Professional Documents
Culture Documents
Vitrectomy Surgery For Primary Retinal Detachment
Uploaded by
Avluz AdiansuhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vitrectomy Surgery For Primary Retinal Detachment
Uploaded by
Avluz AdiansuhCopyright:
Available Formats
Management of Specific Diseases
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
Vitrectomy Surgery for Primary Retinal
Detachment
Renaud Duval a, b · Kourous A. Rezaei c, d
a
Department of Ophthalmology, University of Montréal, and b Maisonneuve-Rosemont Hospital,
Montréal, Qué., Canada; c Department of Ophthalmology, Rush University Medical Center, and
d
Illinois Retina Associates, Chicago, Ill., USA
Abstract et al. [4] introduced vitrectomy causing a para-
Small-gauge pars plana vitrectomy has emerged as one digm shift in the management of retinal detach-
of the leading approaches to the management of prima- ment. 20-gauge instrumentation was widely used
ry retinal detachment in recent years. Developments in until the advent of small-gauge surgery with the
technology and instrumentation have improved this pro- 25-gauge system by Fujii et al. [5], the 23-gauge
cedure and given surgeons a wide variety of tools to tack- system by Eckardt [6], and finally the 27-gauge
le this pathology. In this chapter, the techniques utilized system by Oshima et al. [7]. Following such ad-
in the management of primary retinal detachments are vances in technology, the use of pars plana vitrec-
discussed. © 2014 S. Karger AG, Basel tomy (PPV) for the repair of rhegmatogenous ret-
inal detachment increased dramatically. Medicare
data for fees in the USA shows a 72% increase in
Surgical management of primary rhegmatoge- the use of PPV for rhegmatogenous retinal de-
nous retinal detachment has changed drastically tachment from 1997 to 2007 [8]. A number of fac-
over the years, and the incremental improvements tors are responsible for such a gain in popularity:
in the repair of retinal detachment have led to pro- improved cutters and fluidics, wide-angle visual-
gressively higher success rates. Jules Gonin’s [1] ization, availability of heavy liquids, and improved
first operation using thermocautery to coagulate retinopexy techniques. Successful outcomes of
both the choroid and retina at the location of the small-gauge PPV for the repair of rhegmatoge-
retinal break achieved retinal reattachment in 30– nous retinal detachment has been shown to be
40% of cases. Rosengren [2] demonstrated that in- high in most series, with primary success rates
ternal tamponade of the retinal break with air fol- reaching up to 95.7% [9]. In this chapter some of
lowing external diathermy achieved retinal reat- the techniques developed by retina surgeons from
tachment in 76% of cases. Custodis [3] introduced around the world that we have utilized in the re-
scleral indentation in 1949 and brought the suc- pair of primary retinal detachment using small-
cess rate up to 84%. In the early 1970s, Machemer gauge PPV surgery are discussed.
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
Downloaded by:
Surgical Techniques very safe and efficient procedure with the added
benefit of increased postoperative comfort for
Instrumentation the patients. It also diminishes the risk of hav-
Vitrectomy with either 23- or 25-gauge cannu- ing the patient cough or ‘buck’ on the endotra-
lated trocar systems has many advantages such as cheal tube during or after extubation, which has
decreased rate of scelrotomy suturing with less been associated with massive suprachoroidal
trauma to the conjunctiva and subsequent dry eye hemorrhage [19]. General anesthesia eliminates
symptoms, reduced postoperative suture-in- patient movement during surgery and the dis-
duced astigmatism, improved patient comfort in comfort associated with scleral depression. In
the postoperative period with faster recovery, appropriate patients, local anesthesia alone is
more efficient surgical time, reduced rate of scle- safe and effective, offering excellent analgesia
rotomy-related retinal breaks, and reduced air jet and akinesia for the duration of even the longest
toxicity [10–17]. of cases: approximately 5.0 ml of a 50/50 mix-
The use of valved trocars has further improved ture of 2% xylocaine (AstraZeneca, Wilming-
the fluidics in vitrectomy surgery, offering a ton, Del., USA) and 0.5% bupivacaine (Astra-
closed system. This reduces the potential for reti- Zeneca) injected into the retrobulbar space by
nal incarceration, limits the formation of bubbles inserting a 25-gauge Atkinson needle (BD Vis-
at the fluid-heavy liquid interface when exchang- itec, Franklin Lanes, N.J., USA) connected to a
ing instruments, and reduces the risk of intraop- 10-ml syringe into the lower eyelid, at the junc-
erative suprachoroidal hemorrhage due to intra- tion between the lateral and middle third. Sup-
operative hypotony. plemental retrobulbar anesthesia during the
Illumination during vitrectomy surgery has case can be delivered by making a conjunctival
significantly improved in recent years, especially snip in the inferior fornix and passing a curved
with the advent and improvements in small- retrobulbar cannula into the sub-Tenon space.
gauge chandelier light illumination, lighted and Optimal anesthesia is essential since vitrectomy
curved laser probes allowing surgeon-assisted for repair of primary retinal detachment may
scleral depression, and endolaser treatment close involve manipulation of the globe with scleral
to the ora serrata in phakic patients without the depression.
need for an endoilluminator [18]. Care is taken in positioning the patient’s head
Wide-angle visualization provided by either a to assure that the patient’s chin is positioned in a
contact or a noncontact system is another major horizontal plane (not angled) to ensure adequate
advancement in PPV surgery for retinal detach- exposure of the entire retina throughout the sur-
ment repair. New-generation viewing systems of- gery, especially in patients with prominent brows
fer excellent viewing angles even through small or small palpebral fissures. Prepping the skin
pupils, often without needing a skilled assistant. around the eye and the eye lashes with 10% povi-
done-iodine solution (Rougier, Mirabel, Que.,
Anesthesia, Prepping, and Draping Canada) and the conjunctiva with 5% povidone-
Anesthesia for small-gauge PPV consists of ei- iodine solution following the draping is done in a
ther local or general anesthesia. The type of an- sterile fashion.
esthesia selected should be tailored to the pa- Preservative-free lubricant (Genteal; Alcon,
tient. General anesthesia can be delivered either Fort Worth, Tex., USA) is applied on the sur-
in the form of endotracheal intubation or laryn- face of the cornea. Attention is given through-
geal mask anesthesia. In the hands of an experi- out the surgery to avoid corneal drying and to
enced anesthetist, laryngeal mask anesthesia is a minimize the need for epithelial debridement
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
PPV for Primary Retinal Detachment 175
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
upper borders of the lateral and medial recti
muscles to ensure maximum range of move-
ment, making sure to avoid injuring the ciliary
arteries and nerves. A chandelier light (25-gauge
Alcon Chandelier Lighting System; Alcon, Fort
Worth, Tex., USA) is used in vitrectomies for re-
pairing primary retinal detachment. The trocar
for the chandelier light is inserted inferotempo-
rally, just inferior to the infusion cannula (fig. 1).
During peripheral scleral depressed vitreous
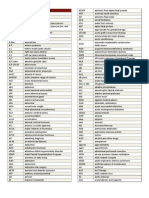
Fig. 1. The location of valved trochars (Alcon MIVS) and
chandelier light (Alcon) during vitrectomy surgery for
shaving, this localization ensures superior visual-
retinal detachment. A corneal protector is used to avoid ization and shaving of the inferior peripheral vit-
microscope light toxicity during trochar insertion. The reous (without the need of an endoilluminator),
chandelier light is inserted inferotemporally below the which is the most frequent site of proliferative
infusion light for maximum inferior illumination.
vitreoretinopathy and recurrent retinal detach-
ment [21]. The incision is not bevelled to avoid
the angling of the chandelier light during sur-
during surgery [20]. Further, a corneal protec- gery, and may need to be sutured at the conclu-
tor is placed on the surface of the cornea when sion of the operation.
no intravitreal procedures are performed, i.e. The chandelier light is inserted perpendicular
during trocar insertion and removal at the be- to the sclera to prevent lenticular glare during
ginning and end of surgery to reduce retinal surgery in phakic patients. Furthermore, care is
light exposure. taken to turn off the chandelier light when not
needed and to avoid shining the chandelier light
Vitrectomy Procedure directly on the macula.
The location of the sclerotomies is measured The fluidic parameters of the vitrectomy ma-
with callipers. Generally, in phakic eyes, the scle- chine are set to proportional vacuum with the
rotomies are measured at 4 mm posterior to the highest constant cut rate available (Alcon). The
limbus to limit the possibility of accidental lens maximum vacuum can be set at 650 mm Hg and
touch during surgery. In pseudophakic and is controlled with the foot pedal. The cut rate is
aphakic patients, the sclerotomies are placed be- currently set at 5,000 cuts/min and is not changed
tween 3 and 3.5 mm posterior to the limbus. The throughout the surgery. During peripheral vitre-
eye is stabilized with toothed forceps and the tro- ous shaving, the vacuum is kept at around 100–
cars are inserted in a bevelled fashion. An angle 150 mm Hg to prevent peripheral iatrogenic
of around 20° is used for trocar insertion and breaks. For efficient vitrectomy, the vitrectomy
kept throughout the creation of the sclerotomy probe engages the vitreous at all times (by moving
to generate an oblique scleral tunnel, which is it towards the vitreous).
likely to be self-sealing at the conclusion of the Illumination intensity is kept as low as neces-
surgery. The inferotemporal infusion cannula is sary for visualization throughout the surgery to
placed in the usual manner at the meridian of the minimize any light toxicity. This is especially true
inferior border of the lateral rectus muscle and its for the chandelier light which is often immobile
tip is visualized prior to turning on the infusion. throughout the surgery. The chandelier light does
The superotemporal and superonasal scleroto- not need to be kept on throughout the surgery
mies may be placed around the meridians of the and should be turned on only when needed.
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
176 Duval · Rezaei
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
Removing the Vitreous
Vitrectomy is begun by inserting the instruments
in the vitreous cavity. The first step is to verify the
perfusion of the optic nerve. The pulsation of the
central retinal artery and/or the sudden pallor of
the optic nerve may indicate a mismatch between
pressure of the infusion line inside the eye and
the patient’s diastolic blood pressure. Keeping
the infusion pressure around 25 mm Hg and
avoiding a diastolic blood pressure below 60 mm
Fig. 2. Scleral depressed vitrectomy by the surgeon in a
Hg usually allows adequate optic nerve and reti- phakic patient. Illumination is provided by chandelier
nal perfusion during surgery with valved trocar light. The cutter shaft is almost parallel to the surface of
systems. the retina. Lower suction and the maximum cut rate is
The next step is induction of posterior vitreous used during peripheral shaving. The cutter should never
be anterior to the ora in a phakic patient.
detachment (PVD). Although most patients with
retinal detachment already have PVD, many
times they may only have partial PVD. Young and
highly myopic patients usually do not have PVD tached retina, making the induction of the PVD
upon presentation. and vitrectomy easier and safer.
PVD is induced by positioning the cutter just The separation of the hyaloid should be ex-
above the optic nerve, turning off the cutting tended as far anteriorly as possible and deemed
function of the vitreous cutter, and applying al- safe. Once the posterior hyaloid/Weiss ring is en-
most full aspiration. Attention should be given to gaged, attention should be given to the peripheral
avoid ocular hypotony and retinal incarceration retina using the wide-angle viewing system. The
into the tip of the vitrectomy probe during this appearance of peripheral retinal hemorrhages,
step. Once the posterior hyaloid (or Weiss ring) is which are generally the precursors of iatrogenic
engaged, the posterior hyaloid is elevated in an peripheral retinal breaks during this maneuver, is
anterior-posterior direction while monitoring the a reliable sign that the posterior edge of the ante-
status of the detached retina using wide-angle vi- rior vitreous base has been reached and that fur-
sualization. In case the retina is partially detached, ther hyaloid separation is not possible and should
the port of the cutter is kept away from the de- not be attempted.
tached area throughout this maneuver to prevent Following the induction of PVD, core vitrec-
incarceration of the retina into the vitrectomy tomy is performed followed by peripheral vitrec-
probe. In total retinal detachment, the light pipe tomy. A thorough shaving of the vitreous base
can be used to shield the port of the vitrectomy over 360° may reduce the potential for recurrence
from a very mobile retina. In case the retina is of the retinal detachment from vitreous traction.
very mobile, the amount of vacuum may need to Scleral depression is utilized to adequately visual-
be adjusted. In very bullous retinal detachment, ize the peripheral vitreous (fig. 2). Although a
the subretinal fluid may be drained through the skilled assistant could provide the required sup-
peripheral break prior to induction of PVD. In port for this task, greater control and indepen-
these scenarios, a localized vitrectomy is per- dence is achieved with the use of chandelier illu-
formed around the break followed by drainage of mination. The vitreous base is meticulously
the subretinal fluid through the same break. This shaved over 360° with the help of scleral depres-
generally leads to a dramatic flattening of the de- sion. The infusion pressure may be reduced to
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
PPV for Primary Retinal Detachment 177
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
Flattening the Retina
Drainage of subretinal fluid and flattening of the
retina is performed in one of two approaches de-
pending on the location of the retinal breaks and
the conformation of the retinal detachment. For
posteriorly located breaks and small detachments,
a fluid-air exchange can be performed while the
subretinal fluid is aspirated through the retinal
break with the soft-tip endodrainage cannula.
Caution must be observed when performing this
Fig. 3. Perfluoron injection in a patient with valved tro-
chars. The injections are done slowly and optic nerve per-
maneuver in macula on retinal detachments to
fusion is monitored during the injection. For egression of avoid the expansion of subretinal fluid under the
the fluid during injection, one may either use the vent macula. For anteriorly located breaks and large
supplied with the trochars or suction of the cutter as detachments, we prefer the use of heavy liquids
shown in this figure. Illumination is provided through
such as Perfluoron (Alcon) to expel the subretinal
chandelier light.
fluid through the peripheral break [22]. When us-
ing valved trocars, care must be taken to prevent
the increase of intraocular pressure while injecting
15–20 mm Hg to ease scleral indentation. The heavy liquids into the eye since it is a closed sys-
scleral depression is performed gently by apply- tem. This can be achieved in several ways:
ing constant pressure. Sudden changes in depres- • Using a dual-bore cannula (MedOne Surgical
sion pressure including extreme depression of the Inc., Sarasota, Fla., USA)
sclera or letting go of the depression should be • Placing a vent (Alcon) in one of the valved
avoided during this procedure. In phakic pa- trocars and using the chandelier light for
tients, the shaft of the cutter needs to be almost illumination
parallel to the retina (and not angled) to avoid • Aspirating fluid with the vitrector while
touching the lens. Further, peripheral vitreous injecting the heavy liquid and using
shaving should never be attempted anterior to the chandelier light for illumination (preferred
ora in phakic patients since it would lead to iatro- technique)
genic cataract formation. • Removing the chandelier light from its
During peripheral vitreous shaving, vitreous cannula (25-gauge EDGEPLUS trocar/
traction is relieved around all the breaks, including cannula; Alcon, Fort Worth, Tex., USA) and
amputating the flap of horseshoe tears. Following leaving the trocar (which is not valved) open
peripheral vitreous shaving, the peripheral retina is temporarily
examined with a scleral depressor and endoillumi- The heavy liquid is injected slowly over the op-
nator over 360°. All retinal breaks are identified tic nerve while monitoring the perfusion of the
and marked with either endodiathermy or endola- optic nerve. The tip of the cannula is kept inside
ser. Shifting the fluid away from under the break the heavy liquid bubble throughout the injection
with scleral depression and using the endolaser on process (fig. 3). The eye may be tilted away from
a higher duration and power is generally enough to the retinal break (prior to the heavy liquid reach-
mark the breaks and often avoids the need for using ing it) to optimize the displacement of subretinal
endodiathermy. It is important to mark the breaks fluid through the peripheral break. The retina is
prior to the use of any tamponade agent since they usually almost completely reattached under heavy
can make the recognition of the breaks difficult. liquid following this step.
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
178 Duval · Rezaei
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
In cases of midperipheral breaks or fairly large
breaks, the heavy liquid may be injected up to the
posterior edge of the retinal break, and then a par-
tial air-fluid exchange is performed to displace
the anterior subretinal fluid through the break.
This approach may minimize the possibility of
heavy liquid migration into the subretinal space. a
Retinopexy
Retinopexy is applied once the retina is flattened
under air or heavy liquid. A curved illuminated
laser probe is ideal for this task. It provides excel-
lent illumination during scleral depressed ante-
rior photocoagulation in phakic patients (fig. 4a).
Alternatively, a curved nonilluminated laser
probe can be used together with chandelier light b
illumination. In pseudophakic or aphakic pa-
Fig. 4. a Scleral depressed peripheral endolaser treat-
tients, a straight laser probe may be used. Initial ment in a phakic patient. This maneuver is performed
settings for the endolaser can be at 200 ms for du- with the curved lighted laser probe (Alcon). Background
ration and 160 mW for power and then titrated to illumination is provided through the chandelier light at a
obtain a moderate intensity laser burn (fig. 4b). lower setting (generally 10% illumination). b Laser spots
during scleral depressed peripheral endolaser treatment.
Endolaser is first applied around the breaks and
then one may perform 360° scleral depressed
photocoagulation on the peripheral vitreous base
up to the ora serrata. The laser burns are more ing displaced posteriorly by the enlarging air bub-
confluent in the area of retinal detachment and ble [24]. It is paramount not to release aspiration
less confluent in attached retina. One must avoid during this process since heavy liquid may reflux
laser burns at the 3-o’clock and 9-o’clock merid- from the cannula and enter the subretinal space
ians (posterior ciliary nerves). due to gravitational forces. Once all anterior fluid
During scleral depressed peripheral endolaser has been drained and the level of the heavy liquid
photocoagulation, it is important to release scler- is past the most posterior of retinal breaks, the
al depression slowly while working under heavy soft-tip cannula is placed above the optic nerve
liquids to prevent the formation of bubbles at the and the heavy liquid is completely removed from
heavy liquid-fluid interface. the eye. The heavy liquid is then washed off of the
extrusion line by aspirating a small quantity of bal-
Heavy Liquid Removal anced salt solution (Bausch & Lomb, Rochester,
Once retinopexy is completed, the heavy liquid is N.Y., USA) from a plastic cup. A few drops of bal-
removed during a fluid-air exchange. At the be- anced salt solution are then squirted on the retinal
ginning of the exchange, the soft-tip cannula is surface with a 30-gauge needle on a 1-ml syringe
kept in the fluid phase above the heavy liquid to to gather and help remove small residual heavy
transform the vitreous cavity into a two-phase sys- liquid droplets [25]. The anterior retina is reexam-
tem: air and heavy liquid [23]. The soft-tip can- ined one final time under air to assure all the
nula on the extrusion line is then kept on the break breaks are well surrounded, and if necessary sup-
to aspirate any anterior subretinal fluid that is be- plemental photocoagulation is added.
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
PPV for Primary Retinal Detachment 179
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
Sclerotomy Closure and Gas Injection Postoperatively
Preservative free lubricant (Genteal, Alcon) is ap- All patients are positioned face down at the con-
plied to the surface of the cornea and a corneal clusion of surgery. Patients are routinely evalu-
protector is placed on the cornea. The chandelier ated on postoperative day 1.
cannula is removed and the sclerotomy is sutured
with 8-0 Vicryl (Ethicon, Somerville, N.J., USA)
since it does not have a bevelled insertion. All the A Few Pearls for the Safe, Efficient, and
trocars are removed. Brief compression of the Successful Repair of Primary Retinal
sclerotomy site with a cotton-tip is performed to Detachment
assure they are water tight. In case of sclerotomy
leakage, a transconjunctival 8-0 Vicryl suture is • Chandelier light illumination allows scleral
passed through the leaking sclerotomy. Air is re- depressed vitreous shaving without the need
placed with a nonexpansile concentration of for a skilled assistant
long-acting gas (usually 14% C3F8; Sonomed Es- • Decrease retinal light exposure by turning off
calon, Lake Success, N.Y., USA) through a chim- the chandelier light when not in use and ad-
ney technique. The desired concentration and just its light intensity to the minimal amount
type of gas is prepared inside a 60-ml syringe con- needed
nected to a 30-gauge needle. A chimney is pre- • Lowering the infusion pressure during the
pared by removing the plunger of a 3-ml syringe scleral depressed vitrectomy reduces the
connected to a 25-gauge needle. Both needles are amount of force needed to indent the sclera
inserted into the vitreous cavity through the pars • During 360° laser photocoagulation, avoid
plana superiorly around 11 o’clock and 1 o’clock, burns, 3- and 9-o’clock meridians, and apply
and the air-gas exchange is performed by having less confluent laser to the attached retina.
an assistant inject the gas. Attention must be giv- • Gentle release of scleral depression while in-
en to assure that the tip of the needle is inside the denting under heavy liquid minimizes bubble
vitreous cavity. After injecting about 50 ml of the creation
gas volume, the chimney is removed and the in- • In a very bullous detachment, reducing the
traocular pressure is measured with the Barra- height of the detachment by draining the sub-
quer tonometer (Ocular Instruments, Bellevue, retinal fluid at the beginning of the case may
Wash., USA). Additional gas is injected as needed simplify the subsequent maneuvers
to achieve a target intraocular pressure of around • While lasering under air for an extended pe-
10–15 mm Hg. Subconjunctival injection of ste- riod of time, consider reducing the air pressure
roids and antibiotics is given followed by applica- to around 25 mm Hg (with valved trocars) and
tion of topical cycloplegic drops and antibiotic place a few drops of balanced salt solution on
ointment. The eye is patched and a shield is placed the posterior pole to prevent the drying of the
over the eye. macula and its associated toxic effects [26]
References
1 Gonin J: Le traitement du décollement 3 Custodis E: Bedeutet die Plombeaufna- 4 Machemer R, Buettner H, Norton EW,
rétinien. Ann Ocul 1921;158:175–194. hung auf die Sklera einen Fortschritt in Parel JM: Vitrectomy: a pars plana ap-
2 Rosengren B: Über die Behandlung der der operativen Behandlung der proach. Trans Am Acad Ophthalmol
Netzhaut-Ablösung mittelst Diathermie Netzhaut-Ablösung? Ber Dtsch Oph- Otolaryngol 1971;75:813.
und Luftinjektionen in den Glaskörper. thalm Ges 1953;58:102.
Acta Ophthalmol 1938;16:3–42.
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
180 Duval · Rezaei
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
5 Fujii GY, de Juan E Jr, Humayun MS, 12 Gosse E, Newsom R, Lochhead J: The 20 Garcia-Valenzuela E, Abdelsalam A,
Pieramici DJ, Chang TS, Awh C, Ng E, incidence and distribution of iatrogenic Eliott D, Pons M, Iezzi R, Puklin JE, Mc-
Barnes A, Wu SL, Sommerville DN: A retinal tears in 20-gauge and 23-gauge Dermott ML, Abrams GW: Reduced
new 25-gauge instrument system for vitrectomy. Eye (Lond) 2012;26:140– need for corneal epithelial debridement
transconjunctival sutureless vitrectomy 143. during vitreo-retinal surgery using two
surgery. Ophthalmology 2002;109: 13 Nakano T, Uemura A, Sakamoto T: Inci- different viscous surface lubricants. Am
1807–1812. dence of iatrogenic peripheral retinal J Ophthalmol 2003;136:1062–1066.
6 Eckardt C: Transconjunctival sutureless breaks in 23-gauge vitrectomy for macu- 21 Sternberg P Jr, Meredith T: Manage-
23-gauge vitrectomy. Retina 2005;25: lar diseases. Retina 2011;31:1997–2001. ment of recurrent retinal detachment
208–211. 14 Issa SA, Connor A, Habib M, Steel DH: after silicone oil injection. Arch Oph-
7 Oshima Y, Wakabayashi T, Sato T, Ohji Comparison of retinal breaks observed thalmol 1987;105:27–28.
M, Tano Y: A 27-gauge instrument sys- during 23 gauge transconjunctival vit- 22 Coll GE, Chang S, Sun J, Wieland MR,
tem for transconjunctival sutureless rectomy versus conventional 20 gauge Berrocal MH: Perfluorocarbon liquid in
microincision vitrectomy surgery. Oph- surgery for proliferative diabetic reti- the management of retinal detachment
thalmology 2010;117:93–102. nopathy. Clin Ophthalmol 2011;5:109– with proliferative vitreoretinopathy.
8 Ramulu PY, Do DV, Corcoran KJ, 114. Ophthalmology 1995;102:630–638.
Corcoran SL, Robin AL: Use of retinal 15 Scartozzi R, Bessa AS, Gupta OP, Regillo 23 Chang S, Lincoff H, Zimmerman NJ,
procedures in Medicare beneficiaries CD: Intraoperative sclerotomy-related Fuchs W: Giant retinal tears. Surgical
from 1997 to 2007. Arch Ophthalmol retinal breaks for macular surgery, 20- techniques and results using perfluoro-
2010;128:1335–1340. vs. 25-gauge vitrectomy systems. Am J carbon liquids. Arch Ophthalmol 1989;
9 Schneider EW, Geraets RL, Johnson Ophthalmol 2007;143:155–156. 107:761–766.
MW: Pars plana vitrectomy without 16 Hirata A, Yonemura N, Hasumura T, 24 Kirchhof B, Wong D: Essentials in Oph-
adjuvant procedures for repair of pri- Murata Y, Negi A: Effect of infusion air thalmology: Vitreo-Retinal Surgery. Ber-
mary rhegmatogenous retinal detach- pressure on visual field defects after lin, Springer, 2007.
ment. Retina 2012;32:213–219. macular hole surgery. Am J Ophthalmol 25 Garcia-Valenzuela E, Ito Y, Abrams GW:
10 Fujii GY, De Juan E Jr, Humayun MS, et 2000;130:611–616. Risk factors for retention of subretinal
al: Initial experience using the transcon- 17 Duval R, Hui JM, Rezaei KA: Rate of perfluorocarbon liquid in vitreoretinal
junctival sutureless vitrectomy system sclerotomy suturing in 23-gauge prima- surgery. Retina 2004;24:746–752.
for vitreoretinal surgery. Ophthalmol- ry vitrectomy. Retina 2014;34:679–683. 26 Winter M, Eberhardt W, Scholz C,
ogy 2002;109:1814–1820. 18 Eckardt C: Twin lights: a new chandelier Reichenbach A: Failure of potassium
11 Lakhanpal RR, Humayun MS, de Juan E illumination for bimanual surgery. Reti- siphoning by Müller cells: a new hy-
Jr, et al: Outcomes of 140 consecutive na 2003;23:893–894. pothesis of perfluorocarbon liquid-in-
cases of 25-gauge transconjunctival sur- 19 Pollack AL, McDonald HR, Ai E, John- duced retinopathy. Invest Ophthalmol
gery for posterior segment disease. Oph- son RN, Dugel PU, Folk J, Grand MG, Vis Sci 2000;41:256–261.
thalmology 2005;112:817–824. Lambert HM, Schwartz S, Miller RD:
Massive suprachoroidal hemorrhage
during pars plana vitrectomy associated
with Valsalva maneuver. Am J Ophthal-
mol 2001;132:383–387.
Kourous A. Rezaei, MD
Illinois Retina Associates, Ingalls Hospital Professional Building
71 West 156th Street, Suite 400
Harvey, IL 60426 (USA)
E-Mail karezaei@yahoo.com
198.143.38.97 - 6/22/2015 11:28:31 PM
Kellogg Health Sciences Libr.
PPV for Primary Retinal Detachment 181
Downloaded by:
Oh H, Oshima Y (eds): Microincision Vitrectomy Surgery. Emerging Techniques and Technology.
Dev Ophthalmol. Basel, Karger, 2014, vol 54, pp 174–181 (DOI: 10.1159/000360464)
You might also like
- Infusion Therapy TrainingDocument19 pagesInfusion Therapy Trainingjeremie cruz100% (1)
- Difficult IV Access C PGDocument42 pagesDifficult IV Access C PGFitrii WulanDari FitriNo ratings yet
- Mastering The BDS 2nd Year Hemant Gupta, 8th Ed PDFDocument807 pagesMastering The BDS 2nd Year Hemant Gupta, 8th Ed PDFSatvika67% (3)
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 66Document15 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 66sarasjunkNo ratings yet
- Review Article: A Review of Innovations in Rhegmatogenous Retinal Detachment Surgical TechniquesDocument6 pagesReview Article: A Review of Innovations in Rhegmatogenous Retinal Detachment Surgical TechniquesAnonymous S0MyRHNo ratings yet
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumDocument6 pagesComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinNo ratings yet
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumDocument6 pagesComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinNo ratings yet
- Midcheek Lift Using Facial Soft-Tissue Spaces of The MidcheekDocument11 pagesMidcheek Lift Using Facial Soft-Tissue Spaces of The MidcheekЩербакова ЛенаNo ratings yet
- Reconstruction of Periorbital Defects Using A Modified Tenzel FlapDocument6 pagesReconstruction of Periorbital Defects Using A Modified Tenzel FlapChandra BudiNo ratings yet
- 1 s2.0 S1319453417301418 MainDocument4 pages1 s2.0 S1319453417301418 MainEzra MargarethNo ratings yet
- 69 EdDocument10 pages69 EdAnna ListianaNo ratings yet
- Pterygium Management - Today: Medical ScienceDocument3 pagesPterygium Management - Today: Medical ScienceLiestiono NasiNo ratings yet
- Telaah Jurnal Rhizky Shasqia Putri NurDocument23 pagesTelaah Jurnal Rhizky Shasqia Putri NurrhizkyNo ratings yet
- Procedures in The TraumaDocument22 pagesProcedures in The TraumaJuan Jose SarastiNo ratings yet
- Sjab 059Document10 pagesSjab 059Hải Dương MinhNo ratings yet
- Anastesi Operasi Katarak AyuDocument23 pagesAnastesi Operasi Katarak AyuOfkom UnhasNo ratings yet
- Treatment of Primary Pterygium: Role of Limbal Stem Cells and Conjunctival Autograft TransplantationDocument4 pagesTreatment of Primary Pterygium: Role of Limbal Stem Cells and Conjunctival Autograft TransplantationdianamariniNo ratings yet
- Pars Plana VitrekDocument8 pagesPars Plana VitrekAnggisari Danastri DharmaNo ratings yet
- CLINICAL NEUROENDOSCOPY: A BRIEF HISTORYDocument94 pagesCLINICAL NEUROENDOSCOPY: A BRIEF HISTORYBivolaru AlinNo ratings yet
- Anaesthesia for Vitreo-Retinal SurgeryDocument6 pagesAnaesthesia for Vitreo-Retinal Surgeryluis castro martinezNo ratings yet
- Modified Keyhole Technique 2020Document5 pagesModified Keyhole Technique 2020GrahamOliverAceroVieraNo ratings yet
- Dr. Ankur Kumar, Dr. Kishor KumarDocument4 pagesDr. Ankur Kumar, Dr. Kishor KumarValentina Gracia ReyNo ratings yet
- Blefaroplastia No Quirugica ArticuloDocument8 pagesBlefaroplastia No Quirugica ArticuloDaniela GonzalezNo ratings yet
- Use Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenDocument4 pagesUse Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenYelisa PatandiananNo ratings yet
- Pneumatic RetinopexyDocument36 pagesPneumatic RetinopexyMartínJiménezNo ratings yet
- Retinal Physician - Visualization in Vitrectomy - An UpdateDocument12 pagesRetinal Physician - Visualization in Vitrectomy - An UpdateDr. M. Hannan JamilNo ratings yet
- Astigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionDocument6 pagesAstigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- International Journal of Science publishes article on innovative hysterectomy techniqueDocument12 pagesInternational Journal of Science publishes article on innovative hysterectomy techniqueBlink TdmNo ratings yet
- Editorial: The Management of Retinal Detachment: Techniques and PerspectivesDocument3 pagesEditorial: The Management of Retinal Detachment: Techniques and PerspectivesSarahNo ratings yet
- Cers Cadwell LucDocument3 pagesCers Cadwell LucVictorioStokNo ratings yet
- Ormond 2013Document12 pagesOrmond 2013Hafiz AlfarizieNo ratings yet
- Pterygium Excision With Free Conjunctival Limbal AutograftDocument7 pagesPterygium Excision With Free Conjunctival Limbal AutograftIOSRjournalNo ratings yet
- A Review of Natural Orifice Translumenal Endoscopic Surgery (NOTES) For Intra-Abdominal SurgeryDocument20 pagesA Review of Natural Orifice Translumenal Endoscopic Surgery (NOTES) For Intra-Abdominal SurgerylifeofnameNo ratings yet
- Gibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryDocument7 pagesGibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryjuanguapoNo ratings yet
- Endoscopic Skull Base SurgeryDocument25 pagesEndoscopic Skull Base Surgerypramod454992No ratings yet
- Opth 14 2087Document4 pagesOpth 14 2087Savitri IndrasariNo ratings yet
- Abstractbook2020 2Document50 pagesAbstractbook2020 2alpaslan alkanNo ratings yet
- Techniques To Address Conchal ExcessDocument2 pagesTechniques To Address Conchal ExcessArdi WiraNo ratings yet
- TMP 99 BADocument6 pagesTMP 99 BAFrontiersNo ratings yet
- Dorsal Slit Sleeve Technique For Male Circumcision: SurgicalDocument4 pagesDorsal Slit Sleeve Technique For Male Circumcision: SurgicaladiwinataNo ratings yet
- Amniotic Membrane Transplantation For Primary Pterygium SurgeryDocument5 pagesAmniotic Membrane Transplantation For Primary Pterygium SurgerySa 'ng WijayaNo ratings yet
- Efficacy of Autologous Blood Clot in Primary Pterygium Surgery Compared With Suture Technique in A Tertiary Hospital of BangladeshDocument7 pagesEfficacy of Autologous Blood Clot in Primary Pterygium Surgery Compared With Suture Technique in A Tertiary Hospital of BangladeshBOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)No ratings yet
- VYplastyDocument6 pagesVYplastyVineet ArunNo ratings yet
- Sebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfDocument9 pagesSebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfKaustubh KeskarNo ratings yet
- Evisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsDocument6 pagesEvisceration With Autogenous Scleral Graft and Bioceramic Implantation Within The Modified Scleral Shell 133 Cases Over 17 YearsSaraelsy MonterrosoNo ratings yet
- Video Telescopic Operating Microscope - A Recent Development in Reptile MicrosurgeryDocument4 pagesVideo Telescopic Operating Microscope - A Recent Development in Reptile MicrosurgeryChecko LatteNo ratings yet
- Primary Transcutaneous Lower Blepharoplasty With Routine Lateral Canthal Support: A Comprehensive 10-Year ReviewDocument10 pagesPrimary Transcutaneous Lower Blepharoplasty With Routine Lateral Canthal Support: A Comprehensive 10-Year ReviewFelyana GunawanNo ratings yet
- Comparison of MISS and limbal techniquesDocument7 pagesComparison of MISS and limbal techniquesvikrizkaNo ratings yet
- Crico 2013Document3 pagesCrico 2013Ismael Erazo AstudilloNo ratings yet
- Emergency Cricothyrotomy Performed by Surgical Airway-Naive Medical PersonnelDocument9 pagesEmergency Cricothyrotomy Performed by Surgical Airway-Naive Medical PersonnelnadaNo ratings yet
- A Prospective Observational Study On Scola For Ventral Hernia With Diastasis Recti - Our Experience at A Tertiary Care HospitalDocument4 pagesA Prospective Observational Study On Scola For Ventral Hernia With Diastasis Recti - Our Experience at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- JClinOphthalmolRes43143-3289519 090815Document6 pagesJClinOphthalmolRes43143-3289519 090815Wielda MutafadhilahNo ratings yet
- 10 1 1 115Document151 pages10 1 1 115Angela TorrenteNo ratings yet
- 2 Clinicopathological Comparative Vs Surgical 2018Document6 pages2 Clinicopathological Comparative Vs Surgical 2018solikin ikinNo ratings yet
- 11 I January 2023Document4 pages11 I January 2023IJRASETPublicationsNo ratings yet
- Logarajah, 2021Document6 pagesLogarajah, 2021Aze Andrea PutraNo ratings yet
- 266 2023 Article 3444Document7 pages266 2023 Article 3444Ingook SongNo ratings yet
- SAJS Vol543 2112 HIG SA Guidelines For The Management of Ventral HerniasDocument29 pagesSAJS Vol543 2112 HIG SA Guidelines For The Management of Ventral HerniasMonika Diaz KristyanindaNo ratings yet
- ProQuestDocuments 2015-03-24Document13 pagesProQuestDocuments 2015-03-24zerin_atinNo ratings yet
- Modified Lower Blepharoplasty With Fat Repositioning Via Transconjunctival Approach To Correct Tear Trough DeformityDocument6 pagesModified Lower Blepharoplasty With Fat Repositioning Via Transconjunctival Approach To Correct Tear Trough DeformityenviNo ratings yet
- Zingaretti Et Al. 2019Document5 pagesZingaretti Et Al. 2019Walid SasiNo ratings yet
- Prognostic Factors and Management of Patients With Choanal AtresiaDocument7 pagesPrognostic Factors and Management of Patients With Choanal AtresiaNalendra Tri WidhianartoNo ratings yet
- Evolution in Tissue Expander Design For Breast Reconstruction: Technological Innovation To Optimize Patient OutcomesDocument10 pagesEvolution in Tissue Expander Design For Breast Reconstruction: Technological Innovation To Optimize Patient OutcomesFauzi Novia Isnaening TyasNo ratings yet
- Practical Handbook for Small-Gauge Vitrectomy: A Step-By-Step Introduction to Surgical TechniquesFrom EverandPractical Handbook for Small-Gauge Vitrectomy: A Step-By-Step Introduction to Surgical TechniquesNo ratings yet
- Legal and Ethical Issues of Euthanasia: Argumentative Essay: October 2013Document10 pagesLegal and Ethical Issues of Euthanasia: Argumentative Essay: October 2013Rika DasNo ratings yet
- Pars Plana Vitrectomy PDFDocument12 pagesPars Plana Vitrectomy PDFAvluz AdiansuhNo ratings yet
- Tugas Bahasa Inggris 2Document2 pagesTugas Bahasa Inggris 2Avluz AdiansuhNo ratings yet
- 1 PBDocument6 pages1 PBAvluz AdiansuhNo ratings yet
- Fulltext PDFDocument21 pagesFulltext PDFAvluz AdiansuhNo ratings yet
- MMYazisipdf JNS 776Document12 pagesMMYazisipdf JNS 776Guz CaemmNo ratings yet
- Pars Plana Vitrectomy PDFDocument12 pagesPars Plana Vitrectomy PDFAvluz AdiansuhNo ratings yet
- 1499 FullDocument8 pages1499 FullAvluz AdiansuhNo ratings yet
- 1499 FullDocument8 pages1499 FullAvluz AdiansuhNo ratings yet
- 10 1111@jphp 12812Document11 pages10 1111@jphp 12812Avluz AdiansuhNo ratings yet
- 10 1111@jphp 12812Document11 pages10 1111@jphp 12812Avluz AdiansuhNo ratings yet
- 10 1111@jphp 12812Document11 pages10 1111@jphp 12812Avluz AdiansuhNo ratings yet
- 1 SMDocument7 pages1 SMAvluz AdiansuhNo ratings yet
- Uji Aktivitas Antidiare Ekstrak Etanol 70% Kulit Buah Jengkol ( (Benth.) I.C.Nielsen) Terhadap Mencit Jantan Yang Diinduksi Oleum RiciniDocument6 pagesUji Aktivitas Antidiare Ekstrak Etanol 70% Kulit Buah Jengkol ( (Benth.) I.C.Nielsen) Terhadap Mencit Jantan Yang Diinduksi Oleum RiciniNovianHendroNo ratings yet
- Analytical Exposition TextDocument1 pageAnalytical Exposition TextAvluz AdiansuhNo ratings yet
- bb10 Chap2 PDFDocument20 pagesbb10 Chap2 PDFAvluz AdiansuhNo ratings yet
- Assessment Form Research Paper Congress Competition Exit MRC 2017Document1 pageAssessment Form Research Paper Congress Competition Exit MRC 2017Avluz AdiansuhNo ratings yet
- Brochure Langkisau Resort Hotel & RestaurantDocument2 pagesBrochure Langkisau Resort Hotel & RestaurantAvluz AdiansuhNo ratings yet
- BirdbrainDocument1 pageBirdbrainplastoneNo ratings yet
- Ucm 467056Document47 pagesUcm 467056Harmit Singh Bindra100% (1)
- Analytical Exposition TextDocument1 pageAnalytical Exposition TextAvluz AdiansuhNo ratings yet
- Antimalarial Activity of Papaya Leaf ExtractsDocument5 pagesAntimalarial Activity of Papaya Leaf ExtractsFaris AgazaliNo ratings yet
- Descriptive TextDocument5 pagesDescriptive TextAvluz AdiansuhNo ratings yet
- The Point of ImmunizationDocument1 pageThe Point of ImmunizationAvluz AdiansuhNo ratings yet
- IV Fluids: Prepared By: Via Mae G. DaralDocument29 pagesIV Fluids: Prepared By: Via Mae G. DaralMARIANN JEAN ANDREA CULANAG MATALINESNo ratings yet
- Nursing Skills Checklist FinalDocument6 pagesNursing Skills Checklist Finalapi-380356845No ratings yet
- The Different Types of IV Sets and Their UsesDocument1 pageThe Different Types of IV Sets and Their UsesPatricia VasquezNo ratings yet
- Tranaxemic AcidDocument6 pagesTranaxemic AcidCharan Teja ReddyNo ratings yet
- Skills Modules 3.0 Checklist Intravenous Medications: Administering Piggyback Intermittent Intravenous MedicationsDocument2 pagesSkills Modules 3.0 Checklist Intravenous Medications: Administering Piggyback Intermittent Intravenous MedicationsKarima JonesNo ratings yet
- Common Medical AbbreviationsDocument13 pagesCommon Medical Abbreviationsohio770No ratings yet
- CALCULATING IV DRIP RATESDocument15 pagesCALCULATING IV DRIP RATESIvan DanusaputraNo ratings yet
- Nursing Orientation Program Intravenous TherapyDocument45 pagesNursing Orientation Program Intravenous TherapyMarianne LayloNo ratings yet
- How to Infuse HYQVIA with a PumpDocument38 pagesHow to Infuse HYQVIA with a PumpShaya NirenbergNo ratings yet
- NCLEX-RN/HAAD/Prometric Examinations ReviewDocument11 pagesNCLEX-RN/HAAD/Prometric Examinations ReviewmonmonNo ratings yet
- JBDS Pregnancy 201017Document36 pagesJBDS Pregnancy 201017Majid KhanNo ratings yet
- KCL Pharmacy Society Calculations GuideDocument48 pagesKCL Pharmacy Society Calculations GuideJasvir SamraNo ratings yet
- ATLS 9th Pre-Test 1 - 1Document12 pagesATLS 9th Pre-Test 1 - 1a.e.noushiNo ratings yet
- Pre & Post Operative Nursing CareDocument33 pagesPre & Post Operative Nursing CareJohnmark SimonNo ratings yet
- Neonatal Infusion Therapy - HandoutDocument9 pagesNeonatal Infusion Therapy - HandoutAde PurnaNo ratings yet
- Sodium Nitroprusside Theory and PracticeDocument17 pagesSodium Nitroprusside Theory and PracticesourabhmoonNo ratings yet
- NCM 417 - Final Exam 2015Document12 pagesNCM 417 - Final Exam 2015Mae DacerNo ratings yet
- Iron Deficiency Anaemia: Pathophysiology, Assessment, Practical ManagementDocument9 pagesIron Deficiency Anaemia: Pathophysiology, Assessment, Practical ManagementSantiago López JosueNo ratings yet
- Crane NutritionDocument8 pagesCrane NutritionMarvin MonterrosoNo ratings yet
- Medadv CatalogDocument39 pagesMedadv CatalogFrank PereiraNo ratings yet
- Sustainable Design of Mobile Transilluminator Vein Finder DeviceDocument12 pagesSustainable Design of Mobile Transilluminator Vein Finder DeviceTohid TalefifuNo ratings yet
- ATSP Booklet 2019 FinalDocument24 pagesATSP Booklet 2019 FinalShreya BNo ratings yet
- SickKids NICU Nutrition Guidelines July 2020Document2 pagesSickKids NICU Nutrition Guidelines July 2020Shuaib KauchaliNo ratings yet
- Dka ChartDocument2 pagesDka Chartmrsothea100% (1)
- IDNT Interv v3Document1 pageIDNT Interv v3zulfaNo ratings yet
- The Many Benefits of Coconut Water KefirDocument3 pagesThe Many Benefits of Coconut Water KefirMa Geobelyn LopezNo ratings yet