Professional Documents
Culture Documents
Pelaez - Et - Al - 2014 - NandU - Pelvic Floor Muscle Training Included in A Pregnancy Exercise Program Is Effective in Primary Prevention of Urinary Incontinence
Uploaded by
Shannon DolanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pelaez - Et - Al - 2014 - NandU - Pelvic Floor Muscle Training Included in A Pregnancy Exercise Program Is Effective in Primary Prevention of Urinary Incontinence
Uploaded by
Shannon DolanCopyright:
Available Formats
Neurourology and Urodynamics 33:67–71 (2014)
Pelvic Floor Muscle Training Included in a Pregnancy
Exercise Program Is Effective in Primary Prevention of
Urinary Incontinence: A Randomized Controlled Trial
Mireia Pelaez,1* Silvia Gonzalez-Cerron,2 Rocı́o Montejo,2 and Rubén Barakat1
1
Faculty of Physical Activity and Sport Sciences-INEF, Technical University of Madrid-UPM, Madrid, Spain
2
Universitarian Hospital of Fuenlabrada, Madrid, Spain
Aims: To investigate the effect of pelvic floor muscle training (PFMT) taught in a general exercise class during preg-
nancy on the prevention of urinary incontinence (UI) in nulliparous continent pregnant women. Methods: This was a
unicenter two armed randomized controlled trial. One hundred sixty-nine women were randomized by a central com-
puter system to an exercise group (EG) (exercise class including PFMT) (n ¼ 73) or a control group (CG) (n ¼ 96).
10.1% loss to follow-up: 10 from EG and 7 from CG. The intervention consisted of 70–75 sessions (22 weeks, three times
per week, 55–60 min/session including 10 min of PFMT). The CG received usual care (which included follow up by
midwifes including information about PFMT). Questions on prevalence and degree of UI were posed before (week 10–
14) and after intervention (week 36–39) using the International Consultation on Incontinence Questionnaire-Urinary
Incontinence Short Form (ICIQ-UI SF). Results: At the end of the intervention, there was a statistically significant
difference in favor of the EG. Reported frequency of UI [Never: CG: 54/60.7%, EG: 60/95.2% (P < 0.001)]. Amount of
leakage [None: CG: 45/60.7%, EG: 60/95.2% (P < 0.001)]. There was also a statistically significant difference in ICIQ-
UI SF Score between groups after the intervention period [CG: 2.7 (SD 4.1), EG: 0.2 (SD 1.2) (P < 0.001)]. The estimat-
ed effect size was 0.8. Conclusion: PFMT taught in a general exercise class three times per week for at least 22 weeks,
without former assessment of ability to perform a correct contraction was effective in primary prevention of UI in
primiparous pregnant women. Neurourol. Urodynam. 33:67–71, 2014. ß 2013 Wiley Periodicals, Inc.
Key words: gestation; nulliparous; physical exercise; physical therapy; prevention
INTRODUCTION MATERIALS AND METHODS
Urinary incontinence (UI) is a well recognized health prob-
Design
lem that significantly reduces the quality of life and affects
women of all ages.1–3 Pregnancy and childbirth are considered This was a unicenter, two armed, open label, randomized
to be important risk factors in the development and the wors- controlled trial.
ening of UI.1,4
Pelvic floor muscle training (PFMT) is an effective technique
Participants
in the prevention and treatment of UI in the general popula-
tion4 and its effectiveness has also been found during preg- Pregnant women attending the local hospital for antenatal
nancy.1 Moreover, based on different studies, it has been care were asked to participate in the study. Recruitment took
found to be as effective as other treatments5,6 and according place between October 2009 and October 2011, and final data
to a review by Cochrane, it should be included in the first line collection finished on June 2011. Inclusion criteria were: being
of conservative management and of primary prevention of healthy and primiparous pregnant with singleton fetus, being
UI.7 in gestational week 10–14, not suffering from UI, able to com-
In most studies, PMFT is conducted by physiotherapists and municate in Spanish and able to give informed written con-
its efficacy when taught by other professionals such as fitness sent. Exclusion criteria were: planning not to give birth in
instructors has not been found.8 To quote Bø and Haakstad8 it Fuenlabrada University Hospital and any contraindication
would be less time-consuming, more cost-effective and possi- according to the American College of Obstetricians and Gyne-
bly more motivating if PFMT could be taught in a group set- cologists Guidelines.9 One hundred sixty nine women were
ting by fitness instructors. However the professional who included in the study. It was approved by the Ethical
should design and lead the session must meet different
requirements. A Physical Activity and Sport Sciences graduate
has both the theoretical and practical knowledge to design ex- Conflict of interest: none.
Mickey Karram led the peer-review process as the Associate Editor responsible for
ercise programs taking into account the training principles, the paper.
and moreover has a pedagological background which could *Correspondence to: Mireia Pelaez, PhD, Faculty of Physical Activity and Sport Sci-
enhance motivation and long-term learning. ences-INEF, Technical University of Madrid-UPM, Martı́n Fierro, 7, 28040 Madrid,
We hypothesized that PFMT taught by a Physical Spain. E-mail: mireiapelaez@gmail.com
Received 25 July 2012; Accepted 14 January 2013
Activity and Sport Sciences graduate and included in a Published online 6 February 2013 in Wiley Online Library
pregnancy exercise program is effective in primary prevention (wileyonlinelibrary.com).
of UI. DOI 10.1002/nau.22381
ß 2013 Wiley Periodicals, Inc.
68 Pelaez et al.
Committee of Fuenlabrada University Hospital (Madrid, Spain) contraction or any measurement of pelvic floor muscle
and followed the ethical guidelines outlined in the Declaration strength. Women were asked to test themselves at home by
of Helsinki (last modified in 2008). All women provided writ- trying to stop the flow while urinating, touching the vaginal
ten informed consent. The study is listed in ClinicalTRials.gov and anal openings and using a mirror to see if they could
(NCT 01578369). squeeze around the pelvic openings and upward lift.
The PFMT followed a progression, starting with one set of
eight contractions and increasing the number of total contrac-
Intervention
tions to one hundred, divided in different sets of slow (6 sec)
Women in the exercise group (EG) were asked to participate and fast contractions (five contractions as fast as possible). To
in a structured exercise program for at least 22 weeks (14–36 increase motivation and abilities, we used different exercises
weeks of gestation). The program consisted of 70–78 group (Fig. 1), positions and sometimes music to follow the beat.
sessions (8–12 women). The sessions were held three times Women were encouraged to perform 100 contractions distrib-
per week and were 55–60 min in duration. The sessions were uted in different sets every day.
performed in the hospital, in a well-lit room under favorable To enhance motivation and adherence, group dynamics and
environmental conditions (altitude 600 m; temperature, 19– exercises in pairs were included. Talking about needs and feel-
218C; humidity, 50–60%). ings were also allowed and encouraged.
Each session consisted of 8 min of warm-up; 30 min of low Women in the control group (CG) received usual care (which
impact aerobics (performing different choreographies) includ- included follow up by midwifes including information about
ing 10 min of general strength training (e.g., core muscles, PFMT) and were not asked not to train their pelvic floor
pectoralis, gluteus, quadriceps, calves, biceps); 10 min of PFMT muscles.
and 7 min of cool down, which included stretching, relaxation
or massage. All subjects used a heart rate monitor (Accurex
Randomization
Plus, Polar Electro OY, Finland) during the training sessions to
control the exercise intensity (65–70% age predicted maxi- A statistical randomization computer program was used to
mum heart rate value). The Borg Rating of Perceived Exertion perform a simple randomization to allocate women into each
Scale was also used to guide exercise intensity (12–14 ‘‘some- group.
what hard’’).10
The whole session, including PFMT was designed and taught
Outcome Measures
by a Physical Activity and Sport Sciences graduate. At the be-
ginning of the program, women received information of anato- The primary outcomes were (i) the reported frequency, (ii)
my and function of the PFM and why the muscles may prevent amount, and (iii) impact on daily life of UI. These outcomes
and treat the UI. At first, women learned to perceive their pelvic were measured by the validated International Consultation
floor, and then learned how to do adequate contractions. There on Incontinence Questionnaire-Urinary Incontinence Short
was no former assessment of ability to perform a correct Form (ICIQ-UI SF).11 Women completed the forms at the end of
Fig. 1. Examples of some of the proposed exercises in pelvic floor muscle training. PFM, pelvic floor muscles.
Neurourology and Urodynamics DOI 10.1002/nau
Pelvic Floor Muscle Training During Pregnancy 69
intervention (between 36 and 40 weeks of gestation). Before Effect size was also calculated on ICIQ-Score using t-stats and
intervention, women were interviewed to provide maternal sample size.
characteristics such as education level or pre-pregnancy physi-
cal activity habits. To enhance the quality of measurements,
RESULTS
the three interviewers were trained and informed about how
to make women feel comfortable talking about their UI. Initially, 169 women were included in the study. Data from
152 women were analyzed (10.1% loss to follow-up: 10 from
the EG and 7 from the CG). Figure 2 shows the study flow
Power Calculations
chart with the numbers of drop-outs and their reasons. All
To estimate the sample size, a 95% confidence level, 80% women included on analysis attended at least 80% of 70–78
statistical power, and a 20% of losses were accepted. Assum- exercise sessions during at least 22 weeks.
ing, in the usual care situation, a prevalence of 39% of women Background variables at baseline are shown in Table I. There
affected by UI at the end of gestation (week 36)3 and estimat- were no differences between groups in mean age, pre-preg-
ing a reduction of 20% of women affected by UI in the treat- nancy BMI, education, and pre-pregnancy physical exercise
ment group, it was considered that 156 women should be habits at baseline.
included. At the end of intervention (week 36 of pregnancy) there were
statistically significant differences in favor of the EG as shown
in Table II). 95.2% of women in the EG reported no leakage
Statistical Analyses
versus a 60.7% of women in the CG. Only women of CG had a
Background variables are given as frequencies and percen- frequency of leakage more than of once a week (17/19.1%). The
tages, and means with standard deviations (SD). Chi-squared amount of leakage reported by incontinent women in the EG is
and Mann–Whitney tests were used to analyze differences in referred as a ‘‘a small amount’’ (3/4.8%) but in the CG, women
categorical variables and t-test for quantitative variables. P- reported ‘‘a small amount’’ (27/30.6%), ‘‘a moderate amount’’ (5/
values <0.05 were considered to be statistically significant. 5.6%), and even ‘‘a large amount’’ (3/3.4%).
Fig. 2. Study flow chart with the number of drop-outs and their reasons.
Neurourology and Urodynamics DOI 10.1002/nau
70 Pelaez et al.
TABLE I. Background Variables Before Intervention in the Exercise and was in accordance with these data. We also estimated a reduc-
Control Groups tion of 20% of women affected by UI in the EG, and the reduc-
tion obtained was higher: a 34.5%.
Exercise Control
The reduction of UI found in the EG is in accordance with
(n ¼ 63) (n ¼ 89) P-value
other studies in which PFMT is lead by physiotherapists.
Mørkved et al.1 found 16% difference in the prevalence of UI
Age (years) 29.9 (3.3) 29.1 (4.5) 0.23
Pre-pregnancy BMI 23.6 (4.3) 22.7 (3.8) 0.23
in favor of the training group in pregnant nulliparous women.
Educational level However this study included incontinent women (32% and
College 23/37.1 23/25.8 0.07 31% in training and CG respectively) at baseline and there
High school 29/46.8 38/42.7 was only one supervised session per week. Stafne et al.12
<High school 10/16.1 28/31.5 found fewer women in the intervention group reporting any
Pre-pregnancy PA weekly UI (11% vs. 19%) at the end of intervention (32–36
Inactive 33/53.2 56/62.9 0.15 weeks of gestation). Only one weekly group session was led
Active 29/46.8 33/37.1 by physiotherapists during the 12-week exercise program.
To date, we have only found two studies in which PFMT
BMI, body mass index; PA, physical habits.
was not conducted by physiotherapists. The first one by Bru-
Mean with standard deviation (SD) and numbers (n) with percentages (%)
(n ¼ 152).
baker et al.13 shows the feasibility of a pelvic fitness and edu-
cation class for affected and non pregnant women. The
women in this study trained twice a week for 11 weeks. The
In regards to how much leaking affects their daily lives, the results showed statistically and clinically significant improve-
mean in the CG was higher than in the EG (0.9 (SD 1.8) vs. 0.1 ment in pelvic floor and sexual function. The second study, by
(SD 0.6), respectively. Finally, ICIQ-UI SF Score shows statisti- Bø and Haakstad8 had a RCT design and PFMT were led by
cally significant differences between the groups and the esti- certified aerobics instructors. No effect of PFMT was found
mated effect size was 0.8. and that is in contrast with our results.
We found common points in Bø and Haakstad8 and the
present study. An important point is that there was no former
DISCUSSION
assessment of ability to perform a correct contraction. The sec-
The major finding of the present study was that PFMT in- ond common point was the exercise program structure. Per-
cluded in a pregnancy exercise program, with three sessions haps, one of the main differences was the adherence to the
per week over the course of at least 22 weeks, is effective in program. Only 40% of women in the aforementioned study
primary prevention of UI in pregnancy, without individual as- attended at least 80% of exercise sessions. In our study, all
sessment of the ability to contract the pelvic floor muscles. women included on analysis (100%) attended at least 80% of
The strengths of the present study include the use of an RCT sessions. Other differences were the length of the program (12
design, high adherence and the implementation of an exercise weeks vs. 22 in the present study) and the total number of
program following ACOG recommendations, conducted by a pelvic floor muscle contractions per day (36 vs. 100 respective-
Physical Activity and Sport Sciences graduate. Some of the ly). Furthermore, in the Bø et al. study, there were incontinent
limitations of the study are: no pad test, no assessment of women at baseline (26.9% in the EG and 20.7% in the CG).
PFM strength and the non-blinded design. These results show the importance that a Physical Activity
The prevalence rates of UI in the CG were very similar to and Sport Sciences graduate design and lead the exercise pro-
those that we took into account to estimate the sample size. grams to make them effective and motivating for the pregnant
We assumed a prevalence of 39% of women affected by UI at population. They also suggest that the three times per week fre-
the end of gestation (week 36)3 and in our study we found quency is well accepted. Although there were positive results
that a 39.3% of women in the CG were affected by UI, which without individual assessment, it may well be that the effect
would have been far stronger if there had been individual as-
sessment of the ability to contract the pelvic floor muscles.
TABLE II. Results From ICIQ-UI SF Questionnaire After Intervention in Usual care for pregnant women includes 8–12 sessions with
Exercise and Control Groups a midwife in which women learn about the pelvic floor as
well as other issues concerning labor, breastfeeding and child
Exercise Control
care, but there is no standardized protocol. These results sug-
(n ¼ 63) (n ¼ 89) P-value
gest the need for accompaniment, monitoring and motivation
through the whole gestation period for PFMT to be effective
Reported frequency of UI
Never 60/95.2 54/60.7 0.0001
and the importance of the development of multidisciplinary
Once a week 3/4.8 18/20.2 teams composed of different professionals to monitor and
2–3 times per week 0/0.0 9/10.1 nurture pregnant women through gestation to ensure the
Once a day 0/0.0 7/7.9 highest quality of life as possible.
Several times per day 0/0.0 1/1.1 In future, it would be of interest to compare the prevalence
Amount of leakage of UI between groups 2 years after delivery as well as other
None 60/95.2 54/60.7 0.0001 aspects regarding the quality of life of these women; and to
A small amount 3/4.8 27/30.3 study the effectiveness of this type of program in the treat-
A moderate amount 0/0.0 5/5.6
ment of UI in affected women.
A large amount 0/0.0 3/3.4
How much does leaking 0.10 (0.64) 0.97 (1.8) 0.0001
affect daily life CONCLUSION
ICIQ-Score 0.24 (1.2) 2.66 (4.1) 0.0001
This study shows the effectiveness of PFMT included in a
Mean with standard deviation (SD) and numbers (n) with percentages (%) pregnancy exercise program on primary prevention of UI dur-
(n ¼ 152). ing pregnancy in nulliparous continent women. It also
Neurourology and Urodynamics DOI 10.1002/nau
Pelvic Floor Muscle Training During Pregnancy 71
suggests the importance of both the program design and the 5. Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic
floor exercises, electrical stimulation, vaginal cones, and no treatment in
role of a Physical Activity and Sport Sciences graduate in en- management of genuine stress incontinence in women. BMJ 1999;318:
hancing adherence to the program. 487–93.
6. Castro RA, Arruda RM, Zanetti MR, et al. Single-blind, randomized, controlled
trial of pelvic floor muscle training, electrical stimulation, vaginal cones,
ACKNOWLEDGMENTS and no active treatment in the management of stress urinary incontinence.
Clinics (Sao Paulo) 2008;63:465–72.
The authors would like to acknowledge the technical assis- 7. Hay-Smith EJ, Bø Berghmans LC, Hendriks HJ, et al. Pelvic floor muscle train-
tance of the Gynecology and Obstetrics Service of Fuenlabrada ing for urinary incontinence in women. Cochrane Database Sys Rev 2007;
University Hospital, the assistance of Ms. Marta de Rio and all CD001407.
participating woman. 8. Bø K, Haakstad LA. Is pelvic floor muscle training effective when taught in a
general fitness class in pregnancy? A randomised controlled trial. Physio-
therapy 2011;97:190–5.
REFERENCES 9. American College of Obstetricians and Gynecologists (ACOG). Exercise dur-
ing pregnancy and the postpartum period. Committee Opinion 267. Obstet
1. Mørkved S, Bø K, Schei B, et al. Pelvic floor muscle training during pregnancy Gynecol 2002;99:171–3.
to prevent urinary incontinence: A single-blind randomized controlled trial. 10. Artal R, O’Toole M, White S. Guidelines of the ACOG for exercise during preg-
Obstet Gynecol 2003;101:313–9. nancy and postpartum period. Br J Sports Med 2003;37:6–1.
2. Zhu L, Li L, Lang JH, et al. Prevalence and risk factors for peri- and postpar- 11. Avery K, Donovan J, Peters TJ, et al. ICIQ: A brief and robust measure for
tum urinary incontinence in primiparous women in China: A prospective evaluating the symptoms and impact of urinary incontinence. Neurourol
longitudinal study. Int Urogynecol J 2012;23:563–72. Urodyn 2004;23:322–30.
3. Solans-Domenech M, Sánchez E, Espuña-Pons M, et al. Urinary and anal 12. Stafne S, Salvensen KA, Romundstad P, et al. Does regular exercise
incontinence during pregnancy and postpartum: Incidence, severity, and including pelvic floor muscle training prevent urinary and anal inconti-
risk factors. Obstet Gynecol 2010;115:618–28. nence during pregnancy? A randomized controlled trial. BJOG 2012;119:
4. Boyle R, Hay-Smith EJ, Cody JD, et al. Pelvic floor muscle training for preven- 1270–80.
tion and treatment of urinary and faecal incontinence in antenatal and 13. Brubaker L, Shott S, Tomezsko J, et al. Pelvic floor fitness using lay instruc-
postnatal women. Cochrane Database Syst Rev 2012;17:CD007471. tors. Obstet Gynecol 2008;111:1298–304.
Neurourology and Urodynamics DOI 10.1002/nau
You might also like
- Art-Previene El Ejercicio Regular Incluido MSP La Iu e Ia en El EmbarazoDocument11 pagesArt-Previene El Ejercicio Regular Incluido MSP La Iu e Ia en El EmbarazoPaula RangelNo ratings yet
- A Comparison of Two PFMT Programs in Females With Stress Urinary IncontineneceDocument11 pagesA Comparison of Two PFMT Programs in Females With Stress Urinary Incontinenecemenna lNo ratings yet
- Futbol y Vo2Document5 pagesFutbol y Vo2Sandra R A MedinaNo ratings yet
- Phys TherDocument16 pagesPhys TherNovie AstiniNo ratings yet
- Pelvic Floor Muscle Training Protocol For Stress Urinary Incontinence in Women: A Systematic ReviewDocument9 pagesPelvic Floor Muscle Training Protocol For Stress Urinary Incontinence in Women: A Systematic ReviewKarem FernandezNo ratings yet
- Jurnal Propriosepsi GeriatriDocument9 pagesJurnal Propriosepsi GeriatriIra AdventiaNo ratings yet
- Hypo PF functionDocument17 pagesHypo PF functionIvan Garcia OsorioNo ratings yet
- Jpts 25 1087 PDFDocument5 pagesJpts 25 1087 PDFArry FirmansyahNo ratings yet
- Kegel Exercise PDFDocument5 pagesKegel Exercise PDFDisaKNNo ratings yet
- International Journal of Health Sciences and ResearchDocument7 pagesInternational Journal of Health Sciences and ResearchariniNo ratings yet
- Effect of A Physiotherapy Program in Women With Primary DysmenorrheaDocument6 pagesEffect of A Physiotherapy Program in Women With Primary DysmenorrheaPaula RangelNo ratings yet
- Bibliography (Critical Care Nursing)Document2 pagesBibliography (Critical Care Nursing)bijoiiNo ratings yet
- Does Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled TrialDocument7 pagesDoes Regular Exercise in Pregnancy Influence Duration of Labor? A Secondary Analysis of A Randomized Controlled Trialana pintoNo ratings yet
- Impact of Applying Different Physical Activity GuidelinesDocument9 pagesImpact of Applying Different Physical Activity GuidelinesnirchennNo ratings yet
- Ansai Et Al. (2016) PDFDocument8 pagesAnsai Et Al. (2016) PDFvabrandaoNo ratings yet
- Experiences of Exercise During pregnancyDocument9 pagesExperiences of Exercise During pregnancyNuno RobertoNo ratings yet
- Postnatal Exercises Improve Quality of LifeDocument4 pagesPostnatal Exercises Improve Quality of LiferohiniNo ratings yet
- Women's Health Reports Knowledge and Practice of Pelvic Floor ExercisesDocument7 pagesWomen's Health Reports Knowledge and Practice of Pelvic Floor ExercisesQORI KARUNIA WANTINo ratings yet
- Inter Fan ZhangDocument9 pagesInter Fan ZhangrizkaNo ratings yet
- Complementary Therapies in Clinical Practice: Semiha Ayd In Özkan, Gülay Rath FischDocument6 pagesComplementary Therapies in Clinical Practice: Semiha Ayd In Özkan, Gülay Rath FischAlek OkeNo ratings yet
- Muscle Strength Training Program in Nonagenarians - A Randomized Controlled TrialDocument6 pagesMuscle Strength Training Program in Nonagenarians - A Randomized Controlled TrialGabriel ArcenioNo ratings yet
- Metode de Reeducare PosturalaDocument4 pagesMetode de Reeducare PosturalaMaria RamonaNo ratings yet
- Effect of A Postpartum Training Program On Prevale PDFDocument9 pagesEffect of A Postpartum Training Program On Prevale PDFHardik SinghNo ratings yet
- 2002 PDFDocument6 pages2002 PDFIMaa Wati AlbiizzahNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologyana pintoNo ratings yet
- Perineal Massage and Training Reduce TraumaDocument7 pagesPerineal Massage and Training Reduce TraumaGum GulNo ratings yet
- Oliveira 2007Document8 pagesOliveira 2007Carlos VieiraNo ratings yet
- Effects of Prenatal Perineal Massage and Kegel Exercise On The Episiotomy RateDocument10 pagesEffects of Prenatal Perineal Massage and Kegel Exercise On The Episiotomy RateIOSRjournalNo ratings yet
- Pelvic Floor Rehabilitation in The Treatment of Women With Dyspareunia: A Randomized Controlled Clinical TrialDocument7 pagesPelvic Floor Rehabilitation in The Treatment of Women With Dyspareunia: A Randomized Controlled Clinical TrialFERNANDA SILVEIRANo ratings yet
- Kidney Paper 2018Document5 pagesKidney Paper 2018samah hossnyNo ratings yet
- Does Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialDocument6 pagesDoes Exercise Training During Pregnancy Affect Gestational Age? A Randomised Controlled TrialTrnidad Moder GarvizoNo ratings yet
- Jurnal Obgyn GueDocument4 pagesJurnal Obgyn Gueamel_ariefNo ratings yet
- Regular Exercise During Pregnancy To Prevent Gestational DiabetesDocument8 pagesRegular Exercise During Pregnancy To Prevent Gestational DiabetesEgie Nugraha Fitriyan ApriyadiNo ratings yet
- Oral Presentation David Oktavianus Tambunan TerbaruDocument34 pagesOral Presentation David Oktavianus Tambunan TerbaruMunifah YusriyahNo ratings yet
- Jurnal Post PartumDocument11 pagesJurnal Post PartumjayaNo ratings yet
- Role of Kegel's Exercise On Postpartum Perineal Fitness Randomised Control TrialDocument6 pagesRole of Kegel's Exercise On Postpartum Perineal Fitness Randomised Control TrialCatalina DincaNo ratings yet
- Effects of Leg Strength Exercise On Muscle Strength, Flexibility and Symptoms of Urinary Incontinence of Elderly WomenDocument9 pagesEffects of Leg Strength Exercise On Muscle Strength, Flexibility and Symptoms of Urinary Incontinence of Elderly Womenkang soon cheolNo ratings yet
- Vikranth .G .R Lawrence Mathias Mohd Meraj Ghori: BackgroundDocument8 pagesVikranth .G .R Lawrence Mathias Mohd Meraj Ghori: BackgroundSekar AyuNo ratings yet
- Efects of Inspiratory Muscle Training in Older AdultsDocument10 pagesEfects of Inspiratory Muscle Training in Older AdultsMaría Camila Zuluaga AriasNo ratings yet
- Physical Activity During Pregnancy and Its Influence On Delivery Time: A Randomized Clinical TrialDocument14 pagesPhysical Activity During Pregnancy and Its Influence On Delivery Time: A Randomized Clinical TrialZaray EspinosaNo ratings yet
- Environmental Research and Public Health: International Journal ofDocument10 pagesEnvironmental Research and Public Health: International Journal ofrestu pangestutiNo ratings yet
- Pilares Eficiente para El Suelo PelvicoDocument6 pagesPilares Eficiente para El Suelo PelvicoRitaNo ratings yet
- Effects of pelvic floor muscle training during pregnancyDocument8 pagesEffects of pelvic floor muscle training during pregnancyelfanizar yusandiNo ratings yet
- LP Post Partum SpontanDocument16 pagesLP Post Partum SpontanPutri PuspitaNo ratings yet
- Hipopresivos y Dolor Lumbar Cronico 2021Document9 pagesHipopresivos y Dolor Lumbar Cronico 2021klgarivasNo ratings yet
- Bo Et AlDocument6 pagesBo Et AlMaria Betania NunesNo ratings yet
- 1 Monteiro Etal 2021Document6 pages1 Monteiro Etal 2021Gabriel GursenNo ratings yet
- Papn MS Id 000156Document7 pagesPapn MS Id 000156niekoNo ratings yet
- Comparative Effect of Vision Deprived Balance Training Over Free Vision Balance Training Among Stroke SubjectsDocument8 pagesComparative Effect of Vision Deprived Balance Training Over Free Vision Balance Training Among Stroke SubjectsijphyNo ratings yet
- A Comparative Study To Determine The Efficacy of Routine Physical Therapy Treatment With and Without Kaltenborn Mobilization On Pain and Shoulder Mobility in Frozen Shoulder PatientsDocument4 pagesA Comparative Study To Determine The Efficacy of Routine Physical Therapy Treatment With and Without Kaltenborn Mobilization On Pain and Shoulder Mobility in Frozen Shoulder Patientsfi.afifah NurNo ratings yet
- Mobility Training After Hip FractureDocument7 pagesMobility Training After Hip FracturewirasenaNo ratings yet
- RCT Zumba ExerciseDocument5 pagesRCT Zumba ExerciseSukmarahayuNo ratings yet
- Pilates Reduces Postpartum FatigueDocument5 pagesPilates Reduces Postpartum FatigueHidroterapia lucenaNo ratings yet
- Mulligan Sustained Natural Apophyseal Glides Versus Thoracic Manipulation On Mechanical Neck Pain: A Randomized Controlled StudyDocument12 pagesMulligan Sustained Natural Apophyseal Glides Versus Thoracic Manipulation On Mechanical Neck Pain: A Randomized Controlled StudyAbdul Latiful KhabirNo ratings yet
- A Clinical Study of Programmed Labour and Its Maternal and Foetal OutcomeDocument4 pagesA Clinical Study of Programmed Labour and Its Maternal and Foetal OutcomeInternational Organization of Scientific Research (IOSR)No ratings yet
- Effects of Pelvic Floor Muscle Training Combined With Estriol On Pelvic Floor Dysfunction After Total Hysterectomy Applied in PerimenopauseDocument6 pagesEffects of Pelvic Floor Muscle Training Combined With Estriol On Pelvic Floor Dysfunction After Total Hysterectomy Applied in PerimenopauseChoirul AkbarNo ratings yet
- Effectiveness of StretchingDocument10 pagesEffectiveness of Stretchingاحمد العايديNo ratings yet
- Exercise in Pregnancy: Effect On Fitness and Obstetric Outcomes - A Randomized TrialDocument4 pagesExercise in Pregnancy: Effect On Fitness and Obstetric Outcomes - A Randomized TrialInes NozicaNo ratings yet
- Exercise and Sporting Activity During Pregnancy: Evidence-Based GuidelinesFrom EverandExercise and Sporting Activity During Pregnancy: Evidence-Based GuidelinesRita Santos-RochaNo ratings yet
- The Art of Healing Movement: Exploring Therapeutic Wu Shu Gymnastics.From EverandThe Art of Healing Movement: Exploring Therapeutic Wu Shu Gymnastics.No ratings yet
- Stages of Labor: Latent, Active, Transition & PlacentalDocument18 pagesStages of Labor: Latent, Active, Transition & Placentallushxene84No ratings yet
- Obstetrics and GynacologyDocument14 pagesObstetrics and GynacologykalkidanNo ratings yet
- Demographic Data: #2 RefusedDocument31 pagesDemographic Data: #2 Refusedjp102090No ratings yet
- Nfhs-5 India ReportDocument713 pagesNfhs-5 India ReportROHIT DASNo ratings yet
- MRDE 101 Full TextbookDocument512 pagesMRDE 101 Full TextbookSedekholie ChadiNo ratings yet
- 1st & 2nd Trimester Pregnancy LossDocument48 pages1st & 2nd Trimester Pregnancy LossAbdullah EssaNo ratings yet
- LS 2 M1L1L3Document7 pagesLS 2 M1L1L3Alvin Arquibel DescatamientoNo ratings yet
- TPCN 1295 FormDocument1 pageTPCN 1295 FormTeddy WilsonNo ratings yet
- PREECLAMPSIA Case ScenarioDocument2 pagesPREECLAMPSIA Case Scenariosabao kizuiteNo ratings yet
- Stages of Prenatal DevelopmentDocument36 pagesStages of Prenatal DevelopmentRuru LavariasNo ratings yet
- The Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesDocument9 pagesThe Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesimuhammadfahmiNo ratings yet
- Columbia Sexuality and Gender Law Clinic - Surrogacy Law and Policy Report - June 2016 PDFDocument90 pagesColumbia Sexuality and Gender Law Clinic - Surrogacy Law and Policy Report - June 2016 PDFShantanu AgnihotriNo ratings yet
- Mechanisms of Normal Vertex LabourDocument65 pagesMechanisms of Normal Vertex LabourBasmala We PasNo ratings yet
- Incompetent NCPDocument1 pageIncompetent NCPJohn Francis Velasco100% (6)
- NCM 107 Clinical Case in Gynecology 1Document35 pagesNCM 107 Clinical Case in Gynecology 1Kyle Randolf CuevasNo ratings yet
- Safe Abortion – A Moral ObligationDocument20 pagesSafe Abortion – A Moral ObligationJerico RelopezNo ratings yet
- Ibnu Sina Hospital, Tuesday, April 19th, 2022 (Period April 10th - 17th, 2022)Document4 pagesIbnu Sina Hospital, Tuesday, April 19th, 2022 (Period April 10th - 17th, 2022)MirahAvishaNo ratings yet
- UNIT - II - SUBCENTRE - AnandDocument34 pagesUNIT - II - SUBCENTRE - AnandAnand gowdaNo ratings yet
- Family PlanningDocument59 pagesFamily PlanningDhruva PatelNo ratings yet
- Edexcel: IgcseDocument15 pagesEdexcel: IgcseAdele FernandoNo ratings yet
- Female Reproductive System: Understanding Puberty and Hormonal ChangesDocument33 pagesFemale Reproductive System: Understanding Puberty and Hormonal ChangesHoneychrise ConcepcionNo ratings yet
- Glanville Williams Legal and Illegal AbortionDocument14 pagesGlanville Williams Legal and Illegal AbortionoduronyarkolawreneNo ratings yet
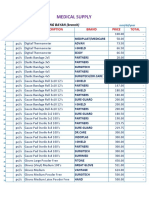
- Medical Supply and Baby Product ListingDocument5 pagesMedical Supply and Baby Product ListingParmasya Ng Bayan Bacolor Main BranchNo ratings yet
- Fundal Height MeasurementDocument2 pagesFundal Height MeasurementCuttie Anne GalangNo ratings yet
- Everything You Need to Know About the Menstrual CycleDocument16 pagesEverything You Need to Know About the Menstrual CycleCoxnxkNo ratings yet
- Obstetric History TakingDocument5 pagesObstetric History TakingAshish Mishra [33]No ratings yet
- Intrapartum Category I, II, and III Fetal Heart Rate Tracings - Management - UpToDateDocument18 pagesIntrapartum Category I, II, and III Fetal Heart Rate Tracings - Management - UpToDateMadeline lunaNo ratings yet
- Chapter 3 Human ReproductionDocument7 pagesChapter 3 Human Reproductionsara DaphneNo ratings yet
- Chapter#3 Developmental PsychologyDocument32 pagesChapter#3 Developmental Psychologyfatima bilalNo ratings yet
- Surrogacy Laws in India and in Other Foreign Countries - PowerpointDocument36 pagesSurrogacy Laws in India and in Other Foreign Countries - PowerpointSAYANTAN ROYNo ratings yet