Professional Documents
Culture Documents
553 Full PDF
Uploaded by
Timothy John ValenciaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
553 Full PDF
Uploaded by
Timothy John ValenciaCopyright:
Available Formats
CLIN.CHEM.
30/4,553-556 (1984)
Effects of Storage Temperature and Time before Centrifugation on Ionized
Calcium in Blood Collected in Plain Vacutainer Tubes and Silicone-Separator
(SST) Tubes
John Toffaietti,”2 Nancy Biosser,2and Kathryn Klrvan3
We studied the stability of ionized calcium and pH in samples h with or without separation from the clot in both plain and
stored at either room temperature or 4 #{176}C,
in centrifuged and silicone-separator tubes. We then evaluated the potential
uncentrifuged blood-collection tubes and in centrifuged tubes value of, and precautions for, using routinely collected
containing a silicone-separator gel (SST tubes).At room samples for measurement of ionized calcium.
temperature,inuncentrifuged blood from healthy individuals,
mean ionized calcium usually increased no more than 10
Materials and Methods
mol/L per hour; at 4 #{176}C
it did not change detectably for 70 h. Ionized calcium, pH, and ionized calcium corrected to pH
This stability was fortuitous, however: the concentrations of 7.4 were measured simultaneously with a Radiometer ICA 1
both hydrogen and lactate ions in these samples increased, ionized calcium analyzer (Radiometer America Inc., West-
apparently with offsetting effects on the concentration of lake, OH 44145). Dialyzable calcium was measured by
ionized calcium. Blood stored for 70 h at 4 #{176}C
in centrifuged continuous-flow analysis (1), and lactate (8) and phosphate
(9) by centrifugal analysis. Measurements of ionized calci-
SST tubes, although showing a slightly greater change in
um, pH, and dialyzable calcium were done in duplicate.
ionized calcium, had less change of pH and no change in the
Blood samples from apparently healthy volunteers, ages
ionized calcium corrected to pH 7.4. In 11 heparinized whole-
23-57 years, were collected in large syringes, then injected
blood samples from eight patients in intensive care, the mean
into evacuated blood-collection tubes containing either no
change per hour in ionized calcium and pH after storage at additive (plain Vacutainer Tubes) or a silicone gel for
room temperature was + 10 mol/L and -0.04 units, respec- maintaining separation of serum from erythrocytes after
tively. centrifugation (SST), both from Becton Dickinson, Ruther-
ford, NJ 07070. For anticoagulants we used either sodium
AdditionalKeyphrases:pH lactate variation, source of heparin (Becton Dickinson) or a calcium-titrated heparin
sample handling . ion-selective electrodes ionized calci-
solution (no. S 4500, Radiometer). Samples were stored at
um vs total calcium room temperature or 4 #{176}C,
(22-25 #{176}C) as noted.
Eleven whole-blood samples, collected in heparinized sy-
One of the subcommittees of the AACC Ionized Calcium ringes (no. MQ6O1 or MQ6O5LD; Marquest Medical Prod-
Working Group was formed to gather information and ucts, Inc., Englewood, CO 80112), containing 30 or 40 mt.
formulate guidelines for collection of samples for measuring units of lithium heparin per milliliter, were selected without
concentrations of ionized calcium; a preliminary report has conscious bias from eight patients who were either in
recently appeared (1). Here, we report our study of the intensive care or undergoing surgery. These samples were
effects of temperature of storage, delay in cell separation, kept on ice before the initial analysis of the whole blood,
and type of blood-collection tube on results for ionized then stored at room temperature for 2 h before re-analysis.
calcium, which may be useful in developing such guidelines.
We have observed little change in dialyzable calcium in Results
serum from blood left to clot for as long as 6 h at room
Table 1 shows the mean, SD, and range of changes in
temperature (2), which is longer than usual for processing
ionized calcium, corrected ionized calcium, and pH in plas-
samples for determinations of ionized calcium (3-5). Fogh-
ma and serum from blood samples that were left uncentri-
Andersen et al. (6) have also reported that clotted blood may
fuged for as long as 3 h. In both plasma and serum the mean
be stored at 0-4 #{176}C for as long as 4 h without affecting
change and most of the individual changes of ionized
results for ionized calcium. The most rapid analyses require
calcium were within the imprecision of the method, about 20
the use of heparinized whole blood or plasma, but calcium
molfL. One sample consistently had a greater change,
binding by heparin and problems with protein adherence to
increasing by 40 to 55 mol/L in 1 to 3 h.
electrodes are drawbacks to procedures involving heparin
With longer storage before centrifugation, as shown in
(7).
Table 2, ionized calcium in blood from four of the five donors
By measuring the changes in ionized calcium, pH, and
changed by no more than 20 molJL after 4 h, although
related constituents, we wanted to determine whether less-
blood from the other donor changed by 80 mo1!L at 4 h. By
rapid collection and handling procedures would still give
6 h, the ionized calcium in all the samples increased by 50
satisfactory results for ionized calcium in serum. We mea-
mo1JL or more. The corrected ionized calcium, however, did
sured ionized calcium, pH, and in some cases dialyzable
not change detectably in plasma or serum.
calcium, lactate, and phosphate in blood samples stored
In general, the pH of the serum or plasma samples
without separation from the clot for as long as 24 h at room
changed by about 0.01 unit per hour of storage at room
temperature, and in samples stored at 4#{176}C
for as long as 70
temperature; lactate, in the study shown in Table 2, in-
creased by two- to threefold during 6 h.
‘Department of Pathology, 2 Clinical Chemistry Laboratory, and Although not shown in Table 1, 28 mt. units of sodium
S Blood Gas Laboratory, Duke University Medical Center, Durham, heparin per milliliter decreased both ionized and dialyzable
NC 27710. calcium by about 100 &moI/L from their concentrations in
Received July 25, 1983; accepted January 18, 1984. serum. This indicates that the effect of heparin was not an
CLINICAL CHEMISTRY, Vol. 30, No. 4, 1984 553
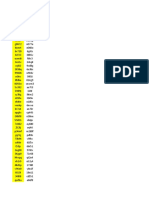
Table 1. Effect of Time before Centrifugation on Changes in Ca2, Ca27.4, and pH in Blood Samples
Stored at Room Temperature
aCa2, iimol,L 4tCa2 umol/L oH
h before
centrlf. Mean SD Range Mean SD Range Mean SD
Plasma containing sodium heparin (28 mt. units/mL)a
0.5 5 23 -15to45 2 22 -20 to40 -0.01 0
1.0 27 26 -5to55 23 18 0 to 40 -0.01 0.005
2.0 18 16 Oto4O 5 15 -15 to 25 -0.02 0.003
3.0 20 25 -lOtoSO -5 27 -40 to 20 -0.04 0.004
SerumL
1.0 33 18 10to45 8 11 -5 to20 -0.02 0.010
2.0 8 33 -35 to 45 -15 30 -50 to 25 -0.03 0.007
3.0 20 25 -45 to 40 -19 30 -60to15 -0.05 0.017
a Changesare relative
toconcentrations
inplasma from blood centrifugedwithin5 mm after collection.
bchangesare relativeto concentrations in serum from blood centrifuged within30 mm aftercollection.
n = 5 donors.
Table 2. Effect of Time before Centrifugation on Changes in Ca2, Ca27.4, pH, and Lactate in Blood
Samples Stored at Room Temperature
Mactate,
aCa2, pmol/L Ca2,4, imoI/L apH mmol/L
h before
centrif. Mean SD Range Mean SD Range Mean SD Mean SD
Plasma containing calcium-titrated heparin (22 mt. units/L)#{176}
2 20 19 5to45 3 5 -5tolO -0.04 0.024 1.5 0.1
4 35 30 20 to 80 3 6 -5 to 10 -0.06 0.049 2.5 0.5
6 65 20 50 to 95 3 8 -10 to10 -0.10 0.041 3.6 0.3
24 157 64 110to230 -130 45 -90 to -180 -0.37 0.150 10.5 2.2
Serumb
2 23 12 15 to40 9 9 0 to20 -0.02 0.011 1.5 0.6
4 19 13 5 to 35 -11 3 -15 to -10 -0.04 0.010 2.2 0.8
6 36 16 25 to 60 -1 17 -15 to 20 -0.06 0.015 2.7 0.7
24 72 11 65to85 -56 14 -4Oto-65 -0.14 0.039 5.4 1.1
Footnotes and n as in Table 1.
artifact of methodology. The use of calcium-titrated sodium Table 3. Changes in Serum Stored for 6 h at 4 #{176}C
heparin, 22 mt. units/mL, eliminated any detectable differ- after Centrifugatlon a
ence in ionized or dialyzable calcium between serum and Mean SD Range
plasma.
Plain tubes
We also measured dialyzable calcium in the samples ACa2, imol/L -2 7 -lOto5
represented in Tables 1 and 2. Up to 4 h, dialyzable calcium pH -0.01 0.003 -0.005 to -0.01
changed by no more than 30 JLmolJL in any sample; the lactate, mmol/L 0.0 0.1 -0.1 to 0.1
change after 6 h was no more than 50 mol/L, consistent iCa274, mol/L -8 10 -2OtoO
with an earlier report (2). SSTtubes
To determine the stability of ionized calcium and pH at Ca2, .mol/L 2 4 Oto7
ApH -0.01 0.003 -0.01 to -0.015
4#{176}C,
we collected blood samples from four volunteers into Alactate,mmol/L 0.0 0.2 -0.2 to 0.1
large syringes, injected the samples into both plain Vacu- Ca274, Lmol/L -3 4 -5toO
tamer Tubes and SST tubes, let them clot for 0.5 h, a Results are from four volunteers. Blood was allowed toclotfor30 mm at
centrifuged, then stored the unopened tubes at 4#{176}Cfor 6 h. room temperaturebeforecentrifugation.
Samples were analyzedimmediately
As Table 3 shows, serum separated from cells in either plain and 6 h aftercentrifugation.
tubes or SST tubes underwent no detectable changes in
ionized calcium, corrected ionized calcium, pH, or lactate for
6 h. However, there was consistently a bias between similar analysis, were divided into three groups: (a) uncentrifuged
samples from plain tubes and SST tubes. blood left in plain tubes for 24 or 70 h, (b) centrifuged blood
Of 12 blood samples simultaneously injected from a large left in plain tubes for 24 or 70 h, and (c) centrifuged blood
syringe into a plain tube and an SST tube, then allowed to left in SST tubes for 24 or 70 h before analysis. As Table 5
clot for 30 mm, ionized calcium was always slightly higher shows, ionized calcium was relatively stable at 4#{176}C under
in samples from SST tubes, as shown in Table 4. The higher all these conditions but most stable in the uncentrifuged
concentrations of lactate in samples from SST tubes appear tubes. The pH was altered most in the uncentrifuged tubes,
to account for these changes. The corrected ionized calcium and lactate, measured in one set of uncentrifuged samples,
was the same in samples from plain tubes or SST tubes. increased by almost threefold (data not shown). Values for
After the 6-h storage study, we wanted to determine how pH and ionized calcium corrected to pH 7.4 varied least for
long samples could be stored at 4#{176}C
before changes in the blood stored in the SST tubes.
ionized calcium or pH became significant. Sets of samples In addition to samples from healthy persons (Tables 1-5),
were collected from each of six healthy volunteers and left to we also studied 11 heparinized whole-blood samples from
clot for 20 mm at 4 #{176}C.
Some were then analyzed for baseline eight patients in intensive care or undergoing surgical
values of ionized calcium and pH; others, kept at 4#{176}Cuntil procedures. As shown in Table 6, the changes in ionized
554 CLINICALCHEMISTRY, Vol. 30, No. 4, 1984
Table 4. Differences in Ca2, pH, and Lactate between Serum from Plain Tubes and from SST Tubes1
Plain tubes SST tubes DIfference
Mean SD Mean SD Mean SD Range
Ca2, hmol/L 1250 40 1270 40 23 9 10 to 40
Ca274, rnol/L 1270 40 1270 30 6 7 0 to 20
pH 7.44 0.04 7.41 0.03 -0.025 0.012 -0.01 to 0.04
Lactate,mmol/L 1.76 0.43 1.92 0.4.3 0.21 0.16 0 to 0.4
‘Blood allowed to clot for 30 mm at room temperature before centritugationand analysis.
n = 12 each.
on Values for Ca2, pH, and Ca2+74a
Table 5. Effect of Stora ge at 4#{176}C
PlaIn tubes, uncentrifuged Plain tubes, centrifuged SST tubes, centrIfuged
Storage,
h Mean SD Range Mean SD Range Mean SD Range
tCa, pmol’L
24 2 8 -10 to10 16 18 -20 to 30 25 8 20 to 40
70 0 16 -20 to20 21 12 10 to 40 30 12 10 to 40
ispH
24 -0.04 0.02 0 to -0.06 -0.03 0.02 0.01 to -0.06 -0.04 0.01 -0.02 to 0.06
70 -0.08 0.04 -0.01 to -0.13 -0.08 0.03 -0.03 to -0.12 -0.05 0.02 -0.04 to -0.08
iCa74, mo1/L
24 -21 15 Oto-40 2 8 -lOtolO 0 6 -lOtoO
70 -53 18 -20 to-70 -32 18 -10 to -60 -2 4 -10 toO
‘Results are from six different healthy individuals.
Table 6. Effect of Storage at Room Temperature on Ca2 and pH in Uncentrifuged Heparinized Blood
from Patients In intensive Care1
niolIL pH
O.2h 2.2h O.2h 2.2 h
Moan 820 840 24 7.32 7.28 -0.039
SD 340 330 19 0.17 0.16 0.021
Range 0.29-1.16 1.34-1.16 0 to 50 7.00-7.55 6.96-7.50 0 to -0.08
= 11 samples from eight patients.
calcium in any sample after 2 h of storage at room tempera- gives the least change in pH and corrected ionized calcium
ture ranged from 0 to 50 (mean 24) pmol/L, and the changes after 70 h of storage at 4#{176}C. Nonetheless, we consistently
in pH ranged from 0 to -0.08 (mean 0.04) pH unit, both observed a 20 mo1/L bias in ionized calcium between serum
ranges slightly greater than those seen in the healthy from plain tubes and that from SST tubes (Table 1), appar-
individuals. ently because of the lower initial pH in samples from the
SS’T tubes. As shown in Table 3, some heparinized whole-
Discussion blood samples from patients in intensive care had slightly
Among the clinical uses of calcium measurements are greater changes in calcium and pH after storage at room
monitoring of patients in surgery or intensive care, daily temperature than did samples from healthy individuals,
monitoring of patients to maintain appropriate concentra- although the maximum change in ionized calcium for any
tions of calcium, and determinations for purposes of diagno- sample was only 25 umo1/L per hour.
sis. Although special collection and handling procedures for Our data from healthy volunteers and hospitalized pa-
ionized calcium may be economically justified for the rela- tients indicate that ionized calcium in serum is stable,
tively few patients in intensive care, they may be impracti- especially if stored at 4#{176}C,
whether the blood is centrifuged
cal for measurements on large numbers of other patients. or not. However, we emphasize several cautions: First,
Given the large number of total calcium measurements aerobic handling is not acceptable unless other means of pH
requested, more efficient collection and handling procedures correction, perhaps such as that incorporated into the Radi-
are necessary if ionized calcium becomes the predominant ometer ICA 1 display, are used. Second, because most of our
clinical measurement for calcium. studies involved healthy donors, we do not rule out the
The use of ordinary sodium heparin in plasma or whole possibility that samples from some patients may undergo
blood should be discouraged, because it decreases the values changes of pH that are not compatible with delays in
for ionized calcium. Calcium-titrated sodium heparin would processing. Finally, this apparent stability of ionizedcalci-
be a better choice when fast analyses are needed; further- um seems to be a dynamic process, such that the hydrogen
more, results obtained on samples so treated should agree cation and the lactate anion from the lactic acid offset the
with those from serum, the sample type used for most other effect of the other, respectively releasing and chelating
chemistry assays and which reportedly gives fewer prob- ionized calcium. Although doubling or tripling the concen-
lems with maintenance of the calcium electrodes (7) than tration of lactate in samples stored at 4#{176}C did not apprecia-
does plasma or whole blood. bly affect our measurements of ionized calcium, this may
Blood may remain uncentrifuged at room temperature for have been fortuitous for the samples we studied.
as long as 2 h or at 4#{176}C
for 24 to 70 h without appreciable If total calcium remains the calcium measurement in
change in the concentration of ionized calcium; use of SST greatest use, then special handling of a few samples for
tubes to keep serum and cells separated after centrifugation determinations of ionized calcium should present few prob-
CLINICAL CHEMISTRY, Vol. 30, No.4, 1984 555
lems. However, as instrumentation for ionized calcium tion with the ion-specific electrode, and factors affecting the results.
continues to improve, measurements of ionized calcium may Clin Chem 19, 565-574 (1973).
eventually displace total calcium, and more efficient proce- 4. Husdan H, L.eung M, Oreopoulos D, Rapaport A. Measurement
dures for blood collection and handling will be needed. of serum and plasma ionic calcium with the “Space-Stat 20 Ionized
Calcium Analyzer.” Clin Chem 23, 1175-1777 (1977).
Further work is needed to confirm conclusively that storage
of blood at room temperature for 2 h or at 4 #{176}C
for longer 5. Fogh-Andersen N. Ionized calcium analyzer with built-in pH
correction. Clin Chem 27, 1264-1267 (1981).
periods does not alter ionized calcium values by more than
6. Fogh-Andersen N, Christiansen TF, Komarmy L, Siggaard-
about 2%. Andersen 0. Measurement of free calcium ion in capillary blood and
serum. Clin Chem 24, 1545-1552 (1978).
7. Larsson L, Finnstrom U, Nilsson B, Ohman S. Evaluation of
Radiometer ICA 1 as a routine instrument for serum ionized
References calcium and its application for whole blood capillary samples from
1. Graham G, Burritt M. Preliminary report: AACC Ionized Calci- newborn infants. Scand J Clin Lab Invest 43 (Suppl 165),21-26
um Working Group on Reference Intervals. Clin Chem 29, 1187 (1983).
(1980). Abstract. 8. Pesce MA, Bodourian SH, Nicholson JF. Rapid kinetic measure-
2. Toffaletti J, Kirvan K. Spectrophotometric micro method for ment of lactate in plasma with a centrifugal analyzer. Gun Chem
measurement of dialyzable calcium by use of cresolphthalein com- 21,1932-1934 (1975).
plexone and continuous-flow analysis. Clin Chem 26,1562-1565 9. Wentz PE, Savory J, Cross RE. Improved method of measure-
(1980). ment of inorganic phosphate in serum with a centrifugal analyzer.
3. Ladenson J, Bowers GN. Free calciumin serum. I. Determina- Clin Chem 22, 257-260 (1976).
CLIN.CHEM. 30/4,556-559(1984)
Urea, Creatinine, and Glucose Determined in Plasma and Whole Blood by a
Differential pH Technique
M. Ripamonti, A. Mosca, E. Rovida, M. Luzzana, L Luzi, F. Ceriotti, F. Cottini, and L. Rossi-Bernardi
We report the conditions (buffer composition and enzyme Materials and Methods
activity) required for estimating three frequently determined
Instrumentation. pH was measured with a commercially
analytes-urea, glucose, and creatinine-by use of an im- available differential pH analyzer (Delpas CL; Kontron AG,
proved version of the differential pH apparatus previously Milan, Italy), an instrument similar in design to the home-
described (C/in Chem 29: 80-85, 1983). For each analyte, made instrument we previously described (2). Improved
we used only one specific enzyme, thus avoiding a chain of features consist of a thermostated stainless-steel block to
auxiliary and indicator reactions. The method requires about ensure a better temperature control of the two electrodes, a
a minute for each determination in undiluted plasma or whole 16-character alphanumeric display, a printer, and a key-
blood. board for parameter entry and instrument control. All
measurements here reported were obtained by use of this
apparatus at 23 #{176}C except for creatinine, which was mea-
We previously described (1,2) a new instrument, based on
sured at 37 #{176}C. An IL919 analyzer (Instrumentation Labora-
the differential measurement of pH, and illustrated its
tory, Milan, Italy) and IL-associated chemical procedures
application by the determination of glucose in plasma. We
were used as comparison methods for the determination of
believe that this pH technique can find interesting applica-
urea and creatinine. Computations were performed by an
tions in clinical chemistry. Indeed, the two more interesting
Altos ACS 8000/2 (Altos Computer Systems, Cuppertino,
advantages are that (a) the system automatically performs a
CA). The software was written in PASCAL high-level lan-
sample blank and (b) turbid solutions can be analyzed
guage.
directly. Moreover, many reactions lead to a change of pH in
the solution. The most relevant among them are: the Chemicals and solutions. Lyophilized jack-bean urease
(EC 3.5.1.5) was from Ames/Miles (Milan). A solution of it
oxidoreductase-catalyzed reactions involving NAD/NADH
was prepared by dissolving a suitable amount in 10 mL of
or NADP/NADPH interconversion; the reactions involving
0.1 mol/L KC1 and adjusting the pH to 7.50 with 0.1 mol/L
transfer of phosphate residue; reactions producing CO2 and
K2C03; 15 mL of glycerol was added as a stabilizing agent.
NH3; and reactions involving ester bond synthesis or cleav-
The final activity was 1440 kUIL. For each urea determina-
age. Clearly, a potentially wide range of analytes and
tion, we routinely used 11.2 U of urease. Typically, the
enzyme activities can be detected by this technique.
measurement was taken 20 s after the enzyme was added.
We now describe our further refinement of the technique
No significant loss of urease activity in solution was detect-
and its extension to determination of urea, creatinine, and
ed after six months at 4 #{176}C, but a 12% loss of activity was
glucose in plasma and whole blood.
observed after four days at room temperature.
Creatinine (99% pure) and creatinine iminohydrolase (EC
3.5.4.21, microbial source) were from Farmitalia Carlo
Dipartimento di Scienze e Tecnologie Biomediche, Centro di
Fisiologia del Lavoro Muscolare del CNR, do Ospedale S. Raffaele, Erba, Milan. The enzyme suspension was dialyzed against
University of Milan, Via Olgettina 60, 20132 Milan, Italy. 0.1 molIL KC1 solution containing NaN3, 1 g/L. The pH was
Received September 12, 1983; accepted January 5, 1984. then adjusted to 7.54 with 10 mmolIL NaOH, with continu-
556 CLINICALCHEMISTRY, Vol.30, No. 4, 1984
You might also like
- 553 FullDocument4 pages553 FullakintunjiNo ratings yet
- Inorganic Phosphorus and Potassium Are Putative Indicators of Delayed Separation of Whole BloodDocument6 pagesInorganic Phosphorus and Potassium Are Putative Indicators of Delayed Separation of Whole Bloodanon_837143581No ratings yet
- Original ArticleDocument8 pagesOriginal ArticleAshlea HunterNo ratings yet
- Plasma: Ifcc Transport Storage BloodDocument6 pagesPlasma: Ifcc Transport Storage BloodFalanta SandaNo ratings yet
- Temp of Blood During Delay ProcessDocument11 pagesTemp of Blood During Delay ProcessDwitaRiadiniNo ratings yet
- References: Effect of Urine PH, Storage Time, and Temperature On Stability of Catecholamines, Cortisol, and CreatinineDocument4 pagesReferences: Effect of Urine PH, Storage Time, and Temperature On Stability of Catecholamines, Cortisol, and CreatinineFitria Rizky AmaliaNo ratings yet
- The Preservation of Whole Blood: Max M. Strumia,, Miss Margaret Dolan, Miss Louise ColwellDocument6 pagesThe Preservation of Whole Blood: Max M. Strumia,, Miss Margaret Dolan, Miss Louise ColwellRevi NisaNo ratings yet
- 9 LeinoDocument4 pages9 LeinoLorena Ek MaciasNo ratings yet
- Comparative Erythrocytes Osmotic Fragility Test and Some Haematological Parameters in Hbaa and Hbss SubjectsDocument11 pagesComparative Erythrocytes Osmotic Fragility Test and Some Haematological Parameters in Hbaa and Hbss SubjectsvisiniNo ratings yet
- Plasma CalciumDocument4 pagesPlasma CalciumÁureo BarbosaNo ratings yet
- Effects of Storage Temperature, Storage Time, and Hemolysis On The-Manying Shi q1Document13 pagesEffects of Storage Temperature, Storage Time, and Hemolysis On The-Manying Shi q1rince noveliaNo ratings yet
- VIDAS miniVIDAS ServiceManual 31-01-2011 (1) - 2Document21 pagesVIDAS miniVIDAS ServiceManual 31-01-2011 (1) - 2metana90No ratings yet
- Advances in Medical SciencesDocument6 pagesAdvances in Medical SciencesMihaela-Alexandra PopNo ratings yet
- Leino Koivula 2009 Stability of Chemical and Immunochemical Analytes in Uncentrifuged Plasma SamplesDocument3 pagesLeino Koivula 2009 Stability of Chemical and Immunochemical Analytes in Uncentrifuged Plasma SamplestestNo ratings yet
- The Role of Organic Acid Analysis in The Diagnosis of Peroxisomal Biogenesis DisordersDocument4 pagesThe Role of Organic Acid Analysis in The Diagnosis of Peroxisomal Biogenesis DisorderssaranyaNo ratings yet
- Bioc416 PDFDocument53 pagesBioc416 PDFrJ100% (2)
- The Effect of Storage Conditions On Sample Stability in The Routine Clinical LaboratoryDocument5 pagesThe Effect of Storage Conditions On Sample Stability in The Routine Clinical LaboratorysidomoyoNo ratings yet
- 1 s2.0 S0009898117305223 MainDocument7 pages1 s2.0 S0009898117305223 MainsdadsaNo ratings yet
- NMAM Lead in Blood 8003Document4 pagesNMAM Lead in Blood 8003Auliya Kaisa SabatatanNo ratings yet
- Potassium Transport in The Acetylcholinesterase-Deficient Erythrocytes of Paroxysmal Nocturnal Hemoglobinuria (PNH)Document6 pagesPotassium Transport in The Acetylcholinesterase-Deficient Erythrocytes of Paroxysmal Nocturnal Hemoglobinuria (PNH)Buat DownloadNo ratings yet
- IndianJPatholOncol 7 4 625 630Document6 pagesIndianJPatholOncol 7 4 625 630Yaser MNo ratings yet
- Comparison of Blood Ethanol Stabilities in Different Storage PeriodsDocument7 pagesComparison of Blood Ethanol Stabilities in Different Storage PeriodsOlgui HepnarováNo ratings yet
- Calcium BookDocument28 pagesCalcium BookLucius33No ratings yet
- Delay in Specimen Processing-Major Source of Preanalytical Variation in Serum ElectrolytesDocument7 pagesDelay in Specimen Processing-Major Source of Preanalytical Variation in Serum ElectrolytesNitra NingtiyasNo ratings yet
- Treatment of Hyperkalemia: Something Old, Something New: Richard H. Sterns, Marvin Grieff and Paul L. BernsteinDocument9 pagesTreatment of Hyperkalemia: Something Old, Something New: Richard H. Sterns, Marvin Grieff and Paul L. BernsteinJaime CastilloNo ratings yet
- Acidbasephysiology1 170701101432Document25 pagesAcidbasephysiology1 170701101432Ro RyNo ratings yet
- WTTH - Inappetence & LethargyDocument3 pagesWTTH - Inappetence & LethargyCabinet VeterinarNo ratings yet
- Cardigan 2011Document5 pagesCardigan 2011MaulidaNo ratings yet
- 1 s2.0 S1043466697902179 MainDocument6 pages1 s2.0 S1043466697902179 MaintestNo ratings yet
- Too Many Normal Saline? Fluids in Various ConditionDocument26 pagesToo Many Normal Saline? Fluids in Various ConditionHandrian RahmanNo ratings yet
- s00604 007 0733 ZDocument6 pagess00604 007 0733 Zprakashjyoti0901No ratings yet
- JURNAL AOAC Penetapan Selenium Dengan AAS (Inggris)Document5 pagesJURNAL AOAC Penetapan Selenium Dengan AAS (Inggris)Altar NuriaNo ratings yet
- Long-Term Stability of Biomarkers of The Iron Status in Human Serum and PlasmaDocument5 pagesLong-Term Stability of Biomarkers of The Iron Status in Human Serum and PlasmatestNo ratings yet
- The Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine OsmolalityDocument7 pagesThe Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine Osmolalitysafdar aliNo ratings yet
- Clinical Chemistry: Presented by Alyazeed Hussein, BSCDocument43 pagesClinical Chemistry: Presented by Alyazeed Hussein, BSCMONFOLANo ratings yet
- DM Management HCHDocument1 pageDM Management HCHKelvinTMaikanaNo ratings yet
- 12 Bicarbonate, Calcium, Phosphate and MagnesiumDocument38 pages12 Bicarbonate, Calcium, Phosphate and MagnesiumFrances FranciscoNo ratings yet
- En Calcium (Ocpc)Document4 pagesEn Calcium (Ocpc)makjoe19No ratings yet
- Unit 8Document3 pagesUnit 804Cabanting, Mark Louie G.No ratings yet
- 626 FullDocument4 pages626 FullOmar ReynosoNo ratings yet
- Sickle Cell Anemia A Molecular Disease PDFDocument6 pagesSickle Cell Anemia A Molecular Disease PDFFayza RihastaraNo ratings yet
- Influence of Tail Versus Cardiac Sampling On Blood Glucose and Lipid Profiles in MiceDocument6 pagesInfluence of Tail Versus Cardiac Sampling On Blood Glucose and Lipid Profiles in MicePaul SimononNo ratings yet
- tmp6536 TMPDocument8 pagestmp6536 TMPFrontiersNo ratings yet
- VARIANT - HPLC - Retention - Time - As - A - Diagnostic - Tool - For - HemogDocument13 pagesVARIANT - HPLC - Retention - Time - As - A - Diagnostic - Tool - For - HemogUMMID WashimNo ratings yet
- Fluid Resuscitation: Ringer Lactate Versus Normal Saline-A Clinical StudyDocument4 pagesFluid Resuscitation: Ringer Lactate Versus Normal Saline-A Clinical StudyMirela Marina BlajNo ratings yet
- Anemia of Chronic Renal Failure in DogsDocument7 pagesAnemia of Chronic Renal Failure in Dogsfawzi badiNo ratings yet
- NCM 109 Skills Lab Day 13.1 Arterial Blood Gas Abg22Document38 pagesNCM 109 Skills Lab Day 13.1 Arterial Blood Gas Abg22Sheena Patricia ArasulaNo ratings yet
- Specimen Collection & Pre Analytical ErrorDocument4 pagesSpecimen Collection & Pre Analytical Errors8903082No ratings yet
- cASE STUDIES ANSWERDocument7 pagescASE STUDIES ANSWERNur Liyana0% (1)
- Study of StabilityDocument6 pagesStudy of Stabilitycrt79xqykpNo ratings yet
- The Influence of Blood Storage Time On The Potassium Level of Patients Receiving Packed Red Cell (PRC) Transfusion in Adam Malik General Hospital, MedanDocument6 pagesThe Influence of Blood Storage Time On The Potassium Level of Patients Receiving Packed Red Cell (PRC) Transfusion in Adam Malik General Hospital, MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- High-Throughput Characterization of Indices of Clinical Chemistry and HematologyDocument22 pagesHigh-Throughput Characterization of Indices of Clinical Chemistry and HematologyCheng Ho OcNo ratings yet
- Hendriani-G1C221023-Jasus Class ADocument2 pagesHendriani-G1C221023-Jasus Class AHendrianiNo ratings yet
- En Calcium Arsenazo Baosr6x117 UsDocument3 pagesEn Calcium Arsenazo Baosr6x117 UscarineNo ratings yet
- Dileep N. LOBO, Zeno STANGA, J. Alastair D. SIMPSON, John A. ANDERSON, Brian J. ROWLANDS and Simon P. ALLISONDocument7 pagesDileep N. LOBO, Zeno STANGA, J. Alastair D. SIMPSON, John A. ANDERSON, Brian J. ROWLANDS and Simon P. ALLISONMaria De Los AngelesNo ratings yet
- Evaluation of Serum Hyaluronic Acid Level and Hyaluronidase Activity in Acute and Chronic Hepatitis CDocument7 pagesEvaluation of Serum Hyaluronic Acid Level and Hyaluronidase Activity in Acute and Chronic Hepatitis CRaja SharmaNo ratings yet
- BiochemMed2019 01Document6 pagesBiochemMed2019 01iq_dianaNo ratings yet
- Ch6 Electrolytes and Blood GasesDocument53 pagesCh6 Electrolytes and Blood GasesLara MasriNo ratings yet
- Acid-Base and Electrolyte Handbook for Veterinary TechniciansFrom EverandAcid-Base and Electrolyte Handbook for Veterinary TechniciansAngela Randels-ThorpNo ratings yet
- Cah Kit Control c1 & c2 634986 (January 29-30, 2015)Document19 pagesCah Kit Control c1 & c2 634986 (January 29-30, 2015)Timothy John ValenciaNo ratings yet
- SportsDocument52 pagesSportsTimothy John ValenciaNo ratings yet
- 500BM PVs TJ Valencia 12 12 2017Document12 pages500BM PVs TJ Valencia 12 12 2017Timothy John ValenciaNo ratings yet
- 500BM PVs TJ Valencia 12 12 2017Document12 pages500BM PVs TJ Valencia 12 12 2017Timothy John ValenciaNo ratings yet
- Sir TJ Panget: Oo NgaDocument13 pagesSir TJ Panget: Oo NgaTimothy John ValenciaNo ratings yet
- SportsDocument52 pagesSportsTimothy John ValenciaNo ratings yet
- 500BM PVs TJ Valencia 12 12 2017Document12 pages500BM PVs TJ Valencia 12 12 2017Timothy John ValenciaNo ratings yet
- MinalungaoDocument1 pageMinalungaoTimothy John ValenciaNo ratings yet
- My HeartDocument3 pagesMy HeartTimothy John ValenciaNo ratings yet
- Cah Kit Control c1 & c2 634986 (January 29-30, 2015)Document19 pagesCah Kit Control c1 & c2 634986 (January 29-30, 2015)Timothy John ValenciaNo ratings yet
- Sir TJ Panget: Oo NgaDocument13 pagesSir TJ Panget: Oo NgaTimothy John ValenciaNo ratings yet
- 500BM PVs TJ Valencia 12 12 2017Document12 pages500BM PVs TJ Valencia 12 12 2017Timothy John ValenciaNo ratings yet
- Full Blood Chem: No. Examination Result (MG/DL) Multiplier Final ResultDocument3 pagesFull Blood Chem: No. Examination Result (MG/DL) Multiplier Final ResultTimothy John ValenciaNo ratings yet
- Types of MycosesDocument8 pagesTypes of MycosesTimothy John ValenciaNo ratings yet
- CPH ReflectionDocument1 pageCPH ReflectionTimothy John ValenciaNo ratings yet
- WWW - Studyguide.pk: AS Physics - Revision Notes Unit 2 - Electricity and Thermal PhysicsDocument3 pagesWWW - Studyguide.pk: AS Physics - Revision Notes Unit 2 - Electricity and Thermal PhysicsHany ElGezawyNo ratings yet
- ANSI-AWWA (American Water Works Association)Document1 pageANSI-AWWA (American Water Works Association)Vaniya GoelNo ratings yet
- E&DPlan 0506Document44 pagesE&DPlan 0506Farhan ShahNo ratings yet
- Alpha Amylase Production PDFDocument31 pagesAlpha Amylase Production PDFGaurav BangarhNo ratings yet
- NASA Facts The Planet VenusDocument8 pagesNASA Facts The Planet VenusBob AndrepontNo ratings yet
- Nanosilica Improves Recycled Concrete AggregatesDocument9 pagesNanosilica Improves Recycled Concrete AggregatesSanjeeva YedavalliNo ratings yet
- Odorcarb Ultra Media SDS (GHS v1.01)Document8 pagesOdorcarb Ultra Media SDS (GHS v1.01)jeanjean283No ratings yet
- Acids and Bases YMS X ALJDocument9 pagesAcids and Bases YMS X ALJFaqihah Syahindah Mohammed FiroozNo ratings yet
- Domain 1 MathematicsDocument129 pagesDomain 1 Mathematicsjyothish100% (2)
- PH4211 Statistical Mechanics: Problem Sheet 2Document4 pagesPH4211 Statistical Mechanics: Problem Sheet 2Roy VeseyNo ratings yet
- Essential Molecular BiologyDocument19 pagesEssential Molecular BiologySandra JelynNo ratings yet
- NEMA WC-71-1999-icea-71-1999icea-s-96-659-1999Document10 pagesNEMA WC-71-1999-icea-71-1999icea-s-96-659-1999jan carlos martinezNo ratings yet
- Sect 8 - Ref GalvadermDocument19 pagesSect 8 - Ref GalvadermamymonuskinNo ratings yet
- Concrete Society - Concrete Advice No 26 - RC Bund StructuresDocument3 pagesConcrete Society - Concrete Advice No 26 - RC Bund StructuresKarishma JuttunNo ratings yet
- Basic Flow MetersDocument3 pagesBasic Flow Metersladybuzz89No ratings yet
- Drug CalculationsDocument6 pagesDrug CalculationsLighto RyusakiNo ratings yet
- Prepartion of 4 Bromo 2 ChloroacetanildeDocument11 pagesPrepartion of 4 Bromo 2 ChloroacetanildeAmil Patel0% (1)
- Us 6796382 United States Patent 6,796,382 B2Document11 pagesUs 6796382 United States Patent 6,796,382 B2Daniel SullivanNo ratings yet
- MSDS HF - PV KPMDocument8 pagesMSDS HF - PV KPMPrabuEswarNo ratings yet
- Preparation of Tin TetraiodideDocument2 pagesPreparation of Tin Tetraiodidestudent_4_evaNo ratings yet
- Engineering MaterialsDocument16 pagesEngineering MaterialsYosef Ganang Jati NugrohoNo ratings yet
- The Public's Love Affair With Geodes: Rock MineralDocument3 pagesThe Public's Love Affair With Geodes: Rock MineralSerkan KocapinarNo ratings yet
- Sikacrete Fire Protection Mortar 201102Document12 pagesSikacrete Fire Protection Mortar 201102maximgh100% (1)
- Ambasador AntalisDocument136 pagesAmbasador AntalisNostalgia 80No ratings yet
- PumpsDocument33 pagesPumpsSamson HaykonNo ratings yet
- Chapter 5 FiltrationDocument26 pagesChapter 5 FiltrationRalph Evidente100% (1)
- The Soil. Physical, Chemical and Biological Properties: Cations/soils-GlossaryDocument13 pagesThe Soil. Physical, Chemical and Biological Properties: Cations/soils-GlossaryAr Chandra MauliNo ratings yet
- Introduction To Antibiotics: Mrs Natasha MahajanDocument17 pagesIntroduction To Antibiotics: Mrs Natasha Mahajannatasha jadhavNo ratings yet
- Asme WPS Demo PWHT PDFDocument3 pagesAsme WPS Demo PWHT PDFGanesh rohitNo ratings yet
- Automated Sorting of Polymer Flakes Fluorescence Labeling and Development of A Measurement System PrototypeDocument12 pagesAutomated Sorting of Polymer Flakes Fluorescence Labeling and Development of A Measurement System PrototypeSəkinə ƏliyevaNo ratings yet