Professional Documents
Culture Documents
Jurnal Hot Water Pancreatitis
Uploaded by
Diyah LestariCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Hot Water Pancreatitis
Uploaded by
Diyah LestariCopyright:
Available Formats
Iran J Public Health, Vol. 46, No.1, Jan 2017, pp.
136-138 Letter to the Editor
Applying Hot Compresses with Rhubarb and Mirabilite to
Reduce Pancreatic Leakage Occurrence in the Treatment of
Severe Acute Pancreatitis
Yunxia WANG 1, *Xinhui ZHANG 2, Chunying LI 1
1. Dept. of Hepatobiliary Surgery, Liaocheng People’s Hospital, Shandong, 252000, China
2. Dept. of Hemopathology, Liaocheng People’s Hospital, Shandong, 252000, China
*Corresponding Author: Email: li_chunying1@163.com
(Received 23 May 2016; accepted 18 Jun 2016)
Dear Editor-in-Chief
According to traditional Chinese medicine theory tract, lower intra-abdominal pressure, reduce en-
(1), pancreatitis is a “splenic precordial pain” or dotoxin-induced intestinal mucosa injuries, re-
“hypochondriac pain,” caused by excessive drink- duce the secretion of pancreatic amylase, elimi-
ing, gluttony, or gloomy mood, or secondary to nate inflammatory edema, and reduce IL-6 levels
biliary tract ascariasis, gallstones, and other dis- in the blood (4, 5). In contrast, mirabilite is salty,
eases. To date, no specific drugs have been able bitter, and cold in nature, usually processed into
to cure acute pancreatitis, and management is crystals. Because patients with pancreatitis gather
typically conservative. Traditional Chinese and heat in the Fu, which can obstruct of Fu Qi, using
Western medicine, when used in combination, external hot compress can eliminate heat, toxins,
can achieve good results. stagnation, and edema from extravasated blood.
We explored the effectiveness of nursing with the Moreover, it can quickly relieve the patients’ clin-
application of hot compresses of rhubarb and ical symptoms of abdominal pain and distension
mirabilite in reducing the occurrence of pancrea- (6-8).
tic leakage in the treatment of severe acute pan- As mentioned, patients in the intervention group
creatitis. We included 96 patients with severe were treated with traditional Chinese medicine
acute pancreatitis diagnosed at our hospital from internally and externally. First, 20 g of rhubarb
September 2013 to September 2015, and ran- was soaked in 200 ml of boiled water for 30 min
domly divided them into a control group (n = 47) until the water turned dark brown. The raw rhu-
and an intervention group (n = 49). The control barb was then filtered out and the remaining wa-
group received standard nursing care and thera- ter was cooled down to a temperature appropri-
py, while the intervention group received a com- ate for ingestion. Subsequently, 100 ml of the
bination of rhubarb infusion and hot compresses medicinal liquid was given to the patient through
with rhubarb and mirabilite. Rhubarb is cold in an indwelling gastric tube, which was then closed
nature; it prevents blood stasis, promotes heat for 1 h. This 100 ml dose was repeated two times
removal and purgation, and breaks stagnation. a day for a week. An additional 100 ml of the
These effects are pivotal for eliminating excess prepared medicinal liquid was given as retention
heat, enhancing indigestion, and stimulating me- enema. A lubricant was used to facilitate the in-
tabolism (2, 3). Rhubarb can clear the intestinal sertion of 25–30 cm of a one-time anal tube and
136 Available at: http://ijph.tums.ac.ir
Wang et al.: Applying Hot Compresses with Rhubarb and Mirabilite …
the liquid was injected using a syringe. Subse- were tested by ranked-sum tests. P < 0.05 indi-
quently, the tube was removed, and patient was cated statistical significance.
asked to lie on their back for 30 min. The times taken for abdominal distension, ab-
External treatment involved hot compressed with dominal pain, and blood and urinary amylase val-
rhubarb and mirabilite. A cotton compress was ues to normalize were significantly shorter in the
made into an elongated bag with a zipper in the intervention group compared with those in the
upper mouth and with wide strips sewn in the control group. By the end of the observation pe-
middle. Next, 500–1000 g of mirabilite was riod, the white blood cell count, C-reactive pro-
grounded into fine foam and fried until hot. This tein level, and interleukin-6 level were reduced in
mixture was then placed into the bag and applied both groups; however, the decline was more ob-
to the patient’s abdomen. We paid close attention vious in the intervention group (Table 1). In ad-
to the temperature in order to avoid skin burns. dition, the overall and full absorption efficiency
The abdominal skin was examined every other rates were significantly higher in the intervention
hour, and the bag was replaced every 24 h. This control group. Nursing satisfaction scores, as well
procedure was repeated until the patient reported as the rate and degree of satisfaction in the inter-
a relief in the abdominal pain and distension. vention group, were all higher than those in the
SPSS v19.0 (IBM Corp., Armonk, NY, USA) was control group (Table 2). The differences were
used for data analyses. Measurement data were statistically significant (P < 0.05).
expressed as mean ± standard deviation. For In conclusion, applying hot compresses with
comparison between groups we used indepen- rhubarb and mirabilite to nurse patients with se-
dent sample t-tests, while that within the groups vere acute pancreatitis can promote the absorp-
was by paired t-tests. Enumeration data are ex- tion of pancreatic exudates and shorten the re-
pressed by rate, and comparison between the covery time of patients, implying that this me-
groups was tested by χ2 tests, while ranked data thod is valuable to clinical practice.
Table 1: Comparison of serum inflammatory indicators
Group WBC count (109/L) CRP (mg/L) IL-6 (μg/L)
Before After Before After Before After
intervention intervention intervention intervention intervention intervention
Intervention 16.5 ± 2.2 6.6 ± 1.3 13.4 ± 2.6 3.8 ± 1.5 65.9 ± 12.5 21.5 ± 8.3
Control 16.3 ± 2.3 10.5 ± 2.0 13.2 ± 2.7 8.6 ± 1.6 62.3 ± 14.2 34.6 ± 7.6
t 0.242 5.326 0.421 5.766 0.632 5.447
P 0.637 0.023 0.567 0.018 0.527 0.021
Data shown as mean ± standard deviation
Abbreviations: CRP, C-reactive protein; IL-6, interleukin-6; WBC, white blood cell
Table 2: Comparison of satisfaction with nursing care
Group Cases Satisfaction degree Very Satisfied Unsatisfied Satisfaction
score satisfied rate
Intervention 49 8.6 ± 1.7 20 (40.8) 22 (44.9) 7 (14.3) 42 (85.7)
Control 47 6.4 ± 1.3 13 (27.7) 19 (40.4) 15 (31.9) 32 (68.1)
t 6.245 6.203 4.221
P 0.010 0.045 0.040
Data shown as cases (%) or as mean ± standard deviation
Available at: http://ijph.tums.ac.ir 137
Iran J Public Health, Vol. 46, No.1, Jan 2017, pp. 136-138
Acknowledgements 4. Gao Q, Liang N (2015). Integrated traditional
Chinese medicine improves acute pancrea-
The authors declare that there is no conflict of titis via the downregulation of PRSS1 and
SPINK1. Exp Ther Med, 9: 947-54.
interest. 5. Gao Z, Xu J, Sun D, Zhang R, Liang R,
Wang L, Fan R (2014). Traditional Chi-
References nese medicine, Qing Ying Tang, ameli-
orates the severity of acute lung injury in-
1. Ji CH, Tang CW, Feng WM, Bao Y, Yao LQ duced by severe acute pancreatitis in rats
(2016). A Chinese Herbal Decoction, via the upregulation of aquaporin-1. Exp
Huoxue Qingyi Decoction, Promotes Re- Ther Med, 8: 1819-24.
habilitation of Patients with Severe Acute 6. Chen WW, Wan MH, Lin ZQ, Yang XN,
Pancreatitis: A Retrospective Study. Evid Guo J, Wen Q, Xia Q (2013). [Health eco-
Based Complement Alternat Med, 2016: nomic evaluation of clinical pathway of
3456510. traditional Chinese medicine in the treat-
2. Yan X, Zhang Q, Feng F (2016). Chemical ment of mild acute pancreatitis]. Sichuan
profiling approach to evaluate the influ- Da Xue Xue Bao Yi Xue Ban, 44: 966-9.
ence of traditional and simplified decoc- 7. Xia Q, Deng LH (2013).[Hot issues on the
tion methods on the holistic quality of Da- treatment of severe acute pancreatitis by
Huang-Xiao-Shi decoction using high- Integrated Traditional Chinese and West-
performance liquid chromatography ern Medicine]. Sichuan Da Xue Xue Bao Yi
coupled with diode-array detection and Xue Ban, 44: 962-5.
time-of-flight mass spectrometry. J Sep Sci, 8. Wang L, Li Y, Ma Q, Liu Y, Rui YY, Xue P,
39: 1442-53. Zhou ZG (2011). Chaiqin Chengqi Decoc-
3. Watanabe Y, Ikarashi N, Satoh T, Ito K, tion decreases IL-6 levels in patients with
Ochiai W, Sugiyama K (2012). Inhibitory acute pancreatitis. J Zhejiang Univ Sci B,
effects of daiokanzoto (da-huang-gan-cao- 12:1034-40.
tang) on p-glycoprotein. Evid Based Com-
plement Alternat Med, 2012:361516.
138 Available at: http://ijph.tums.ac.ir
You might also like
- Patient ID Consent FSDocument39 pagesPatient ID Consent FSDiyah LestariNo ratings yet
- Nursing Always Events Patient Id 2Document37 pagesNursing Always Events Patient Id 2Diyah LestariNo ratings yet
- Ghcathways Gagal NafasdocxDocument2 pagesGhcathways Gagal NafasdocxDiyah LestariNo ratings yet
- WejgDocument7 pagesWejgDiyah LestariNo ratings yet
- 10 1164@rccm 201806-1034OC PDFDocument48 pages10 1164@rccm 201806-1034OC PDFReynaldo moralesNo ratings yet
- Materi Video Gizi SeimbangDocument3 pagesMateri Video Gizi SeimbangDiyah LestariNo ratings yet
- Book Self Concept Theory Research and Practice Self Research Center PDFDocument504 pagesBook Self Concept Theory Research and Practice Self Research Center PDFmademerlin92No ratings yet
- BingDocument1 pageBingDiyah LestariNo ratings yet
- BingDocument1 pageBingDiyah LestariNo ratings yet
- NEW Pregnancy Hypertension Chapter11Document18 pagesNEW Pregnancy Hypertension Chapter11Diyah LestariNo ratings yet
- NCBI Children Self ConceptDocument32 pagesNCBI Children Self ConceptDiyah LestariNo ratings yet
- Warna Indonesia PhotographyDocument13 pagesWarna Indonesia PhotographyDiyah LestariNo ratings yet
- PreeclampsiaDocument25 pagesPreeclampsiaDiyah LestariNo ratings yet
- Title Title: Some Text Goes Here Some Text Goes Here Some Text Goes Here Some Text Goes HereDocument2 pagesTitle Title: Some Text Goes Here Some Text Goes Here Some Text Goes Here Some Text Goes HereDiyah LestariNo ratings yet
- After Preeclampsia Postpartum Nutrition Handout For PET Foundation 4.27.18 1Document6 pagesAfter Preeclampsia Postpartum Nutrition Handout For PET Foundation 4.27.18 1Raven RosasNo ratings yet
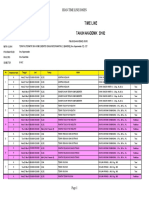
- Time Line: Tahun Akademik 20182Document3 pagesTime Line: Tahun Akademik 20182Diyah LestariNo ratings yet
- Materi Video Gizi SeimbangDocument3 pagesMateri Video Gizi SeimbangDiyah LestariNo ratings yet
- Pricelist Alvin Studio Januari 2019Document15 pagesPricelist Alvin Studio Januari 2019Diyah LestariNo ratings yet
- Pedoman Penyelenggaraan Pelayanan HCU Dan ICU Di RSDocument13 pagesPedoman Penyelenggaraan Pelayanan HCU Dan ICU Di RSDiyah LestariNo ratings yet
- 16.create 3 Step 3D BULB InfographicDocument1 page16.create 3 Step 3D BULB InfographicDiyah LestariNo ratings yet
- Some Ethical Conflicts in Emergency Care: Maria F Jime Nez-HerreraDocument14 pagesSome Ethical Conflicts in Emergency Care: Maria F Jime Nez-HerreraDiyah LestariNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- DOH STAR AWARDS 2019 APPLICATIONDocument2 pagesDOH STAR AWARDS 2019 APPLICATIONLeland C. DagoyNo ratings yet
- Acetaminophen AnalysisDocument2 pagesAcetaminophen AnalysisHastuti RahmasariiNo ratings yet
- MiradryDocument4 pagesMiradryBarakat AyoubNo ratings yet
- Vista General Products CatalogDocument52 pagesVista General Products CatalogVazgen AsatryanNo ratings yet
- Puerperal InfectionDocument28 pagesPuerperal InfectionAgus PratiwaNo ratings yet
- Phaco Chop: Roger F. Steinert, MDDocument9 pagesPhaco Chop: Roger F. Steinert, MDMichael CraneNo ratings yet
- Overrating or Dismissing The Value of Evidence-Based Practice+++Document7 pagesOverrating or Dismissing The Value of Evidence-Based Practice+++pig5evans30No ratings yet
- Obat Antituberkulosis dan Golongan KuinolonDocument3 pagesObat Antituberkulosis dan Golongan KuinolonIntan Eka PutriNo ratings yet
- Cyto B 21518 PDFDocument12 pagesCyto B 21518 PDFNurul Huda KowitaNo ratings yet
- DVT NotesDocument3 pagesDVT NotesTodd EvansNo ratings yet
- Drug Discovery & Development ProcessDocument57 pagesDrug Discovery & Development ProcessHazel Ruth Yara CastilloNo ratings yet
- Class II Correction for 11 Year Old BoyDocument17 pagesClass II Correction for 11 Year Old BoyMu'taz ArmanNo ratings yet
- Design BriefDocument1 pageDesign Briefapi-371764614No ratings yet
- Legal Medicine CRMTCS 6 GuideDocument7 pagesLegal Medicine CRMTCS 6 GuideRendell EusebioNo ratings yet
- VitiligoDocument11 pagesVitiligoNirmal BhowmickNo ratings yet
- 1891 Knowles Complete System of Personal InfluenceDocument154 pages1891 Knowles Complete System of Personal InfluenceJoão Marques Ferreira100% (3)
- Investigatory Project On Biology: Name: Josheen J Regno: Class: Xii BDocument27 pagesInvestigatory Project On Biology: Name: Josheen J Regno: Class: Xii BjimbombbsNo ratings yet
- Safe Work Method StatementDocument4 pagesSafe Work Method StatementShahed Facebook100% (1)
- Combiflam Tablets PI - 08072019Document13 pagesCombiflam Tablets PI - 08072019ArunNo ratings yet
- Dosha Sidhanta According To SushrutaDocument45 pagesDosha Sidhanta According To SushrutaDr ajayNo ratings yet
- ISUOG Basic Training: Gynecological Ultrasound: The BasicsDocument34 pagesISUOG Basic Training: Gynecological Ultrasound: The BasicsTheodoraAlinaNo ratings yet
- D&D5e - Ruins of Symbaroum - Gamemaster's ScreenDocument10 pagesD&D5e - Ruins of Symbaroum - Gamemaster's ScreenDesmond Wolf0% (2)
- MRCP Part 1 Self-Assessment - Medical Masterclass Questions and Explanatory AnswersDocument184 pagesMRCP Part 1 Self-Assessment - Medical Masterclass Questions and Explanatory Answerslionel786No ratings yet
- Hrana Pravila Umiriti Artritisa BolDocument7 pagesHrana Pravila Umiriti Artritisa BolNadrljanskiDusanNo ratings yet
- Breast AnatomyDocument15 pagesBreast Anatomyvarun100% (1)
- Multicultural Lesson PlanDocument6 pagesMulticultural Lesson Planapi-331853863No ratings yet
- Cost-Benefit Analysis Lesson PlanDocument2 pagesCost-Benefit Analysis Lesson PlanlaurahelenkingNo ratings yet
- Principles of sterilization and disinfectionDocument52 pagesPrinciples of sterilization and disinfectionRhomizal MazaliNo ratings yet
- 40 Famous Filipino Scientists and InventorsDocument14 pages40 Famous Filipino Scientists and InventorsAngel Dela PeñaNo ratings yet
- AP2 Unit 6 Exam Review CASDocument12 pagesAP2 Unit 6 Exam Review CASMarera DomnicNo ratings yet