Professional Documents
Culture Documents
Saketh Bhupathiraju - Research Assessment 6 - Major
Saketh Bhupathiraju - Research Assessment 6 - Major
Uploaded by
api-5022818330 ratings0% found this document useful (0 votes)
47 views2 pagesOriginal Title
saketh bhupathiraju - research assessment 6 - major
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
47 views2 pagesSaketh Bhupathiraju - Research Assessment 6 - Major
Saketh Bhupathiraju - Research Assessment 6 - Major
Uploaded by
api-502281833Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Research Assessment #6
Date: October 24, 2019
Subject: Treatment of Aortic Dissection Stanford Type A (Contd.)
MLA Citation:
Khayat, M., Cooper, K., Khaja, M., Gandhi, R., Bryce, Y., & Williams, D. (2018, April).
Endovascular management of acute aortic dissection. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5949590/
Analysis
The manifestation of true knowledge transcends a numerical grade and encompasses a
vision for one day applying that knowledge. Such perspectives were consistently accentuated in
my enlightening conversation with Dr.Wael Abo-Auda today. On that account, I aspire to
cultivate that relentless hunger for learning by elaborating on my questions on the endovascular
management of aortic dissections.
Through a deeper dive into this comprehensive article, I was able to attribute the
treatment of Stanford Type A dissections to surgical intervention through the employment of
“hypothermic circulatory arrest” and “cardiopulmonary bypass”. In that sense, I think that the
invasiveness of these procedures in the reconstruction of the true lumen is a testament to the
rapid and extensive nature of a dissection’s prognosis. Furthermore, I was surprised that the role
of endovascular management in Stanford Type A is typically isolated to branch endografts and
retrograde dissections that “extend into the ascending aorta”. Therefore, I think that the criticality
of the location of Stanford Type A has contributed to the historical prevalence of surgical
procedures as the primary course of treatment. On the other hand, the lack of impending rupture
that constitutes uncomplicated type B dissections has enabled treatment, fascinatingly , by
medicine alone. In addition, the popularity of thoracic endovascular aortic repair (TEVAR)
procedures is a reflection of the cognizance towards of progressive complications in rupture. For
me, this provides a perspective on how the potential volatility of dissections can blur the
distinction between complicated and uncomplicated cases. Furthermore, I was exposed to the
significance of diagnostic imaging in gaining an accurate representation of values such as branch
diameter, the location of tears, and angulation when pursuing endovascular management to
restore perfusion and thrombose the false lumen. In essence, I learned that the accumulation of
this information is critical in the development of a custom endograft to accommodate the
redirection of circulation via the true lumen channel to undermine aneurysmal degeneration.
However, I was confused by how retrograde false lumen thrombosis can cause visceral
malperfusion because I initially believed that the thrombosis of the false lumen channel is critical
in reducing the risk of rupture. Does the thrombosis of the retrograde false lumen create
increased branch vessel damage due to increased pressure or are the vessels occluded due to
thrombosis at the arch of the aorta? How do the effects of the closure of the primary tear differ
from those of the thrombosed retrograde channel? How is a dissection flap fenestration effective
despite the sustenance of blood flow to the false lumen and how is rupture/aneurysmal
degeneration then avoided in the long-term?
On that note, I hope to conduct further research on the premise of dissection flap
fenestrations and their effectiveness. I feel that the curiosity and confusion that I have fostered
this week will serve as momentum into my search for answers next week. In addition, I feel that
I’ve continued to be exposed to valuable knowledge regarding the importance of vessel anatomy
and the valuable distinctions of complicated vs.uncomplicated determine the efficacy of
diagnosis and treatment. I’d like to conclude my assessment with a resonating quote from
Dr.Abo-Auda, “ the eye does not see what the mind does not know”.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- ITE Crash Course - CardiologyDocument260 pagesITE Crash Course - CardiologyDre2323No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Aortic Dissection PP PresentationDocument64 pagesAortic Dissection PP PresentationKonstantin DimitrovNo ratings yet
- Aortoiliac DiseaseDocument110 pagesAortoiliac DiseaseAmr AbdelghaffarNo ratings yet
- Extracranial Carotid Artery Aneurysm - UpToDateDocument25 pagesExtracranial Carotid Artery Aneurysm - UpToDateDiego RodriguesNo ratings yet
- Amls Pretest BlsDocument13 pagesAmls Pretest BlsrkopecmdNo ratings yet
- Chest Pain and DiscomfortDocument2 pagesChest Pain and DiscomfortGerryNickNo ratings yet
- Evaluation and Treatment of Hypertensive Emergencies in Adults - UpToDateDocument13 pagesEvaluation and Treatment of Hypertensive Emergencies in Adults - UpToDaterolland_arrizaNo ratings yet
- Test Taking StrategyDocument15 pagesTest Taking StrategyAumrishNo ratings yet
- Chest X-RayDocument39 pagesChest X-Rayendah cahya sufianyNo ratings yet
- Use of "Bioglue" in Aortic Surgical RepairDocument3 pagesUse of "Bioglue" in Aortic Surgical RepairLeonardoCampanelliNo ratings yet
- Abdominal Aortic AneurysmDocument10 pagesAbdominal Aortic AneurysmSNo ratings yet
- Erythema Marginatum Chorea: Migratory Polyarthritis Cardiac Involvement Subcutaneous NodulesDocument27 pagesErythema Marginatum Chorea: Migratory Polyarthritis Cardiac Involvement Subcutaneous NodulesMisbah KaleemNo ratings yet
- Stroke Mimics: Incidence, Aetiology, Clinical Features and TreatmentDocument18 pagesStroke Mimics: Incidence, Aetiology, Clinical Features and TreatmentCristianNo ratings yet
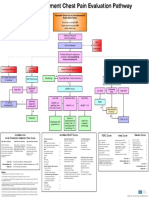
- Emergency Department Chest Pain Evaluation PathwayDocument2 pagesEmergency Department Chest Pain Evaluation Pathwaymuhammad sajidNo ratings yet
- Philippines Relative Value Unit:Surgeries 2007Document6 pagesPhilippines Relative Value Unit:Surgeries 2007Katherine 'Chingboo' Leonico Laud50% (2)
- DsaDocument235 pagesDsaLalaine De Jesus100% (1)
- Chest Pain in Pediatrics: Tisha K. Yeh, MD and Jay Yeh, MDDocument5 pagesChest Pain in Pediatrics: Tisha K. Yeh, MD and Jay Yeh, MDMahmoud AbouelsoudNo ratings yet
- Radiology Ordering GuideDocument27 pagesRadiology Ordering GuideRahim Rajab AliNo ratings yet
- Unit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsDocument85 pagesUnit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsCherry RahimaNo ratings yet
- IVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesDocument151 pagesIVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesMarc Imhotep Cray, M.D.100% (2)
- Cardiologia Croatica 2021 16 - 1-2 - 83Document1 pageCardiologia Croatica 2021 16 - 1-2 - 83daia4322746No ratings yet
- Journal (10 24 22)Document3 pagesJournal (10 24 22)Louigen DagaydayNo ratings yet
- Acute Limb IschemicDocument14 pagesAcute Limb IschemicLuke FloydNo ratings yet
- Turner Syndrome: A Guide For FamiliesDocument30 pagesTurner Syndrome: A Guide For FamiliesTatiana Pogo RamosNo ratings yet
- Internal Medicine Essentials For Clerkship Students 2Document369 pagesInternal Medicine Essentials For Clerkship Students 2asdf234234888100% (5)
- Vascular EmergenciesDocument43 pagesVascular EmergenciesMohammad BanisalmanNo ratings yet
- Full Download pdf of Vascular Medicine: A Companion to Braunwald’s Heart Disease 3rd Edition Mark Creager - eBook PDF all chapterDocument69 pagesFull Download pdf of Vascular Medicine: A Companion to Braunwald’s Heart Disease 3rd Edition Mark Creager - eBook PDF all chapterlugeydieen100% (4)
- ABSTRACT TEVAR - Achmad Ismail S Putra NewDocument3 pagesABSTRACT TEVAR - Achmad Ismail S Putra NewPutra AchmadNo ratings yet
- Diseccion Aortica Acguda CronicaDocument10 pagesDiseccion Aortica Acguda Cronicaarturo garciaNo ratings yet
- Old Free 120 - Answers & Explanations (BW)Document17 pagesOld Free 120 - Answers & Explanations (BW)frabziNo ratings yet