Professional Documents
Culture Documents
Lab Approach
Uploaded by
Muhammad ShaikhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lab Approach
Uploaded by
Muhammad ShaikhCopyright:
Available Formats
R E V I E W ARTICLE
Diagnostic Approach to Primary Immunodeficiency Disorders
M MADKAIKAR, A MISHRA AND K GHOSH
From Department of Pediatric Immunology and Leukocyte Biology, National Institute of Immunohaematology (ICMR), 13th Floor,
NMS Bldg, KEM Hospital, Parel, Mumbai, India.
Correspondence to: Dr Manisha Madkaikar, National Institute of Immunohaematology, 13th Floor, NMS Bldg, KEM Hospital,
Parel, Mumbai 400 012, India. madkaikarmanisha@icmr.org.in
Primary immunodeficiency disorders (PIDs) are a heterogeneous group of inherited disorders that affect different components of the
immune system. There are more than 150 different disorders which have been described till date. Despite major advances in the
molecular characterization of PIDs over the last 20 years, many patients remain undiagnosed or are diagnosed too late with severe
consequences. Recognizing different clinical manifestations of PID is the first most important step. It should be followed by use of
appropriate diagnostic tools from a vast number of investigations available. This review will focus on important presenting features of PID
and laboratory approach for diagnosis of suspected cases of PID.
Key words: Antibody deficiency, Phagocytic defects, Immune dysregulation, Primary immunodeficiency disorders, Severe
combined immunodeficiency (SCID).
P
rimary immunodeficiency disorders (PIDs) persistent infection is the major manifestation of primary
comprise more than 150 different disorders that immunodeficiency (PID), though the pattern, infecting
affect the development, function, or both of the microorganisms and the severity of infections is usually
immune system [1]. In most cases, PIDs are different. While most children with recurrent infections
monogenic disorders that follow a simple Mendelian have a normal immune system, it is important to recognize
inheritance; however, some PIDs are of more complex a child with an underlying PID from a normal child so that
polygenic origin. All forms of PIDs are rare and have an further investigations can be ordered selectively. Prompt
overall prevalence of approximately 1:10,000 live births and accurate diagnosis of PID not only helps to direct the
with the exception of IgA deficiency. However, a much most appropriate treatment, and predict prognosis, but also
higher rate is observed among populations with high it is important for further genetic counseling for the family.
consanguinity or among genetically isolated populations.
The treatment modalities for PID mainly include
PIDs are classified into eight major categories immunoglobulin replacement, antibiotics and bone
according to the component of the immune system marrow transplantation. Immunoglobulin replacement and
primarily involved [1]: judicious use of prophylactic antibiotics can prevent the
significant end organ damage and improve long-term
1. Combined T-cell and B-cell immunodeficiencies
outcome and quality of life in many patients with PID if
2. Predominantly antibody deficiencies diagnosed early [2]. Hematopoietic stem cell
3. Other well defined immunodeficiency syndromes transplantation is used for treating many of the severe
immunodeficiencies. In centers specialized in treating
4. Diseases of immune dysregulation
these conditions, the survival and cure of the disease can
5. Congenital defects of phagocyte number and function reach up to 95%, depending on the condition of the patient
6. Defects in innate immunity at the time of treatment and the donor availability [3]. Thus
it is important to recognize children with PID before
7. Autoinflammatory disorders significant end organ damage occurs to maximize the
8. Complement deficiencies. opportunity for successful treatment and a normal lifespan.
In infants and children (early childhood), the immune In this review we have highlighted the important
system is not fully developed and they are also exposed to clinical manifestations of PIDs including the pattern of
many pathogens as they mix with family members and infections which would alert the clinicians to suspect PID
other children in the nursery. Therefore recurrent and the laboratory approach required for further
infections are common in young children. Recurrent or evaluation of some common categories of PID.
INDIAN PEDIATRICS 579 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
RECOGNIZING CLINICAL MANIFESTATIONS OF PID Box 1 Warning Signs for Suspicion of Primary
Immuno-deficiency Disorders [4].
Careful clinical evaluation is crucial for recognition of
patients with PID. It is important to know the presenting • Four or more new ear infections within 1 year.
features and warning signs of PID in order to decide the • Two or more serious sinus infections within 1 year.
need for further investigations. The European Society of • Two or more months on antibiotics with little effect.
Immunodeficiencies (ESID) has suggested 10 warning • Two or more pneumonias within 1 year.
signs for suspicion of PID [4] (Box 1) [4,7].
• Failure of an infant to gain weight or grow normally.
Although this does not include comprehensive list of • Recurrent, deep skin or organ abscesses.
all signs and symptoms of PID, patients showing these • Persistent thrush in mouth or fungal infection on skin.
signs must be evaluated further for an underlying PID.
• Need for intravenous antibiotics to clear infections.
While evaluating such children, important clinical features
like age at presentation, pattern of infection, non- • Two or more deep-seated infections including septicemia.
infectious manifestations and family history should also • A family history of PID.
be taken into consideration as these give an important clue
to the underlying immune defect [5]. Though it is difficult Lymphopenia is commonly seen with patients with
to predict a specific PID on the basis of infections with SCID and requires further evaluation for specific
particular organisms, they definitely provide an important diagnosis. However normal absolute lymphocyte count
clue to underlying immune defect (Table I). The important does not rule out combined immunodeficiency, thus
distinct clinical manifestations of different categories of further laboratory evaluation is required in case of strong
PID are discussed below. clinical suspicion. Neutropenia is seen in many PIDs [8]
Combined T and B Cell Deficiency including CD40L deficiency.
There are 22 different groups of diseases that have been Predominant Antibody Deficiency
included in this category [1]. Severe combined This category includes 6 groups of diseases [1] of which
immunodeficiencies (SCID) like Adenosine deaminase X-linked agammaglobulinemia (XLA) and common
(ADA) deficiency, purine nucleotide phosphorylase variable immunodeficiency (CVID) are the commonest.
(PNP) deficiency, RAG1/2 deficiency, α chain deficiency, Patients with XLA typically present after 6-9 months of
IL7Rα deficiency, and JAK3 deficiency and combined age when the level of protective maternal IgG starts going
immunodeficiency (CID) like CD40 ligand deficiency (X- down [9]. Recurrent sinopulmonary infections due to S.
linked hyper IgM) are some of the common combined pneumonia or H. influenza, otitis media, and septicemia
immunodefciencies. These patients usually present are the most common clinical manifestations. Less
within first six months of life with failure to thrive, chronic common manifestations include enteroviral infections
diarrhea, persistent oral thrush, skin rash, pneumonia, with resultant chronic meningitis, dermatomyositis, and
and sepsis. Disseminated BCG infection is commonly rheumatoid like arthritis. Patients of CVID usually
seen in patients with SCID. Similarly, prolonged present later in life that is after 5 years though some may
interstitial pneumonia of viral etiology such as present as early as 2 years of age. There is also an
parainfluenza virus or cytomegalovirus or Pneumocystis increased risk of cancer in CVID cases predominantly
jerovici is also common in patients with combined with lymphoreticular tumors and some patients can also
immunodeficiency [6, 7]. develop autoimmune diseases [10].
Omenn syndrome is a rare autosomal recessive
Other Well-defined PID
disease usually presenting in neonatal period,
characterized by symptoms of SCID associated with other This category includes 9 different groups of diseases
findings like erythroderma, lymphadenopathy, such as Ataxia telengiectasia (AT), DiGeorge syndrome,
hepatosplenomegaly and eosinophilia. Most of the Wiskott-Aldrich syndrome (WAS) and hyper IgE
patients with PNP deficiency have neurological problems syndrome (HIGE) [1]. Patients with AT or Nijmejen
including developmental delay, hypertonia, spasticity, Breakage syndrome can present at the age of 6 months to
tremors, ataxia, retarded motor development, behavioral 5 years with gait abnormalities or neurodevelopmental
difficulties and varying degrees of mental retardation. delay. Progressive cerebellar ataxia with discrete or
Characteristic abnormality in ADA deficient SCID includes pronounced telengiectasia involving the conjunctiva
cupping at the end of the ribs demonstrated on a chest ears and sometimes face are the classical findings in
radiograph. They may also present with delayed ataxia-telengiectasia. Patients with DiGeorge syndrome
development, deafness and seizures. present in neonatal period. This defect should be
INDIAN PEDIATRICS 580 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
TABLE I CLUES TO THE PRESENCE OF PRIMARY IMMUNODEFICIENCY
PID Category Infectious complications Organisms Diagnostic tests
Combined T and Systemic viral Bacteria: Pyogenic bacteria T cells:
B cell deficiency infections, Campylobacter Listeria Lymphocyte subsets:
gastroenteritis 1. T, Tc, Th, B , NK
2. DNT cells
3. Memory, naïve and activated T cell
Viruses: All, especially, respiratory Specific cell surface antigen expressions:
syncytial virus, EBV, parainfluenza 1. CD132:
type 3 2. CD127
Fungi:Candida, Aspergillus 3. CD154
Functional assays:
pSATA5 expression after stimulation
Mycobacteria: Nontuberculous pSTAT3 expression after stimulation
including BCG T cell proliferation assays by CFSE
Protozoa:Pneumocystis jiroveci, Certain cytokine estimations: IL-10,
Toxoplasma gondii, IL-12 and INF g
Cryptosporidium parvum RBC ADA levels
Antibody Upper and lower Bacteria:S. pneumoniae, H. influenzae B cells:
deficiency respiratory tract, M. catarrhalis, P. aeruginosa, S. aureus 1. B cell numbers: CD19, CD79a, CD20
GI tract, skin N. meningitidis, M. pneumoniae 2. Intracellular Btk expression
infections, sepsis, 3. Immunoglobulin estimation by
meningitis nephelometry:Ig G, A, E,M
Specific antibody responses
Viruses: Enteroviruses
Protozoa: Giardia lamblia
Phagocytic Respiratory tract, Liver Bacteria: S.aureus, P. aeruginosa Phagocytic Functions:
defects or lung abscesses, GI Nocardia asteroids, S. typhi 1. CD18, CD11 expression:
diseases, urinary tract 2. DHR
problems Fungi: Candida, Aspergillus 3. NBT
Mycobacteria: Nontuberculous
including BCG
Complement Meningitis, systemic Bacteria: Streptococci, Functional hemolytic assay (CH50 and
deficiency bacterial infections H. influenzae, AH50 assays) and serum concentration
Neiserria measurement for complement components
Viruses: CMV, HSV
suspected in patients with cardiac defects with pneumatocele formation are the commonest presenting
hypoplastic thymus, hypocalcemia and facial manifestations of HIES due to STAT3 defect [11]. Patients
dysmorphism. Eczema in infancy and recurrent with HIES due to DOCK8 deficiency usually present with
staphylococcal skin boils and pneumonia with disseminated moluscum contagiosum (Fig.1) or
INDIAN PEDIATRICS 581 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
disseminated viral warts [12]. Autosomal dominant HIES neutrophil disorder like LAD-I [16], SCN or CGD. Patients
is commonly associated with multiple connective tissue with LAD-II have severe mental retardation, short stature,
and skeletal abnormalities including scoliosis, hyper a distinctive facial appearance and the rare Bombay (Hh)
extensibility, pathologic fractures, retained primary phenotype. Eczematous rash with deep seated abscesses
dentition, craniosynostosis, and vascular abnormalities is associated with CGD. Infections due to S. aureus,
[13]. Central nervous system abnormalities are common in Burkholderia cepacia and fungal infections (mainly
HIES. Asymptomatic cerebral T2-weighted hyper- Aspergillus) are common in CGD [17].
intensities, increased prevalence of lacunar infarcts, and
Disseminated atypical mycobacterial infection or
increased Arnold Chiari 1 malformations are seen in the
BCGiosis or recurrent salmonella infection in an otherwise
brain MRI of many patients [14].
well grown individual leads to suspicion to Mendelian
WAS patients present with eczema, petechiae and susceptibility to mycobacterial diseases (MSMD) due to
recurrent sino-pulmonary manifestations [15]. The type-I cytokine defects [18]. Persistent neutrophilia even
incidence of EBV associated lymphoma is also high in in the absence of active infection is a common feature of
these patients. Thrombocytopenia with low mean platelet LAD-I. In severe congenital neutropenia child has
volume gives important clue for diagnosis of WAS. persistently low absolute neutrophil counts (ANC) with
elevated monocytes and eosinophils counts. Cyclic
Phagocytic defects
neutropenia patients present with drop in ANC every 3-4
This category of PID includes 5 groups of diseases [1] of weeks with fever, infections and mouth ulcers.
which leukocyte adhesion deficiency-I (LAD-I), chronic
Diseases of immune dysregulation
granulomatous disease (CGD) and severe congenital
neutropenia (SCN) are some of the common diseases. Four groups of diseases are included in this category [1].
Patients with phagocytic defects usually present in Familial Hemophagocytic Lymphohistiocytosis (FHL)
neonatal period. Delayed separation of umbilical cord that includes Perforin deficiency, UNC13D (Munc13-4)
beyond 2 weeks along with omphalitis is suggestive of a deficiency, Syntaxin 11 deficiency and STXBP2 (Munc
18-2) deficiency and Autoimmune Lymphoproliferative
syndrome (ALPS) are the most common groups of
diseases in this category. Patients with diseases of
perforin defect usually present at less than six months of
age. Patients with Autoimmune Lymphoproliferative
syndrome (ALPS) present at the median age of around 2
years with chronic nonmalignant lymphadenopathy,
splenomegaly and immune cytopenias [19].
Mucocutaneous albinism is seen with patients with
Griselli syndrome and Chediak-Highashi syndrome [20].
Patients with hemophagocytic lymphohistiocytosis
(HLH) (either familial or associated with Chediak-Higashi
or Griscelli syndrome-II, X-linked lymphoproliferative
syndrome) are associated with varying degrees of
cytopenias with hemophagocytosis seen either in the
bone marrow or rarely in the peripheral blood. Patients with
ALPS generally have elevated ALC with recurrent non-
malignant lymphadenopathy and spleno-hepatomegaly.
Patients with Evan’s syndrome should be evaluated for
underlying ALPS as high proportion of these cases have
FAS gene mutation [21]. Autoimmune cytopenias are also
commonly seen in patients with immune dysregulation,
polyendocrinopathy, enteropathy or X-linked (IPEX)
syndrome. Hematolymphoid malignancies are common
with certain PID. Patients with ALPS are at a higher risk of
developing the Non-Hodgkin and Hodgkin lymphoma.
FIG. 1 Patient with HIES due to DOCK8 deficiency with EBV-associated lymphoma is common in patients with
disseminated Molluscum contagiosum. XLP.
INDIAN PEDIATRICS 582 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
Complement deficiency Suspected Combined T and B-cell Immunodeficiency
Patients with complement deficiency present later in life Lymphocyte subset analysis is abnormal in most cases of
usually after 5 years of age. Autoimmune disease and SCID and in many cases of CID. SCID comprises of a
pyogenic infections are often associated with a deficiency group of inherited disorders that characteristically show
of early components (complements 1-4) of the classic abnormalities in T, B, and natural killer (NK) cell
pathway. Terminal complement component deficiencies function. These are categorized broadly as T+ SCID and
(complements 5-9) have increased susceptibility to T-SCID depending on presence or absence of the T cells.
serious infections from Neisseria species [10].
There are many genetic defects which can lead to T-
Complications such as recurrent pneumonia, meningitis,
SCID phenotype [23]. The B cells and NK cells count in
and peritonitis are seen in complement 3 deficiency.
these patients give an important clue to the underlying
LABORATORY APPROACH TO PATIENTS WITH PID molecular defects (Fig. 2). However, there is significant
overlap between these categories and hence specialized
With wide array of assays being available for evaluation
tests like CD132 and CD127 expression, functional
of immune system, it becomes difficult to choose an
studies like pSTAT5 activation in lymphocytes after IL-2
investigation to be performed. The investigations are
stimulation, estimation of enzymes like ADA and PNP in
largely guided by the clinical presentation of the patient,
RBCs, radiation sensitivity test, etc. are required for
the suspected immune defect and the results of initial
specific diagnosis.
laboratory evaluation.
Patients with normal T cell numbers can still have CID.
The most useful first-line immunological
This is usually seen with patients with Omenn syndrome,
investigations include a complete blood count with a
MHC-I or MHC-II deficiency, ZAP 70 deficiency, etc.
differential count on the leucocytes and MPV, lymphocyte
These patients can be evaluated by doing T cell
subset analysis, serum immunoglobulin levels and
proliferation assays (for evaluation of T cell function),
Nitroblue Tetrazolium test (NBT). The panel of antibodies
expression of HLA-DR on T and B cells (for MHC class-II
used for these purpose includes CD3, CD4, CD8, CD56/
expression) and T cell receptor (TCR) V-beta repertoire
16, CD19 and HLA-DR. It is aimed at measuring the
analysis (for assessment of diversity of immune
absolute and relative number of : B cells (CD19+), T cells
response).
(CD3+), T-helper cells (Th, CD3+/CD4+), T-cytotoxic cells
(Tc, CD3+/CD8+), Natural Killer (NK) cells (CD3-/CD56+/ Suspected B-cell Defect
CD16+), and Activated T cells (CD3+/HLA-DR+).
Patients with suspected B cell defects require estimation
It is very important to note that the total lymphocyte of B cell numbers (CD19, CD20 and CD79a), and serum
numbers and T lymphocyte subsets are age-dependent, immunoglobulin levels (IgG, IgA, IgM, IgE and IgG
being markedly increased in newborns and young infants subclasses). Patients with absent B cells and markedly
and decreasing with age. In infants below 4 months of age, reduced Ig are suggestive of agammaglobulinemia which
a CD4 count of <1000/mm3 is generally associated with
impaired cellular immunity, whereas the corresponding
value is <500/mm3 in children over 2 years of age and in
adults [22]. Immunosuppressive therapies like steroids
also significantly alter the values of T and B cell subsets
and should be interpreted carefully.
The results of the initial tests usually give an important
clue to the underlying immune defect. Patients with low T
cell counts are likely to have combined T and B cell defects
(CID). Patients with low or absent B cell and low
Immunoglobulin levels with normal T cell fall in the
category of predominantly antibody deficiency. Patients
with abnormal neutrophil count or abnormal neutrophil
function suggest defects in the phagocytic system.
However, under these broad categories, there are many
subcategories or genetic defects and one needs advanced
laboratory tests available only at specialized centers to
come to a specific diagnosis. Details of evaluation follow: FIG. 2 Evaluation of patients with T- SCID.
INDIAN PEDIATRICS 583 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
can be X-linked (XLA) or autosomal recessive of CD18, CD11a, CD11b and CD11c expression on
agammaglobulinemia. Patients with XLA will have absent peripheral blood leukocytes.
or reduced expression of protein Bruton Tyrosine Kinase
Suspected Immune Dysregulation
(BTK) with carrier mothers showing mosaic pattern.
Patients with reduced Ig with normal to low B cells with There are two important groups of disorders in this
abnormal specific antibody responses suggest common category.
variable immunodeficiency (CVID). Patients with Hyper
Familial Hemophagocytic Lymphohistiocytosis (HLH):
IgM syndrome (HIGM) have markedly low IgG and IgA
HLH can result from secondary causes like infections,
with normal to elevated IgM levels. They can be further
malignancy, rheumatic diseases or toxins or may be due to
evaluated by studying expression of CD40 and CD40L
inherited genetic defect leading to impaired NK cell
(CD154) expression on B cells and T cells respectively.
function. It is also important to differentiate primary HLH
Patients with X-linked HIGM will have abnormal CD 154
from secondary HLH as the patients with primary HLH are
expression on T cells after stimulation and carrier mothers
more likely to relapse after therapy and require
will show mosaic pattern.
hematopoietic stem cell transplantation for long term
Some patients with these disorders may have normal or survival. The diagnosis of HLH is often difficult due to the
only modestly reduced immunoglobulin levels; therefore, rarity of the disease and lack of a specific laboratory test,
the best approach for confirming a diagnosis of an resulting in under diagnosis. In an attempt to overcome
antibody-deficiency disorder is the measurement of serum these difficulties, the FHL study group of the Histiocyte
specific antibody titers (usually IgG) in response to Society has proposed diagnostic guidelines for HLH
vaccine antigens. This approach involves immunizing a (Table II) [24]. The diagnosis of HLH is based on clinical
patient with protein antigens (e.g., tetanus toxoid) and and laboratory criteria which involve complete hemogram,
polysaccharide antigens (e.g., pneumococcus) and bone marrow aspiration studies, liver function tests,
assessing pre- and post-immunization antibody levels. In estimation of S bilirubin, S ferritin, S triglyceride, S
many PIDs, antibody responses to these antigens are
diminished or even absent. TABLE II DIAGNOSTIC CRITERIA FOR HLH PROPOSED BY
HISTIOCYTE SOCIETY
Suspected Phagocytic Defects
1. Molecular diagnosis of hemophagocytic
In a patient with suspected phagocytic defect one must lymphohistiocytosis (HLH) or X-linked
look at the absolute neutrophil count (ANC). A patient lymphoproliferative syndrome (XLP).
with low ANC with early neonatal presentation is
OR
suggestive of severe congenital neutropenia (SCN).
Characteristically, there is marked monocytosis with levels 2. at least 3 of 4:
often two to four times that of normal. There may be a. Fever ≥38.5°C
associated anemia and mild thrombocytosis attributable to b. Splenomegaly
chronic inflammation. Bone marrow examination shows the c. Cytopenias (minimum 2 cell lines reduced)
presence of early precursor cells but very few mature cells Hemoglobin < 9g/dL (in infants < 4 weeks;
beyond the promyelocyte stage or ‘promyelocyte arrest’. Hemoglobin < 10g/dL; Platelets < 100×103/mL;
Patients with cyclic neutropenia have oscillations of Neutrophils < 1×103/mL
neutrophil count with a periodicity of around 21 days. At d. Hepatitis
the nadir, neutrophil counts are generally less than 0.2×109
3. And at least 1 of 4:
per L for 3-5 days, after which they rise rapidly to levels near
the lower limit of normal, about 2×109 per L. Both SCN and a. Hemophagocytosis
cyclic neutropenia commonly result from mutations in b. Ferritin > 500ng/mL
↓
neutrophil elastase gene (ELA-2). c. sIL2Rα (age-based)
Patients with suspected CGD have normal or elevated d. Absent or very low NK function
ANC and can be diagnosed by NBT and DHR test. These 4. Other results supportive of HLH diagnosis:
tests can also detect carrier mothers in X-linked CGD. Final
a. Hypertriglyceridemia (>265 mg/dL)
confirmation of underlying defect can be done by
studying the intracellular expression of gp91 for X-CGD b. Hypofibrinogenemia (<150 mg/dL)
and p22, p67 or p47 for autosomal recessive CGD followed c. Hyponatremia
by molecular analysis of the affected gene. Patients with Source: ASH Education Book January 1, 2009 vol. 2009 no. 1 127-
LAD-I can be easily diagnosed by flowcytometric analysis 131.
INDIAN PEDIATRICS 584 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
fibrinogen and sCD25 levels [25]. Further evaluation There is very little data available from India on PID. Being
using NK cell cytotoxicity assay, Perforin expression a country with the second largest population in the world,
studies, Granule release by NK cells and SAP and XIAP we are likely to have large number of patients with PIDs.
expression on lymphocytes and MUNC 13-4 and Recognizing a suspicious case of PID at a regional
SYNTAXIN-11 by western blot help significantly in hospital level is important to ensure timely referral to a
diagnosis of genetic HLH. specialized centre for diagnosis and treatment for these
patients. We need to create awareness about these
Autoimmune lymphoproliferative syndromes (ALPS): disorders and possibly establish more centers with
Autoimmune lymphoproliferative syndrome (ALPS) is a diagnostic facilities for their evaluation.
disorder of lymphocyte homeostasis characterized by
non-malignant lymphoproliferation autoimmunity mostly Contributors: MM has conceived and written the manuscript.
directed toward blood cells and increased risk of GK revised the manuscript for important intellectual content.
lymphoma. If ALPS is suspected based on clinical findings, MA compiled the data and helped in manuscript writing. The
final manuscript was approved by all authors.
initial laboratory evaluation includes flow cytometric
Funding: None; Competing interests: None stated.
analysis of peripheral blood circulating TCR ab+ DNT
cells and estimation of serum B12, soluble FAS ligand REFERENCES
(sFASL), interleukin (IL) -10 and IL-18 levels. The
1. Al-Herz W, Bousfiha A, Casanova JL, Chapel H, Conley
recommended percentage of TCR ab+DNT cells required ME, Cunningham-Rundles C, et al. Primary
for a diagnosis is greater than or equal to 1.5% of total immunodeficiency diseases: an update on the classification
lymphocytes or 2.5% of T lymphocytes in the setting of from the International Union of Immunological Societies
normal or elevated lymphocyte counts. The presence of Expert Committee for Primary Immunodeficiency.
elevated TCR ab+ DNT cells coupled with high serum or Frontiers in Immunology. 2011;2:54.
plasma levels of either IL -10, IL-18, (sFASL) or vitamin B12 2. Piguet D, Tosi C, Luthi JM, Andresen I, Juge O. Redimune
can accurately predict the presence of germ line or somatic ((R)) NF Liquid, a ready-to-use, high-concentration
FAS mutations [26]. intravenous immunoglobulin therapy preparation, is safe
and typically well tolerated in the routine clinical
Suspected Complement Deficiency management of a broad range of conditions. Clin Exp
Immunol. 2008;152:45-9.
In patients with suspected complement deficiency, initial 3. Notarangelo LD, Forino C, Mazzolari E. Stem cell
evaluation is done with the CH50 (which tests the transplantation in primary immunodeficiencies. Curr Opin
classical and final lytic components except C9) and AH 50 Allergy Clin Immunol. 2006;6:443-8.
(which tests alternative and final lytic pathways) assays. 4. Subbarayan A, Colarusso G, Hughes SM, Gennery AR,
These tests should be done in laboratories with Slatter M, Cant AJ, et al. Clinical features that identify
children with primary immunodeficiency diseases.
considerable experience of these assays. To avoid
Pediatrics. 2011;127:810-6.
misinterpretation due to the possible effects of 5. Slatter MA, Gennery AR. Clinical immunology review
complement consumption by immune complex formation, series: an approach to the patient with recurrent infections
it is advisable that the assays be performed when the in childhood. Clin Exp Immunol. 2008;152:389-96.
patient has completely recovered from immune complex 6. Winkelstein JA, Marino MC, Ochs H, Fuleihan R, Scholl
disease or infection. Both the tests require blood to be PR, Geha R, et al. The X-linked hyper-IgM syndrome:
taken atraumatically and serum be separated within 1 hour clinical and immunologic features of 79 patients. Medicine
and stored at -700C. If either of these screening tests (Baltimore). 2003;82:373-84.
identifies failure of a complement pathway on two 7. Berrington JE, Flood TJ, Abinun M, Galloway A, Cant AJ.
Unsuspected Pneumocystis carinii pneumonia at
occasions, the specific component defect should be
presentation of severe primary immunodeficiency. Arch
determined. Dis Child. 2000;82:144-7.
CONCLUSION 8. Bouma G, Ancliff PJ, Thrasher AJ, Burns SO. Recent
advances in the understanding of genetic defects of
Diagnosis of specific PID from a large spectrum of neutrophil number and function. Br J Haematol.
disorders requires expertise in clinical and laboratory 2010;151:312-26.
evaluation. Wide array of assays are available for 9. Wood P, Stanworth S, Burton J, Jones A, Peckham DG,
Green T, et al. UK Primary Immunodeficiency Network.
evaluation of immune system which help immensely in
Recognition, clinical diagnosis and management of patients
the diagnosis of PIDs. Knowledge of clinical presentation with primary antibody deficiencies: a systematic review.
of these disorders, correct interpretation of initial results Clin Exp Immunol. 2007;149:410-23.
of immunophenotyping of lymphocytes is essential for 10. Zi Yin E, Frush DP, Donnelly LF, Buckleyl RH. Primary
choosing the appropriate test for specific diagnosis. immunodeficiency disorders in pediatric patients: Clinical
INDIAN PEDIATRICS 585 VOLUME 50__JUNE 16, 2013
MADKAIKAR, et al. PRIMARY IMMUNODEFICIENCY DISORDERS
features and imaging findings. Am J Roentgeno. Haematol. 2011;87:1-9.
2001;176:1541-52. 20. Dessinioti C, Stratigos AJ, Rigopoulos D, Katsambas AD.
11. Woellner C, Gertz EM, Schäffer AA, Lagos M, Perro M, A review of genetic disorders of hypopigmentation: lessons
Glocker EO, et al. Mutations in STAT3 and diagnostic learned from the biology of melanocytes. Exp Dermatol.
guidelines for hyper-IgE syndrome. J Allergy Clin 2009;18:741-9.
Immunol. 2010;125:424-32. 21. Teachey D, Manno CS, Axsom KM, Andrews T, Choi JK,
12. Zhang Q, Davis JC, Lamborn IT, Freeman AF, Jing H, Greenbaum BH, et al. Unmasking Evans syndrome: T-cell
Favreau AJ, et al. Combined immunodeficiency associated phenotype and apoptotic response reveal autoimmune
with DOCK8 mutations. N Engl J Med. 2009;361:2046- lymphoproliferative syndrome (ALPS). Blood.
55. 2005;105:2443.
13. Buckley RH. The Hyper-IgE syndrome. Clin Rev Allergy 22. Melaranci C, Ciaffi P, Zerella A, Martinelli V, Cutrera R,
Immunol. 2001;20:139-54. Plebani A, et al. T cell subpopulation in paediatric healthy
14. Freeman AF, Collura-Burke CJ, Patronas NJ, Ilcus LS, children: age-normal values. J Clin Lab Immunol.
Darnell D, Davis J, et al. Brain abnormalities in patients 1992;38:143-9.
with hyperimmunoglobulin E syndrome. Pediatrics. 23. Walshe D, Gaspar HB, Thrasher AJ, Cale CM, Gilmour
2007;119:e1121-5. KC. Signal transducer and activator of transcription 5
15. Albert MH, Notarangelo LD, Ochs HD. Clinical spectrum, tyrosine phosphorylation for the diagnosis and monitoring
pathophysiology and treatment of the Wiskott-Aldrich of patients with severe combined immunodeficiency. J
syndrome. Curr Opin Hematol. 2010. Nov 11. [Epub ahead Allergy Clin Immunol. 2009;123:505-8.
of print] 24. Henter J, Horne A, Aricó M, Egeler RM, Filipovich
16. Madkaikar M, Currimbhoy Z , Gupta M, Desai M, Rao M. AH, Imashuku S, et al. HLH-2004: Diagnostic and
Clinical profile of leukocyte adhesion deficiency. Indian therapeutic guidelines for hemophagocytic lymphohistio-
Pediatr. 2011;49:1-4. cytosis. Pediatr Blood Cancer. 2006;48:124-31.
17. Holland SM. Chronic granulomatous disease. Clin Rev 25. Janka GE. Familial and acquired hemophagocytic
Allergy Immunol. 2010;38:3-10. lymphohistiocytosis. Eur J Pediatr. 2007;166:95–100.
18. Al-Muhsen S, Casanova JL. The genetic heterogeneity of 26. Caminha I, Fleisher TA, Hornung RL, Dale JK, Niemela JE,
mendelian susceptibility to mycobacterial diseases. J Price S, et al. Utilizing biomarkers to predict the presence of
Allergy Clin Immunol. 2008;122:1043-51. FAS mutations in patients with features of the autoimmune
19. Madkaikar M, Mhatre S, Gupta M, Ghosh K. Advances in lymphoproliferative syndrome. J Allergy Clin Immunol.
autoimmune lymphoproliferative syndromes. Eur J 2010;125:946-9.
INDIAN PEDIATRICS 586 VOLUME 50__JUNE 16, 2013
You might also like
- Vries-Driessen2011 Article EducationalPaperDocument9 pagesVries-Driessen2011 Article EducationalPaperCristian HaroNo ratings yet
- Cvid Lancet 2008Document14 pagesCvid Lancet 2008Andre GarciaNo ratings yet
- Jurnal 2Document8 pagesJurnal 2tasya tazkia regita zahraNo ratings yet
- Immunode Ficiency Disorders: Education GapsDocument16 pagesImmunode Ficiency Disorders: Education GapsNadejda MarcovaNo ratings yet
- Overview of Immunodeficiency DisordersDocument25 pagesOverview of Immunodeficiency DisordersLuisa AlandeteNo ratings yet
- Immunodeficiency BriefingDocument4 pagesImmunodeficiency BriefingAldiyanzah Lukman100% (1)
- A Rose Is A Rose Is A Rose But CVID Is Not CVID - Common Variable Immune Deficiency (CVID) What Do We Know in 2011Document61 pagesA Rose Is A Rose Is A Rose But CVID Is Not CVID - Common Variable Immune Deficiency (CVID) What Do We Know in 2011vishnupgiNo ratings yet
- Materi Dr. R. A. Myrna Alia, M.kes, Sp.a (K)Document33 pagesMateri Dr. R. A. Myrna Alia, M.kes, Sp.a (K)Handoyo KooNo ratings yet
- Ten Warning Signs of Primary Immunodeficiency: A New Paradigm Is Needed For The 21st CenturyDocument8 pagesTen Warning Signs of Primary Immunodeficiency: A New Paradigm Is Needed For The 21st CenturyVette Angelikka Dela CruzNo ratings yet
- Primary Immunodeficiency: Review Open AccessDocument8 pagesPrimary Immunodeficiency: Review Open AccessMutiara ChairunnisaNo ratings yet
- IPOPI Booklet VaccinesDocument12 pagesIPOPI Booklet VaccinesnarNo ratings yet
- Pproach To The Child With Recurrent Infections Presentation and Investigation of Primary ImmunodeficiencyDocument5 pagesPproach To The Child With Recurrent Infections Presentation and Investigation of Primary ImmunodeficiencyTri Ayu WdNo ratings yet
- Autoimmunity in Common Variable ImmunodeficiencyDocument11 pagesAutoimmunity in Common Variable ImmunodeficiencyAldito GlasgowNo ratings yet
- Primary Immunodeficiency - PMCDocument1 pagePrimary Immunodeficiency - PMCfaniNo ratings yet
- Common Variable Immunodeficiency: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Classification, and ManagementDocument21 pagesCommon Variable Immunodeficiency: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Classification, and ManagementViviana LunaNo ratings yet
- Ijms 21 05223 PDFDocument42 pagesIjms 21 05223 PDFrohailNo ratings yet
- Cytomegalovirus in Primary ImmunodeficiencyDocument9 pagesCytomegalovirus in Primary ImmunodeficiencyAle Pushoa UlloaNo ratings yet
- Infectious and Noninfectious Pulmonary Complications in Patients With Primary Immunodeficiency DisordersDocument12 pagesInfectious and Noninfectious Pulmonary Complications in Patients With Primary Immunodeficiency Disorderskim leNo ratings yet
- Immune DeficiencyDocument18 pagesImmune DeficiencyDr anas AbdullahNo ratings yet
- Autoinmunidad e InmunodeficienciaDocument9 pagesAutoinmunidad e InmunodeficienciaJorge Verdugo MuñozNo ratings yet
- Szczawinska Poplonyk2009 PDFDocument12 pagesSzczawinska Poplonyk2009 PDFFernando CruzNo ratings yet
- Chronic Mucocutaneous Candidiasis Report of Three Cases With Different PhenotypesDocument4 pagesChronic Mucocutaneous Candidiasis Report of Three Cases With Different PhenotypesDhilah Harfadhilah FakhirahNo ratings yet
- CMV Infection As A Possible Cause of Chronic Diarrhea in Patient With Autosomal Recessive Hyper Ige Syndrome Case ReportDocument2 pagesCMV Infection As A Possible Cause of Chronic Diarrhea in Patient With Autosomal Recessive Hyper Ige Syndrome Case ReportBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- ImmunodeficiencyDocument18 pagesImmunodeficiencyjannah.orangeNo ratings yet
- 2448 9190 Ram 67 03 202Document12 pages2448 9190 Ram 67 03 202anonimo exeNo ratings yet
- State-Of-The-Art Diagnostic Evaluation of Common Variable ImmunodeficiencyDocument9 pagesState-Of-The-Art Diagnostic Evaluation of Common Variable ImmunodeficiencyGreen LightNo ratings yet
- Chapter 15 - The Immunocompromised Host - APIC Text OnlineDocument35 pagesChapter 15 - The Immunocompromised Host - APIC Text OnlineManalAbdelazizNo ratings yet
- Amaya Uribe2019Document21 pagesAmaya Uribe2019kim leNo ratings yet
- 07 Intravenous Immunoglobulin Replacement Therapy in Children With Primary Immunodeficiency Diseases A Nurse S GuideDocument9 pages07 Intravenous Immunoglobulin Replacement Therapy in Children With Primary Immunodeficiency Diseases A Nurse S GuidekiminoooNo ratings yet
- Immune Deficincies - SarahDocument10 pagesImmune Deficincies - SarahkhaledNo ratings yet
- Is Lec Immunodeficiency DiseasesDocument9 pagesIs Lec Immunodeficiency DiseasesKez AmolatoNo ratings yet
- Diagnostic_Testing_Procedures_Document6 pagesDiagnostic_Testing_Procedures_Sarah Marie ArquizaNo ratings yet
- Immunodeficiency 2017 FinalA - 304963 - 284 - 2104 - v3Document6 pagesImmunodeficiency 2017 FinalA - 304963 - 284 - 2104 - v3Muhammed Hashim MNo ratings yet
- Reviewofprimary ImmunodeficiencydiseasesDocument58 pagesReviewofprimary Immunodeficiencydiseasespriti adsulNo ratings yet
- Caso Clínico 1Document24 pagesCaso Clínico 1VillafuerteLizGabyNo ratings yet
- 1 s2.0 S2352304219300881 MainDocument12 pages1 s2.0 S2352304219300881 Mainpdfs studiesNo ratings yet
- Cancers Related To Immunodeficiencies: Update and PerspectivesDocument13 pagesCancers Related To Immunodeficiencies: Update and PerspectivesHabiby Habibaty QolbiNo ratings yet
- Pediatric ImmunologyDocument12 pagesPediatric ImmunologyCharles BayogNo ratings yet
- Current Approach To Primary Immunodeficiency Diseases: March 2019Document9 pagesCurrent Approach To Primary Immunodeficiency Diseases: March 2019Ryan ProxyNo ratings yet
- Reviews Mechanisms, biomarkers and targets for adult-onset Still’s diseaseDocument16 pagesReviews Mechanisms, biomarkers and targets for adult-onset Still’s diseaseRafaela PerezNo ratings yet
- Immunodeficiency Diseases: Professor Shahenaz M.HussienDocument17 pagesImmunodeficiency Diseases: Professor Shahenaz M.HussienVINAY KUMAR DHAWANNo ratings yet
- Pediatric HIV Immune Reconstitution Inflammatory Syndrome (IRISDocument15 pagesPediatric HIV Immune Reconstitution Inflammatory Syndrome (IRISFihzanNo ratings yet
- DR - Dinesh AgarwalDocument20 pagesDR - Dinesh AgarwalPushpanjali Crosslay HospitalNo ratings yet
- Babesiosis in Pregnancy: An Imitator of HELLP SyndromeDocument6 pagesBabesiosis in Pregnancy: An Imitator of HELLP Syndromemade dharmaNo ratings yet
- Immunocompromised DefinitionDocument5 pagesImmunocompromised Definitionapi-511284651No ratings yet
- Ijns 07 00074Document13 pagesIjns 07 00074sunilpkumar18No ratings yet
- Pulmonary Manifestation of PIDDocument14 pagesPulmonary Manifestation of PIDYandiNo ratings yet
- IMMUNOLOGY DISORDERS EXPLAINEDDocument27 pagesIMMUNOLOGY DISORDERS EXPLAINEDShadma KhanNo ratings yet
- Nelson 2017Document28 pagesNelson 2017Santiago GonzalezNo ratings yet
- Management of Patients With Immune Deficiency DisordersDocument11 pagesManagement of Patients With Immune Deficiency DisordersmasheennavirgoNo ratings yet
- MLS 704 Presentation #2Document46 pagesMLS 704 Presentation #2NjeodoNo ratings yet
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2From EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2No ratings yet
- Immunological Changes With Age and Innovative Approaches To Bolster Immune Function in Older AdultsDocument11 pagesImmunological Changes With Age and Innovative Approaches To Bolster Immune Function in Older AdultsKIU PUBLICATION AND EXTENSIONNo ratings yet
- Ni Hms 316844Document15 pagesNi Hms 316844ntnquynhproNo ratings yet
- Seminar: Enno Schmidt, Detlef ZillikensDocument13 pagesSeminar: Enno Schmidt, Detlef ZillikensUssiy RachmanNo ratings yet
- CHAPTER 6 Infection and DiseasesDocument17 pagesCHAPTER 6 Infection and DiseasesDanica DaniotNo ratings yet
- Allergic Diseases in The Elderly: Review Open AccessDocument10 pagesAllergic Diseases in The Elderly: Review Open AccessAngga Aryo LukmantoNo ratings yet
- Peacock Et Al-2016-Oral DiseasesDocument23 pagesPeacock Et Al-2016-Oral DiseasesGgg2046No ratings yet
- Pediatrics - ImmunodeficiencyDocument3 pagesPediatrics - ImmunodeficiencyJasmine KangNo ratings yet
- Manifestation of Aids With Diarhea 1Document6 pagesManifestation of Aids With Diarhea 1nadyaNo ratings yet
- 143-MPhil Biochemistry-1st-1Document2 pages143-MPhil Biochemistry-1st-1Muhammad ShaikhNo ratings yet
- ANALYTICAL ERRORS OF COLLECTING BLOOD FOR CALCIUM TESTINGDocument17 pagesANALYTICAL ERRORS OF COLLECTING BLOOD FOR CALCIUM TESTINGMuhammad ShaikhNo ratings yet
- Bleeding Disorders 082508Document46 pagesBleeding Disorders 082508Muhammad ShaikhNo ratings yet
- Complete Blood Count Examination By:Muhammad Danyal Hayat and Hamza Sarwar Why CBC Is Performed?Document10 pagesComplete Blood Count Examination By:Muhammad Danyal Hayat and Hamza Sarwar Why CBC Is Performed?Muhammad ShaikhNo ratings yet
- Bio SafetyDocument18 pagesBio SafetyMuhammad ShaikhNo ratings yet
- Assessment of Kidney Diseases by Urinalysis: Presented by Group ADocument22 pagesAssessment of Kidney Diseases by Urinalysis: Presented by Group AMuhammad ShaikhNo ratings yet
- NAB Advertisement for Data Entry, Steno, Clerk PositionsDocument5 pagesNAB Advertisement for Data Entry, Steno, Clerk PositionsTanveer Ahmad AfridiNo ratings yet
- NAB Advertisement for Data Entry, Steno, Clerk PositionsDocument5 pagesNAB Advertisement for Data Entry, Steno, Clerk PositionsTanveer Ahmad AfridiNo ratings yet
- ANALYTICAL ERRORS OF COLLECTING BLOOD FOR CALCIUM TESTINGDocument17 pagesANALYTICAL ERRORS OF COLLECTING BLOOD FOR CALCIUM TESTINGMuhammad ShaikhNo ratings yet
- Nelsen ASCPBoardCertificationExamDocument21 pagesNelsen ASCPBoardCertificationExamMuhammad ShaikhNo ratings yet
- Usage History: Total Balance Used Rs 0.0Document4 pagesUsage History: Total Balance Used Rs 0.0Muhammad ShaikhNo ratings yet
- 2Document3 pages2Muhammad ShaikhNo ratings yet
- Urinalysis Sample Report With Notes - 0Document1 pageUrinalysis Sample Report With Notes - 0sukanto bagchiNo ratings yet
- Histotechnology 4e LookInsideDocument51 pagesHistotechnology 4e LookInsideWildercino RA17% (6)
- Medical Lab TechnologyDocument168 pagesMedical Lab Technologyandrei_niculae_2No ratings yet
- LN Urinalysis FinalDocument138 pagesLN Urinalysis FinalMohsen HaleemNo ratings yet
- Diagnosis of Primary ImmunodeficienciesDocument12 pagesDiagnosis of Primary ImmunodeficienciesMuhammad ShaikhNo ratings yet
- Clinical Chemistry - Learning Guide SeriesDocument117 pagesClinical Chemistry - Learning Guide SeriesjonasNo ratings yet
- Jact01i1p39 PDFDocument12 pagesJact01i1p39 PDFMuflih MahsyarNo ratings yet
- Examination Performance Report Spring 2018 Part 1Document3 pagesExamination Performance Report Spring 2018 Part 1Syed Danish AliNo ratings yet
- Template For Staff Development PlanDocument1 pageTemplate For Staff Development PlanKenrick BajaoNo ratings yet
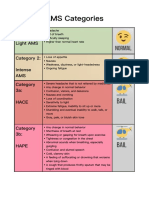
- AMS Symptoms and CategoriesDocument1 pageAMS Symptoms and CategoriesyyggvcNo ratings yet
- Victoria DePonceau SPD ResumeDocument1 pageVictoria DePonceau SPD ResumeVictoria Leigh DePonceauNo ratings yet
- Higado Graso No Alcoholico y Niveles de PCRDocument6 pagesHigado Graso No Alcoholico y Niveles de PCRperuliz19No ratings yet
- B. Bruce Myers, MD PHD FACSDocument5 pagesB. Bruce Myers, MD PHD FACSallison8844No ratings yet
- Shih Tzus: What A Unique Breed!Document5 pagesShih Tzus: What A Unique Breed!Jimmy YauNo ratings yet
- Contractor Safety ManualDocument145 pagesContractor Safety Manualdaladar2008No ratings yet
- Abnormal Psychology Beidel 3rd Edition Test BankDocument4 pagesAbnormal Psychology Beidel 3rd Edition Test BankChuck Simmons100% (25)
- COSH Report - Sir KashmerDocument123 pagesCOSH Report - Sir Kashmerengr rangNo ratings yet
- Diabetes Care in Nigeria - 2015 - Annals of Global Health PDFDocument9 pagesDiabetes Care in Nigeria - 2015 - Annals of Global Health PDFarmanNo ratings yet
- The Essentials of Contraceptive TechnologyDocument355 pagesThe Essentials of Contraceptive TechnologyIndah PurnamasariNo ratings yet
- Psychological JournalDocument3 pagesPsychological JournalDiyah CandraNo ratings yet
- Comparison of Supervised Exercise and Home Exercise After Ankle FractureDocument6 pagesComparison of Supervised Exercise and Home Exercise After Ankle FractureKaren MuñozNo ratings yet
- Full Download Test Bank For Health The Basics 10th Edition by Donatelle PDF Full ChapterDocument36 pagesFull Download Test Bank For Health The Basics 10th Edition by Donatelle PDF Full Chapterpedagog.blocage.5iwtr100% (16)
- Mel Zack 1975Document23 pagesMel Zack 1975Mohammad Jofa Rachman PNo ratings yet
- Conduct Disorder Fact Sheet - K. Elise Parker PDFDocument2 pagesConduct Disorder Fact Sheet - K. Elise Parker PDFepaka02No ratings yet
- The Pan StationsDocument14 pagesThe Pan StationsmuradkhanNo ratings yet
- Proposal Presentation Nairobi - Respicius Shumbusho DamianDocument13 pagesProposal Presentation Nairobi - Respicius Shumbusho DamianShumbusho ConsultingtzNo ratings yet
- No Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateDocument4 pagesNo Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateAnin Kalma MartadinataNo ratings yet
- Occupational Health and Safety Issues of Traffic EnforcersDocument16 pagesOccupational Health and Safety Issues of Traffic EnforcersRhobin Mhark GabitoNo ratings yet
- Pediatric Malnutrition Causes and ManagementDocument38 pagesPediatric Malnutrition Causes and ManagementShafie ElmiNo ratings yet
- Table 6-1 Minimum Filter Efficiencies: ANSI /ASHRAE /ASHE Standard 170-2008Document4 pagesTable 6-1 Minimum Filter Efficiencies: ANSI /ASHRAE /ASHE Standard 170-2008Yousef AlalawiNo ratings yet
- Mental Health EssayDocument2 pagesMental Health EssayROHITNo ratings yet
- CPG Gestational Trophoblastic DiseasesDocument31 pagesCPG Gestational Trophoblastic DiseasesSMR50% (2)
- Lecture 4 Safety Engineering PracticesDocument40 pagesLecture 4 Safety Engineering PracticesPaolo Manuel NagayoNo ratings yet
- Diabetes Type 2 BasicsDocument44 pagesDiabetes Type 2 BasicsMasunji EmanuelNo ratings yet
- The Family Doctor - Prof. Henry S Taylor, M.D., 1860Document324 pagesThe Family Doctor - Prof. Henry S Taylor, M.D., 1860IreneRainsNo ratings yet
- Tobacco Free Generation Next - M. Amebari NongsiejDocument2 pagesTobacco Free Generation Next - M. Amebari NongsiejM. Amebari NongsiejNo ratings yet
- Patient Information Guide: AH-QF-FO-07Document35 pagesPatient Information Guide: AH-QF-FO-07jose rajanNo ratings yet