Professional Documents
Culture Documents
Ineffective Breathing Pattern: Assessment Diagnosis Planning Implementation Rationale Evaluation Independent
Uploaded by
John Glenn Balacano0 ratings0% found this document useful (0 votes)
16 views4 pages Oxygen therapy as Oxygen therapy is used to
needed to maintain oxygen maintain adequate oxygen
saturation above 90%. saturation levels. Low oxygen
levels can lead to respiratory
distress and failure.
Original Description:
NCP
Original Title
ncp-CA
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document Oxygen therapy as Oxygen therapy is used to
needed to maintain oxygen maintain adequate oxygen
saturation above 90%. saturation levels. Low oxygen
levels can lead to respiratory
distress and failure.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views4 pagesIneffective Breathing Pattern: Assessment Diagnosis Planning Implementation Rationale Evaluation Independent
Uploaded by
John Glenn Balacano Oxygen therapy as Oxygen therapy is used to
needed to maintain oxygen maintain adequate oxygen
saturation above 90%. saturation levels. Low oxygen
levels can lead to respiratory
distress and failure.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
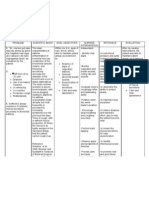
ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION RATIONALE EVALUATION
In 1 hour (short Independent:
After 1 hour of
Subjective: Ineffective term) of nursing Assess the client’s vital signs as Increased BP, RR, and HR
“asthmatic” as breathing intervention, the needed while in distress. occur during the initial hypoxia nursing
what the patient pattern client will be able and hypercapnia. And when it interventions
wrote on the to: becomes severe, BP and HR
paper. drops and respiratory failure the client
1. Establish may result. maintained
a normal,
Objective: effective optimal
- Cough respiratory Assess for the respiratory rate Changes in the respiratory rate breathing
- dyspnea pattern as and rhythm. and rhythm may indicate an
- Abnormal evidenced early sign of impending pattern, as
rise and by the respiratory distress evidenced by
fall of chest absence
- Adventitiou of the Assess the client’s level Anxiety may result from the relaxed
s breath signs and of anxiety struggle of not being able to breathing,
sounds symptoms breathe properly.
of normal
specifically
growing hypoxia, Assess breath sounds and Adventitious sounds may respiratory
sounds with the adventitious breath sounds such indicate a worsening condition
rate or pattern,
- Excessive arterial as wheezing or additional developing
sputum blood complications such as and absence
- Alterations gases pneumonia. Wheezing happens
of dyspnea.
in (ABGs) as a result of bronchospasm.
respiratory within the Diminishing wheezing and
pattern client’s indistinct breath sounds are
- Difficulty in normal or suggestive findings and
verbalizing acceptabl indicate impending respiratory
- Wide eyed e ranges. failure.
look
- Restlessne 2. Client will
ss maintain
optimal Assess the relationship of Reactive airways allow air to
Vital signs: breathing inspiration to expiration move into the lungs more easily
BP: 140/80bmp pattern, than out of the lungs. If the
TEMP: 37’c as client is gasping for air,
RR: 25 breaths evidenced instruction for effective
per min by relaxed breathing is needed.
PR: 93bpm breathing,
normal Assess for dyspnea (Flaring of These indicate respiratory
respiratory nostrils chest retractions, and distress. Once the movement
rate or use of accessory muscle) of air into and out of the lungs
pattern, becomes challenging, the
and breathing pattern changes.
absence
of
dyspnea.
Assess for fatigue Fatigue may indicate distress,
leading to respiratory failure.
Maintain head elevated This promotes maximum lung
expansion and assists in
breathing.
Oxygen saturation is a term
Monitor oxygen saturation referring to the fraction of
oxygen-saturated hemoglobin
relative to the total hemoglobin
in the blood. Normal oxygen
saturation levels are
considered 95-100%
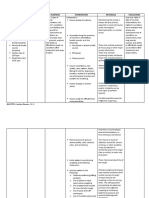
Dependent: The severity of the
exacerbation can be measured
Monitor peaked expiratory flow objectively by monitoring these
rates and forced expiratory values. The peak expiratory
volume as taken by the flow rate is the maximum flow
respiratory therapist. rate that can be generated
during a forced expiratory
maneuver with fully inflated
lungs. It is measured in liters
per second and requires
maximal effort. When done with
good effort, it correlates well
with forced expiratory volume in
1 second (FEV1) measured by
spirometry and provides a
simple, reproducible measure
of airway obstruction.
During a mild to moderate
Monitor arterial blood gases asthma attack, clients may
(ABG) develop respiratory alkalosis.
Hypoxemia leads to increased
respiratory rate and depth, and
carbon dioxide is blown off. An
ominous finding is a respiratory
acidosis, which usually
indicates that respiratory failure
is pending and that mechanical
ventilation may be necessary.
Collaborative:
Short-acting beta-2-adrenergic Short-acting beta2-agonists are
agonist. bronchodilators. They relax the
muscles lining the airways that
carry air to the lungs; treatment
Albuterol (Proventil,
of choice for acute
Ventolin). exacerbation of asthma.
Levalbuterol
(Xopenex).
Terbutaline (Brethine).
Inhaled Corticosteroids.
Budesonide (Pulmicort) Corticosteroids reduce
. inflammation in the airways that
carry air to the lungs and
Fluticasone (Flovent). reduce the mucus made by the
Beclomethasone(Vanc bronchial tubes. Inhaled
steroids should be given after
enase). beta-2-adrenergic agonist.
Mometasone
(Asmanex Twisthaler).
You might also like
- Ineffective Breathing PatternDocument3 pagesIneffective Breathing PatternSandeepNo ratings yet
- Asthma Nursing Care Plans for Breathing DifficultiesDocument5 pagesAsthma Nursing Care Plans for Breathing DifficultiesAstuti Dwi JayantiNo ratings yet
- Name: L.J.A AGE: 20 Years Old SEX: Male CC: Cough and DOB Admitting/Working Diagnosis: AsthmaDocument2 pagesName: L.J.A AGE: 20 Years Old SEX: Male CC: Cough and DOB Admitting/Working Diagnosis: AsthmaMae Therese B. MAGNONo ratings yet
- Gastrectomy NCP IBPDocument3 pagesGastrectomy NCP IBPKevin T. Katada100% (1)
- Nursing Care PlanDocument8 pagesNursing Care Planalexander abasNo ratings yet
- NCP 1 AND SOAPIE 1) Ineffective Breathing PatternDocument5 pagesNCP 1 AND SOAPIE 1) Ineffective Breathing PatternMicaela CrisostomoNo ratings yet
- Bronchial Asthma: Fira Afdila Muhammad Novaldi Nanda ArdiniDocument11 pagesBronchial Asthma: Fira Afdila Muhammad Novaldi Nanda ArdiniPutri IndrianiNo ratings yet
- Daniel P. Soriano BSN 4A Activity 3: Pediatric Nursing Health Assessment and Nursing Care Plan ObjectivesDocument6 pagesDaniel P. Soriano BSN 4A Activity 3: Pediatric Nursing Health Assessment and Nursing Care Plan ObjectivesChezka MendozaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationMargaret ArellanoNo ratings yet
- Maternal Midterm-W2Document2 pagesMaternal Midterm-W2Jireh Vien AtienzaNo ratings yet
- MCN NCPDocument4 pagesMCN NCPPEARL CHRISTINE CUDALNo ratings yet
- NCP - ANAPHYLACTIC SHOCK..2pdfDocument6 pagesNCP - ANAPHYLACTIC SHOCK..2pdfLycah RotoneNo ratings yet
- PE Assessment, Care PlanDocument49 pagesPE Assessment, Care PlanBryan BuendiaNo ratings yet
- goldDocument1 pagegoldCallie ParkNo ratings yet
- Ineffective Airway Clearance-NCPDocument5 pagesIneffective Airway Clearance-NCPJAMES ROD MARINDUQUENo ratings yet
- Assessment Nursing Diagnosis Planning Interventions EvaluationsDocument2 pagesAssessment Nursing Diagnosis Planning Interventions EvaluationsAjay SupanNo ratings yet
- Airway Clearance StrategiesDocument4 pagesAirway Clearance Strategiescammel ramos100% (1)
- Braga, Patricia 4B (NCM 118)Document4 pagesBraga, Patricia 4B (NCM 118)Jessica BragaNo ratings yet
- Scenario 4 - NCPDocument15 pagesScenario 4 - NCPVian RiveraNo ratings yet
- Pediatric Respiratory Anatomy: Course Tak 5 Dula Stephanie PDocument5 pagesPediatric Respiratory Anatomy: Course Tak 5 Dula Stephanie PSteph DulaNo ratings yet
- NCP IcuDocument2 pagesNCP Icujennelyn losantaNo ratings yet
- NCP For Scenario BreathingDocument4 pagesNCP For Scenario Breathingmy moznNo ratings yet
- Ineffective Airway ClearanceDocument1 pageIneffective Airway ClearancejomerdalonaNo ratings yet
- Nursing Process Care Plan For Ineffective Breathing Pattern Assessment Diagnosis Planning Implementation EvaluationDocument19 pagesNursing Process Care Plan For Ineffective Breathing Pattern Assessment Diagnosis Planning Implementation EvaluationZIANAH JOY FAMYNo ratings yet
- CASE SCENARIO and NCPDocument14 pagesCASE SCENARIO and NCPBeverly PagcaliwaganNo ratings yet
- Asthma Attack Nursing Care Plan for Married Female PatientDocument5 pagesAsthma Attack Nursing Care Plan for Married Female PatientMarivic Yuson MalagarNo ratings yet
- Nueva Ecija University of Science and Technology: Case 7Document7 pagesNueva Ecija University of Science and Technology: Case 7jomariNo ratings yet
- NCP FinalDocument5 pagesNCP FinalYoongiNo ratings yet
- Nursing Care Plan: Ineffective Breathing Pattern Related ToDocument4 pagesNursing Care Plan: Ineffective Breathing Pattern Related ToFrudz OrjalezaNo ratings yet
- NCP Pagalanan PablicoDocument15 pagesNCP Pagalanan PablicoRyrey Abraham PacamanaNo ratings yet
- Dela Peña NCP 3Document2 pagesDela Peña NCP 3Mark Teofilo Dela PeñaNo ratings yet
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceJet BautistaNo ratings yet
- Nursing Care Plan (Septick Shock)Document6 pagesNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- Keperawatan Dasar 1 - Kebutuhan OksigenDocument11 pagesKeperawatan Dasar 1 - Kebutuhan OksigenMaulidya AyumiNo ratings yet
- ACUTE RESPIRATORY DISTRESSDocument1 pageACUTE RESPIRATORY DISTRESSchristine louise bernardo100% (1)
- Data NSG Diagnosis Goals & Outcomes NSG Interventions Rationale Evaluation O: StoDocument3 pagesData NSG Diagnosis Goals & Outcomes NSG Interventions Rationale Evaluation O: StoClaudineNo ratings yet
- Nursing Interventions for PneumoniaDocument2 pagesNursing Interventions for PneumoniaGabriel Tolentino70% (10)
- Respiratory Assessment, Intervention and EvaluationDocument1 pageRespiratory Assessment, Intervention and EvaluationJustin Jofer TanNo ratings yet
- Nursing Care Plan for PneumoniaDocument3 pagesNursing Care Plan for PneumoniaFARAH MAE MEDINANo ratings yet
- Nursing Care Plan For Pneumonia NCP PDFDocument3 pagesNursing Care Plan For Pneumonia NCP PDFFARAH MAE MEDINA100% (2)
- Nursing Care Plan: Cues Analysis Nursing Diagnosis Goal and Objectives Intervention Rationale Evaluation SubjectiveDocument6 pagesNursing Care Plan: Cues Analysis Nursing Diagnosis Goal and Objectives Intervention Rationale Evaluation SubjectiveKristel PunoNo ratings yet
- Ineffective Breathing PatternDocument3 pagesIneffective Breathing PatternReichelle Perlas62% (13)
- Iudmc ActivityDocument10 pagesIudmc ActivityJeraldine GumpalNo ratings yet
- Camarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationDocument8 pagesCamarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationEdelweiss Marie CayetanoNo ratings yet
- Cues Nursing Diagnosis Scientific Rationale Objectives Interventions Rationale Evaluation Subjective Cue: Sto: StoDocument7 pagesCues Nursing Diagnosis Scientific Rationale Objectives Interventions Rationale Evaluation Subjective Cue: Sto: StoKasandra Dawn Moquia BerisoNo ratings yet
- NCP FinalDocument16 pagesNCP FinalEuleen Tria PadrigoNo ratings yet
- "She Can't Breathe Well Especially During Episodes of Spasms" As Verbalized byDocument2 pages"She Can't Breathe Well Especially During Episodes of Spasms" As Verbalized byCassey CuregNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- Improve Cardiac Output Through Nursing InterventionsDocument8 pagesImprove Cardiac Output Through Nursing InterventionsJaylord VerazonNo ratings yet
- NCP SciDocument3 pagesNCP SciJaylord VerazonNo ratings yet
- Nursing Care Plan for Improving Respiratory DistressDocument4 pagesNursing Care Plan for Improving Respiratory DistressMichaela JapsayNo ratings yet
- Assessment Diagnosis Planning Intervention EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention EvaluationJohn Glenn BalacanoNo ratings yet
- Nursing Diagnosis PneumoniaDocument1 pageNursing Diagnosis PneumoniaPasa ShresthaNo ratings yet
- Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation IndependentDocument3 pagesNursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation IndependentWyeth Earl Padar EndrianoNo ratings yet
- NCP On DiabetesDocument2 pagesNCP On DiabetesShumaila AlviNo ratings yet
- Nursing Care Plan: Lipa City CollegesDocument13 pagesNursing Care Plan: Lipa City CollegesVincent Maralit MaterialNo ratings yet
- The Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessFrom EverandThe Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessNo ratings yet
- Advanced Recorder Technique: The Art of Playing the Recorder. Vol. 2: Breathing and SoundFrom EverandAdvanced Recorder Technique: The Art of Playing the Recorder. Vol. 2: Breathing and SoundRating: 5 out of 5 stars5/5 (1)
- Furosimide Drug StudyDocument3 pagesFurosimide Drug StudyJohn Glenn BalacanoNo ratings yet
- Quiz in PneumoniaDocument1 pageQuiz in PneumoniaJohn Glenn BalacanoNo ratings yet
- Assessment Diagnosis Planning Intervention EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention EvaluationJohn Glenn BalacanoNo ratings yet
- Substance Abuse PsychologyDocument8 pagesSubstance Abuse PsychologyJohn Glenn BalacanoNo ratings yet
- Blue Bloaters and Pink PuffersDocument2 pagesBlue Bloaters and Pink PuffersAlmir SaraciNo ratings yet
- Ineffective Breathing Pattern: Assessment Diagnosis Planning Implementation Rationale Evaluation IndependentDocument4 pagesIneffective Breathing Pattern: Assessment Diagnosis Planning Implementation Rationale Evaluation IndependentJohn Glenn BalacanoNo ratings yet
- Decena, Cyrille Justine A. BSN-4A: Competency AppraisalDocument4 pagesDecena, Cyrille Justine A. BSN-4A: Competency AppraisalJohn Glenn Balacano100% (2)
- Maternal and Child HealthDocument12 pagesMaternal and Child HealthJohn Glenn BalacanoNo ratings yet
- Balacano, John Glenn Reflection Paper BSN-4ADocument1 pageBalacano, John Glenn Reflection Paper BSN-4AJohn Glenn BalacanoNo ratings yet
- SAIL Questionnaire EnglishDocument3 pagesSAIL Questionnaire EnglishJohn Glenn BalacanoNo ratings yet
- Drug Study ArcoxiaDocument1 pageDrug Study ArcoxiaMichael Baylon DueñasNo ratings yet
- DRUG Stuy CompilationDocument8 pagesDRUG Stuy CompilationJohn Glenn BalacanoNo ratings yet
- Epidemiology of CancerDocument3 pagesEpidemiology of CancerJohn Glenn BalacanoNo ratings yet
- Transformational Theory of LeadershipDocument9 pagesTransformational Theory of LeadershipJohn Glenn BalacanoNo ratings yet
- Six Dimension Scale of Nursing PerformanceDocument4 pagesSix Dimension Scale of Nursing PerformanceJohn Glenn Balacano100% (3)
- Eloor Industrial Health Study - Research Adviser-Dr. Rajan R PatilDocument27 pagesEloor Industrial Health Study - Research Adviser-Dr. Rajan R PatilDr. Rajan R PatilNo ratings yet
- Instruction Manual: VentmeterDocument47 pagesInstruction Manual: VentmeterCarlos Andres Jaimes RicoNo ratings yet
- GEB 0205 Custo Spiro Mobile Spirometry V04 DK 1651 en 001 LENDocument72 pagesGEB 0205 Custo Spiro Mobile Spirometry V04 DK 1651 en 001 LENalbert roviraNo ratings yet
- COPD 385855 Breathing Exercises in The Treatment of Copd An Overview ofDocument11 pagesCOPD 385855 Breathing Exercises in The Treatment of Copd An Overview ofLangit BiruNo ratings yet
- Ophthalmic ENT sLE MCQDocument10 pagesOphthalmic ENT sLE MCQAsif Newaz100% (4)
- Mechanical Ventilation During Anesthesia in Adults - UptoDate 2022Document34 pagesMechanical Ventilation During Anesthesia in Adults - UptoDate 2022Angy KarakostaNo ratings yet
- Status Asthmaticus Case StudyDocument18 pagesStatus Asthmaticus Case Studygeorgeloto12No ratings yet
- UK asthma review finds poor care and preventable deathsDocument24 pagesUK asthma review finds poor care and preventable deathssamNo ratings yet
- Jurnal Copd PDFDocument24 pagesJurnal Copd PDFketut ayu bulanNo ratings yet
- Cindy AprilizaDocument61 pagesCindy AprilizaRegina SaragihNo ratings yet
- Pulmonary Function TestDocument87 pagesPulmonary Function TestRiry AmbarsaryNo ratings yet
- Pulmonary Diseases & Respiratory System AnatomyDocument6 pagesPulmonary Diseases & Respiratory System AnatomyJada NovakNo ratings yet
- The Force Velocity Mechanical Profile in Sprint Running Perspecives in Hamstring Muscle Injury Follow-Up and PreventionDocument8 pagesThe Force Velocity Mechanical Profile in Sprint Running Perspecives in Hamstring Muscle Injury Follow-Up and PreventionMarthinus SchultzNo ratings yet
- Dräger Evita Infinity® V500 Elite: Advanced and Comprehensive Ventilation TherapyDocument4 pagesDräger Evita Infinity® V500 Elite: Advanced and Comprehensive Ventilation TherapyABHINANDAN SHARMANo ratings yet
- The Impact of Pursed-Lips Breathing Maneuver On Cardiac, Respiratory, and Oxygenation Parameters in COPD PatientsDocument6 pagesThe Impact of Pursed-Lips Breathing Maneuver On Cardiac, Respiratory, and Oxygenation Parameters in COPD Patientsmiftahudin sigitNo ratings yet
- University of Guyana School of Medicine Med 1106 - Physiology I DR Kalima ThompsonDocument66 pagesUniversity of Guyana School of Medicine Med 1106 - Physiology I DR Kalima ThompsonKNo ratings yet
- Gera Zeris KotsovosDocument15 pagesGera Zeris KotsovosJoseph HernándezNo ratings yet
- 109 - Obstructive Lung DiseasesDocument8 pages109 - Obstructive Lung DiseasesCharisa Antonette HuelvaNo ratings yet
- Acute Exacerbation of Copd by DR Irappa MadabhaviDocument39 pagesAcute Exacerbation of Copd by DR Irappa MadabhaviIrappa MadabhaviNo ratings yet
- Med-Surg Exam #2 Study GuideDocument33 pagesMed-Surg Exam #2 Study GuideCaitlyn BilbaoNo ratings yet
- Wasserman Chest 1997Document13 pagesWasserman Chest 1997Filip BreskvarNo ratings yet
- SPIROMETRYDocument9 pagesSPIROMETRYaeyousefNo ratings yet
- Pulmonary Function Status of Construction WorkersDocument1 pagePulmonary Function Status of Construction WorkersNabilah BeylaNo ratings yet
- Reference 222Document7 pagesReference 222sabrinaNo ratings yet
- S/5 ADU Carestation: An Integrated Solution For Quality CareDocument6 pagesS/5 ADU Carestation: An Integrated Solution For Quality CareJuan AmaroNo ratings yet
- Pulmonary Function TestsDocument20 pagesPulmonary Function TestsMohamedSalah100% (2)
- Spirometry Testing and Interpretation Guide for Primary CareDocument7 pagesSpirometry Testing and Interpretation Guide for Primary CareAndi JakartaNo ratings yet
- Psychophysiologic Effects of Hatha Yoga On Musculoskeletal and Cardiopulmonary Function: A Literature ReviewDocument17 pagesPsychophysiologic Effects of Hatha Yoga On Musculoskeletal and Cardiopulmonary Function: A Literature ReviewNi Made Wirastuti ShantiNo ratings yet
- Cystic Fibrosis - Management of Pulmonary Exacerbations - UpToDateDocument31 pagesCystic Fibrosis - Management of Pulmonary Exacerbations - UpToDateDylanNo ratings yet
- 02 Incentive SpirometryDocument5 pages02 Incentive SpirometrygireeshsachinNo ratings yet