Professional Documents
Culture Documents
Clinitek Novus
Uploaded by
Rennilia NitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinitek Novus
Uploaded by
Rennilia NitaCopyright:
Available Formats
CLINITEK Novus™
Automated Urine Chemistry Analyzer
CLINITEK NovusTM PRO 12 Urinalysis Cassette
Current Revision and Date 10844208 Rev. A, 2012-01
Product Name CLINITEK Novus PRO 12 Urinalysis Cassette REF 10634644
Materials Required but Not Provided CLINITEK Novus Calibrators REF 10697753
CLINITEK Novus Rinse Additive REF 10697754
Sample Types Urine
Minimum Sample Volume 2 mL
Intended Use
The CLINITEK NovusTM PRO 12 Urinalysis Cassette is designed to be used only with the
CLINITEK Novus Automated Urine Chemistry Analyzer.
The analyzer is a fully automated urinalysis instrument, intended for professional
in vitro diagnostic use in centralized laboratory locations.
The CLINITEK Novus PRO 12 Urinalysis Cassette is intended for the measurement of the
following parameters in urine:
albumin, bilirubin, blood (occult), creatinine, glucose, ketone (acetoacetic acid),
leukocytes, nitrite, pH, protein, urobilinogen, albumin-to-creatinine ratio, and protein-to-
creatinine ratio.
These measurements are used to assist diagnosis in the following areas:
• Carbohydrate metabolism (for example, diabetes mellitus)
• Kidney function
• Liver function
• Metabolic disorders
• Urinary tract infection
The CLINITEK Novus Automated Urine Chemistry Analyzer also reports color and the clarity of
the urine sample.
For in vitro diagnostic use.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
2 of 18
Summary and Explanation
The CLINITEK Novus System combines the principles of reflectance spectroscopy with a
convenient and efficient reagent format to provide qualitative or semi-quantitative results.
The CLINITEK Novus Automated Urine Chemistry analyzer electronically analyzes the color
and intensity of light reflected from a reacted test area. It also determines the specific gravity
and clarity of the urine sample and calculates the protein-to-creatinine ratio and the albumin-
to-creatinine ratio. The system reports the results in clinically meaningful units; refer to the
Tables of Results in the system operating instructions for the results that can be obtained.
Before loading the urinalysis cassette, read the CLINITEK Novus Operator’s Guide and the
CLINITEK Novus Calibration Kit package insert. All directions and procedures must be followed
exactly to obtain reliable test results. Read all instructions carefully before using the product.
The CLINITEK Novus PRO 12 Urinalysis Cassette has been determined to be nonhazardous
under the guidelines issued by OSHA in 29 CFR 1910.1200(d).
Principles of the Procedure
The following table describes the basis for each test pad:
Test Principles of the Procedure
Albumin This test is based on the dye-binding protein-error-of-indicators
principle, using a high affinity sulfonephthalein dye. At a constant pH,
the development of blue color is due to the presence of albumin.
Bilirubin This test is based on the coupling of bilirubin with diazotized
dichloroaniline in a strongly acid medium.
Blood This test is based on the peroxidase-like activity of hemoglobin, which
catalyzes the reaction of diisopropylbenzene dihydroperoxide and
3,3',5,5'-tetramethylbenzidine.
Creatinine This test is based on the peroxidase-like activity of a copper creatinine
complex that catalyzes the reaction of diisopropylbenzene
dihydroperoxide and 3,3',5,5'-tetramethylbenzidine.
Glucose This test is based on a double sequential enzyme reaction. One enzyme,
glucose oxidase, catalyzes the formation of gluconic acid and hydrogen
peroxide from the oxidation of glucose. A second enzyme, peroxidase,
catalyzes the oxidative coupling of 4-amino-antipyrine and 4-
methylcatechol by hydrogen peroxide.
Ketone This test is based on the reaction of nitroprusside with acetoacetic acid.
Leukocytes Granulocytic leukocytes contain esterases that catalyze the hydrolysis
of the derivatized pyrrole amino acid ester to liberate 3-hydroxy-5-
phenyl pyrrole. This pyrrole then reacts with a diazonium salt.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
3 of 18
Test Principles of the Procedure
Nitrite This test depends upon the conversion of nitrate (derived from the diet)
to nitrite by the action of Gram negative bacteria in the urine. At the
acid pH of the test area, nitrite in the urine reacts with ρ-arsanilic acid
to form a diazonium compound. This diazonium compound in turn
couples with 1,2,3,4-tetrahydrobenzo(h)quinolin-3-ol.
pH This test is based on a double indicator principle that gives a broad
range of colors covering the entire urinary pH range.
Protein This test is based on the protein-error-of-indicators principle. At a
constant pH, the presence of protein causes a change in the color of the
indicator.
Urobilinogen This test is based on the Ehrlich reaction in which
ρ-diethylaminobenzaldehyde in conjunction with a color enhancer
reacts with urobilinogen in a strongly acid medium.
Color This non-reactive white pad absorbs the sample to detect urine color.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
4 of 18
Reagents
The CLINITEK Novus PRO 12 Urinalysis Cassette contains sufficient materials to process
450 tests. Until ready to use, store the CLINITEK Novus PRO 12 Urinalysis Cassette unopened
at 15–30°C. The CLINITEK Novus PRO 12 Urinalysis Cassette must be used within 14 days after
loading it into the system.
The CLINITEK Novus PRO 12 Urinalysis Cassette contains the following components:
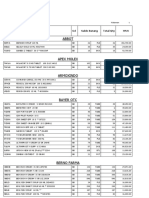
Test Description*
Albumin 1.9% w/w bis (3',3"-diiodo-4',4"-dihydroxy-5',5"-dinitrophenyl)-3,4,5,6-
tetrabromosulfonephthalein; 94.2% w/w buffer; 3.9% w/w nonreactive
ingredients
Bilirubin 0.4% w/w 2,4-dichloroaniline diazonium salt; 37.3% w/w buffer;
62.3 w/w nonreactive ingredients
Blood 6.8% w/w diisopropylbenzene dihydroperoxide;
4.0% w/w 3,3’,5,5’-tetramethylbenzidine; 48.0% w/w buffer;
41.2% w/w nonreactive ingredients
Creatinine 2.5% w/w copper sulfate; 4.5% w/w diisopropylbenzene dihydroperoxide;
2.0% w/w 3,3',5,5'-tetramethylbenzidine; 56.4% w/w buffer;
34.6% w/w nonreactive ingredients
Glucose 3.8% w/w glucose oxidase (bacterial); 0.3% w/w peroxidase (horseradish);
19.2% w/w 4-aminoantipyrine; 11.7% w/w 4-methylcatechol;
26.2% w/w buffer; 38.8% w/w nonreactive ingredients
Ketone 7.1% w/w sodium nitroprusside; 92.9% w/w buffer
Leukocytes 0.4% w/w derivatized pyrrole amino acid ester; 0.2% w/w diazonium salt;
40.9% w/w buffer; 58.5% w/w nonreactive ingredients
Nitrite 1.4% w/w ρ-arsanilic acid; 1.3% w/w 1,2,3,4-tetrahydrobenzo(h)quinolin-
3-ol; 10.8% w/w buffer; 86.5% w/w nonreactive ingredients
pH 0.2% w/w methyl red; 2.8% w/w bromothymol blue; 97.0% w/w
nonreactive ingredients
Protein 0.3% w/w tetrabromphenol blue; 97.3% w/w buffer; 2.4% w/w nonreactive
ingredients
Urobilinogen 0.2% w/w ρ-diethylaminobenzaldehyde; 99.8% w/w nonreactive
ingredients
*Based on dry weight at time of impregnation
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
5 of 18
Warnings and Precautions
Safety data sheets (MSDS/SDS) available on www.siemens.com/diagnostics.
Strict adherence to the following warnings and precautions is required when using the
CLINITEK Novus PRO 12 Urinalysis Cassette:
• Wear gloves when handling the test pads.
• Wear personal protective apparel, including disposable gloves, throughout the assay
procedure. Thoroughly wash hands after removing gloves, and dispose of gloves as
biohazardous waste.
• Do not eat, drink, smoke, or apply cosmetics in areas where reagents or samples are
handled.
• Do not pipet by mouth.
• Dispose of hazardous or biologically contaminated materials according to the practices of
your institution. Discard all materials in a safe and acceptable manner and in compliance
with prevailing regulatory requirements.
Running the Test
Opening the Urinalysis Cassette
CAUTION
Do not open a cassette if you do not intend to load the cassette immediately. Humidity
causes the test pads to deteriorate. For accurate test results, discard the cassette and open a
new one.
To open the cassette, follow the diagram provided on the cassette packaging:
1. Use the foil tab to peel the foil seal off the tray.
2. Remove the cassette from the tray.
3. Pull the shipping card out of the cassette.
CAUTION
Do not use test cards that fall out of the cassette. Dispose of them.
Loading the Urinalysis Cassette
To load the urinalysis cassette, follow the prompts on the system display:
Refer to the system operating instructions for complete information.
1. Select System > Load & Unload.
If a cassette is already loaded in the cassette compartment, the system confirms if you
want to unload the cassette.
2. Select Yes.
If a test card is on the card platform, the system ejects the card.
3. When prompted, open the system cover.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
6 of 18
4. Unlock the cassette compartment door by turning the lock counterclockwise.
5. Hold the cassette by the handle in the front, and slide the cassette toward you on the
cassette compartment rails.
6. Remove the cassette from the system and dispose of it.
7. To load the new cassette, hold the cassette by its handle in the front, and slide the
cassette into the cassette compartment using the rails as your guide.
8. Close the cassette compartment door and turn the lock clockwise to lock the door.
The system is ready to perform a test when the Home screen displays Ready in the
Status bar.
Cassette Storage and Handling
Store the unopened casette at room temperatures at 15–30°C and ensure that humidity does
not exceed 80%. Do not store in a refrigerator. Immediately after removing the urinalysis
cassette from the tray, load the cassette into the system.
The cassette must be used within 14 days after loading into the system. If the cassette is
exposed outside the tray or the closed cassette compartment of the system for longer than
15 minutes, the reagent may not yield satisfactory results. When the cassette is properly
stored in its sealed tray, it is stable until the expiration date.
Important Protection against exposure to light, heat, and ambient moisture is mandatory
to guard against altered reactivity.
Do not use the cassette if the foil lid or plastic tray is damaged. If the test results are
questionable or inconsistent with the expected findings, the following actions are
recommended:
• Confirm that the product is within the expiration date shown on the label.
• Check performance using known positive and negative control materials.
• Retest with fresh product.
If proper results are not obtained, please contact your local technical support provider.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
7 of 18
Sample Collection and Handling
CAUTION
Handle all samples as if they are capable of transmitting infection.
When handling patient samples, wear personal protective apparel, including disposable
gloves. Thoroughly wash hands after removing gloves, and dispose of gloves as
biohazardous waste.
Collect freshly-voided urine in a clean container and test it as soon as possible. A first-
morning specimen is preferred but random collections are acceptable. Test the urine within
2 hours after voiding, sooner if testing for bilirubin or urobilinogen, as these compounds are
very unstable when exposed to room temperature and light. If unable to test within the
recommended time, refrigerate the specimen immediately and let it return to room
temperature before testing. Work areas and specimen containers should always be free of
detergents and other contaminating substances.1
Use of preservatives of any kind is not recommended, as they may affect test results.
Chlorhexidine, which can be found in some skin cleansers or used as a preservative, may
cause elevated protein (and to a lesser extent, reduced bilirubin) test results. Urine collection
tubes containing chlorhexidine may also cause reduced blood and nitrite results. The user
should determine whether the use of such products is warranted.
Procedure
For detailed procedural information, refer to the system operating instructions or to the
online help system.
Materials Provided
REF Contents Number of Tests
10634644 CLINITEK Novus PRO 12 Urinalysis Cassette 450
Materials Required but not Provided
Note The following materials are required for use with the CLINITEK Novus PRO 12 Urinalysis
Cassette.
Item Description
REF 10697753 CLINITEK Novus Calibrators
REF 10697754 CLINITEK Novus Rinse Additive
REF 08787636 URIN-TEK® sample tubes and caps
Commercially available controls with at least 2 levels
5.25% bleach, unscented (0.5% sodium hypochlorite)
Distilled or deionized water for use with the Rinse Additive
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
8 of 18
Preparing the Samples
CAUTION
Test room temperature samples within 2 hours. Urine samples may deteriorate over time, if
testing for bilirubin or urobilinogen, test the samples sooner than 2 hours.
Note Do not test urine samples that are visibly mucoid or bloody. Also, a large amount of
foam on top of a sample might cause inaccurate results or a dispensing error.
To prepare the samples, follow these steps:
1. If samples are refrigerated, allow the samples to reach room temperature.
Test the samples within 2 hours after they reach room temperature.
2. Immediately before testing, mix each sample thoroughly; do not centrifuge.
No additional mixing is required if testing is done within 6 hours.
3. Pour at least 2 mL of each sample into an appropriately labeled URIN-TEK or similar tube.
4. Load the tubes of patient samples into the racks.
For more information on loading patient samples, refer to the system operating
instructions.
Performing Quality Control
Follow government regulations or accreditation requirements for quality control frequency.
Routinely test at least 2 levels (negative/low and positive) of an appropriate commercially
available control to confirm performance of the urinalysis cassette. Controls may also be
randomly placed in each batch of samples tested. Water should NOT be used as a negative
control. Each laboratory should establish its own goals for acceptable standards of
performance, and should question handling and testing procedures if these standards are
not met.
Refer to the system operating instructions for detailed information on calibrating the system
and performing a quality control test.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
9 of 18
Results
Results should always be interpreted in conjunction with the patient’s medical history, clinical
presentation, and other findings.
Expected Results
Expected values for the normal healthy population and the abnormal population are listed
below for each test.
Albumin: Protein in urine can be the result of urological and nephrological disorders.
Albumin has been established as an appropriate marker of glomerular damage. Albumin is
normally present in urine at concentrations of 0.5–2.0 mg/dL (0.005–0.02 g/L). Increased
albumin excretion (2–30 mg/dL or 0.02–0.3 g/L) is indicative of nephropathy in high-risk
groups.2–4
Bilirubin: Normal adult urine contains about 0.02 mg/dL (0.34 μmol/L) of bilirubin, which is
not detectable by even the most sensitive methods. Even trace amounts of bilirubin are
sufficiently abnormal to require further investigation.5 Since very small amounts of bilirubin
(≥ 0.1 mg/dL or 1.7 μmol/L) may be found in the earliest phases of liver disease, the user must
consider whether the sensitivity of CLINITEK Novus PRO 12 Reagent Cassette to bilirubin is
sufficient for the intended use.
Blood: Normally, no hemoglobin is detectable in urine (< 0.010 mg/dL or 100 μg/L; 3 RBC/μL).
Occult blood occurs in urine as intact erythrocytes and hemoglobin, which can occur during
urological, nephrological and bleeding disorders. Small amounts of blood
(0.030–0.065 mg hemoglobin/dL or 300–650 μg/L) are sufficiently abnormal to require
further investigation. The significance of the Trace reaction may vary among patients, and
clinical judgment is required for assessment in an individual case. Blood is often, but not
always, found in the urine of menstruating females.5,6
Creatinine: The normal creatinine concentration in adults is 0.6–2.0 g (5.3–8.8 mmol) of
creatinine per day. Random urine samples may have results that vary from 10–300 mg/dL
(0.9–26.5 mmol/L). Concentrated urine samples from dehydrated individuals or first morning
samples will typically have elevated concentrations (≥ 200 mg/dL or 17.7 mmol/L); diuresis
will typically result in lower concentrations (≥ 50 mg/dL or 4.4 mmol/L).5,7
Glucose: Small amounts of glucose (< 30 mg/dL or 1.67 mmol/L) are normally excreted by
the kidney. These amounts are usually below the sensitivity level of this test but on occasion
may produce a result between Negative and 100 mg/dL (5.5 mmol/L) that is interpreted as a
positive result. Results at the first positive level may be significantly abnormal if found
consistently.2,8
Ketone: Normally, no ketone is detectable in urine (up to 2 mg/dL or 0.2 mmol/L acetoacetic
acid). In ketoacidosis, starvation, or with other abnormalities of carbohydrate or lipid
metabolism, ketones may appear in urine at levels of 10 mg/dL (1.0 mmol/L) or higher before
serum acetoacetate levels are elevated. Clinical judgment is needed to determine the
significance of Trace results, which may occur during physiological stress conditions such as
fasting, pregnancy and frequent strenuous exercise.5
Leukocytes: Normal urine samples generally yield negative results. An increase in leukocytes
(≥ 10 leukocytes/μL) is an indication of pyuria and is found in nearly all diseases of the kidney
and urinary tract; however, pyuria may often be present in non-infective conditions.5 A result
of Small or greater is a useful indicator of infection. Trace results may be of questionable
clinical significance; however, Trace results observed repeatedly may be clinically significant.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
10 of 18
Nitrite: Normally no nitrite is detectable in urine. Many enteric gram-negative organisms give
positive results when their number is greater than 105/mL (0.075 mg/dL or 16.2 μmol/L nitrite
ion or greater).2,6
pH: The normal pH of urine can range from 4.6 to 8.0. Certain dietary conditions can produce
acid or alkaline urines, which can be useful in the treatment of some calculi.5
Protein: In normal urine, less than 150 mg (0.15 g) of total protein is excreted per day
(< 15 mg/dL or 0.15 g/L), while clinical proteinuria is indicated at greater than
500 mg (0.5 g) of protein per day. Positive results may also indicate tubular or overflow
proteinuria in the absence of any glomerular abnormality or proteins of renal origin that may
be excreted during infection. Urinary protein excretions can be temporarily elevated in the
absence of renal abnormality by strenuous exercise, orthostatic proteinuria, dehydration,
urinary tract infections, and acute illness with fever.5,6,9
Urobilinogen: Urobilinogen is normally present in urine at concentrations up to 1.0 mg/dL
(16 μmol/L or 1 Ehrlich Unit/dL). A result of 2.0 mg/dL (33 μmol/L) represents the transition
from normal to abnormal, and the patient and/or urine sample should be evaluated further
for hemolytic and hepatic disease. Evaluation of both the bilirubin and urobilinogen results
helps in the differential diagnosis of jaundice, as well as other liver and biliary disorders.5
Albumin-to-Creatinine Ratio: Albumin is normally present in urine at concentrations of less
than 30 mg albumin/g creatinine (3.4 mg albumin/mmol creatinine). Microalbuminuria is
indicated at a ratio result of 30–300 mg/g (3.4–33.9 mg/mmol) (Abnormal) and clinical
albuminuria at a ratio result of > 300 mg/g (> 33.9 mg/mmol) (High Abnormal).10
Protein-to-Creatinine Ratio: Clinical albuminuria is defined as an albumin-to-creatinine ratio
greater than 58 mg albumin/g creatinine; results above this level indicate declining renal
function.11 Clinical proteinuria is indicated at a ratio result of 300 mg protein/g creatinine
(33.9 mg/mmol).
Color: The normal color of urine is pale yellow to dark yellow.5
Limitations
Limitations given for the reagents include specific substances and conditions that may affect
the test results. As with all laboratory tests, definitive diagnostic or therapeutic decisions
should not be based on any single result or method.
Substances that cause abnormal urine color may affect the readability of reagent areas on
urinalysis reagent strips. These substances include visible levels of blood or bilirubin, drugs
containing dyes (for example, Pyridium, Azo Gantrisin, Azo Gantanol), nitrofurantoin
(Macrodantin, Furadantin), and riboflavin.
Protein: The presence of hemoglobin (≥ 5 mg/dL or 0.05 g/L) may cause elevated results.12
Creatinine: Urine containing blood (≥ 5 mg/dL or 0.05 g/L hemoglobin) or the presence of
cimetidine (Tagamet) may cause falsely elevated results.13
Protein-to-Creatinine Ratio: Both the protein and P:C ratio results should be considered
when making a decision about the clinical diagnosis or need for confirmatory testing.
Blood: Captopril (Capoten) and other compounds containing sulfhydryl groups may reduce
the sensitivity. Certain oxidizing contaminants, such as hypochlorite, may produce false
positive results. Microbial peroxidase associated with urinary tract infection may cause a false
positive reaction.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
11 of 18
Leukocytes: Elevated glucose concentrations (≥ 3 g/dL or 160 mmol/L) may cause decreased
test results. The presence of cephalexin (Keflex), cephalothin (Keflin), or high concentrations
of oxalic acid may also cause decreased test results. Tetracycline may cause decreased
reactivity, and high levels of the drug may cause a false negative reaction. Positive results
may occasionally be due to contamination of the specimen by vaginal discharge.
Nitrite: A negative result does not rule out significant bacteriuria. False negative results may
occur with shortened bladder incubation of the urine, absence of dietary nitrate, or the
presence of nonreductive pathological microbes. The presence of colored precipitates may
cause a false positive result.
Glucose: Urine samples with a pH of 9.0 and greater will cause falsely elevated glucose
results.
Ketone: False Trace results may occur with highly pigmented urine specimens or those
containing large amounts of levodopa metabolites. Compounds that contain sulfhydryl
groups, such as mesna (2-mercaptoethane sulfonic acid) and captopril, may cause false
positive results or an atypical color reaction.
pH: Bacterial growth by certain organisms in a specimen may cause a marked alkaline shift
(pH > 8.0), usually because of urea conversion to ammonia.
Bilirubin: Indican (indoxyl sulfate) can produce a yellow-orange to red color response that
may interfere with the interpretation of a negative or positive reading. Metabolites of
etodolac (Lodine) may cause false positive or atypical results. Atypical colors may indicate the
presence of bile pigment abnormalities and the urine specimen should be tested further.
Urobilinogen: The reagent area may react with interfering substances known to react with
Ehrlich’s reagent, such as ρ-aminosalicylic acid and sulfonamides. False negative results may
be obtained if formalin is present. The test is not a reliable method for the detection of
porphobilinogen.
Color: Because of the inherent differences between the perception of the human eye and the
optical system of the instrument, there may be differences between the color that is
perceived visually and that is reported by the instrument, especially when there are low levels
of a color present.
Performance Characteristics
Performance characteristics of the CLINITEK Novus PRO 12 Reagent Cassette are based on
clinical and analytical studies and depend upon several factors, including the presence or
absence of inhibitory and matrix factors typically found in urine. Each result represents a
range of values. Because of specimen and reading variability, specimens with analyte
concentrations that fall between nominal levels may give results at either level. Results at
levels greater than the second positive level for the glucose, protein, ketone, and
urobilinogen tests will usually be within one level of the true concentration.
Albumin: The test can accurately and specifically determine albumin. A strip result of
15 mg/dL (0.15 g/L) is indicative of clinical albuminuria. The test is not affected by other
proteins at concentrations at least nine times greater than the excretion rate considered to be
abnormal.12,13
Protein: The test is more sensitive to albumin than to globulin, hemoglobin, Bence-Jones
protein, or mucoprotein, which are generally detected at levels of 60 mg/dL (0.6 g/L) or
higher;12 a negative result does not rule out the presence of these other proteins.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
12 of 18
Creatinine: The test will detect creatinine in concentrations as low as 10 mg/dL (0.9 mmol/L)
or as high as 300 mg/dL (26.5 mmol/L). The absence of creatinine in a specimen cannot be
determined.
Protein-to-Creatinine Ratio: Use of the protein-to-creatinine ratio can assist in the diagnosis
of kidney function by minimizing the impact of changes in the protein result due to exercise,
diuresis and urine concentration.7,9 The ratio improves the results for single-void specimens
compared to timed specimens in the discrimination of normal and abnormal levels of protein.
Abnormal ratio results with the CLINITEK Novus correspond to values of
≥ 80 mg albumin/g creatinine (9.0 mg/mmol) or ≥ 300 mg protein/g creatinine
(26.5 mmol/L).
A ratio result of P Norm : C Dil is reported when the protein result is below the sensitivity
limits and the creatinine result is 10 mg/dL (0.9 mmol/L). In this case, consider testing a new
specimen, preferably a first morning collection, for greater confidence in the result. Very low
creatinine results can be caused by adulteration of the urine specimen or by severe renal
failure.14,15
Blood: The test is equally sensitive to myoglobin as to hemoglobin. This test complements
the microscopic examination; a hemoglobin concentration of 0.015–0.062 mg/dL
(150–620 μg/L) is approximately equivalent to 5–20 intact red blood cells per microliter.
Leukocytes: Leukocyte esterase is a reliable indicator of leukocytes in urine.5 A positive
reaction (Small or greater) may be regarded as a positive indication of leukocytes in urine.
Nitrite: The test is specific for nitrite and will not react with any other substance normally
excreted in urine. Nitrite concentration during infection increases with the length of time the
urine specimen is retained in the bladder prior to collection. A minimum of 4 hours of bladder
incubation significantly increases the likelihood of obtaining a positive result.
Glucose: The test is specific for glucose; no substance excreted in urine other than glucose is
known to give a positive result. Ketone bodies and nitrite do not interfere with test results.
This test may be used to determine whether the reducing substance found in urine is glucose.
Ketone: The test reacts with acetoacetic acid in urine. It does not react with acetone or
β-hydroxybutyric acid.
pH: The pH reagent area measures pH values from 5–9. The pH readings are not affected by
variations in the urinary buffer concentration.
Bilirubin: The test is specific for bilirubin and will not react with any other substance normally
excreted in urine.
Urobilinogen: This reagent area will detect urobilinogen in concentrations as low as
0.2 mg/dL (3.2 μmol/L or 0.2 EU/dL) in urine. The absence of urobilinogen in the specimen
cannot be determined.
Color: Several studies showed good agreement between results obtained visually and
instrumentally.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
13 of 18
Clinical Concordance
The performance of the CLINITEK Novus PRO 12 Urinalysis Cassette was assessed on the
predicate analyzer and on the CLINITEK Novus Automated Urine Chemistry analyzer. A total of
340 specimens were evaluated on 3 instruments using 1 lot of urinalysis cassettes. The
following table shows examples results obtained for percent positive agreement and percent
negative agreement, assuming that the comparative analyzer was 100% and 100% specific.
For example, for bilirubin with the predicate analyzer, the table can be read as follows:
• Percent Positive Agreement: For bilirubin, the predicate analyzer reported 300 (N)
results as positive. Of these 300 positive results on the predicate analyzer, the
CLINITEK Novus Automated Urine Chemistry analyzer showed a positive result 99.3% of
the time (the observed rate of agreement). The one-sided 95% upper confidence bound
(UCB) for this agreement rate is 99.9%.
• Percent Negative Agreement: For bilirubin, the predicate analyzer reported 716 (N)
results as negative. Of these 716 negative results on the predicate analyzer, the
CLINITEK Novus Automated Urine Chemistry analyzer showed a negative result 100% of
the time (the observed rate of agreement).
Table 1: Percent Positive and Percent Negative Agreement for the CLINITEK Novus
Automated Urine Chemistry Analyzer Compared to the Predicate Analyzer
Percent Positive Agreement Percent Negative Agreement
Test N % Agreement One-sided 95% N % Agreement One-sided 95%
UCB (%) UCB (%)
Albumin 779 100 NA* 779 98.4 99.4
Bilirubin 1016 99.3 99.9 1016 100 NA
Blood 1016 100 NA 1016 100 NA
Creatinine NA NA NA NA NA NA
Glucose 1016 100 NA 1016 100 NA
Ketone 1017 99.7 99.9 1017 89.1 91.5
Leukocytes 1019 100 NA 1019 99.9 99.9
Nitrite 1016 100 NA 1016 100 NA
pH NA NA NA NA NA NA
Protein 779 99.4 99.8 779 100 NA
Urobilinogen 1016 100 NA 1016 88.6 90.4
Albumin:Creatinine NA NA NA NA NA NA
Protein:Creatinine NA NA NA NA NA NA
*NA = Not applicable
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
14 of 18
Table 2: Exact and Within One-Level Agreement for the CLINITEK Novus Automated
Urine Chemistry Analyzer Compared to the Predicate Analyzer
Test N % Exact Agreement % Within One-Level Agreement
Albumin 779 85.5 100
Bilirubin 1016 94.3 99.8
Blood 1016 88.9 100
Creatinine 1016 79.8 100
Glucose 1016 98.1 100
Ketone 1017 88.8 100
Leukocytes 1019 99.0 99.9
Nitrite 1016 100 100
pH 1016 85.1 99.9
Protein 779 89.6 100
Urobilinogen 1016 90.7 100
Albumin:Creatinine 779 NA* 100
Protein:Creatinine 779 NA 96.9
*NA = Not applicable
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
15 of 18
References
1. CLSI: “Urinalysis and Collection, Transportation, and Preservation of Urine Specimens;
Approved Guideline Second Edition.” CLSI document GP16-A2 (ISBN 1-56238-448-1).
www.clsi.org.
2. Burtis, C.A. and Ashwood, E.R.: Tietz Textbook of Clinical Chemistry, 2nd ed. Philadelphia:
Saunders; 1996; pp. 717–719, 968, 988–989, 2176–2211.
3. Pesce, A.J. and First, M.R.: “Proteinuria: an integrated review” in: Cameron, J.S., et al.
(eds.): Kidney Disease, Vol. 1, 1st ed. New York: Marcel Dekker; 1979; pp. 54–79,
144–157.
4. Kodama, K. et al.: The Range of Albumin Concentrations in the Single-Void First Morning
Urine of 1090 Healthy Young Children. Diab. Research Clin. Prac. 9: 55–58; 1990.
5. Henry, J.B. (ed.): Clinical Diagnosis and Management by Laboratory Methods, 19th ed.
Philadelphia: Saunders; 1996; pp. 164, 411–456.
6. Newall, R.G. and Howell R.: Clinical Urinalysis, The Principles and Practice of Urine
Testing in the Hospital and Community. Buckinghamshire, UK: Bayer Corporation; 1990;
pp. 25–30.
7. Newman, D.J., et al.: Urinary protein and albumin excretion corrected by creatinine and
specific gravity. Clin. Chima. Acta 294: 139–155; 2000.
8. Free, A.H. and Free, H.M.: Urinanalysis in Clinical Laboratory Practice. Cleveland:
CRC Press, Inc.; 1976; pp. 39–56.
9. Pugia, M.J., et al.: Screening School Children for Albuminuria, Proteinuria and Occult
Blood with Dipsticks. Clin. Chem. Lab. Med. 37 (2): 149–157; 1999.
10. Position Statement: Diabetic Nephropathy. Diabetes Care 20: S24–S27; 1997.
11. Warram, J.H., et al.: Effect of Duration of Type I Diabetes on the Prevalence of Stages of
Diabetic Nephropathy Defined by Urinary Albumin/Creatinine Ratio. J. Amer. Soc.
Nephrol. 7: 930–937; 1996.
12. Pugia, M.J., et al.: Assay of Creatinine Using the Peroxidase Activity of Copper-Creatinine
Complexes. Clin. Biochem. 33 (1): 63–70; 2000.
13. Pugia, M.J., et al.: Comparison of Instrument-Read Dipsticks for Albumin and Creatinine in
Urine with Visual Results and Quantitative Methods. J. Clin. Lab. Anal. 12: 280–284;
1998.
14. Mitch, W.E. and Walser, M.: A Proposed Mechanism for Reduced Creatinine Excretion in
Severe Chronic Renal Failure. Nephron 21: 248–254; 1978.
15. Lafolie, P., et al.: Importance of creatinine analysis of urine when screening for abused
drugs. Clin. Chem. 37: 1927–1931; 1991.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
16 of 18
Technical Assistance
For customer support, please contact your local technical support provider or distributor.
www.siemens.com/diagnostics
Trademarks
CLINITEK Novus and URIN-TEK are trademarks of Siemens Healthcare Diagnostics.
CAPOTEN is a trademark of Par Pharmaceutical, Inc.
GANTRISIN and GANTANOL are trademarks of Hoffman-LaRoche Inc.
FURADANTIN and KEFLEX are trademarks of Shionogi Inc.
KEFLIN is a trademark of Eli Lilly and Company.
LODINE is a trademark of Victory Pharma, Inc.
MACRODANTIN is a trademark of Procter and Gamble Pharmaceuticals Puerto Rico, Inc.
PYRIDIUM is a trademark of Warner Chilcott Company, Inc.
TAGAMET is a trademark of SmithKline Beecham Pharmaceuticals Co.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
17 of 18
Definition of Symbols
The following symbols may appear on the labeling and packaging:
Symbol Definition
In vitro diagnostic medical device
Catalog Number
Consult instructions for use
Manufacturer
Temperature limitation (2–8°C)
Contains sufficient for (n) tests
Batch code
Use by
Keep away from light and heat
2010-11-17 Date format (year-month-day)
2010-11 Date format (year-month)
Store upright
© 2012 Siemens Healthcare Diagnostics. All rights reserved.
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
18 of 18
CLINITEK Novus PRO 12 Urinalysis Cassette 10844208_EN, Rev. A
You might also like
- Stellar Evolution and NucleosynthesisDocument26 pagesStellar Evolution and NucleosynthesisEzekiel Lapitan100% (1)
- Abbott Imx OmDocument485 pagesAbbott Imx OmtabaradanielNo ratings yet
- Histamine, Serotonin & The Ergot AlkaloidsDocument31 pagesHistamine, Serotonin & The Ergot AlkaloidsnicewanNo ratings yet
- NMAT 17 Crash Course Review - Biochemistry ReviewerDocument6 pagesNMAT 17 Crash Course Review - Biochemistry ReviewerMikaela Rome Bigay83% (6)
- Lecture 1 - Chromosome & GenomeDocument64 pagesLecture 1 - Chromosome & GenomeFriendlyGoodGirlNo ratings yet
- Clinical Laboratories Point of Care Testing: Rev 2, Ver 1, 6/2013Document22 pagesClinical Laboratories Point of Care Testing: Rev 2, Ver 1, 6/2013Inês PimentaNo ratings yet
- Clinitek 500 (Bayer) CT 500 Service Manual PDFDocument322 pagesClinitek 500 (Bayer) CT 500 Service Manual PDFSwami Meera100% (1)
- Tosoh Bio Science - G8 ChromatogramsDocument1 pageTosoh Bio Science - G8 ChromatogramsimrecoNo ratings yet
- XN-2000 Ifu Na (1211)Document428 pagesXN-2000 Ifu Na (1211)CARLOSNo ratings yet
- Diagnosis of HemophiliaDocument150 pagesDiagnosis of HemophiliaresmasmanNo ratings yet
- GEM 4000 OperatorguideDocument80 pagesGEM 4000 OperatorguideAnnyNo ratings yet
- Data Sheet 29 - Fig Tc704 Conical (Witches Hat) StrainerDocument1 pageData Sheet 29 - Fig Tc704 Conical (Witches Hat) StrainerAnonymous 0OizFXUONo ratings yet
- Bio Rad Laboratories Catalog Items 9.1.2018Document687 pagesBio Rad Laboratories Catalog Items 9.1.2018Vadim ZorinNo ratings yet
- Atellica HEMA RET PLTO 0.5 L x4 Reagent - Atellica HEMA - Rev 03 DXDCM 09017fe98070c55b-1658506190586Document6 pagesAtellica HEMA RET PLTO 0.5 L x4 Reagent - Atellica HEMA - Rev 03 DXDCM 09017fe98070c55b-1658506190586yousra zeidanNo ratings yet
- Cobas U 701 Operators Manual EN (Initial Version) 1.0.0 ENDocument238 pagesCobas U 701 Operators Manual EN (Initial Version) 1.0.0 ENRicky100% (1)
- Instrument Air Systems: A Guide For Power Plant MaintenanceDocument73 pagesInstrument Air Systems: A Guide For Power Plant MaintenanceratheeshNo ratings yet
- LIAISON® Host Interface Manual (Revb)Document26 pagesLIAISON® Host Interface Manual (Revb)Mauricio Antonio Guzman LilloNo ratings yet
- Alchemical Operations Symbolized Through Bird ImageryDocument11 pagesAlchemical Operations Symbolized Through Bird ImageryDorian Taddei100% (1)
- Sysmex CS 5100Document4 pagesSysmex CS 5100Katamba RogersNo ratings yet
- High Performance For ALL: Auto Hematology AnalyzerDocument5 pagesHigh Performance For ALL: Auto Hematology AnalyzerrazaNo ratings yet
- BC 760 BC 780 BrochureDocument2 pagesBC 760 BC 780 BrochureBio AllianceNo ratings yet
- Brochure PDFDocument72 pagesBrochure PDFkisa guyNo ratings yet
- 0812 in Vitro Blood Gas Analyzers GuideDocument9 pages0812 in Vitro Blood Gas Analyzers GuidedjebrutNo ratings yet
- Module 1: Prepare The Necessary Tools and Equipment For The Specific Nail Care Activity Week 1 PRE-TEST: Multiple ChoiceDocument12 pagesModule 1: Prepare The Necessary Tools and Equipment For The Specific Nail Care Activity Week 1 PRE-TEST: Multiple Choicefrancisco50% (2)
- Humastar 100 Humastar 200 - Lis Astm Interface ManualDocument6 pagesHumastar 100 Humastar 200 - Lis Astm Interface ManualPedroNo ratings yet
- R&D Systems Hematology Products: Controls Calibrators Linearity Materials Quality Control ProgramDocument20 pagesR&D Systems Hematology Products: Controls Calibrators Linearity Materials Quality Control Programa sangNo ratings yet
- Twelve-Channel ECG: Blood Gas and Chemistry AnalyzerDocument2 pagesTwelve-Channel ECG: Blood Gas and Chemistry AnalyzerWilliam LukeNo ratings yet
- Service Manual CT 50Document284 pagesService Manual CT 50Alvaro Restrepo GarciaNo ratings yet
- Multistix Reagent StripDocument3 pagesMultistix Reagent StripFrancis TorresNo ratings yet
- Brosur Clinitek Novus BrochureDocument2 pagesBrosur Clinitek Novus BrochureFarly AugusNo ratings yet
- Product Correction 01 08 EnglishDocument6 pagesProduct Correction 01 08 Englishduytaybui94No ratings yet
- ST-200 AQua (HCO3) BrochureDocument2 pagesST-200 AQua (HCO3) BrochureSmart BiomedicalNo ratings yet
- UserManual PDFDocument546 pagesUserManual PDFKader SmailiNo ratings yet
- Mindray Bs 200Document13 pagesMindray Bs 200Roberto AriasNo ratings yet
- Furuno CA-180 / ILab 350 / RX Daytona instructions rev 420.0.2 - 2010-08-01Document75 pagesFuruno CA-180 / ILab 350 / RX Daytona instructions rev 420.0.2 - 2010-08-01Dharmesh Patel100% (1)
- BIO RAD Evolis System ManualDocument4 pagesBIO RAD Evolis System ManualAhmedJuman0% (1)
- Guia de Usuario Fia 8000Document29 pagesGuia de Usuario Fia 8000freddymataNo ratings yet
- 0 Complete Operator Training ManualDocument416 pages0 Complete Operator Training ManualKader SmailiNo ratings yet
- Mind RayDocument41 pagesMind Ray46877537No ratings yet
- Selectra Pro XS, Flexor EL80 Manual Configuración de ReactivosDocument123 pagesSelectra Pro XS, Flexor EL80 Manual Configuración de ReactivosFrancisco Primera0% (1)
- CEA Plus: Warnings and PrecautionsDocument4 pagesCEA Plus: Warnings and PrecautionsAhmed Ben NjahNo ratings yet
- Service ProgramDocument47 pagesService ProgramHuseyn aliyevNo ratings yet
- 1975ec-2026ec-2028ec 2023-04Document57 pages1975ec-2026ec-2028ec 2023-04Sujit KushwahaNo ratings yet
- Elitech Clinical Diagnostics CatalogueDocument10 pagesElitech Clinical Diagnostics Catalogueclinical_pathologyNo ratings yet
- Check Teglink Communication On All Controllers: ProcedureDocument4 pagesCheck Teglink Communication On All Controllers: Procedureالواثقة باللهNo ratings yet
- Prospekt BS 480 EngDocument8 pagesProspekt BS 480 EngArlong87No ratings yet
- Section 4 Adjustment: XS Series S/M December 13, 2007Document34 pagesSection 4 Adjustment: XS Series S/M December 13, 2007Huseyn aliyevNo ratings yet
- Cell Dyn 3200 Operator ManualDocument676 pagesCell Dyn 3200 Operator Manualquankdd100% (1)
- Humaclot Duo PlusDocument54 pagesHumaclot Duo PlusPatricia Tauran0% (1)
- Coulter LH750 Operators GuideDocument184 pagesCoulter LH750 Operators GuideFrank MateosNo ratings yet
- c111 Book PDFDocument1 pagec111 Book PDFMukesh Viswanath Lingamsetty0% (1)
- HA-8180service Manual EnglishDocument551 pagesHA-8180service Manual Englishzhigang yangNo ratings yet
- HumaLyzer Primus User ManualDocument62 pagesHumaLyzer Primus User Manualansarhussain012No ratings yet
- Operators Manual - 989-942M ABL800Document434 pagesOperators Manual - 989-942M ABL800waad100% (1)
- BC5000¡ BC5150 Service Training Material1.0Document180 pagesBC5000¡ BC5150 Service Training Material1.0Jaime EspinosaNo ratings yet
- XS-Series PM Standard Procedure (E)Document10 pagesXS-Series PM Standard Procedure (E)Armando VargasNo ratings yet
- Operating Manual Tissue-Tek TEC 5 (GB)Document42 pagesOperating Manual Tissue-Tek TEC 5 (GB)Engineer AwaisNo ratings yet
- Above and Beyond: BC-760 & BC-780Document3 pagesAbove and Beyond: BC-760 & BC-780Dam L0% (1)
- CD-Ruby Preventive Maintenance ChecklistDocument6 pagesCD-Ruby Preventive Maintenance ChecklistLuis Felipe Fuentes LNo ratings yet
- ADVIA Centaur XP Reference Manual PDFDocument498 pagesADVIA Centaur XP Reference Manual PDFVicky100% (1)
- Folleto PFA 100 SiemensDocument4 pagesFolleto PFA 100 SiemensSantiagoAFNo ratings yet
- G8 Variant EN Rev 09072013 01Document9 pagesG8 Variant EN Rev 09072013 01Nia AmbarwatiNo ratings yet
- Fuji Dri-Chem Nx500Document4 pagesFuji Dri-Chem Nx500Kaushik Bhuva100% (2)
- Mindray BS200 User ManualDocument6 pagesMindray BS200 User ManualMichael OkekeNo ratings yet
- Mission Urine Analyzers All in One Sell SheetDocument6 pagesMission Urine Analyzers All in One Sell SheetDorisjuarsa SmsNo ratings yet
- ADD-00058823-R1 - ARCHITECT Specifications PDFDocument4 pagesADD-00058823-R1 - ARCHITECT Specifications PDFGita RahvitaNo ratings yet
- Catalog # URS-10: 100 Strips Per BoxDocument4 pagesCatalog # URS-10: 100 Strips Per BoxLey100% (1)
- Simple and Rapid Analysis of Nitrofurazone From Blood, Milk, Urine and Meat SamplesDocument3 pagesSimple and Rapid Analysis of Nitrofurazone From Blood, Milk, Urine and Meat SamplesJesus VillanuevaNo ratings yet
- Tanner Scientific 10SG Reagent Test StripsDocument2 pagesTanner Scientific 10SG Reagent Test Stripssaifulmangopo123No ratings yet
- Adoc - Pub Clinical Pathology and Medical LaboratoryDocument9 pagesAdoc - Pub Clinical Pathology and Medical LaboratoryGanezNo ratings yet
- Tugas DR Sari Juli Dan AgustusDocument24 pagesTugas DR Sari Juli Dan AgustusRennilia NitaNo ratings yet
- SK PPDS Angkatan XxiiiDocument6 pagesSK PPDS Angkatan XxiiiRennilia NitaNo ratings yet
- Cancer RiskDocument8 pagesCancer RiskRennilia NitaNo ratings yet
- Clinitek NovusDocument4 pagesClinitek NovusRennilia NitaNo ratings yet
- Viswanathan2011 PDFDocument6 pagesViswanathan2011 PDFRennilia NitaNo ratings yet
- The Endocrine SystemDocument42 pagesThe Endocrine SystemRennilia NitaNo ratings yet
- Cancer RiskDocument8 pagesCancer RiskRennilia NitaNo ratings yet
- VMA CortisolDocument30 pagesVMA CortisolRennilia NitaNo ratings yet
- Crystal DefectsDocument3 pagesCrystal DefectsixbreakxawayNo ratings yet
- Lab Report Vicat TestDocument2 pagesLab Report Vicat TestmanNo ratings yet
- Igcse Coordinated Sciences 0654 Combined Science 0 - 59cc8a591723ddab3bbdfff3 PDFDocument50 pagesIgcse Coordinated Sciences 0654 Combined Science 0 - 59cc8a591723ddab3bbdfff3 PDFBank Yossy WoluslaweNo ratings yet
- Mark Scheme (Results) January 2020Document34 pagesMark Scheme (Results) January 2020Mahadi Hasan KhanNo ratings yet
- Powder injection moulding of multi-material devicesDocument6 pagesPowder injection moulding of multi-material devicesPaulinaIzquierdoNo ratings yet
- STOK BARANG SAAT INI PT. COMBI PUTRA MANDIRIDocument34 pagesSTOK BARANG SAAT INI PT. COMBI PUTRA MANDIRIAtik Marfu'ahNo ratings yet
- Chemicals Zetag MSDS LDP Zetag 3940 (US) - 1010Document6 pagesChemicals Zetag MSDS LDP Zetag 3940 (US) - 1010PromagEnviro.comNo ratings yet
- STAR COACHING CLASS - Parshotam Jethani (98982 16776)Document3 pagesSTAR COACHING CLASS - Parshotam Jethani (98982 16776)Kalp JethaniNo ratings yet
- Harvard Systems Biology 200 SyllabusDocument8 pagesHarvard Systems Biology 200 SyllabusJ100% (2)
- The Kaldnes Moving Bed Process For Wastewater Treatment at Pulp and Paper MillsDocument3 pagesThe Kaldnes Moving Bed Process For Wastewater Treatment at Pulp and Paper Millsvinhphat90No ratings yet
- HUBS1403 - Biomedical Science 1 - Lecture 4. Carbohydrates and LipidsDocument33 pagesHUBS1403 - Biomedical Science 1 - Lecture 4. Carbohydrates and LipidsEvelyn YongNo ratings yet
- ARV-WT112 (U) : Wafer Type Butterfly Valve Universal FlangedDocument2 pagesARV-WT112 (U) : Wafer Type Butterfly Valve Universal FlangedmalNo ratings yet
- Installation and Procedures of Rock BoltDocument36 pagesInstallation and Procedures of Rock BoltKushana Saikirann100% (1)
- Material Safety Data Sheet 1. Product and Company IdentificationDocument4 pagesMaterial Safety Data Sheet 1. Product and Company IdentificationkhairunisaNo ratings yet
- Statistical Theory: Molecular Mass Distributions Step Growth PolymerizationDocument21 pagesStatistical Theory: Molecular Mass Distributions Step Growth PolymerizationTayyab AhsanNo ratings yet
- DHANRAJDocument23 pagesDHANRAJDurgesh Patil DspNo ratings yet
- Water Soluble Polymer Flocculants Synthesis, PDFDocument43 pagesWater Soluble Polymer Flocculants Synthesis, PDFruizgj2011No ratings yet
- Avocado Seed Extract AnalysisDocument14 pagesAvocado Seed Extract AnalysisRatna SariNo ratings yet
- P-SRF N: Process Sterile Air Filter ElementsDocument8 pagesP-SRF N: Process Sterile Air Filter ElementsDavid MartinNo ratings yet
- Uti PDFDocument25 pagesUti PDFMG PolvorosaNo ratings yet
- About Welding Process 43Document1 pageAbout Welding Process 43XerexNo ratings yet
- Protective Coatings: Product CatalogueDocument40 pagesProtective Coatings: Product Cataloguegns1234567890No ratings yet