Professional Documents
Culture Documents
Adrenergic Blockers
Uploaded by
A sisonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Adrenergic Blockers
Uploaded by
A sisonCopyright:
Available Formats
ADRENERGIC BLOCKERS
CLASSIFICATION (SEARCH PA Po)
ACTION: Adrenergic Blockers act by binding to adrenergic receptors, causing dilation of peripheral blood
vessels. Lowers peripheral resistance, resulting in decrease B/P.
USES: Adrenergic blockers are used for benign prostatic hyperplasia, pheochromocytoma, prevention of
tissues necrosis and sloughing associated with extravasation of IV vasopressors.
SIDE EFFECTS: The most common side effects are hypotension, tachycardia, nasal stuffiness, nausea,
vomiting and diarrhea.
CONTRAINDICATIONS: Hypersensitive reactions may occur, and allergies should be identifies before
these products are given. Patients with MI, coronary insufficiency, angina or other evidence of CAD
should not use these products.
PHARMACOKINETICS: onset, peak, and duration vary among products.
INTERACTIONS: Vasoconstrictive and hypertensive effects of epinephrine are antagonized by adrenergic
blockers.
Possible Nursing Diagnoses:
Risk for injury (adverse reactions)
Sleep deprivation
Ineffective tissue perfusion
Impaired Urinary Elimination
Nursing considerations
Assess:
Electrolytes: K, Na, CL, CO2
Weight daily, I and O
B/P lying, Standng before starting treatment, q4hr thereafter
Nausea, vomiting, diarrhea
Skin turgor, dryness of muscuos membranes for hydration status
Administer:
Starting with low dose, gradually increasing to prevent side effects
With food or milk for GI symptoms
Evaluate:
Therapeutic response: decreasded B/P, increased peripheral pulses
Teach patient/family:
To avoid alcoholic beverages
To report dizziness, palpitations,fainting
To change position slowly of fainting may occur
To take product exactly as prescribed
To avoid all OTC products (cough, cold, allergy) unless directed by prescriber
SELECTED GENERIC NAMES
Phentolamine
Silodosin
tamsulosin
PHENTOLAMINE (RX)
Fen-tole’a-meen
Func. Class: Anti-hypertensive
Chem. Class: a-Adrenergic blocker
Do not confuse
Phentolamine / phentermine
Action
a-Adrenergic blocker, binds to a-adrenergic receptors, dilating peripheral blood vessels, lowering
peripheral resistance, lowering blood pressure.
Uses
Hypertension; pheochromocytoma; prevention/treatment of dermal necrosis following extravasation of
norepinephrine, DOPamine, epinephrine
Unbalanced Uses:
Impotence, hypertensive crisis due to MAOIs, symphatomimetic amines, heart failure.
DOSAGE AND ROUTES
Treatment of hypertensive episodes in pheochromocytoma
adult: IM/IV 5mg, repeat if necessary
Child: IV 0.05-0.1 mg/kg/dose, repeat if necessary; max 5mg
Diagnosis of pheochromocytoma
Adult: IV 2.5mg; if negative, repeat with 5 mg IV.
Child: IV 0.1mg/kg IV
Treatment Necrosis
Adult: 5-10mg/10ml NS injected into area of norepinephrine extravasation within 12hr
Child: 0.1-0.2 mg/kg, max 5mg
Prevention of Necrosis
Adult: 10 mg/L of norepinephrine containing sol.
Child: IV 0.1-0.2 mg/kg, max 5mg
Left ventricular Heart failure (Unlabelled)
Adult: IV 0.17-0.4 mg/min
Erectile dysfunction (unlabelled)
Adult: PO 40-80mg
Hypertensive emergency due to MAOIs, sympathomimetic amines (unlabelled)
Adult: IV BOL 5-15 mg/ml
Pharmacokinetics:
Metabolized in the liver, excreted in urine
IM: Peak 15-20 min, duration 3-4 hr
IV: Peak 2 min, duration 10-15 min
Adverse effects
CNS: Dizziness, flushing, weakness, cerebrovascular spasm
CV: Hypotension, tachycardia, angina, dysrhythmias, MI
EENT: Nasal congestion
GI: Dry mouth, nausea, vomiting, diarrhea, abdominal pain
Nursing considerations
Assess:
Weight daily, input and output
Blood pressure lying, standing before starting treatment, q4hr after
Nausea, vomiting, diarrhea, edema in feet, legs daily; skin turgor, dryness of mucous
membranes for hydration status, postural hypotension, cardiac system: pulse, ECG
Administer:
Gum, frequent rinsing of mouth, or hard candy for dry mouth
With vasopressor available
After discontinuing all medication for 24 hr
Treatment during required bed rest, 1 hr after
o IV Route:
After diluting 5mg/1ml sterile H2O for inj; give 5mg or less/min; patient to remain
recumbent during administration
o Cont IV INF Route
Dilute 5-10 mg/500 ml D5W, titrate to patient response
10 mg/L may be added to norepinephrine in IV sol for prevention of dermal necrosis
Evaluate:
Therapeutic response: decreased BP
Teach patient/family:
That bed rest is required during treatment, 1 hr after
Nursing Diagnosis Plan of Action Intervention Rationale Evaluation
Fluid volume Monitor and Decrease in
deficit related to document vital circulating blood
diarrhea signs especially BP volume can cause
and HR. hypotension and
tachycardia.
Alteration in HR is
a compensatory
mechanism to
maintain cardiac
output.
Assess skin turgor Signs of
and oral mucous dehydration are
membranes for also detected
signs of through the skin.
dehydration.
Assess and color A normal urine
and amount of output is
urine. Report considered normal
urine output less if not less than
than 30 ml/hr for 30ml/hour.
2 consecutive Concentrated
hours. urine denotes fluid
defiit.
Monitor and Febrile states
document decrease bodily
temperature. fluids by
perspiration and
increased
respiration.
Monitor fluid Most fluid comes
status in relation into the body
to dietary intake. through drinking,
water in food, and
water formed by
oxidation of foods.
Urge the patient Oral fluid
to drink prescribed replacement is
amount of fluid. indicated for mild
fluid deficit and is
a cost-effective
method for
replacement
treatment.
Aid the patient if Dehydrated
he or she is unable patients may be
to eat without weak and unable
assistance, and to meet
encourage the prescribed intake
family or SO to independently.
assist with
feedings, as
necessary.
Emphasize Fluid deficit can
importance of oral cause a dry, sticky
hygiene. mouth. Attention
to mouth care
promotes interest
in drinking and
reduces
discomfort of dry
mucous
membranes.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Blood BankDocument92 pagesBlood BankDoc PreetiNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Suturing WorkshopDocument88 pagesSuturing WorkshopHamss AhmedNo ratings yet
- RCDSO Guidelines Implant Dentistry PDFDocument16 pagesRCDSO Guidelines Implant Dentistry PDFl4j0b9No ratings yet
- Ipratropium Bromide Plus SalbutamolDocument3 pagesIpratropium Bromide Plus SalbutamolA sison100% (1)
- Lung Cancer (Nursing Care)Document5 pagesLung Cancer (Nursing Care)heiyuNo ratings yet
- Equipment Devices and Procedures in The Intensive Care Unit PDFDocument16 pagesEquipment Devices and Procedures in The Intensive Care Unit PDFJena Rose ReyesNo ratings yet
- Uterine Prolapse Is Falling or Sliding of The Womb (Uterus) From Its Normal Position Into The Vaginal AreaDocument2 pagesUterine Prolapse Is Falling or Sliding of The Womb (Uterus) From Its Normal Position Into The Vaginal AreaA sisonNo ratings yet
- BasketballDocument1 pageBasketballA sisonNo ratings yet
- Volleyball Is A: Team Sport Summer Olympic Games Tokyo 1964 Complete Set of RulesDocument1 pageVolleyball Is A: Team Sport Summer Olympic Games Tokyo 1964 Complete Set of RulesA sisonNo ratings yet
- Vit K Drug Study PDFDocument2 pagesVit K Drug Study PDFA sisonNo ratings yet
- Post Partum Hemorrhage Nursing Care Plan PDFDocument2 pagesPost Partum Hemorrhage Nursing Care Plan PDFA sison100% (1)
- Uterine Prolapse Is Falling or Sliding of The Womb (Uterus) From Its Normal Position Into The Vaginal AreaDocument16 pagesUterine Prolapse Is Falling or Sliding of The Womb (Uterus) From Its Normal Position Into The Vaginal AreaA sisonNo ratings yet
- Qualitative Tests For Amino AcidsDocument15 pagesQualitative Tests For Amino AcidsA sisonNo ratings yet
- Abbreviation PharmaDocument1 pageAbbreviation PharmaA sisonNo ratings yet
- In Service Exam For Breast DR Paul BalisiDocument11 pagesIn Service Exam For Breast DR Paul BalisiAmiel Francisco ReyesNo ratings yet
- The Use of Oral Human Grade Ivermectin With Supplements Known As Immunomodulators For Treating Patients With COVID 19 Infections at HomeDocument16 pagesThe Use of Oral Human Grade Ivermectin With Supplements Known As Immunomodulators For Treating Patients With COVID 19 Infections at HomeAthenaeum Scientific PublishersNo ratings yet
- Grover 2020Document2 pagesGrover 2020Riza Agung NugrahaNo ratings yet
- Epidemiology NewDocument26 pagesEpidemiology NewBabita DhruwNo ratings yet
- PruBSN HEP+ BrochureDocument18 pagesPruBSN HEP+ BrochureMalik TaufiqNo ratings yet
- Deep Incisional SSIDocument2 pagesDeep Incisional SSIJan Michael BuragaNo ratings yet
- Reey8t.b. OsteomyelitisDocument52 pagesReey8t.b. Osteomyelitiskuku93No ratings yet
- Pathophysiology Precipitating Factors: Predisposing FactorsDocument2 pagesPathophysiology Precipitating Factors: Predisposing FactorsChristine Pialan SalimbagatNo ratings yet
- Introduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)Document52 pagesIntroduction To The Diagnostic Manual For Infancy and Early Childhood (DMIC)circlestretchNo ratings yet
- Review Questions-Association and BiasDocument12 pagesReview Questions-Association and BiassanjivdasNo ratings yet
- Lecture NotesDocument61 pagesLecture NotesTom Anthony Tonguia100% (1)
- Jadwal Pit (Uroginekologi Room)Document3 pagesJadwal Pit (Uroginekologi Room)Dwi Adi NugrohoNo ratings yet
- What Causes CancerDocument2 pagesWhat Causes CancerSilla, KyshiaNo ratings yet
- The Navarro Urine TestDocument3 pagesThe Navarro Urine TestSalvator2000100% (2)
- Basics of Fetal MRIDocument80 pagesBasics of Fetal MRIjturos2003No ratings yet
- Assessment Tool Clinical LabDocument1 pageAssessment Tool Clinical Labal gulNo ratings yet
- Treatment Aspects in Perioperative NursingDocument51 pagesTreatment Aspects in Perioperative NursingShibin Jacob100% (2)
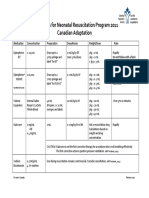
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- Nama: Rina Agustina Nim: 22018028 Unit 7 Promoting Hygiene 3 (Assissting With Elimination)Document3 pagesNama: Rina Agustina Nim: 22018028 Unit 7 Promoting Hygiene 3 (Assissting With Elimination)rinaNo ratings yet
- Jurnal 3Document7 pagesJurnal 3Richa FarellaNo ratings yet
- Drugs Used in Otology and Their FormulationsDocument4 pagesDrugs Used in Otology and Their FormulationsAnish RajNo ratings yet
- Content ServerDocument13 pagesContent ServerMairen RamirezNo ratings yet
- Endocrine SystemDocument61 pagesEndocrine Systemfanboiitsme20No ratings yet
- Congestive Heart FailureDocument13 pagesCongestive Heart FailureAgeng BudianantiNo ratings yet
- Burn GuidelineDocument7 pagesBurn GuidelinegreenNo ratings yet