Professional Documents
Culture Documents
Bacaaaa PDF
Bacaaaa PDF
Uploaded by
Ulen MahuletteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacaaaa PDF
Bacaaaa PDF
Uploaded by
Ulen MahuletteCopyright:
Available Formats
DIABETICMedicine
DOI: 10.1111/j.1464-5491.2009.02866.x
Review Article
Peripheral arterial disease in diabetes—a review
E. B. Jude, I. Eleftheriadou* and N. Tentolouris*
Tameside General Hospital, Ashton-Under-Lyne, UK and *Athens University Medical School, Athens, Greece
Accepted 23 September 2009
Abstract
Diabetic patients are at high risk for peripheral arterial disease (PAD) characterized by symptoms of intermittent
claudication or critical limb ischaemia. Given the inconsistencies of clinical findings in the diagnosis of PAD in the
diabetic patient, measurement of ankle-brachial pressure index (ABI) has emerged as the relatively simple, non-invasive
and inexpensive diagnostic tool of choice. An ABI < 0.9 is not only diagnostic of PAD even in the asymptomatic patient,
but is also an independent marker of increased morbidity and mortality from cardiovascular diseases. With better
understanding of the process of atherosclerosis, avenues for treatment have increased. Modification of lifestyle and
effective management of the established risk factors such as smoking, dyslipidaemia, hyperglycaemia and hypertension
retard the progression of the disease and reduce cardiovascular events in these patients. Newer risk factors such as
insulin resistance, hyperfibrinogenaemia, hyperhomocysteinaemia and low-grade inflammation have been identified,
but the advantages of modifying them in patients with PAD are yet to be proven. Therapeutic angiogenesis, on the
other hand, represents a promising therapeutic adjunct in the management of PAD in these patients. Outcomes after
revascularization procedures, such as percutaneous transluminal angioplasty and surgical bypasses in diabetic
patients, are poorer, with increased perioperative morbidity and mortality compared with that in non-diabetic
patients. Amputation rates are higher due to the distal nature of the disease. Efforts towards increasing
awareness and intensive treatment of the risk factors will help to reduce morbidity and mortality in diabetic patients
with PAD.
Diabet. Med. 27, 4–14 (2010)
Keywords ankle-brachial pressure index, diabetes, peripheral arterial disease, risk factors, treatment
Abbreviations ABI, ankle-brachial pressure index; bFGF, basic fibroblast growth factor; cAMP, cyclic adenosine-3¢,5¢-
monophosphate; CRP, C-reactive protein; DM, diabetes mellitus; HGF, hepatocyte growth factor; HTN, hypertension;
LDL, low-density lipoprotein; MI, myocardial infarction; NGF, nerve growth factor; NO, nitric oxide; PAD, peripheral
arterial disease; PAI, plasminogen activator inhibitor; PCTA, percutaneous transluminal balloon angioplasty; SBP,
systolic blood pressure; T1DM, Type 1 diabetes mellitus; T2DM, Type 2 diabetes mellitus; TcPO2, transcutaneous
partial pressure of oxygen; UKPDS, United Kingdom Prospective Diabetes Study; VEGF, vascular endothelial growth
factor; vWF, von Willebrand factor
ischaemic ulceration or gangrene. Diabetic patients with PAD are
Introduction
at high risk of increased morbidity and mortality from
Peripheral arterial disease (PAD) is a group of disorders cardiovascular diseases. Considering that between 120 and
characterized by narrowing or occlusion of the arteries 140 million people suffer from diabetes mellitus (DM)
resulting in gradual reduction of blood supply to the limbs. worldwide and that diabetic patients are at excess risk of
Patients with PAD may be asymptomatic or may develop developing PAD [1], the implications of the problem are
symptoms of intermittent claudication or symptoms of critical enormous.
limb ischaemia, characterized by pain in the peripheries at rest, The importance of PAD in DM is several-fold. PAD may be
asymptomatic until it reaches an advanced stage [2]. It presents at
an earlier age and progresses more rapidly than in non-diabetic
Correspondence to: Edward B. Jude, MD, Tameside General
Hospital, Ashton-Under-Lyne, Lancashire OL6 9RW, UK. patients. It is usually more severe in extent [3] and often not all
E-mail: edward.jude@tgh.nhs.uk patients may be offered a revascularization procedure when
ª 2010 The Authors.
4 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
Review article DIABETICMedicine
needed. Furthermore, the outcome after revascularization
procedures is poorer and many patients progress to a major
2 ⁄ 1000 at 30 years of age
6 ⁄ 1000 at 60 years of age
7 ⁄ 1000 at 70 years of age
amputation [3]. The presence of PAD is in itself an independent
17.6 ⁄ 1000 for women
8.4 ⁄ 1000 for women
21.3 ⁄ 1000 for men
12.6 ⁄ 1000 for men
factor for increased mortality due to associated cardiovascular
and cerebrovascular diseases [1]. Finally, early detection of PAD
helps in risk factor modification, which reduces progression and
Incidence
13 ⁄ 1000
improves outcome.
NA
NA
NA
NA
NA
Epidemiology
20% in age ‡ 75 years
3% in age < 60 years
The true incidence of PAD is difficult to ascertain and
estimates can be erroneous due to several reasons. A
significant number of patients with PAD are unlikely to
Prevalence
complain of intermittent claudication because the presence of
peripheral neuropathy may mask the symptoms of claudication
17.3%
38.0%
23.5%
33.0%
8.0%
8.7%
NA
NA
[2]. Furthermore, the method used to diagnose PAD
[symptoms of claudication, palpation of peripheral pulses or
ankle-brachial pressure index (ABI)] has a major influence on
Number of
statistics. The results of various clinical trials [4–11] on the
patients
1073
1084
5209
48
173
864
213
642
586
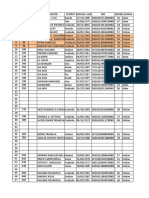
prevalence and incidence of PAD in DM are summarized in
Table 1.
extremity amputation
IC, foot ulcer, lower
Diagnostic criterion
non-invasive testing
Prevalence
IC or pulse deficit
IC, pulse deficit,
Large population-based studies have shown that the prevalence
Pulse deficit
ABI < 0.9
ABI < 0.9
ABI < 0.9
ABI < 0.9
of PAD is higher in patients with DM. The Framingham study [4]
showed that there was a 3.5- and 8.6-fold excess risk among men
IC
and women, respectively, of developing PAD in patients with
Table 1 Epidemiological data for peripheral arterial disease in patients with and without diabetes mellitus
DM. In the Rochester study the prevalence of PAD at the time of
Type 1 and Type 2 diabetes mellitus
Type 1 and Type 2 diabetes mellitus
Type 1 and Type 2 diabetes mellitus
Type 1 and Type 2 diabetes mellitus
diagnosis of DM was 8% between the years 1945 and 1969,
while it was 10.5% in 1970 [5]. The Hoorn study found that the
ABI, ankle-brachial pressure index; IC, intermittent claudication; NA, not available.
prevalence of ABI < 0.9 in individuals with normal glucose
(26% with diabetes mellitus)
tolerance was 7% and increased to 20.9% in diabetic patients
Type 2 diabetes mellitus
Type 1 diabetes mellitus
Type 1 diabetes mellitus
[6], while a pilot study found a prevalence of asymptomatic PAD
General population
General population
of 33% [7].
One study showed that the type of DM does not affect the
Population
prevalence of PAD, identical prevalences being found in
patients with Type 1 (T1DM) and Type 2 DM (T2DM) [8].
However, another study found a much higher prevalence of
PAD (23.5%) in patients with T2DM than in those with
T1DM (8.7%) [9].
1995
1984
1992
1992
1999
1985
1985
2002
1945–1969
Years
Incidence
In the Rochester study [5], the cumulative incidence of PAD in
USA, Minnesota
DM was 21.3 ⁄ 1000 person-years for men and 17.6 ⁄ 1000
North America
Hoorn study
Framingham
person-years for women. In this study, the cumulative
Australia
incidence of PAD was 15% 10 years after the diagnosis of
Country
DM, which increased to 45% 20 years later. In the Framingham
UK
UK
UK
UK
study [4] the incidence of PAD in the diabetic population was
12.6 ⁄ 1000 person-years for men and 8.4 ⁄ 1000 person-years for
References
women, while the figures in non-diabetic people were 3.3 and
1.1 ⁄ 1000 person-years for men and women, respectively.
10
11
5
6
8
9
9
7
One single study examined the incidence of PAD in patients
4
with T1DM [11]; the incidence was 13 events ⁄ 1000 person-
ª 2010 The Authors.
Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14 5
DIABETICMedicine Peripheral arterial disease in diabetes • E. B. Jude et al.
years with no gender difference and was similar to that in patients increase in SBP was associated with a 25% increased risk for
with T2DM. development of PAD at the end of 18 years [17]. Tight BP control
was also associated with lower prevalence of PAD at long-term
follow-up in the UKPDS [19]. Other factors have also been
Amputation rate
associated independently with PAD in patients with both T1DM
Diabetic patients have increased risk of lower-extremity and T2DM. These are summarized in Table 2.
amputations in comparison with non-diabetic subjects and
there is no convincing evidence that revascularization
Pathogenesis of PAD in diabetes
procedures are effective in preventing amputation [3].
Moreover, the severity of PAD in DM assessed Vascular disease in DM affects both the microcirculation and
angiographically has been associated with major amputations large vessels. Microangiopathy is characterized by involvement
[12]. of blood vessels at the level of the arterioles and capillaries,
causing thickening of the basement membrane and making it
more permeable to plasma solutes. PAD in diabetic patients is
Mortality
due to the angiopathy affecting the medium-sized arteries
Large population-based studies have shown that diabetic predominantly and is due to the abnormal metabolic state that
patients with PAD have a three- to four-fold increased prevails in DM. The most important metabolic aberrations are
mortality compared with healthy individuals [6], and patients chronic hyperglycaemia, insulin resistance and dyslipidaemia,
with critical limb ischaemia and DM have a shorter amputation- which render the arteries susceptible to atherosclerosis. Various
free survival period than patients with critical ischaemia but types of affected cells work in tandem to create atheroma, the
without DM [13]. The 5-year mortality in diabetic patients with hallmark of atherosclerosis. In brief, some of the cellular events in
critical limb ischaemia is 30% [14]. the process of atherosclerosis are as follows.
DM impairs endothelial function, through hyperglycaemia,
excess circulating free fatty acids, increased oxidative stress and
Risk factors for PAD in diabetes
inhibition of endothelial nitric oxide (MO) synthase. Thus, there is
Various risk factors have been described for the increased a decrease in NO and prostacyclin and an increase in endothelin-I
predisposition to the development of PAD in DM. Many studies and angiotensin-II, which are potent vasoconstrictors [28].
[4,5,9–11,15–27] have attempted to resolve this complicated DM augments the process of atheroma formation. There is an
issue by comparing diabetic patients with PAD with non-diabetic increase in plasma and cellular concentration of histamine, which
patients with PAD and between diabetic patients with and may contribute to the increased endothelial permeability in
without PAD. diabetic patients with PAD [28]. The migration of T lymphocytes
Increasing age correlates strongly with PAD in patients with into the intima, their activation and secretion of cytokines is
both T1DM and T2DM [9]. Although in the Framingham study enhanced. Monocytes ingest oxidized low-density lipoprotein
[4] much of the excess risk associated with DM was found in (LDL) molecules on reaching the subendothelial space and
those < 75 years old, the Framingham-offspring study found that become foam cells, which lead to fatty streak formation, the
for each 10 years of age, the odds ratio of PAD was 2.6 [15]. precursors of the atheroma. The atheromatous plaque so formed
In the Framingham and Rochester studies, the incidence of is unstable as diabetic endothelial cells secrete cytokines that
PAD was higher in men than in women [4,5]. Diabetic women inhibit production of collagen by smooth muscle cells [29]. They
are more likely to have PAD compared with non-diabetic women also secrete metalloproteinases, which break down the collagen
of similar age [16]. While premenopausal women in the general in the fibrous cap of atheromas, leading to a tendency to plaque
population enjoy relative protection from atherosclerosis due to rupture and thrombus formation [30]. Endothelial cells produce
their hormonal status, DM blunts the benefit of the female gender increased amounts of tissue factor, a major procoagulant factor.
[10], especially in the elderly group. Migration of medial vascular smooth muscle cells into the intimal
In the United Kingdom Prospective Diabetes Study (UKPDS) fatty streak lesion is enhanced. These cells then produce
[17], duration and degree of hyperglycaemia were associated extracellular matrix, aggravating atheroma formation.
with an increased risk for incident PAD independently of other Hyperglycaemia also increases intracellular concentration of
factors. Each 1% increase in HbA1c was associated with a 28% glucose in platelets as its uptake is non-insulin dependent. This
excess risk for incident PAD at the end of 18 years. In another leads to decreased production of platelet-derived NO and excess
study, the odds ratio of PAD was 28.9 and 51.1 for a DM production of oxygen free radicals [29].
duration of 20–29 years and > 30 years, respectively, in patients Calcium haemostasis regulating platelet shape, secretion,
with T1DM, while it was 3.8 and 4.3 for a DM duration of 10– aggregation and thromboxane production is disturbed in DM
19 years and > 20 years, respectively, in patients with T2DM [31]. Platelet expression of receptor proteins for von Willebrand
[18]. factor (vWF) and fibrin products is increased in DM, which could
The UKPDS found that increased systolic blood pressure (SBP) be the result of decreased production of the antiaggregants NO
was an independent risk factor for PAD and each 10-mmHg and prostacyclin, and increased production of fibrinogen and
ª 2010 The Authors.
6 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
Review article DIABETICMedicine
Table 2 Risk factors for peripheral arterial disease in diabetes mellitus
References Risk factor Type of diabetes mellitus
1,4,5,9,15,17,28 Increasing age 1, 2
4,5,10 Male gender 2
1,5,11,17,18,21,28 Duration of diabetes mellitus 1, 2
17,28 Degree of hyperglycaemia 2
4,15,17 Smoking 2
4,11,15,17,19 Hypertension 1, 2
9,11,15,17,18,20,21 Dyslipidaemia 1, 2
22 Increased serum lipoprotein (a) levels 1, 2
23 Reduced serum apolipoprotein (a) levels 2
9,15,21 Obesity, central body fat distribution 2
11,24 Insulin resistance 1, 2
1,15 Increased serum fibrinogen levels 2
25 Hyperhomocysteinaemia Non-diabetics
9,11,18 Microalbuminuria 1, 2
26 Increased levels of von Willebrand factor 2
26 Increased levels of thrombin–antithrombin complexes 2
27 Increased levels of intercellular adhesion molecules 2
platelet activators such as thrombin and vWF [32]. This increase PARTNERS programme [34] showed that 48% of the 6369
in intrinsic platelet activity contributes to the state of enhanced patients, of whom 41% had DM, were aware of their condition.
thrombotic potential. Some data suggest that patients with DM develop more
Diabetic patients have impaired fibrinolytic activity [1]. In symptomatic forms of PAD such as intermittent claudication,
addition, there are increased circulating levels of procoagulants foot ulcers and critical limb ischaemia symptoms [35], while
such as tissue factor, factor VII and decreased levels of other studies have found no difference in the frequency of
anticoagulants such as antithrombin-III and protein C, thus symptoms between diabetic and non-diabetic patients [9].
favouring a tendency to coagulation, impaired fibrinolysis and Diabetic patients with decreased pain perception due to
persistence of thrombi [33]. peripheral neuropathy may delay the recognition of PAD [2].
Patients with impaired glucose tolerance have elevated levels of Peripheral neuropathy and PAD are known risk factors for
C-reactive protein (CRP), which is strongly associated with PAD. foot ulceration [36]; almost 40–60% of diabetic patients with
CRP inhibits endothelial NO synthase and stimulates the foot ulcers have PAD, which is associated with a higher
production of procoagulant tissue factor, leucocyte adhesion amputation rate and mortality [36]. With impaired circulation
molecules, chemotactic substances and plasminogen activator and sensation, foot ulceration and infection develop commonly.
inhibitor (PAI)-1 and thus contributes to a thrombotic Development of dry gangrene is the end-stage presentation of
environment [28]. PAD, indicating that in the absence of a revascularization
procedure a major amputation is unavoidable.
Diabetic patients with PAD have poorer lower extremity
Profile of PAD in diabetes
function compared with non-diabetic subjects with PAD; they
The pattern of PAD involvement differs between diabetic and have shorter mean walking distance and slower fast pace
non-diabetic patients. Diabetic patients with PAD commonly velocities than non-diabetic patients with PAD. This was due
show involvement of the arteries below the knee, especially at to the associated peripheral neuropathy, differences in exertional
the tibial and peroneal arteries, and involvement of the leg symptoms and greater cardiovascular disease in diabetic
profunda femoris [3]. Also, it is more commonly symmetrical patients [37].
and multi-segmental, and stenoses can be seen even in the
collateral vessels. Non-diabetic patients with PAD usually
Diagnosis of PAD
present with single, unilateral, proximal arterial involvement.
Some, but not all studies, reported that PAD progresses more A history of intermittent claudication or absence of peripheral
rapidly in DM. pulses on palpation is unreliable for detection of PAD. The
dorsalis pedis pulse is absent congenitally in about 10–15% of the
population. However, a history of claudication, presence of
Clinical presentation
bruits proximally and findings of chronic ischaemia in the
The majority of diabetic patients with PAD are asymptomatic peripheries such as cold feet, pallor on limb elevation and
(up to 75%) when ABI < 0.9 is the criterion for the diagnosis. The dependent rubor, trophic skin changes and distal gangrene are all
ª 2010 The Authors.
Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14 7
DIABETICMedicine Peripheral arterial disease in diabetes • E. B. Jude et al.
diagnostic of PAD. Peripheral Doppler ultrasonography, colour duplex ultrasound and magnetic resonance angiography help in
duplex scanning, ABI measurement, plethysmography, localizing PAD lesions and planning intervention. Traditional or
transcutaneous oximetry [transcutaneous partial pressure of digital subtraction angiography remains the gold standard
oxygen (TcPO2)] and magnetic resonance angiography are the against which all other diagnostic modalities should be
battery of non-invasive tests currently available. compared. It is to be used when a vascular intervention is
An ABI < 0.9 has been used as a criterion for diagnosis in most planned [1]. A proposed protocol for the diagnosis of PAD in
studies on PAD, because of its simplicity and non-invasiveness patients with and without DM is depicted in Fig. 1.
(Table 3). However, studies on resting ABI and post-exercise ABI
have been conflicting. An arteriographically controlled study
Treatment
showed that significant stenoses (> 50%) were present in diabetic
patients with palpable foot pulses and ABI > 1 [12]. Questions The aims in the management of the diabetic patient with PAD are
have been raised about the reliability of ABI in the diagnosis of to improve symptoms and to prevent cardiovascular morbidity
PAD as it was found that ABI was high in hypotensive or and mortality. Treatment of PAD can be considered in three
normotensive patients and low in hypertensive patients [38]. The stages: lifestyle and risk factor modifications, drug therapy and
sensitivity and specificity of ABI were 70.6% and 88.5%, vascular interventions.
respectively, in patients with PAD diagnosed by colour duplex
ultrasound [1].
Lifestyle modifications
Measurement of pre- and post-exercise ABI is currently
recommended for the screening and diagnosis of PAD, until Lifestyle modifications are the first mode of therapy as metabolic
more reliable diagnostic tools become available. The ABI and lipid abnormalities improve with smoking cessation,
measured with ankle SBP just before and after 5 min of exercise, weight loss and dietary modifications.
exercise may reveal significant PAD before resting ABI Cigarette smoking is the single most important risk factor for
becomes abnormal. A drop in ankle BP > 20% indicates the development of atherosclerosis and smoking cessation may
significant PAD, while an absence of such a fall virtually rules halt the progression of disease [28]. Smoking increases the risk
out PAD [1]. Medial arterial calcification (Mönckeberg’s and reduces the success of peripheral vascular intervention [15].
sclerosis), found in up to 47% of patients with T1DM in one Physical exercise improves exercise tolerance and most of the
study [39], is common in patients with DM or renal failure and in studies have shown at least a doubling in walking distance [41].
heavy smokers and this can falsely raise ABI to values > 1.3 [1], Noteworthy, these changes were found without significant
masking the presence of PAD [40]. A recent study suggested that improvement in blood flow, but exercise increases
diabetic patients with an ABI ‡ 1.4 should be considered as cardiovascular fitness, oxidative enzyme activities, NO
PAD-equivalent [40]. Medial arterial calcification may also production and insulin sensitivity [29], enhances utilization of
render the artery non-compressible and hence ankle BP may not fatty acids in calf muscles, and improves walking biomechanics
be assessable. However, the presence of calcification is not a as well as blood rheology. Exercise training leads to modest
measure of the severity of the disease or the extent of reductions in BP, cholesterol and glucose levels.
stenosis ⁄ occlusion. An alternative approach in these patients is
to measure the great toe BP using a strain gauge sensor or a
Risk factor modifications
photoplethysmograph [2]. Determination of TcPO2 may help
assess healing of ischaemic skin lesions, but is not reliable for the Glycaemic control
diagnosis of PAD in DM [2]. Continuous-wave Doppler may There is no conclusive evidence to suggest that optimal glycaemic
identify occlusive PAD but is a qualitative test only. Colour control lowers the risk of PAD [42]. In the presence of an
Table 3 The role of ankle-brachial pressure index (ABI) for the diagnosis of peripheral arterial disease (PAD) in patients with diabetes mellitus
Advantages References Disadvantages References
Simple 1,28 ABI ‡ 1.4 (medial arterial calcification) unreliable, 28,40
should be considered as PAD equivalent
Non-invasive 1,28 Arteriographically evident stenoses > 50% 12
with resting ABI > 1
Reproducible 1,28 › ABI in hypotensive or normotensive patients 38
fl ABI in hypertensive patients
Sensitivity of 90% and specificity 98% 1,28
for the detection of haemodynamically
significant (> 50%) stenosis in leg arteries
Post-exercise ABI: drop of ankle-blood 1
pressure > 20% indicates PAD
ª 2010 The Authors.
8 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
Review article DIABETICMedicine
FIGURE 1 Proposed protocol for the diagnosis of peripheral arterial disease (PAD) in patients with and without diabetes mellitus. Reprinted with
permission from N Engl J Med 2001; 344: 1608–1621. ABI, ankle-brachial index; TBI, toe-brachial index.
increased risk of cardiovascular events with increasing levels of reduced major cardiovascular events by 37%, irrespective of
glycaemia [17] and hyperglycaemia being the important pretreatment LDL-cholesterol levels [46].
metabolic factor in atherogenesis, optimal glycaemic control
would be sensible in patients with PAD. Medications that Hypertension
improve insulin resistance may have advantages over other Optimal control of hypertension (HTN) to 130 ⁄ 80 mmHg
hypoglycaemic agents, since insulin resistance is a risk factor for reduces stroke and death rates. Long-term tight BP control was
PAD. However, metformin was not superior to sulphonylureas associated with a 50% lower risk for PAD in the UKPDS with no
or insulin in the prevention of PAD in DM [42]. In the difference between the primary medications (captopril and
PROACTIVE study only patients without PAD at baseline atenolol) used for the management of HTN [19]. The HOPE
benefited from treatment with pioglitazone [43]. study [47] showed that ramipril decreased the rates of
myocardial infarction (MI), stroke and death in diabetic
Dyslipidaemia patients with cardiovascular disease. The reduction of
Aggressive management of dyslipidaemia in patients with DM cardiovascular morbidity and mortality in patients with PAD
and PAD is warranted and the primary aim is LDL-cholesterol was 25%. A recent study also showed that intensive BP control
levels < 2.6 mmol ⁄ l or even lower (< 1.8 mmol ⁄ l) [28]. Statins reduces the risk for cardiovascular events in diabetic patients
are the treatment of choice in such patients. The 4S-Study [44] with PAD [48].
showed that simvastatin reduced claudication in patients with There have been no reports of worsening of symptoms after
PAD, although there were no specific data regarding diabetic control of HTN in patients with PAD. A meta-analysis concluded
patients. The Heart Protection Study showed that lowering LDL- that b-blockade was not associated with reduced treadmill
cholesterol with simvastatin reduces cardiovascular mortality walking performance in PAD patients with intermittent
and morbidity in diabetic patients by almost 25% [45], while the claudication [49]. Currently, it is recommended that b-blockers
Collaborative Atorvastatin Diabetes Study showed that be used as and when indicated, except in patients with critical
aggressive treatment with atorvastatin in diabetic patients limb ishaemia.
ª 2010 The Authors.
Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14 9
DIABETICMedicine Peripheral arterial disease in diabetes • E. B. Jude et al.
cAMP inhibits thromboxane A2 production and platelet
Drug therapy aggregation by inhibiting phospholipase and cyclooxygenase.
Antiplatelet agents Cilostazol induces vasodilation by inhibiting calcium-induced
Antiplatelet agents are of benefit in patients with PAD, as platelet contractions of smooth muscle cells.
hyperactivity leads to formation of thrombus at sites of Treatment with cilostazol increases pain-free and maximal
atherosclerotic plaques. Antiplatelet agents produce treadmill walking distances and improves quality of life
angiographic improvement, increase walking distance, reduce significantly more than pentoxifylline [54]. A pooled analysis
the need for vascular intervention, improve patency rates after of eight Phase III trials of 436 diabetic patients with intermittent
vascular interventions and reduce cardiovascular mortality. The claudication showed that patients who received cilostazol
Anti-platelet Trialists’ Collaboration has shown that an increased their maximal walking distances, initial claudication
antiplatelet agent, usually aspirin, reduces cardiovascular distance and absolute claudication distance more than those with
deaths by 25% in patients with symptomatic atherosclerotic placebo [55]. Response rates and safety data were similar in
disease. This reduction in death rates was 18% in the subset of patients with and without DM.
patients with intermittent claudication [50]. However, these Cilostazol is contraindicated in patients with congestive heart
studies have not reported data separately in diabetic patients with failure and severe hepatic or renal impairment. Cilostazol is a
PAD. promising therapy for patients with claudication and DM among
Aspirin alone is as effective as aspirin combined with the limited options available for these patients [2].
dipyridamole, sulphinpyrazone or ticlopidine in preventing The above drugs for intermittent claudication are
graft occlusion or reduction in risk of death from recommended in the event of failure of lifestyle modifications.
cardiovascular events [51]. However, aspirin with dipyridamole Clinical trials have shown no efficacy of vasodilator drugs such as
resulted in least progression of PAD compared with aspirin alone papavarine in PAD and they are not recommended.
or placebo in an arteriographically controlled trial [52]. A dose of
325 mg did not show any additional benefit over a dose of 75 mg. Drugs of possible benefit
Ticlopidine, an antiplatelet thienopyridine agent, improves Iloprost, a prostacyclin derivative, reduces levels of PAI-1 (which
clinical outcomes in patients with PAD but is not recommended is associated with increased fibrinogen levels and
because of adverse effects (neutropenia and thrombotic hypercoaguability) and also increases walking capacity in
thrombocytopenic purpura). diabetic patients with PAD [56]. Further studies are required
Clopidogrel is a second-generation thienopyridine drug with before iloprost could be recommended for use.
fewer side-effects. The CAPRIE study [53] compared
clopidogrel with aspirin in > 19 000 patients and found that Critical leg ischaemia
the overall decrease in the primary endpoints of MI, stroke or In patients with critical leg ischaemia a revascularization
vascular deaths was 8.7%, and clopidogrel decreased the end- procedure should always be considered. In addition,
point of MI by 19.2% over that of aspirin irrespective of the appropriate foot care, sufficient footwear, debridement of foot
primary cardiovascular disease. The study also showed that in ulcers, non-adherent dressings and treatment of infections with
the subgroup (about 30% of the 19 000 patients) with PAD at antibiotics are essential for preventing amputation [1].
baseline, those who received clopidogrel had 24% lower
primary end-points of MI, stroke or vascular death in Therapeutic angiogenesis
comparison with aspirin. However, there was no particular Therapeutic angiogenesis represents a novel approach to increase
reference to DM. blood flow to ischaemic tissues by induction of a collateral
vascular network. This can be achieved by administration of
Intermittent claudication angiogenic factors such as vascular endothelial growth factor
Two agents are available for the treatment of intermittent (VEGF), basic fibroblast growth factor (bFGF), hepatocyte
claudication: pentoxifylline and cilostazol. Pentoxifylline, a growth factor (HGF) and nerve growth factor (NGF). Two
methylxanthine derivative is a haemorheological agent that modes of angiogenesis are emerging; the first is the topical (into
reduces blood viscosity. It also has antiplatelet action and reduces the muscles or arteries of the lower limbs) administration of the
serum fibrinogen levels. Results of pentoxifylline in claudication recombinant growth factor protein, and the second is
varied in different studies, with some suggesting favourable incorporation of genes encoding angiogenic growth factors into
results in diabetic patients but most demonstrating a modest a vector (virus or plasmid) to deliver DNA to human cells [57].
improvement in symptoms suggesting that pentoxifylline is not Topical, rather than intravenous, administration of these factors
justified for routine use [28]. Pentoxifylline may benefit patients is preferred because systemic toxicity is low and higher
with severe claudication symptoms and those in whom exercise concentrations of the growth factors are achieved locally.
and ⁄ or cilostazol is not effective or is contraindicated. Intramuscular administration of VEGF and intra-arterial
Cilostazol, a quinolone derivative, is a selective administration of bFGF resulted in clinical improvement.
phosphodiesterase-III inhibitor that suppresses cyclic adenosine- Importantly, both treatments were safe and well tolerated [57].
3¢,5¢-monophosphate(cAMP)degradation. Increasedintraplatelet Treatment with bFGF gene therapy by intramuscular injection
ª 2010 The Authors.
10 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
Review article DIABETICMedicine
FIGURE 2 Proposed protocol for the management of peripheral arterial disease (PAD) in patients with diabetes mellitus (DM). AE, adverse effects; VEGF,
vascular endothelial growth factor; bFGF, basic fibroblast growth factor; HGF, hepatocyte growth factor; NGF, nerve growth factor; PCTA, percutaneous
transluminal balloon angioplasty; BG, bypass grafting.
into thigh and calf muscles in patients with severe limb ischaemia transplanted into the lower limb muscles. All indices of blood
resulted in improvement in clinical outcomes [57]. However, flow improved, while pain was reduced in 87% of the patients
only a few patients with DM were included in these studies and [58]. Although clinical experience is limited, stem cell therapy
we must wait to gain confidence in the efficacy of these treatments represents a promising therapeutic adjunct in the management of
in patients with DM. HGF and NGF promote neovascularization PAD and further research is needed.
in experimental DM [57] and experience in humans is limited. It is early to conclude on the position of the novel therapies in
Human bone-marrow cells contain stem cells that have the the management of PAD in DM and more data from randomized
potential for differentiation into a variety of tissues, including controlled trials are necessary to establish their efficacy and
endothelium. Transplantation of autologous bone-marrow stem safety. However, given that the tibial arteries are predominantly
cells in 10 patients with severe PAD into the common femoral involved in diabetes, and that revascularization procedures are
artery and the thigh and calf muscles resulted in clinical not usually performed at this site, their indication may be for the
improvement and increase in ABI. In another study, autologous management of severe limb ischaemia not amenable to
peripheral blood stem cells in 62 patients with severe PAD were revascularization surgery. They may also be useful for the
ª 2010 The Authors.
Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14 11
DIABETICMedicine Peripheral arterial disease in diabetes • E. B. Jude et al.
management of PAD in patients at high surgical risk due to severe However, the outcome after amputation in diabetic patients with
comorbidities. PAD is poorer. The 3-year survival after an amputation is < 50%
and a second amputation is exceedingly common after the first;
survival is lower than in non-diabetic subjects undergoing
Revascularization procedures
successful revascularization [3]. A proposed protocol for the
Classically, the indications for a revascularization procedure in management of PAD in patients with DM is depicted in Fig. 2.
PAD are disabling claudication affecting quality of life after
medical therapy has failed to improve symptoms, and critical
Summary
limb ischaemia symptoms. The revascularization procedures
currently available are percutaneous transluminal balloon Patients with DM are prone to develop PAD. PAD begins
angioplasty (PCTA) with or without stenting and surgical earlier, progresses more rapidly and is more commonly
revascularization by means of bypass grafting using asymptomatic in DM. Distal arterial involvement of the tibial
autogenous vein or a synthetic graft or endarterectomy for and peroneal arteries is the predominant pattern. Lifestyle
localized lesions. modifications are of benefit. Drug therapy is advised in patients
The number of revascularization procedures for PAD is about who do not respond to lifestyle modification. Antiplatelet
8- to16-fold higher in diabetic compared with non-diabetic therapy can retard the onset and progression of PAD and reduce
patients. Additionally, patients with DM have distal cardiovascular events in diabetic patients. Therapeutic
revascularization procedures more often than non-diabetic angiogenesis represents a promising therapeutic adjunct in the
patients [1]. The choice of a procedure depends on many management of PAD and further research is needed. The results
factors such as site and extent of the disease, distal run off and of revascularization procedures for proximal lesions are similar
surgical risk due to associated cardiovascular disease. Proximal, to those in non-diabetic patients, but results in distal bypasses
short segment disease in the iliac and femoral segments is are poor in the long term. Amputation rates after
amenable to PCTA, with results comparable to that in non- revascularization are much higher in diabetic than in non-
diabetic patients. More distal disease in the popliteal and tibial diabetic patients. Mortality in general and perioperative
arteries is better managed by bypass grafting, but with a higher mortality are also high in diabetic patients. Early, aggressive
peri-procedural morbidity and mortality [1]. PCTA below the management of the risk factors and timely referral for
knee is restricted to patients with critical limb ischaemia who are revascularization might improve outcome in patients with PAD.
at high risk during surgical revascularization because of
comorbidities. They may achieve satisfactory limb salvage rates
Competing interests
at least in the short term. However, in view of the distal and
diffuse nature of the disease in diabetic patients, the procedures Nothing to declare.
are technically difficult to perform. The distal run off tends to be
poor and hence the results are worse, revascularization is often
References
not possible and amputation rates are much higher in diabetic
patients with critical limb ischaemia [14]. 1 American Diabetes Association. Peripheral arterial disease in people
with diabetes. Diabetes Care 2003; 26: 3333–3341.
2 Jude EB. Intermittent claudication in the patient with diabetes. Br J
Outcomes Diabetes Vasc Dis 2004; 4: 238–242.
3 Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial
The results of PCTA with or without stenting are better for disease in diabetic and nondiabetic patients: a comparison of
proximal lesions, with reported primary patency rates of 90% at severity and outcome. Diabetes Care 2001; 24: 1433–1437.
4 Kannel WB, McGee DL. Update on some epidemiologic features of
1 year [10] and 85% at 4 years for iliac angioplasty, and 80% at
intermittent claudication: the Framingham Study. J Am Geriatr Soc
1 year for femoral angioplasty. Re-stenosis rates are higher in 1985; 33: 13–18.
diabetic compared with non-diabetic patients after 5 Melton LJ III, Macken KM, Palumbo PJ, Elveback LR. Incidence and
femoropopliteal PCTA [59] and high lipoprotein(a) levels [59] prevalence of clinical peripheral vascular disease in a population-
predict restenosis. Antiplatelet agents and cilostazol reduce based cohort of diabetic patients. Diabetes Care 1980; 3: 650–654.
6 Beks PJ, Mackaay AJ, de Neeling JN, de Vries H, Bouter LM, Heine
restenosis rates after PCTA.
RJ. Peripheral arterial disease in relation to glycaemic level in an
Graft occlusion after peripheral revascularization procedures elderly Caucasian population: the Hoorn study. Diabetologia 1995;
is higher and limb salvage rates are lower in patients with DM [1]. 38: 86–96.
However, limb salvage rates were similar in diabetic and non- 7 Elhadd T, Robb R, Jung R, Stonebridge P, Belch J. Pilot study of
diabetic patients after distal revascularization in some studies prevalence of asymptomatic peripheral arterial occlusive disease in
patients with diabetes attending a hospital clinic. Pract Diabetes Int
[60]. Peripheral neuropathy and foot ulceration are associated
1999; 16: 163–166.
with lower limb salvage rates in diabetic patients. 8 Welborn TA, Knuiman M, McCann V, Stanton K, Constable IJ.
Survival of diabetic patients following a surgical Clinical macrovascular disease in Caucasoid diabetic subjects: lo-
revascularization procedure is slightly lower than that in non- gistic regression analysis of risk variables. Diabetologia 1984; 27:
diabetic patients, but similar for more proximal procedures [1]. 568–573.
ª 2010 The Authors.
12 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
Review article DIABETICMedicine
9 Walters DP, Gatling W, Mullee MA, Hill RD. The prevalence, 27 Jude EB, Douglas JT, Anderson SG, Young MJ, Boulton AJ. Cir-
detection, and epidemiological correlates of peripheral vascular culating cellular adhesion molecules ICAM-1, VCAM-1, P- and E-
disease: a comparison of diabetic and non-diabetic subjects in an selectin in the prediction of cardiovascular disease in diabetes
English community. Diabet Med 1992; 9: 710–715. mellitus. Eur J Intern Med 2002; 13: 185–189.
10 Dormandy JA, Rutherford RB. Management of peripheral arterial 28 Marso SP, Hiatt WR. Peripheral arterial disease in patients with
disease (PAD). TASC Working Group. TransAtlantic Inter-Society diabetes. J Am Coll Cardiol 2006; 47: 921–929.
Consensus (TASC). J Vasc Surg 2000; 31: S1–S296. 29 Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis:
11 Olson JC, Erbey JR, Forrest KY, Williams K, Becker DJ, Orchard epidemiology, pathophysiology, and management. JAMA 2002;
TJ. Glycemia (or, in women, estimated glucose disposal rate) pre- 287: 2570–2581.
dict lower extremity arterial disease events in type 1 diabetes. 30 Uemura S, Matsushita H, Li W, Glassford AJ, Asagami T, Lee KH
Metabolism 2002; 51: 248–254. et al. Diabetes mellitus enhances vascular matrix metalloproteinase
12 Faglia E, Favales F, Quarantiello A, Calia P, Clelia P, Brambilla G activity: role of oxidative stress. Circ Res 2001; 88: 1291–1298.
et al. Angiographic evaluation of peripheral arterial occlusive dis- 31 Li Y, Woo V, Bose R. Platelet hyperactivity and abnormal Ca(2+)
ease and its role as a prognostic determinant for major amputation homeostasis in diabetes mellitus. Am J Physiol Heart Circ Physiol
in diabetic subjects with foot ulcers. Diabetes Care 1998; 21: 625– 2001; 280: H1480–H1489.
630. 32 Vinik AI, Erbas T, Park TS, Nolan R, Pittenger GL. Platelet
13 Malmstedt J, Leander K, Wahlberg E, Karlstrom L, Alfredsson L, dysfunction in type 2 diabetes. Diabetes Care 2001; 24: 1476–
Swedenborg J. Outcome after leg bypass surgery for critical limb 1485.
ischemia is poor in patients with diabetes: a population-based co- 33 Carr ME. Diabetes mellitus: a hypercoagulable state. J Diabetes
hort study. Diabetes Care 2008; 31: 887–892. Complications 2001; 15: 44–54.
14 Faglia E, Clerici G, Clerissi J, Gabrielli L, Losa S, Mantero M et al. 34 Hirsch AT, Hiatt WR. PAD awareness, risk, and treatment: new
Early and five-year amputation and survival rate of diabetic patients resources for survival—the USA PARTNERS program. Vasc Med
with critical limb ischemia: data of a cohort study of 564 patients. 2001; 6: 9–12.
Eur J Vasc Endovasc Surg 2006; 32: 484–490. 35 Dyet JF, Nicholson AA, Ettles DF. Vascular imaging and inter-
15 Murabito JM, Evans JC, Nieto K, Larson MG, Levy D, Wilson PW. vention in peripheral arteries in the diabetic patient. Diabetes Me-
Prevalence and clinical correlates of peripheral arterial disease in the tab Res Rev 2000; 16 (Suppl. 1): S16–S22.
Framingham Offspring Study. Am Heart J 2002; 143: 961–965. 36 Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-
16 Abbott RD, Brand FN, Kannel WB. Epidemiology of some onset diabetic foot ulcers stratified by etiology. Diabetes Care 2003;
peripheral arterial findings in diabetic men and women: experiences 26: 491–494.
from the Framingham Study. Am J Med 1990; 88: 376–381. 37 Dolan NC, Liu K, Criqui MH, Greenland P, Guralnik JM, Chan C
17 Adler AI, Stevens RJ, Neil A, Stratton IM, Boulton AJ, Holman RR. et al. Peripheral artery disease, diabetes, and reduced lower
UKPDS 59: hyperglycemia and other potentially modifiable risk extremity functioning. Diabetes Care 2002; 25: 113–120.
factors for peripheral vascular disease in type 2 diabetes. Diabetes 38 Carser DG. Do we need to reappraise our method of interpreting
Care 2002; 25: 894–899. the ankle brachial pressure index? J Wound Care 2001; 10: 59–
18 Zander E, Heinke P, Reindel J, Kohnert KD, Kairies U, Braun J 62.
et al. Peripheral arterial disease in diabetes mellitus type 1 39 Costacou T, Huskey ND, Edmundowicz D, Stolk R, Orchard TJ.
and type 2: are there different risk factors? Vasa 2002; 31: 249– Lower-extremity arterial calcification as a correlate of coronary
254. artery calcification. Metabolism 2006; 55: 1689–1696.
19 Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long- 40 Aboyans V, Ho E, Denenberg JO, Ho LA, Natarajan L, Criqui MH.
term follow-up after tight control of blood pressure in type 2 dia- The association between elevated ankle systolic pressures and
betes. N Engl J Med 2008; 359: 1565–1576. peripheral occlusive arterial disease in diabetic and nondiabetic
20 Laakso M, Pyorala K. Lipid and lipoprotein abnormalities in dia- subjects. J Vasc Surg 2008; 48: 1197–1203.
betic patients with peripheral vascular disease. Atherosclerosis 41 Tsai JC, Chan P, Wang CH, Jeng C, Hsieh MH, Kao PF et al. The
1988; 74: 55–63. effects of exercise training on walking function and perception of
21 Katsilambros NL, Tsapogas PC, Arvanitis MP, Tritos NA, Alexiou health status in elderly patients with peripheral arterial occlusive
ZP, Rigas KL. Risk factors for lower extremity arterial disease in disease. J Intern Med 2002; 252: 448–455.
non-insulin-dependent diabetic persons. Diabet Med 1996; 13: 42 Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year
243–246. follow-up of intensive glucose control in type 2 diabetes. N Engl J
22 James RW, Boemi M, Sirolla C, Amadio L, Fumelli P, Pometta D. Med 2008; 359: 1577–1589.
Lipoprotein (a) and vascular disease in diabetic patients. Diabeto- 43 Dormandy JA, Betteridge DJ, Schernthaner G, Pirags V, Norgren L.
logia 1995; 38: 711–714. Impact of peripheral arterial disease in patients with diabe-
23 O’Neal DN, Lewicki J, Ansari MZ, Matthews PG, Best JD. Lipid tes—results from PROactive (PROactive 11). Atherosclerosis 2009;
levels and peripheral vascular disease in diabetic and non-diabetic 202: 272–281.
subjects. Atherosclerosis 1998; 136: 1–8. 44 Pyorala K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG,
24 Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Ze- Thorgeirsson G. Cholesterol lowering with simvastatin improves
nari L et al. HOMA-estimated insulin resistance is an independent prognosis of diabetic patients with coronary heart disease. A sub-
predictor of cardiovascular disease in type 2 diabetic subjects: group analysis of the Scandinavian Simvastatin Survival Study (4S).
prospective data from the Verona Diabetes Complications Study. Diabetes Care 1997; 20: 614–620.
Diabetes Care 2002; 25: 1135–1141. 45 Heart Protection Study Collaborative Group. MRC ⁄ BHF Heart
25 Cheng SW, Ting AC, Wong J. Fasting total plasma homocysteine Protection Study of cholesterol lowering with simvastatin in 20,536
and atherosclerotic peripheral vascular disease. Ann Vasc Surg high-risk individuals: a randomised placebo-controlled trial. Lancet
1997; 11: 217–223. 2002; 360: 7–22.
26 Gosk-Bierska I, Adamiec R, Alexewicz P, Wysokinski WE. Coag- 46 Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA,
ulation in diabetic and non-diabetic claudicants. Int Angiol 2002; Neil HA, Livingstone SJ et al. Primary prevention of
21: 128–133. cardiovascular disease with atorvastatin in type 2 diabetes in the
ª 2010 The Authors.
Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14 13
DIABETICMedicine Peripheral arterial disease in diabetes • E. B. Jude et al.
Collaborative Atorvastatin Diabetes Study (CARDS): multicen- 53 CAPRIE Steering Committee. A randomised, blinded, trial of
tre randomised placebo-controlled trial. Lancet 2004; 364: 685– clopidogrel versus aspirin in patients at risk of ischaemic events
696. (CAPRIE). CAPRIE Steering Committee. Lancet 1996; 348: 1329–
47 Heart Outcomes Prevention Evaluation Study Investigators. Effects 1339.
of ramipril on cardiovascular and microvascular outcomes in people 54 Chapman TM, Goa KL. Cilostazol: a review of its use in inter-
with diabetes mellitus: results of the HOPE study and MICRO- mittent claudication. Am J Cardiovasc Drugs 2003; 3: 117–138.
HOPE substudy. Heart Outcomes Prevention Evaluation Study 55 Rendell M, Cariski AT, Hittel N, Zhang P. Cilostazol treatment of
Investigators. Lancet 2000; 355: 253–259. claudication in diabetic patients. Curr Med Res Opin 2002; 18:
48 Mehler PS, Coll JR, Estacio R, Esler A, Schrier RW, Hiatt WR. 479–487.
Intensive blood pressure control reduces the risk of cardiovascular 56 Cozzolino D, Coppola L, Masi S, Salvatore T, Sasso FC, De Lucia D
events in patients with peripheral arterial disease and type 2 dia- et al. Short- and long-term treatments with iloprost in diabetic
betes. Circulation 2003; 107: 753–756. patients with peripheral vascular disease: effects on the cardiovas-
49 Radack K, Deck C. Beta-adrenergic blocker therapy does not cular risk factor plasminogen activator inhibitor type-1. Eur J Clin
worsen intermittent claudication in subjects with peripheral arterial Pharmacol 1999; 55: 491–497.
disease. A meta-analysis of randomized controlled trials. Arch In- 57 Papanas N, Maltezos E. Advances in treating the ischaemic diabetic
tern Med 1991; 151: 1769–1776. foot. Curr Vasc Pharmacol 2008; 6: 23–28.
50 Antiplatelet Trialists’ Collaboration. Collaborative overview of 58 Yang XF, Wu YX, Wang HM, Xu YF, Lu X, Zhang YB et al.
randomised trials of antiplatelet therapy—I: prevention of death, [Autologous peripheral blood stem cells transplantation in treat-
myocardial infarction, and stroke by prolonged antiplatelet therapy ment of 62 cases of lower extremity ischemic disorder]. Zhonghua
in various categories of patients. Antiplatelet Trialists’ Collabora- Nei Ke Za Zhi 2005; 44: 95–98.
tion. BMJ 1994; 308: 81–106. 59 Maca TH, Ahmadi R, Derfler K, Ehringer H, Gschwandtner ME,
51 Antiplatelet Trialists’ Collaboration. Collaborative overview of Horl W et al. Influence of lipoprotein(a) on restenosis after fem-
randomised trials of antiplatelet therapy—II: maintenance of vas- oropopliteal percutaneous transluminal angioplasty in Type 2 dia-
cular graft or arterial patency by antiplatelet therapy. Antiplatelet betic patients. Diabet Med 2002; 19: 300–306.
Trialists’ Collaboration. BMJ 1994; 308: 159–168. 60 Panneton JM, Gloviczki P, Bower TC, Rhodes JM, Canton LG,
52 Hess H, Mietaschk A, Deichsel G. Drug-induced inhibition of Toomey BJ. Pedal bypass for limb salvage: impact of diabetes on
platelet function delays progression of peripheral occlusive arterial long-term outcome. Ann Vasc Surg 2000; 14: 640–647.
disease. A prospective double-blind arteriographically controlled
trial. Lancet 1985; 1: 415–419.
ª 2010 The Authors.
14 Journal compilation ª 2010 Diabetes UK. Diabetic Medicine, 27, 4–14
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Datex-Ohmeda E-Modules - Technical Reference ManualDocument747 pagesDatex-Ohmeda E-Modules - Technical Reference ManualJuanNo ratings yet
- Laporan MR Jaga Siang MalamDocument10 pagesLaporan MR Jaga Siang MalamUlen MahuletteNo ratings yet
- Data SoahukuDocument41 pagesData SoahukuUlen MahuletteNo ratings yet
- New AbstrackDocument1 pageNew AbstrackUlen MahuletteNo ratings yet
- Inggris3 en IdDocument16 pagesInggris3 en IdUlen MahuletteNo ratings yet
- Inggris3 en IdDocument29 pagesInggris3 en IdUlen MahuletteNo ratings yet
- 9700 Y07 SP 31Document16 pages9700 Y07 SP 31Deepti NageshNo ratings yet
- Glycogenesis & GlycogenolysisDocument68 pagesGlycogenesis & GlycogenolysisAnn Michelle TarrobagoNo ratings yet
- Jakob Von Uexkull An IntroductionDocument59 pagesJakob Von Uexkull An IntroductionAnonymous 59RRzvNo ratings yet
- Acute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaDocument30 pagesAcute Complications of Diabetes Mellitus: Hypoglycemia and Hypoglycemic ComaCristinaGheorgheNo ratings yet
- Directional Terms and Body TermsDocument26 pagesDirectional Terms and Body TermsMartinArciniegaNo ratings yet
- Biological Classification 3Document1 pageBiological Classification 3Dr-Atin Kumar SrivastavaNo ratings yet
- Ashrafology's Clinical Examination NotesDocument41 pagesAshrafology's Clinical Examination NotesAnjnaNo ratings yet
- Pembahasan UKDI KLINIK 3 Batch Ags 15 PDFDocument524 pagesPembahasan UKDI KLINIK 3 Batch Ags 15 PDFakbar faerusNo ratings yet
- 214 PGTRB Grade 1 Pet Exam Study Material 1Document8 pages214 PGTRB Grade 1 Pet Exam Study Material 1anithaNo ratings yet
- Perioperative Nursing CareDocument47 pagesPerioperative Nursing CareTessa Bagus AriyantoNo ratings yet
- ICU One Pager Vasopressors.1.2Document1 pageICU One Pager Vasopressors.1.2Nguyễn Ngọc Quỳnh NhưNo ratings yet
- Craniotomy & NeuromonitoringDocument21 pagesCraniotomy & NeuromonitoringMarisa GoddardNo ratings yet
- Biomedical Model Question PaperDocument5 pagesBiomedical Model Question PaperDibboNo ratings yet
- Maternal and Child Health NursingDocument6 pagesMaternal and Child Health NursingRoanne DivinagraciaNo ratings yet
- Tai Chi ChuanDocument89 pagesTai Chi Chuandani100% (1)
- The Limits of Friendship - The New YorkerDocument7 pagesThe Limits of Friendship - The New YorkerEmeraldNo ratings yet
- Test Bank For Essentials of Anatomy and Physiology 7th Edition by MartiniDocument36 pagesTest Bank For Essentials of Anatomy and Physiology 7th Edition by Martiniremovaltinemangkvk100% (49)
- Alison Smith, Michael Witty-Heme, Chlorophyll, and Bilins - Methods and Protocols (2001)Document351 pagesAlison Smith, Michael Witty-Heme, Chlorophyll, and Bilins - Methods and Protocols (2001)Andres CastilloNo ratings yet
- Wa0042Document65 pagesWa0042MirafudinNo ratings yet
- R J Epstein-Human Molecular Biology - An Introduction To The Molecular Basis of Health and Disease-Cambridge University Press (2002)Document655 pagesR J Epstein-Human Molecular Biology - An Introduction To The Molecular Basis of Health and Disease-Cambridge University Press (2002)Libros a Color ConceNo ratings yet
- Effect of Injury and Immobilization On MuscleDocument19 pagesEffect of Injury and Immobilization On Musclesonali tushamerNo ratings yet
- Chandulal - Nanavati - Bio - Prelim Class 10th IcseDocument4 pagesChandulal - Nanavati - Bio - Prelim Class 10th IcseOmMen GamingNo ratings yet
- Musculoskeletal SystemDocument92 pagesMusculoskeletal SystemBrenda LynNo ratings yet
- Heart Beat +GSM Engineering Final Year ProjectthesisDocument111 pagesHeart Beat +GSM Engineering Final Year Projectthesisrauf2063036100% (1)
- Empty Nose SyndromeDocument4 pagesEmpty Nose SyndromeMohamad AtefNo ratings yet
- Guide To The Parasites of Fishes of Canada Parte 3Document103 pagesGuide To The Parasites of Fishes of Canada Parte 3majo.castellon.alcarazNo ratings yet
- Wolff's LawDocument3 pagesWolff's LawThe Bens Mbr 17No ratings yet
- SPM Summary ModuleDocument6 pagesSPM Summary ModulerazifNo ratings yet
- Aerobic Work Capacity Training BuilderDocument10 pagesAerobic Work Capacity Training BuilderJawad KhawajaNo ratings yet