et al.
Table 6 Incidence of placenta previa at ultrasound, persistence until delivery and incidence at birth
GA at US Incidence at US Persistence Incidence at birth
n (weeks) P.p. def US type (n (%)) (n (%)) (n (%))
Taipale et al. 199711 6428 12 –16 > 14 mm TV 156/6428 (2.4) 10/156 (6.4) 10/6428 (0.16)
Lauria et al. 199612 > 2910 15–20 ≥ 0 mm TA + TV 31/2910 (1.1) 5/36 (14) 5/ > 2910 (< 0.17)
Rizos et al. 197916 1098 16 –18 > 0 mm TA 58/1098 (5.3) 5/52 (10) 5/1098 (0.46)
Taipale et al. 19989 3696 18–23 > 0 mm TV 57/3969 (1.5) 5/57 (8.8) 5/3696 (0.14)
> 15 mm 27/3969 (0.68) 5/27 (18.5) 5/3696 (0.14)
≥ 25 mm 10/3696 (0.27) 4/10 (40) 4/3696 (0.11)
Present study 8650 20 –23 > 0 mm TA + TV 42/8650 (0.48) *28/42 (67.0) *28/8650 (0.32)
≥ 25 mm 12/8650 (0.14) 12/12 (100) 12/8650 (0.14)
*Excluding one case of Cesarean section because of fetal malpresentation with overlapping placenta at 22 weeks and normal placental position at
control sonography. GA, gestational age; US, ultrasound; P.p. def, definition of placenta previa (degree of overlap over internal os); TA,
transabdominal scan; TV, transvaginal scan.
occurred in 4.2% of cases and to our knowledge missed no
REFERENCES
diagnosis of placenta previa at delivery, confirms reports12,22
which demonstrate that transabdominal ultrasound is satis- 1 Crane JMG, Van Den Hof MC, Dodds L, Armson A, Liston R.
factory for screening for placenta previa. Neonatal outcomes with placenta previa. Obstet Gynecol 1999; 93:
541–4
Another topic of discussion is the question: what is the cut-
2 Gorodeski IG, Bahari CM. The effect of placenta previa localization
off point of placental overlapping of the internal cervical os upon maternal and fetal-neonatal outcome. J Perinat Med 1987; 15:
for predicting placenta previa with a specificity of 100%? 167–77
Regarding the natural history of the condition, it seems likely 3 Jouppila P. Vaginal bleeding in the last two trimesters of pregnancy:
that the dimension at which spontaneous regression is pos- a clinical and ultrasonic study. Acta Obstet Gynecol Scand 1979; 58:
461–7
sible varies with gestational age. An overlap of 25 mm or
4 McShane PM, Heyl PS, Epstein MF. Maternal and perinatal
more had a persistence rate of placenta previa to term of 40% morbidity resulting from placenta previa. Obstet Gynecol 1985;
in a study group performing ultrasound at 18 –23 weeks9. In 65: 176–82
our group with a further advanced period of assessment of 5 Iyasu S, Saftlas AK, Rowley DL, Koonin LM, Lawson HW, Atrash HK.
20–23 weeks, all 12 patients with an overlap of 25 mm or The epidemiology of placenta previa in the United States, 1979 through
1987. Am J Obstet Gynecol 1993; 168: 1424–9
more delivered by Cesarean section, indicating that an over-
6 Wexler P, Gottesfeld KR. Second trimester placenta previa. An
lap of 25 mm or more might be incompatible with the chance apparently normal placentation. Obstet Gynecol 1977; 50: 706–9
of regression if assessed at this time of pregnancy. 7 Andersen ES, Steinke NMS. The clinical significance of asymptomatic
As a consequence of these data, it seems justified to inform mid-trimester low placentation diagnosed by ultrasound. Acta
patients in these situations about their prognosis as follows: Obstet Gynecol Scand 1988; 67: 339–41
8 McClure N, Dornan JC. Early identification of placenta previa.
• In the case of ‘low’ placental position, there is a probability
Br J Obstet Gynaecol 1990; 97: 959–61
of Cesarean section similar to that of ‘normal’ placental 9 Taipale P, Hiilesmaa V, Ylöstalo P. Transvaginal ultrasonography at
position. 18–23 weeks in predicting placenta previa at delivery. Ultrasound
• In the case of ‘overlapping’ placenta, Obstet Gynecol 1998; 12: 422–5
with an overlap of up to 20 mm there is a high probability of 10 Sherman SJ, Carlson DE, Platt LD, Medearis AL. Transvaginal ultra-
sound: does it help in the diagnosis of placenta previa? Ultrasound
placental-position-originated complications at delivery, with
Obstet Gynecol 1992; 2: 256–60
a chance of spontaneous regression; follow-up sonography 11 Taipale P, Hiilesmaa V, Ylöstalo P. Diagnosis of placenta previa by
should be performed; transvaginal sonographic screening at 12–16 weeks in a nonselected
with an overlap of 25 mm or more there is a very high probabil- population. Obstet Gynecol 1997; 89: 364–7
ity of the necessity of Cesarean section, with a very low chance 12 Lauria MR, Smith RS, Treadwell MC, Comstock CH, Kirk JS, Lee W,
Bottoms SF. The use of second-trimester transvaginal sonography
of regression.
to predict placenta previa. Ultrasound Obstet Gynecol 1996; 8:
Our experience with placental localization at 20 –23 weeks 337–40
shows that this phase of pregnancy is late enough to reduce 13 Taylor VM, Kramer MD, Vaughan TL, Peacock S. Placenta previa
to a minimum the frequency of false-positive cases of predic- and prior Cesarean delivery: how strong is the association? Obstet
tion of placenta previa at birth. With an incidence in our Gynecol 1994; 84: 55–7
14 Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: a 22-year
group of 0.32% of placenta previa at birth, it seems unlikely
analysis. Am J Obstet Gynecol 1999; 180: 1432–7
that we lacked reports of considerable numbers of placenta 15 Williams MA, Mittendorf R, Lieberman E, Monson RR, Schoenbaum SC,
previa because of incomplete feedback from the patients; Genest DR. Cigarette smoking during pregnancy in relation to placenta
thus the sensitivity at this stage of pregnancy seems to be high previa. Am J Obstet Gynecol 1991; 165: 28–32
using a combination of routine transabdominal and indic- 16 Rizos N, Doran TA, Miskin M, Benzie RJ, Ford JA. Natural history
of placenta previa ascertained by diagnostic ultrasound. Am J Obstet
ated transvaginal sonography. Furthermore, in Group III,
Gynecol 1979; 133: 287–91
there was neither fetal nor maternal death: at this phase of 17 Townsend RR, Laing FC, Nyberg DA, Brooke Jeffrey R, Wing VW.
pregnancy it is not yet too late to prevent severe complications Technical factors responsible for ‘placental migration’: sonographic
of pregnancy by adequately counseling the pregnant women. assessment. Radiology 1986; 160: 105–8
500 Ultrasound in Obstetrics and Gynecology
Placenta previa Becker et al.
18 Farine D, Fox HE, Jakobson S, Timor-Tritsch IE. Vaginal ultrasound for 21 Leerentveld RA, Gilberts ECAM, Arnold MJCW, Wladimiroff JW.
diagnosis of placenta previa. Am J Obstet Gynecol 1988; 159: 566–9 Accuracy and safety of transvaginal sonographic placental localization.
19 Farine D, Fox HE, Jakobson S, Timor-Tritsch IE. Is it really a Obstet Gynecol 1990; 76: 759–62
placenta previa? Eur J Obstet Gynecol Reprod Biol 1989; 31: 103–8 22 Smith RS, Lauria MR, Comstock CH, Treadwell MC, Kirk JS, Lee W,
20 Timor-Tritsch IE, Yunis RA. Confirming the safety of transvaginal Bottoms SF. Transvaginal ultrasonography for all placentas that
sonography in patients suspected of placenta previa. Obstet Gynecol appear to be low-lying or over the internal cervical os. Ultrasound
1993; 81: 742 – 4 Obstet Gynecol 1997; 9: 22–4
Ultrasound in Obstetrics and Gynecology 501
You might also like
- Plprevia PDFDocument3 pagesPlprevia PDFAtikah RahmadhaniNo ratings yet
- Screening For Placenta Accreta at 11-14 Weeks of GestationDocument6 pagesScreening For Placenta Accreta at 11-14 Weeks of Gestationjuljim01No ratings yet
- VASA Previa CaseDocument3 pagesVASA Previa CasewijeNo ratings yet
- Natural History of Vasa Previa Across Gestation Using A Screening ProtocolDocument7 pagesNatural History of Vasa Previa Across Gestation Using A Screening ProtocolwijeNo ratings yet
- Grayscale USG of Placenta AccretaDocument5 pagesGrayscale USG of Placenta AccretaDara Mayang SariNo ratings yet
- Good18.Prenatally Diagnosed Vasa Previa A.30Document9 pagesGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Indications and Risks of Vacuum Assisted Deliveries.: OriginalDocument2 pagesIndications and Risks of Vacuum Assisted Deliveries.: OriginalgagagigoNo ratings yet
- Ultrasound in Obstet Gyne - 2006 - Yang - Sonographic Findings of Placental Lacunae and The Prediction of AdherentDocument5 pagesUltrasound in Obstet Gyne - 2006 - Yang - Sonographic Findings of Placental Lacunae and The Prediction of AdherentdanielNo ratings yet
- Cesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDocument9 pagesCesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDinorah MarcelaNo ratings yet
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocument5 pagesRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioNo ratings yet
- Placenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDocument26 pagesPlacenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDiana PanaitNo ratings yet
- Normal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case ReportDocument3 pagesNormal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case Reportdiaaabdallah209No ratings yet
- Antenatal Diagnosis of Placenta Accreta: A Review: C. H. ComstockDocument8 pagesAntenatal Diagnosis of Placenta Accreta: A Review: C. H. Comstockpamela tyas milanaNo ratings yet
- 1 s2.0 S0002937819312062 MainDocument9 pages1 s2.0 S0002937819312062 MainprofbarrosordemNo ratings yet
- Reech Presentation and Maternal and Perinatal Outcome in A Tertiary Care Teaching Hospital of Central NepalDocument4 pagesReech Presentation and Maternal and Perinatal Outcome in A Tertiary Care Teaching Hospital of Central NepalSharad GajuryalNo ratings yet
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDocument6 pagesSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNo ratings yet
- Natural History of Fetal Position During Pregnancy.11Document6 pagesNatural History of Fetal Position During Pregnancy.11PutriNo ratings yet
- Prenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromaDocument5 pagesPrenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromawitaNo ratings yet
- A First Trimester Scan May Reveal The Presence of Placenta Accreta. Absence of The Anterior Uterine Wall During Caesarean Section: An Unexpected Placenta Accreta That Was Treated ConservativelyDocument3 pagesA First Trimester Scan May Reveal The Presence of Placenta Accreta. Absence of The Anterior Uterine Wall During Caesarean Section: An Unexpected Placenta Accreta That Was Treated ConservativelyBOHR International Journal on GynaecologyNo ratings yet
- Yolk Sac Shape OutcomeDocument11 pagesYolk Sac Shape OutcomeSofyan QadriNo ratings yet
- Mode of Delivery of Twin Gestation With Very Low Birthweight: Is Vaginal Delivery SafeDocument8 pagesMode of Delivery of Twin Gestation With Very Low Birthweight: Is Vaginal Delivery SafeaetpbgNo ratings yet
- Twins PecepDocument8 pagesTwins Pecepjj_cani91No ratings yet
- Antenatal Diagnosis of Placenta Accreta: A Review: C. H. ComstockDocument8 pagesAntenatal Diagnosis of Placenta Accreta: A Review: C. H. ComstockponekNo ratings yet
- The "Vanishing Twin" Syndrome - A Myth or Clinical Reality in The Obstetric Practice?Document3 pagesThe "Vanishing Twin" Syndrome - A Myth or Clinical Reality in The Obstetric Practice?ariniNo ratings yet
- Cesarean Scar Pregnancies and Their ManagementDocument7 pagesCesarean Scar Pregnancies and Their ManagementClinton SitanggangNo ratings yet
- Placenta Previa PDFDocument15 pagesPlacenta Previa PDFDamaris GonzálezNo ratings yet
- MJCU Volume 86 Issue December Pages 4259-4265Document7 pagesMJCU Volume 86 Issue December Pages 4259-4265SamarNo ratings yet
- Plasenta Previa PDFDocument4 pagesPlasenta Previa PDFZuriatun HasanahNo ratings yet
- Print 1 FixDocument10 pagesPrint 1 Fixafriskha bulawanNo ratings yet
- Partus LamaDocument11 pagesPartus LamaSulis SipinNo ratings yet
- Aogs 13333Document7 pagesAogs 13333TiAs TiAriyahNo ratings yet
- Uterine Artery Doppler Flow Studies in Obstetric PracticeDocument4 pagesUterine Artery Doppler Flow Studies in Obstetric Practiceyuyun wahyuniNo ratings yet
- Intrauterine Fetal TransfusionsDocument10 pagesIntrauterine Fetal TransfusionsSaddam FuadNo ratings yet
- Acreta 2014Document12 pagesAcreta 2014pshz92No ratings yet
- Delayed Interval Delivery in Twin Pregnancy Without Cerclage: CaseDocument2 pagesDelayed Interval Delivery in Twin Pregnancy Without Cerclage: Caselailatul husnaNo ratings yet
- Ultrasound in Obstet Gyne - 2019 - Alexandrescu - EP05 07 A Rare Form of Turner Syndrome Diagnosed in The FirstDocument1 pageUltrasound in Obstet Gyne - 2019 - Alexandrescu - EP05 07 A Rare Form of Turner Syndrome Diagnosed in The Firstcringu.ionescuNo ratings yet
- Pregnancy Outcome of Single Previous Cesarean SectionDocument4 pagesPregnancy Outcome of Single Previous Cesarean SectionDhesy WildayaniNo ratings yet
- 1 s2.0 S0090825804003610 Main PDFDocument3 pages1 s2.0 S0090825804003610 Main PDFRirin WahyuniNo ratings yet
- Thy Box Timo Munoz-Chapuli2015Document6 pagesThy Box Timo Munoz-Chapuli2015PABLO ALBERTO SANCHEZ BARRERANo ratings yet
- Baru MDocument3 pagesBaru MRezky Wulandari RoniNo ratings yet
- Acta Obstet Gynecol Scand - 2019 - Litwinska - Ventriculo Amniotic Shunting For Severe Fetal VentriculomegalyDocument6 pagesActa Obstet Gynecol Scand - 2019 - Litwinska - Ventriculo Amniotic Shunting For Severe Fetal VentriculomegalyApotik ApotekNo ratings yet
- A Rare Shape of Placenta Placenta Bipartite, Bilobata, Dimidiate, Duplex: A Rare Case ReportDocument3 pagesA Rare Shape of Placenta Placenta Bipartite, Bilobata, Dimidiate, Duplex: A Rare Case ReportVandana Liju Dev VasudevanNo ratings yet
- Evaluation of Pregnancy Outcome Using Usg Scoring SystemDocument4 pagesEvaluation of Pregnancy Outcome Using Usg Scoring SystemSanjay GoleNo ratings yet
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Document4 pagesOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusNo ratings yet
- Referensi No 7Document5 pagesReferensi No 7Bagus Wanda HabibullahNo ratings yet
- Anal Sphincter Tears at Vaginal Delivery Risk.5Document8 pagesAnal Sphincter Tears at Vaginal Delivery Risk.5Melian AnitaNo ratings yet
- Objectives:: CorrespondenceDocument5 pagesObjectives:: Correspondenceraudatul jannahNo ratings yet
- Prenatal DiagnosisDocument8 pagesPrenatal DiagnosisEstefania GutierrezNo ratings yet
- Sonographic Prediction of Outcome of Vacuum Deliveries: A Multicenter, Prospective Cohort StudyDocument10 pagesSonographic Prediction of Outcome of Vacuum Deliveries: A Multicenter, Prospective Cohort Studysuyudi kimikoNo ratings yet
- Cerclage Twins EJOGRB 2024Document6 pagesCerclage Twins EJOGRB 2024Willans Eduardo Rosha HumerezNo ratings yet
- Gray Scale and Doppler Ultrasound in Placenta AccrDocument5 pagesGray Scale and Doppler Ultrasound in Placenta AccrRicky JunaediNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyMikaNo ratings yet
- Kaplan1998 PDFDocument6 pagesKaplan1998 PDFAmsir LimbongNo ratings yet
- Prediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksDocument4 pagesPrediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksBudi Darmawan DiswanNo ratings yet
- Caug Hey 2005Document7 pagesCaug Hey 2005Andreea BorislavschiNo ratings yet
- Management of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51Document13 pagesManagement of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51indra_strongNo ratings yet
- Fetal Station at Caesarean Section and Risk of SubDocument6 pagesFetal Station at Caesarean Section and Risk of Subggdsnzwbn7No ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentFrom EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNo ratings yet
- Spinal Anesthesia in PediatricsDocument10 pagesSpinal Anesthesia in PediatricsGunther MirandaNo ratings yet
- Children and Neonates Anesthesia in Magnetic Resonance Environment in Italy - BMC Anest22Document9 pagesChildren and Neonates Anesthesia in Magnetic Resonance Environment in Italy - BMC Anest22Gunther MirandaNo ratings yet
- Coana 34 648Document6 pagesCoana 34 648Gunther MirandaNo ratings yet
- Wjo 13 11Document26 pagesWjo 13 11Gunther MirandaNo ratings yet
- Regional Anesthesia To Ameliorate Postoperative Analgesia Outcomes in Pediatric Surgical Patients - Loreane18Document19 pagesRegional Anesthesia To Ameliorate Postoperative Analgesia Outcomes in Pediatric Surgical Patients - Loreane18Gunther MirandaNo ratings yet
- Consensus Guidelines For Sustained Neuromuscular Blockade in Critically Ill Children - Pedane07Document7 pagesConsensus Guidelines For Sustained Neuromuscular Blockade in Critically Ill Children - Pedane07Gunther MirandaNo ratings yet
- Placenta Previa 2Document6 pagesPlacenta Previa 2Gunther MirandaNo ratings yet
- Esteves2 PDFDocument4 pagesEsteves2 PDFGunther MirandaNo ratings yet
- Placenta Previa 1Document2 pagesPlacenta Previa 1Gunther MirandaNo ratings yet
- Transvaginal Ultrasonography For Cervical Assessment For Induction of LaborDocument8 pagesTransvaginal Ultrasonography For Cervical Assessment For Induction of LaborGunther MirandaNo ratings yet
- Esteves 1Document6 pagesEsteves 1Gunther MirandaNo ratings yet
- Antenatal Fetal AssessmentDocument7 pagesAntenatal Fetal AssessmentFitriana Nur RahmawatiNo ratings yet
- 1 s2.0 S0146000508000487 Main PDFDocument6 pages1 s2.0 S0146000508000487 Main PDFKatherin J.No ratings yet
- PGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryDocument8 pagesPGI MANIMTIM - Vaginal Delivery, Breech Delivery and Operative Vaginal DeliveryKim Adarem Joy ManimtimNo ratings yet
- Duty Report 5.12.1978Document55 pagesDuty Report 5.12.1978Riyan W. PratamaNo ratings yet
- Roisin Ryan Obstetrics Final Year RevisionDocument78 pagesRoisin Ryan Obstetrics Final Year RevisionDanny SchNo ratings yet
- Case Note 13: Patient DetailsDocument3 pagesCase Note 13: Patient DetailsBINCY0% (1)
- Preterm Labour: Muhammad Hanif Final Year MBBSDocument32 pagesPreterm Labour: Muhammad Hanif Final Year MBBSArslan HassanNo ratings yet
- NCM QuizDocument7 pagesNCM QuizKyla Marie NabongNo ratings yet
- This Study Resource WasDocument4 pagesThis Study Resource WasOrange AlvarezNo ratings yet
- Hms Implementation GuideDocument122 pagesHms Implementation GuideShuaib KauchaliNo ratings yet
- Chapter 06 Leifer Study Guide KeyDocument4 pagesChapter 06 Leifer Study Guide KeyTyler Finkle92% (12)
- High Risk of PregnancyDocument16 pagesHigh Risk of PregnancyGeraldine PatayanNo ratings yet
- Learner: Lord Mvoula: Test Name Completion Date Score Timespent ResultDocument3 pagesLearner: Lord Mvoula: Test Name Completion Date Score Timespent ResultLord M.No ratings yet
- 3 Tetty+Rumondang+HarahapDocument6 pages3 Tetty+Rumondang+HarahapKurratul 'AiniNo ratings yet
- Lubchanco Classification of Newborns-BoysgirlsDocument1 pageLubchanco Classification of Newborns-BoysgirlsTri Kartika UtomoNo ratings yet
- Maternity MOH 333 PDFDocument4 pagesMaternity MOH 333 PDFMajivaNo ratings yet
- 17 JMSCRDocument5 pages17 JMSCRbela melizaNo ratings yet
- WaterbirthDocument2 pagesWaterbirthapi-405873549No ratings yet
- NCM 107a Care of The Pregnant WomanDocument43 pagesNCM 107a Care of The Pregnant WomanMelchizedek Tagarino Torio100% (1)
- Prenatal Workout Plan: GlowbodyptDocument10 pagesPrenatal Workout Plan: GlowbodyptDébora BezerraNo ratings yet
- Film ScriptDocument4 pagesFilm ScriptclinvilNo ratings yet
- Feasibility Study of Birthing Center in Tuguegarao CityDocument14 pagesFeasibility Study of Birthing Center in Tuguegarao CityUmma Eugenio Agustin75% (4)
- د يزن ابو غربية نسائيةDocument55 pagesد يزن ابو غربية نسائيةobadaNo ratings yet
- Home Birth Setting Versus Hospital Birth SettingDocument4 pagesHome Birth Setting Versus Hospital Birth SettingAmanda Bonita PersaudNo ratings yet
- Guideline No. 402 Diagnosis and Management of Placenta PreviaDocument13 pagesGuideline No. 402 Diagnosis and Management of Placenta PreviaAndrés Gaviria CNo ratings yet
- Dr. Pranav Nursing Academy: Date 23/10/2019Document2 pagesDr. Pranav Nursing Academy: Date 23/10/2019Vicky RathoreNo ratings yet
- A Rare Case Report - Syncephalus Conjoint TwinsDocument3 pagesA Rare Case Report - Syncephalus Conjoint Twinsalifa9393No ratings yet
- Kompilasi - ICD MM Dan PM - Reference GuideDocument93 pagesKompilasi - ICD MM Dan PM - Reference GuidehijraNo ratings yet
- Partograph UseDocument8 pagesPartograph UseJulianne B. Dela Cruz100% (2)
- Partograph Case StudyDocument9 pagesPartograph Case StudyRully Fatriani, M.Keb.No ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Kuliah IUGR PPDS 2023Document48 pagesKuliah IUGR PPDS 2023Fransisko ReinardNo ratings yet