Professional Documents
Culture Documents
Antimicrobial Susceptibility Test
Uploaded by
MATTHEW EARL MALUMAY100%(1)100% found this document useful (1 vote)
145 views4 pagesDiffusion Test Procedures
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDiffusion Test Procedures
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
145 views4 pagesAntimicrobial Susceptibility Test
Uploaded by
MATTHEW EARL MALUMAYDiffusion Test Procedures
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
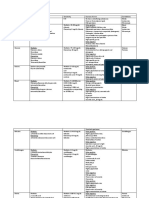
Exercise Number 5
Antimicrobial Susceptibility Test Diffusion Test Procedures
MATTHEW EARL G. MALUMAY | BATCH HILUSA 2022 | IDCM
OUTLINE Antimicrobial Susceptibility Testing
I. Antimicrobial Susceptibility Testing Antimicrobial Susceptibility Testing (AST)
II. Disc Diffusion Method Significant bacteria isolated from clinical
III. Resistance to Antimicrobial Drugs samples; guide the clinician on which
IV. Origin of Drug Resistance antimicrobial for patient management and
V. Cross Resistance generated susceptibility pattern data for
VI. Limitation of Drug Resistance suspected pathogen.
VII. CLINICAL IMPLICATIONS OF DRUG
Check the effectiveness of drug against
RESISTANCE: Staphylococci
microorganisms and to select the best drug
VIII. CLINICAL IMPLICATIONS OF DRUG
RESISTANCE: Gram-Negative Enteric that acts against the microorganisms.
Bacteria Right Microbe →Right Drug →Right Cure
IX. Antimicrobial Activity in Vitro
X. Factors Affecting Antimicrobial Activity Methods of Antimicrobial Susceptibility Testing:
Disc Diffusion Method
REFERENCE o Agar or solid media cultured with
lawn of isolate and impregnated with
Laboratory Manual in Microbiology and
antibiotic discs.
Parasitology Iloilo Doctors College of Medicine
o Plate is incubated for the organism to
Jawetz, Melnick and Adelberg’s Medical grow and antimicrobial to diffuse into
Microbiology 27th Edition Karen Carrol Steohen the agar.
Morse Timothy Mietzner Steve Miller Serial Dilution
o Organism is tested against a serial
increase in concentration of
antimicrobial in solid or broth media.
o Turbidity –sign of microbial growth on
broth medium and concentration of
antimicrobial without turbidity is
noted.
Combination of Increasing Amount of
Antibiotic impregnated in a Strip
o Least amount of antibiotic that exhibits
inhibition of growth is taken.
Disc Diffusion Method
Disc Diffusion Method by Kirby Bauer
principled after regression line graph, the
higher the antimicrobial concentration, the
smaller the zone of inhibition.
To generate a dynamically changing gradient
of antibiotic concentrations.
Inhibition Zone Edge –formed at a critical time
where the concentration of the antibiotic to inhibit
the organism before it reaches cell (critical) mass.
Factors Standardized on Disc Diffusion Method:
Depth of Agar
o Thick Agar →Slow Diffusion →Tested
Organism grows Faster
≈FALSE RESISTANT
Matthew Earl G. Malumay MD-SOON IDCM 1
Antimicrobial Susceptibility Test Diffusion Test Procedures
o 4 mm –standard depth of agar. entire surface of the agar plate to obtain
Concentration of Antibiotic uniform inoculum. Allow the plate to dry for
o Indicated in CLSI Manual and followed for 3-5 minutes (not more than 15 minutes).
regression graph. 3. Within 15 minutes, after the plates are
Inoculum Size inoculated, apply antibiotic impregnated discs
o 0.5 McFarland Nephelometer –standard to the surface of the inoculated plates with
inoculum size →1.5 x 108 bacterial sterile forceps. Gently press down all discs
suspension/mL. onto the agar with forceps or inoculating loop
Culture Media to ensure complete contact with the agar
o Mueller Hinton Agar [Recommended] surface. Special arrangements of the discs
o Sheep Blood Agar or Horse Blood should not be closer than 15 mm to edge of
[Fastidious Organisms] the plate and far enough to prevent
Control Strains overlapping zone of inhibition (at least 20 mm
o American Type Culture Collection (ATCC) apart).
–quality control testing of reagents, 4. Within 15 minutes after the discs are applied,
materials and supplied to conduct the plates are inverted and placed in the
microbial procedures. incubator at 35 degrees Celsius.
o Escherichia coli ATCC 25922 5. Within 16-18 hours of incubation, examine
o Pseudomonas aeruginosa ATCC 27853 the plates and measure to the nearest whole
o Staphylococcus aureus ATCC 29213 millimeter the zone of complete inhibition.
o Haemophilus influenza ATCC 49766
Resistance to Antimicrobial Drugs
PURPOSE: Sensitivity –zone of inhibition surrounding the
antibiotic disc.
To determine the sensitivity of commonly
isolated, rapidly growing pathogens, Resistance –no zone of inhibition surrounding the
Staphylococcus aureus and Enterobateriaceae antibiotic disc.
Family to antimicrobial agents.
Mechanisms of Microorganisms that exhibit Drug
To guide the clinician in selecting the best Resistance:
antibiotic agent for the patient. Microorganisms produce Enzymes that
destroy the active drug.
To control the use of inappropriate antibiotic in
o Staphylococci resistant to penicillin G
clinical practice.
produce B lactamase that destroys the
MATERIALS: drug.
Inoculating Needle/Loop o Gram (-) bacteria resistant to
Saline Solution aminoglycosides (by plasmid) produce
Antibiotic Disc adenylating, phosphorylating or
Turbidity Standard acetylating enzymes that destroy the
Cotton Swab Forceps drug.
Mueller Hinton Agar (MHA) Plates Microorganisms change Permeability to the
drug.
PROCEDURE: o Tetracyclines accumulate in susceptible
1. Fish isolated colonies using inoculating loop of bacteria but not in resistance bacteria.
morphological type suspended directly into o Streptococci have natural permeability
saline. Repeat this procedure until the barrier to aminoglycosides.
turbidity of suspension matches on standard o Resistance to Amikacin and
prepared by adding 0.5 mL if 0.048 Barium Aminoglycosides has lack of permeability
Chloride to 99.5 mL of 0.36 N Sulfuric Acid. to the drugs caused by an outer
2. Dip a sterile swab on applicator stick into membrane change that impairs active
standardized suspension. Remove excess fluid transport into the cell.
by pressing and rotating the swab against the Microorganisms develop an Altered Structural
side of the tube above the fluid level. Streak Target for the Drug.
the swab evenly in three directions over the o Erythromycin-resistant organisms have
altered receptor on 50S subunit of
Matthew Earl G. Malumay MD-SOON IDCM 2
Antimicrobial Susceptibility Test Diffusion Test Procedures
ribosome →Methylation of 23S ribosomal o Plasmids determine resistance to
RNA. penicillins and cephalosporins by carrying
o Resistance to penicillin and cephalosporins genes for the formation of β-lactamases.
has lost or altered PBPs.
Cross-Resistance
Microorganisms develop an Altered Metabolic
Microorganisms resistant to a certain drug may
Pathway that bypasses the reaction inhibited
also be resistant to other drugs that share a
by the drug.
mechanism of action, closely related chemically or
o Sulfonamide-resistant bacteria do not
have a similar mode of binding or action.
require PABA but mammalian cells require
preformed folic acid. Limitation of Drug Resistance
Microorganisms develop an Altered Enzyme Ways to Minimize the Emergence of Drug
that can still perform its metabolic function Resistance:
but is much less affected by the drug. Maintaining sufficiently high levels of the drug
o Dihydrofolic acid reductase is inhibited in in tissues to inhibit original population and
trimethoprim-resistant bacteria less first-step mutants.
efficiently than in trimethoprim-susceptible Administering two drugs that do not give
bacteria. cross-resistance →delays the emergence of
Microorganisms can develop Efflux Pumps mutants resistant to other drug.
that transport the antibiotics out of the cell. Avoid exposure of microorganisms to valuable
o Gram (+) and (-) developed efflux pumps drug by limiting its use.
for tetracyclines, macrolides,
fluoroquinolone and B-lactam agents. CLINICAL IMPLICATIONS OF
DRUG RESISTANCE: Staphylococci
Resistance to Antimicrobial Drugs Most staphylococci were susceptible to penicillin
Nongenetic Origin of Drug Resistance G → β-lactamase producers → resistant to
o Active replication of bacteria is required penicillin G.
for antibacterial drug actions.
Vancomycin –major drug for treatment of MRSA
o Consequently, microorganisms that are
infections but recovery of isolates with
metabolically inactive (nonmultiplying) are
intermediate resistance and reports of several
phenotypically resistant to drugs.
cases of high-level resistance to vancomycin have
o Microorganisms lose specific target
spurred the search for newer agents.
structure for a drug for several
generations and be resistant. Newer Agents with Activity against MRSA:
o Microorganisms infect the host at sites Daptomycin
where antimicrobials are excluded or are Linezolid
not active. Quinupristin–Dalfopristin
Genetic Origin of Drug Resistance Ceftaroline (novel cephalosporin agent)
o Drug-resistant microbes emerge as a
result of genetic change and subsequent Sensitive (Staphylococcus aureus):
selection processes by antimicrobial drugs. Cefuroxime
Chromosomal Resistance Ciprofloxacin
o Spontaneous mutation in a locus that Clindamycin
controls susceptibility to a given PiperacillinTazobactam
antimicrobial drug. Ampicillin
o Chromosomal mutants are resistant by Levofloxacin
virtue of change in structural receptor for Nitrofurantoin
a drug. Resistant (Staphylococcus aureus):
Extrachromosomal Resistance Nalidixic Acid
o Plasmids –extrachromosomal genetic
elements; carry genes for resistance to
antimicrobial drugs →control the
formation of enzymes capable of
destroying antimicrobial drugs.
Matthew Earl G. Malumay MD-SOON IDCM 3
Antimicrobial Susceptibility Test Diffusion Test Procedures
CLINICAL IMPLICATIONS
OF RUG RESISTANCE:
Gram-Negative Enteric Bacteria
Most drug resistance in enteric bacteria is
attributable to widespread transmission of
resistance plasmids.
Half the strains of Shigella species are now
resistant to multiple drugs.
Salmonellae have also developed resistance to
tetracyclines incorporated into animal feeds.
A clone of Salmonella serotype Typhimurium
phage type DT104 emerged and spread globally
which is resistant to ampicillin, chloramphenicol,
streptomycin, sulfonamides and tetracycline.
Plasmids carrying drug resistance genes occur in
gram-negative bacteria of normal gut microbiota.
Abundant Use of Antimicrobial Drugs →
Suppression of drug-susceptible organisms in gut
microbiota →Favors persistence and growth of
drug-resistant bacteria (Enterobacter, Klebsiella,
Proteus, Pseudomonas and Serratia species and
fungi).
Antimicrobial Activity in Vitro
Antimicrobial Activity in Vitro:
Potency of Antibacterial Agent in Solution
Concentration in Body Fluids or Tissues
Susceptibility of Microorganism to Known
Concentrations of the Drug
Factors Affecting Antimicrobial Activity
pH of Environment
Components of Medium
Stability of Drug
Size of Inoculum
Length of Incubation
Metabolic Activity of Microorganisms
Sensitive (Escherichia coli):
Cefuroxime
Resistant (Escherichia coli):
Nalidixic Acid
Tetracycline
Clindamycin
Trimethoprim Sulfamethoxazole
Matthew Earl G. Malumay MD-SOON IDCM 4
You might also like
- The Pyridine Nucleotide CoenzymesFrom EverandThe Pyridine Nucleotide CoenzymesJohannes EverseNo ratings yet
- Antimicrobial Susceptibilty TestingDocument47 pagesAntimicrobial Susceptibilty TestingpixholicNo ratings yet
- Microbiology LAB 7Document3 pagesMicrobiology LAB 7jqtdNo ratings yet
- 2.13.08 Cold Agglutinin RogersDocument27 pages2.13.08 Cold Agglutinin RogersJessica StewartNo ratings yet
- Immunology & Serology Week 1Document2 pagesImmunology & Serology Week 1Romie SolacitoNo ratings yet
- Virulence Factors of Pathogenic Bacteria PDFDocument9 pagesVirulence Factors of Pathogenic Bacteria PDFSafira Najwa ElzamNo ratings yet
- IMH Laboratory ManualDocument56 pagesIMH Laboratory ManualHaniya KhanNo ratings yet
- Count the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLDocument81 pagesCount the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLAris ResurreccionNo ratings yet
- Tests For Dengue GROUP 3Document22 pagesTests For Dengue GROUP 3chocoholic potchiNo ratings yet
- Mycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceDocument59 pagesMycology: Rochelle D. Darlucio-Yabut, RMT, MPH Our Lady of Fatima University College of Medical Laboratory ScienceClaire GonoNo ratings yet
- BSC Licensure Sample QuestionsDocument144 pagesBSC Licensure Sample QuestionsSAMMY0% (1)
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- Laboratory Safety and Microscopy Principles for BACT211Document86 pagesLaboratory Safety and Microscopy Principles for BACT211kurotsukki todorokiNo ratings yet
- Chapter 024Document49 pagesChapter 024Gerald John PazNo ratings yet
- Hema 2 Reviewer (Midterms)Document20 pagesHema 2 Reviewer (Midterms)Rachel Marie M. Gania100% (1)
- Immuno Sero CompleteDocument33 pagesImmuno Sero CompleteAngela ReyesNo ratings yet
- 20 MycobacteriaDocument47 pages20 MycobacteriaStephen Jao Ayala UjanoNo ratings yet
- CH 10 Precipitation and AgglutinationDocument17 pagesCH 10 Precipitation and AgglutinationFedz FederisoNo ratings yet
- CNS Microbiology MeningitisDocument26 pagesCNS Microbiology MeningitisSaransh GhimireNo ratings yet
- Lecture 6 - Microbial GeneticsDocument26 pagesLecture 6 - Microbial Geneticsapi-3703352100% (1)
- Antigens: Substances Recognized by Immune CellsDocument11 pagesAntigens: Substances Recognized by Immune CellsAnushka Sharma0% (1)
- Chapter 002Document68 pagesChapter 002Gerald John PazNo ratings yet
- 4-Microbiology & ParasitologyDocument2 pages4-Microbiology & ParasitologyIbrahimFikry100% (1)
- Microbiology Revision E6.5Document132 pagesMicrobiology Revision E6.5massprithiv58No ratings yet
- CampylobacterDocument2 pagesCampylobactersarguss14No ratings yet
- DNA to Cells: A Brief History of CytogeneticsDocument5 pagesDNA to Cells: A Brief History of CytogeneticsRomie SolacitoNo ratings yet
- Microbiology 15 Campylobacter, Vibrio Etc 431-449Document18 pagesMicrobiology 15 Campylobacter, Vibrio Etc 431-449JenNo ratings yet
- Introduction To Viruses 2Document32 pagesIntroduction To Viruses 2mega kharisma kusumawarniNo ratings yet
- Mycobacteria: Nocardia, Rhodococcus, Tsukamurella and GordoniaDocument7 pagesMycobacteria: Nocardia, Rhodococcus, Tsukamurella and Gordonia20C – Gorospe, Rhai Chezka V.No ratings yet
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDocument4 pagesLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNo ratings yet
- Clinical Chemistry II - EnzymologyDocument9 pagesClinical Chemistry II - EnzymologyWynlor AbarcaNo ratings yet
- Immunology and Serology Lab IntroductionDocument10 pagesImmunology and Serology Lab IntroductionAldren Beliber100% (1)
- Gram Negative Cocci (Lecture Notes)Document5 pagesGram Negative Cocci (Lecture Notes)Dayledaniel Sorveto100% (1)
- CC 2 Lab CompreDocument81 pagesCC 2 Lab CompreLyra Dennise LlidoNo ratings yet
- MUST To KNOW in Histopathology1 PDFDocument34 pagesMUST To KNOW in Histopathology1 PDFEdel Gannaban BinasoyNo ratings yet
- Kirby-Bauer Disc Diffusion Method Antibiotic Susceptibility Testing Skill Based LearningDocument59 pagesKirby-Bauer Disc Diffusion Method Antibiotic Susceptibility Testing Skill Based Learningtummalapalli venkateswara rao100% (1)
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Document6 pages(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNo ratings yet
- Parasitology Lecture OverviewDocument17 pagesParasitology Lecture Overviewlouie100% (1)
- Laboratory Activity 10: Osmotic Fragility Test (Oft)Document27 pagesLaboratory Activity 10: Osmotic Fragility Test (Oft)Marie LlanesNo ratings yet
- 3.2 Acid Fast StainingDocument26 pages3.2 Acid Fast StainingMiguel CuevasNo ratings yet
- Must To Know in Medical Technology Laws EthicsDocument2 pagesMust To Know in Medical Technology Laws EthicsZhiddah JapzonNo ratings yet
- Minimal Inhibitory Concentration TestDocument26 pagesMinimal Inhibitory Concentration TestZandhika Alfi PratamaNo ratings yet
- Agents of Mycoses Identification and CharacteristicsDocument44 pagesAgents of Mycoses Identification and CharacteristicsRia AlcantaraNo ratings yet
- Clinical MicrosDocument28 pagesClinical MicrosKristine Jamella Maris NaragNo ratings yet
- (Trans) Chapter 16: Anemias - Red Blood Cell Morphology and Approach To DiagnosisDocument4 pages(Trans) Chapter 16: Anemias - Red Blood Cell Morphology and Approach To Diagnosisgotvelvet world dominationNo ratings yet
- Antigen and Its PropertiesDocument20 pagesAntigen and Its Propertiestusharpremin92% (12)
- Midterm ParasitologyDocument18 pagesMidterm ParasitologyAngelic AngelesNo ratings yet
- Clinical Instrumentation, MLT 2760, BCC, EXAM 01Document5 pagesClinical Instrumentation, MLT 2760, BCC, EXAM 01alphacetaNo ratings yet
- DermatophytesDocument1 pageDermatophytesKoo ThaNo ratings yet
- Bacterial and Viral GeneticsDocument52 pagesBacterial and Viral GeneticsPradeep Tomar100% (1)
- Micro para OSCE For YL6 BacteriaDocument2 pagesMicro para OSCE For YL6 Bacteriagzldiwa100% (1)
- Molbio HandoutDocument29 pagesMolbio HandoutHazel FlorentinoNo ratings yet
- Family of StreptococcaceaeDocument10 pagesFamily of StreptococcaceaeLovely B. AlipatNo ratings yet
- Lecture Notes BacteriologyDocument133 pagesLecture Notes BacteriologyLovely B. AlipatNo ratings yet
- Introduction to the Characteristics of FungiDocument32 pagesIntroduction to the Characteristics of FungiAnonymousNo ratings yet
- Hypersensitivity: by Yundzir FurqanDocument18 pagesHypersensitivity: by Yundzir FurqanFuЯqanFriesNo ratings yet
- Bacterial Culture Media: classification, types and usesDocument10 pagesBacterial Culture Media: classification, types and usesnosila_oz854No ratings yet
- Culture and Sensitivity-1Document21 pagesCulture and Sensitivity-1lalemchanie16No ratings yet
- Antibiotic Sensitivity TestingDocument8 pagesAntibiotic Sensitivity TestingHaseeba KhanNo ratings yet
- Antibiotic Sensitivity TestDocument10 pagesAntibiotic Sensitivity TestJ.A. LauronNo ratings yet
- Surgery ParathyroidDocument11 pagesSurgery ParathyroidMATTHEW EARL MALUMAYNo ratings yet
- Surgery Systemic Response to InjuryDocument11 pagesSurgery Systemic Response to InjuryMATTHEW EARL MALUMAYNo ratings yet
- Surgery Systemic Response to InjuryDocument11 pagesSurgery Systemic Response to InjuryMATTHEW EARL MALUMAYNo ratings yet
- Surgery PancreasDocument11 pagesSurgery PancreasMATTHEW EARL MALUMAYNo ratings yet
- Legal Medicine by Pedro SolisDocument792 pagesLegal Medicine by Pedro SolisNLainie Omar100% (3)
- Hemostasis-09 20 2019Document9 pagesHemostasis-09 20 2019MATTHEW EARL MALUMAYNo ratings yet
- Cutaneous Manifestations of Juvenile Onset Lupus Erythematosus: A Clinical StudyDocument5 pagesCutaneous Manifestations of Juvenile Onset Lupus Erythematosus: A Clinical StudyMaya SusantiNo ratings yet
- Temporary Nursing Staff - Cost and Quality Issues: OriginalresearchDocument10 pagesTemporary Nursing Staff - Cost and Quality Issues: OriginalresearchRobert CoffinNo ratings yet
- RAPID Resources for Lowering Fertility and Achieving Sustainable Development in the PhilippinesDocument41 pagesRAPID Resources for Lowering Fertility and Achieving Sustainable Development in the PhilippinesLeyrra Paclibar DiduloNo ratings yet
- Anacardium OrientaleDocument21 pagesAnacardium OrientaleAlexandre Funcia100% (1)
- Name:Muhammad Mustafa REG NO.12397 Assighment:Behavioural Science Topic:Conflict ManagementDocument15 pagesName:Muhammad Mustafa REG NO.12397 Assighment:Behavioural Science Topic:Conflict Managementmustafa wazirNo ratings yet
- Clinical Importance of Pittadhara KalaDocument61 pagesClinical Importance of Pittadhara KalaSwanand Avinash JoshiNo ratings yet
- Hog Restrainer SpecificationsDocument12 pagesHog Restrainer SpecificationsEdsel Jay RaperNo ratings yet
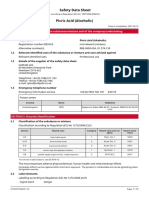
- Safety Data Sheet Picric Acid (Alcoholic)Document14 pagesSafety Data Sheet Picric Acid (Alcoholic)tarek aneesNo ratings yet
- Nur 111 Session 10 Sas 1Document9 pagesNur 111 Session 10 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Septoplasty: Information For Patients From Head and NeckDocument4 pagesSeptoplasty: Information For Patients From Head and NeckKris RNo ratings yet
- Cam CMD 2022 Presentation SepDocument156 pagesCam CMD 2022 Presentation SepLeBron JamesNo ratings yet
- Coe, & Vandegrift. 2015 (Youth Politics and Culture in Contemporary LA A Review)Document23 pagesCoe, & Vandegrift. 2015 (Youth Politics and Culture in Contemporary LA A Review)Alejandro MolinaNo ratings yet
- God's Cancer ParmacyDocument5 pagesGod's Cancer ParmacyNick BantoloNo ratings yet
- Capstone SolutionDocument1 pageCapstone Solutiondave magcawasNo ratings yet
- Roaduser and Vehicle CharacteristicsDocument62 pagesRoaduser and Vehicle CharacteristicsreashmapsNo ratings yet
- Cholera Toolkit 2013Document280 pagesCholera Toolkit 2013UNICEFNo ratings yet
- Jurnal Internasional BiofarmasetikaDocument9 pagesJurnal Internasional BiofarmasetikaHandriko DsNo ratings yet
- Esthetiques Spa 201005Document134 pagesEsthetiques Spa 201005Kristina0% (1)
- pm597 Week15 Capstone Project AqsahchoudharyDocument14 pagespm597 Week15 Capstone Project Aqsahchoudharyapi-560364244No ratings yet
- Majalah ISO Ed. 132 PDFDocument27 pagesMajalah ISO Ed. 132 PDFFranki Hari M100% (1)
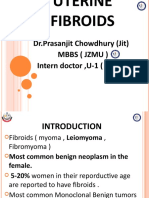
- Understanding Uterine FibroidsDocument52 pagesUnderstanding Uterine FibroidsDoctor JitNo ratings yet
- Endoscopy Gold Standard for Diagnosing Gastric MalignancyDocument2 pagesEndoscopy Gold Standard for Diagnosing Gastric MalignancyBenjie Balisi0% (1)
- Nutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Document16 pagesNutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Priscilia FooNo ratings yet
- Referred PainDocument9 pagesReferred PainElsa Tamara SaragihNo ratings yet
- Effect of Prone Positioning on Respiratory Rate and Oxygen Saturation in Infants with RDSDocument3 pagesEffect of Prone Positioning on Respiratory Rate and Oxygen Saturation in Infants with RDSAgustina VivoNo ratings yet
- Central Causes of DizzinessDocument9 pagesCentral Causes of DizzinessGLORIA MEDINA HERNANDEZNo ratings yet
- Infant Formula and Early Childhood CariesDocument5 pagesInfant Formula and Early Childhood Cariesmutiara hapkaNo ratings yet
- Acute Pain Questions - LathaDocument5 pagesAcute Pain Questions - LathaNishanth yedavalliNo ratings yet
- Nutritious Philippine Herbs Combat MalnutritionDocument5 pagesNutritious Philippine Herbs Combat MalnutritionPeter Pantazia0% (1)
- Abnoramal ECGDocument20 pagesAbnoramal ECGImmanuelNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)