Professional Documents
Culture Documents
Concept Map PE
Uploaded by
Robert Mariasi0 ratings0% found this document useful (0 votes)
262 views3 pagesOriginal Title
Concept Map PE.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
262 views3 pagesConcept Map PE
Uploaded by
Robert MariasiCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
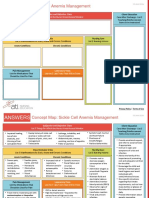
Concept Map
Student Name: Erickson’s Developmental Stage Related to pt. & Cite
Instructor: References (1)
The patient is 39 years old which means she is in the 6th group
based on the staging of Erik Erickson's. The psychosocial crisis is
Patient Education (In Pt.) & Discharge Planning (home needs) represented by intimacy vs isolation while the basic virtue is love.
During this period, people focus on creating a loving relationship
1. Inform the patient about the importance of adhering to blood-thinning and tend to share more intimately with others. Based on the fact that
treatment. Teach her about the possible complications, how to use it and our patient is married for the last 8 years and already has children History of Present Illness (HPI), Pathophysiology of Admitting Dx (Cite
when to stop taking them. we can state that on a physiological level she is doing well and there References) Medical, Surgical, Social History (1).
2. Teach the patient about monitoring her anticoagulant treatment should be no difficulties in her mental evolution. (McLeod,2018)
3. Teach the patient about determining d-dimers level periodically to ensure The patient started having difficulties breathing for the last 4 days. Things got
that there is no risk for other pulmonary thromboembolism even worse. In the beginning, she found it hard to do any physical work
4. Teach the patient about DVT prevention ( fluid intake, physical activity) because of her incapacity to breath correctly. When admitted to the hospital
5. Instruct the patient to quit smoking and provide information on the she was already suffering from dyspnea. More than this she confirmed she
correlation between cigarette smoking and thrombosis. started coughing severely in the last hours and felt like she was not getting
6. Instruct the patient to monitor her health status and attend regularly the enough oxygen.
meetings with the cardiologist.
7. Teach the patient about possible signs of bleeding such as urine in the Cultural considerations, ethnicity, occupation, religion,
family support, insurance. (1) (14) Pathophysiology:
stool or blood, or nose and gum bleeding. Pulmonary thromboembolism is a frequent disease and potentially fatal. It is
(Corrigan,Prucnal,2016) Socioeconomic/Cultural/Spiritual Orientation &
Psychosocial Considerations/Concerns, to include the the second cause of sudden death after that of cardiac origin. PE is
following Social Determinants of Health characterized by high frequency, gravity related to massive thrombus
The patient is married and has one child. She has an active social life migration, relapses, impaired right ventricular function, and an extreme
but she declines any physical activity. She works as a school symptomatic polymorphism, responsible for a large number of errors
professor so she spends a lot of time sitting. Based on ethnicity, she diagnosis. Three main causes predispose the patient to the formation of
is caucasian. She has no strong religion beliefes that could interfere thrombi. They form its so-called triad Virchow: Venous endothelium injury,
with the treatment. She also has full insurance. blood stasis, and hypercoagulability. The most common causes described in
the literature are venous stasis, hypercoagulation, immobilization, surgery and
Diagnostic Test/ Lab Results with dates and trauma, pregnancy, oral contraceptives and substitution estrogens,
Normal Ranges (3) malignancies, hereditary factors, various acute medical conditions, and HIV
infection. Individuals with HIV have a risk of developing TEP and DVT by
40% higher than the uninfected population.
Test Norms Date Current (Morrone,2018)
Value Patient Information Chief Complaint
Troponin 0 7/18/19 0.1 (1) Medical History
Glucose 80- 7/18/19 124 Name: A.M Sudden dyspnea with chest pain, continuous
100 Age: 39 coughing, wheezing.
Creatinine 0.5- 7/18/19 1.1 Gender: F Admitting Diagnosis The patient denies any medical history. Other than the usual pathologies such
1.3 Code Status: Full Status Pulmonary Thromboembolism as viral colds and recurrent streptococcal tonsilitis, nothing is important for
RBC 4.2- 7/18/19 5.33 DPOA: N/A
5.4 the given pathology.
Living Will: N/A
HGB 12-16 7/18/19 14.3
Tonsilitis:
HCT 38- 7/18/19 44
Streptococcal infections are caused by one of many streptococcal species
47%
WBC 5.000- 7/18/19 1000 (Streptococcus). These gram-positive bacteria spheres can cause many
10.000 Medical Management/ Orders/ Medications & Allergies (2) diseases, including streptococcal pharyngitis, pneumonia, skin infections,
D-Dimers <0.5 7/18/19 1.4 wounds, heart and blood valves.
Name Dose RT Freq. MOA RN Onset/Peak
ESR <20 7/18/19 44
Considerations /Duration
LDH 140- 7/18/19 260 (Insulin) Surgical History
200 Rivaroxaban 20 mg P,O Q.D Factor Xa inhibitors *Risk for bleeding
U/L *Does not require
INR determination
The patient denies any medical interventions.
Electrogardiogram : S1Q3T3 , right bundle
*Drug Interactions
branch block with other blood Social History
thining medication
Atorvastatin 40mg P.O Q.D Antilipemic Agent *Monitor the
The patient admits she is a smoker for the last 10 years. She never stopped
Cardiac ultrasound = regional kinetic disorder, smoking and tends to smoke approximately 1 pack per day. She is also
therapeutic effect
remodeling of the LV. *Assess for muscle overweight because she enjoys eating food high in fats and does not engage in
pain
*Avoid
physical activity. She also admits she is drinking a cup of coffee per day and
Pulmonary angiography: thrombus at the level like salty food.
administrating
of the segmentary branches of the pulmonary together with
artery (this is the method which confirmed the digoxin.
diagnosis) *Avoid this
medication during
(Yamamoto,2018) pregnancy
Priority nursing diagnosis #1 Vital Signs (4) Neurological (5) Cardiovascular (6) Respiratory (7) Priority nursing diagnosis #2
Temperature: 98.9 F Shortness of Breath Ineffective breathing patter as
Pain as r/t by the decreased Heart Rate = 120 bpm Anxiety Present Pulse, Hyperventilation r/t by the increasing respirators
pulmonary tissue perfusion which is Respiratory Rate =30 Dizziness due to Chest Pain, Tachypnea
also associated with obstructed rate. (Herdman,Kamitsuru,2017)
cycles/min hyperventilation Tachycardia, Cough is present
pulmonary blood flow. O2 Sat = 90% Otherwise awake and alert High Blood Pressure, Wheezing
(Herdman,Kamitsuru,2017) Cranial Nerves Intact No signs of atrial fibillation
Blood Pressure : 140/88
Nutrition/Hydration GI (9) GU (10) Rest/ Exercise (11)
(8) Normal Bower Sound Clear urine. Chronic Fatigue.
Signs of Dehydration. The Abdomen is painless and Absent Dysuria The patient declines any
patient has dry skin, admits soft. Absent hematuria physical activity .
she drinks les fluids than There are no evident signs Normal Renal Function
required. She also enjoys of obstruction or any GI
Outcome/Goal #1 eating salty food. pathology Outcome/Goal #2
By the end of the shift, I expect By the end of the shift, I expect the
the patient to be pain-free or have patient to no longer be in a state of
her pain level under control and tachypnea. Her blood saturation level
proving that she can breathe will be within the normal range.
Integumentary (12) Endocrine (13) Psychosocial (14) Misc. (Ht/Wt)
effectively
Peripheral Edema No palpable nodules at the Anxious patient and stated Height - 5'3"
(Herdman,Kamitsuru,2017)
Cyanosis level of the thyroid. that she was afraid of dying. Weight - 168 lbs
Pallor No signs of diabetes Even so, she was able to BMI -29.8
Sweating due to anxiety ( polyuria,polydipsia,polyph communicate with the
agia ). medical staff and The patient is overweight
No heat or cold intolerance understood the message. (25-29.9) Interventions # 2
Interventions #1 1. Assess the respiratory rhythm, depth,
1. Assess for s/s of pain and rate.
2. Administered pain medication as 2. Implement the measures needed to
Assessment/ Evaluation #1 Assessment/ Evaluation #2
instructed improve the breathing pattern such as
1. It is known that early intervention for pain management can reduce improve
putting the patient in a high fowler
impaired gas exchange. Monitor gas exchange after treatment1,toTachypnea
evaluate the is frequent during PE. Evaluating the respiratory rate
3. Ude additional measure to relieve response. can ensure that we can avoid any type of complications. position.
the pain as a relaxation technique and
different body positions 2. Pain medication allows the patient to breathe effectively. This will pulse
2. The be oximetry evaluation can help us detect any early 3. Assess lung for the presence of any
reflected by the fact that the patient will no longer be in a state of tachypnea.3.
changes in terms of blood oxygenation. abnormal sounds
Continuously evaluating the patient will ensure that the pain level is kept
4. Provide reassurance to reduce the
under control. 4.Monitor pulse oximetry to ensure that the
anxiety level (Herdman,Kamitsuru,2017) 3. Pain tends to get worse with breathing which can result in
ineffective breathing pattern. By assessing we can also promote a o2 saturation is within a normal range.
4. Anxiety can also lead to shallow respiration and increasing dyspnea. (Herdman,Kamitsuru,2017)
healthy
By reducing the stress level we should see that the patient breathing pattern that would avoid the accumulation of
is feeling
better carbon dioxide in the body. (Herdman,Kamitsuru,2017)
PC Outcomes/Goal PC Interventions PC Evaluation Plan
By the end of the shift, the patient will be stable. The patient will understand the importance of the given medication
The patient will show signs of perfusion She will no longer have difficulties breathing. and will closely follow the physician’s opinion.
Potential Complications/ at risk She will feel less anxious. The patient will meet her appointments and keep under control her
without accusing any pain or shortness of
for (Herdman,Kamitsuru,2017) lipid levels and will also prevent future PE.
breath.
Pulmonary Arterial Hypertension The patient will no longer have any pain and will be able to breath
The patient will have no signs of
due to ineffective vascularization normally.
arrhythmia
Cor Pulmonale due to the effect of The patient will engage in a salt-free diet to reduce the risk of
No long term complications.
ineffective respiratory rate on the recurrence. (Herdman,Kamitsuru,2017)
heart
Severe hypoxemia due to lack of
oxygenation of the blood.
References
Corrigan, D., Prucnal, C., & Kabrhel, C. (2016). Pulmonary embolism: the diagnosis, risk-stratification, treatment and disposition of
emergency department patients. Clinical and experimental emergency medicine, 3(3), 117–125. doi:10.15441/ceem.16.146
Morrone, D., & Morrone, V. (2018). Acute Pulmonary Embolism: Focus on the Clinical Picture. Korean circulation journal, 48(5),
365–381. doi:10.4070/kcj.2017.0314
Saul McLeod,(2018),Erik Erikson's Stages of Psychosocial Development, Simply Psychology,Retrieved on 6/18/2019 from:
https://www.simplypsychology.org/Erik-Erikson.html
T. Heather Herdman ,Shigemi Kamitsuru,(2017),NANDA International Nursing Diagnoses,Thieme,ISBN-10:9781626239296
Yamamoto T. (2018). Management of patients with high-risk pulmonary embolism: a narrative review. Journal of intensive care, 6, 16.
doi:10.1186/s40560-018-0286-8
You might also like
- Concept Map 2Document1 pageConcept Map 2lanrevoiceNo ratings yet
- CHF Concept MapDocument4 pagesCHF Concept MapLisaSanders99No ratings yet
- Nusing CareplanDocument3 pagesNusing Careplanardec_143No ratings yet
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- DRUG ANALYSIS TABLEDocument10 pagesDRUG ANALYSIS TABLEChanel BalinbinNo ratings yet
- Scientific Explanation of Expected Outcomes and InterventionsDocument4 pagesScientific Explanation of Expected Outcomes and InterventionsGensen Cu RoxasNo ratings yet
- CAP Pneumonia CaseDocument46 pagesCAP Pneumonia CaseMatty FelNo ratings yet
- Advanced Chronic Obstructive Pulmonary DiseaseDocument39 pagesAdvanced Chronic Obstructive Pulmonary Diseases1882No ratings yet
- Nursing Care Plan for Stroke PatientDocument12 pagesNursing Care Plan for Stroke PatientMj WilliamsNo ratings yet
- Content: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderDocument4 pagesContent: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderRaffy Sebastian Seballos100% (1)
- Med-Surg Care PlanDocument13 pagesMed-Surg Care Planapi-520453750No ratings yet
- Concept Map (Aplastic Anemia) b1Document6 pagesConcept Map (Aplastic Anemia) b1Ran PioloNo ratings yet
- Rheumatic Joint Disease Study GuideDocument18 pagesRheumatic Joint Disease Study Guidechalinsammy1No ratings yet
- Drug Card SennaDocument1 pageDrug Card SennaAdrianne Bazo100% (1)
- Impaired Tissue Integrity - CellulitisDocument3 pagesImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangNo ratings yet
- LCPDDocument7 pagesLCPDakoismeNo ratings yet
- Sepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultDocument11 pagesSepsis Is The Consequence of A Dysregulated Inflammatory Response To An Infectious InsultShrests SinhaNo ratings yet
- Case Studies On Major Concepts: NeurologicalDocument37 pagesCase Studies On Major Concepts: NeurologicalJek Dela CruzNo ratings yet
- GROUP 3 - CASE STUDY - TraumaDocument5 pagesGROUP 3 - CASE STUDY - TraumaDinarkram Rabreca EculNo ratings yet
- CvaDocument42 pagesCvad_94No ratings yet
- St. Anthony's Nursing Care Plan for Acute Chest PainDocument1 pageSt. Anthony's Nursing Care Plan for Acute Chest PainjoegeNo ratings yet
- Peds Concept MapDocument5 pagesPeds Concept Mapapi-496323326No ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas ExchangeKarylle PetilNo ratings yet
- Concept Map Pleural EffusionDocument1 pageConcept Map Pleural Effusionapi-341263362No ratings yet
- CHF Cardiomegaly Volume OverloadDocument1 pageCHF Cardiomegaly Volume Overloadnursing concept mapsNo ratings yet
- Concept Map 3 MM (Abdominal Pain)Document2 pagesConcept Map 3 MM (Abdominal Pain)Matt McKinleyNo ratings yet
- Careplan 5 MedsurgDocument8 pagesCareplan 5 Medsurgapi-509642710No ratings yet
- Narratives Case NotesDocument4 pagesNarratives Case NotesKnigh RiderNo ratings yet
- Concept Map Meningitis TheoryDocument3 pagesConcept Map Meningitis TheoryMia AuliaNo ratings yet
- Concept Map Template NURS 3073Document4 pagesConcept Map Template NURS 3073Savanna ChambersNo ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Management For Acute Lymphocytic LeukemiaDocument3 pagesManagement For Acute Lymphocytic LeukemiamarivohNo ratings yet
- CVA Impaired Physical MobilityDocument3 pagesCVA Impaired Physical MobilityJasmineNo ratings yet
- NCM 106 - Case Analysis - Nursing Care Plan of Heart FailureDocument2 pagesNCM 106 - Case Analysis - Nursing Care Plan of Heart FailureMarisol Jane JomayaNo ratings yet
- CarePlan #2Document3 pagesCarePlan #2Monika StasiakNo ratings yet
- Nursing Interview Guide To Collect Subjective Data From The Client Questions RationaleDocument19 pagesNursing Interview Guide To Collect Subjective Data From The Client Questions RationaleKent Rebong100% (1)
- Child - AsthmaDocument2 pagesChild - AsthmaCleoanne Gallegos0% (1)
- ARDS Care Respiratory Care Plan PDFDocument2 pagesARDS Care Respiratory Care Plan PDFeric parl0% (1)
- GRP 4 CLO 2 Concept Map PT 1 PDFDocument14 pagesGRP 4 CLO 2 Concept Map PT 1 PDFMaria Lyn Ocariza ArandiaNo ratings yet
- Description: Congestive Heart FailureDocument22 pagesDescription: Congestive Heart FailurePinklet Arleena CubianNo ratings yet
- NUR129 Endocrine Concept Mapping InstructorDocument8 pagesNUR129 Endocrine Concept Mapping InstructorAmber EssmanNo ratings yet
- Pulmonary-Tuberculosis - NCPDocument5 pagesPulmonary-Tuberculosis - NCPMae Therese B. MAGNONo ratings yet
- Nursing Care Plan Breast CancerDocument1 pageNursing Care Plan Breast CancerAhmed SalahNo ratings yet
- ACTIVE LEARNING TEMPLATE: System DisorderDocument1 pageACTIVE LEARNING TEMPLATE: System DisorderDeo FactuarNo ratings yet
- NCPDocument9 pagesNCPKarell Eunice Estrellado Gutierrez100% (1)
- CHD With NCPDocument10 pagesCHD With NCPJohanna Kirsten F. DaguioNo ratings yet
- Nursing Care PlanDocument14 pagesNursing Care PlanVin Landicho100% (1)
- SIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)Document11 pagesSIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)itsmesubu100% (2)
- Nursing DiagnosisDocument10 pagesNursing DiagnosisZaty ChaiyOkk100% (1)
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocument2 pagesNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- Assessment Explanation of The Problem Objectives Interventions Rationale Evaluation Subjective: Sto: DX: StoDocument2 pagesAssessment Explanation of The Problem Objectives Interventions Rationale Evaluation Subjective: Sto: DX: StoSalwa ZeinNo ratings yet
- Modifiable and Non-Modifiable Risk Factors for Aortic AneurysmDocument5 pagesModifiable and Non-Modifiable Risk Factors for Aortic AneurysmJanine Gerunda100% (1)
- SOAPIE and FDAR DocumentationDocument3 pagesSOAPIE and FDAR DocumentationDanna Kim AuxteroNo ratings yet
- Hyperkalemia Discharge PlanDocument2 pagesHyperkalemia Discharge PlanDe Sesto Rhys CarloNo ratings yet
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Business Report - McDonald in Spain FranchiseDocument5 pagesBusiness Report - McDonald in Spain FranchiseRobert MariasiNo ratings yet
- Medical Case AnalysisDocument13 pagesMedical Case AnalysisRobert MariasiNo ratings yet
- Korean Film AnalysisDocument4 pagesKorean Film AnalysisRobert MariasiNo ratings yet
- (Final) Marketing CaseDocument21 pages(Final) Marketing CaseRobert MariasiNo ratings yet
- Two Communication CourseDocument7 pagesTwo Communication CourseRobert MariasiNo ratings yet
- RequestDocument1 pageRequestRobert MariasiNo ratings yet
- Glass & BarnesDocument6 pagesGlass & BarnesRobert MariasiNo ratings yet
- Paraphrase Q&ADocument10 pagesParaphrase Q&ARobert MariasiNo ratings yet
- Running Head: Polysomnography 1: Polysomnography Questions Name Institutional AffiliationDocument8 pagesRunning Head: Polysomnography 1: Polysomnography Questions Name Institutional AffiliationRobert MariasiNo ratings yet
- Effectiveness of A School District Closure For Pandemic in Uenza A (H1N1) On Acute Respiratory Illnesses in The Community: A Natural ExperimentDocument8 pagesEffectiveness of A School District Closure For Pandemic in Uenza A (H1N1) On Acute Respiratory Illnesses in The Community: A Natural ExperimentRobert MariasiNo ratings yet
- Request MARKETING STRATEGY PROPOSALDocument1 pageRequest MARKETING STRATEGY PROPOSALRobert MariasiNo ratings yet
- Question 1: Tweeter Feed Proposal (488 Words) : Outline Communication CourseDocument2 pagesQuestion 1: Tweeter Feed Proposal (488 Words) : Outline Communication CourseRobert MariasiNo ratings yet
- Maintaining Restaurant Business ContinuityDocument8 pagesMaintaining Restaurant Business ContinuityRobert MariasiNo ratings yet
- Modchang Et AlDocument13 pagesModchang Et AlRobert MariasiNo ratings yet
- Davis Et Al PDFDocument8 pagesDavis Et Al PDFRobert MariasiNo ratings yet
- Running Head: Epidemiology 1: Influenza A Outbreak Community Response Plan Name Institutional Affiliation DateDocument6 pagesRunning Head: Epidemiology 1: Influenza A Outbreak Community Response Plan Name Institutional Affiliation DateRobert MariasiNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptRobert MariasiNo ratings yet
- The Two-Party Political System in The U.S.ADocument9 pagesThe Two-Party Political System in The U.S.ARobert MariasiNo ratings yet
- The Two-Party Political System in The U.S.ADocument9 pagesThe Two-Party Political System in The U.S.ARobert MariasiNo ratings yet
- Leadership and Hedgehog Effect 1Document8 pagesLeadership and Hedgehog Effect 1Robert MariasiNo ratings yet
- Workplace Communication: Student Name Course Number UniversityDocument8 pagesWorkplace Communication: Student Name Course Number UniversityRobert MariasiNo ratings yet
- Health Economics Assignment 4Document7 pagesHealth Economics Assignment 4Robert MariasiNo ratings yet
- Social Distancing SociologyDocument7 pagesSocial Distancing SociologyRobert MariasiNo ratings yet
- Chapters 11 and 22 QuestionsDocument1 pageChapters 11 and 22 QuestionsRobert MariasiNo ratings yet
- Health Economics The Organization of Health Insurance MarketsDocument33 pagesHealth Economics The Organization of Health Insurance MarketsRobert MariasiNo ratings yet
- Patient Medical Records: ECG ResultsDocument12 pagesPatient Medical Records: ECG ResultsRobert MariasiNo ratings yet
- 20200501191343cf Bus499 Week3 Assignment 1 TemplateDocument9 pages20200501191343cf Bus499 Week3 Assignment 1 TemplateRobert MariasiNo ratings yet
- Health Economics Health System Reform: Tianxu ChenDocument32 pagesHealth Economics Health System Reform: Tianxu ChenRobert MariasiNo ratings yet
- Health Economics Health System Reform: Tianxu ChenDocument32 pagesHealth Economics Health System Reform: Tianxu ChenRobert MariasiNo ratings yet
- Young People's Ghost Stories in Hong Kong: JosephboscoDocument23 pagesYoung People's Ghost Stories in Hong Kong: JosephboscoRobert MariasiNo ratings yet
- Classification of MD PDFDocument167 pagesClassification of MD PDFyagnaashi9092No ratings yet
- NIRS-InVOS - Reference - Guide For Pediatric UseDocument50 pagesNIRS-InVOS - Reference - Guide For Pediatric UseRaluca LNo ratings yet
- BTS Guideline For Oxygen Use in Adults in HealthcareDocument89 pagesBTS Guideline For Oxygen Use in Adults in HealthcareSoto BrissetteNo ratings yet
- Observer agreement for respiratory signs and oximetry in infants with lower respiratory infectionsDocument4 pagesObserver agreement for respiratory signs and oximetry in infants with lower respiratory infectionsIvan VeriswanNo ratings yet
- Nursing Assessment, Interventions and Evaluation of Mood and Mental StateDocument8 pagesNursing Assessment, Interventions and Evaluation of Mood and Mental StateCrisha Ann Billones BacutaNo ratings yet
- LiverpoolSpO2 MonitoringDocument6 pagesLiverpoolSpO2 MonitoringRiantha SibabutarNo ratings yet
- Oxygen TherapyDocument14 pagesOxygen TherapyEdward NewgateNo ratings yet
- Looney V Moore-Third Amended Complaint 6-21-13Document27 pagesLooney V Moore-Third Amended Complaint 6-21-13mnm3eNo ratings yet
- Guidelines For Sedation and Anesthesia in GI Endos PDFDocument11 pagesGuidelines For Sedation and Anesthesia in GI Endos PDFHernan RuedaNo ratings yet
- Normal Oxygen Transport: Susanne A ClarkDocument256 pagesNormal Oxygen Transport: Susanne A Clarkghoncheh0% (1)
- Hemant Surgical Aero Oxygen ConcentratorDocument1 pageHemant Surgical Aero Oxygen ConcentratorKaushik Hanskumar ShahNo ratings yet
- Reflective Type Blood Oxygen Saturation Detection System Based On MAX30100Document6 pagesReflective Type Blood Oxygen Saturation Detection System Based On MAX30100Emily JulianaNo ratings yet
- F.SARAWI NCP SIC Drug StudyDocument30 pagesF.SARAWI NCP SIC Drug StudyaldwinNo ratings yet
- Capnografo Nellcor NPB-75 Servicio PDFDocument71 pagesCapnografo Nellcor NPB-75 Servicio PDFAgustín CarranzaNo ratings yet
- Initial Assessment and Management OF Pediatric Trauma PatientsDocument11 pagesInitial Assessment and Management OF Pediatric Trauma PatientsCarlos TellezNo ratings yet
- SM en RADICA7 Radical-7 Service Manual Rev.ADocument40 pagesSM en RADICA7 Radical-7 Service Manual Rev.AJose Mellado AlvarezNo ratings yet
- Neonatal Resuscitation Program: 7 EditionDocument64 pagesNeonatal Resuscitation Program: 7 EditionStacy LuceroNo ratings yet
- Assessment PacketDocument3 pagesAssessment Packetapi-337353986No ratings yet
- Pulse Oximetry: Review Open AccessDocument7 pagesPulse Oximetry: Review Open AccessAlain SoucotNo ratings yet
- Veterinary CatalogueDocument28 pagesVeterinary Catalogueelectronico1000No ratings yet
- The New Trauma Score (NTS) : A Modification of The Revised Trauma Score For Better Trauma Mortality PredictionDocument9 pagesThe New Trauma Score (NTS) : A Modification of The Revised Trauma Score For Better Trauma Mortality PredictionstellaNo ratings yet
- Radical-7: Providing Upgradable Rainbow Technology in Multiple Configurations For Maximum Clinical FlexibilityDocument3 pagesRadical-7: Providing Upgradable Rainbow Technology in Multiple Configurations For Maximum Clinical FlexibilityAlondra Lucero MejíaNo ratings yet
- User Manual-Handheld Vital Sign MonitorDocument34 pagesUser Manual-Handheld Vital Sign MonitorJuanNo ratings yet
- 00 Anaethesia NotesDocument62 pages00 Anaethesia Notesoe jarmanNo ratings yet
- Funda Finals Skills NotesDocument17 pagesFunda Finals Skills NotesPauline AñesNo ratings yet
- Pulse Oximeter Based Mobile Biotelemetry ApplicationDocument5 pagesPulse Oximeter Based Mobile Biotelemetry Applicationekrem akarNo ratings yet
- RLE - Reviewer-SuctioningDocument16 pagesRLE - Reviewer-SuctioningVinzii DrtNo ratings yet
- Newborn Assesment in The Delivery RoomDocument9 pagesNewborn Assesment in The Delivery RoomHaRoIsGaNo ratings yet
- Pulse Oximetry v2Document15 pagesPulse Oximetry v2sars_86No ratings yet
- Resmed StellerDocument10 pagesResmed StellersongdashengNo ratings yet