Professional Documents
Culture Documents
Asthma PDF
Uploaded by
Sophia Fulache0 ratings0% found this document useful (0 votes)
29 views1 pageOriginal Title
Asthma.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views1 pageAsthma PDF
Uploaded by
Sophia FulacheCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Asthma
Wednesday, January 15, 2020 10:47 PM
A chronic inflammatory disorder of the respiratory track. Most common illness in children. Increased bronchial reactivity to a variety of stimuli, which produces
episodic bronchospasm and airway obstruction. Asthma onset in adulthood: often without distinct allergies. Asthma onset in ch ildhood: often associated with
definite allergens. Prognosis: More than half of asthmatic children become asymptomatic as adults; more than half with onset after age 15 have persistent
disease, with occasional severe attacks. Status asthmaticus is an acute asthma attack that fails to clear with bronchodilator therapy.
Causes and Pathophysiology Assessment
- Allergy - History
○ Family history ○ Intermittent attacks of dyspnea and wheezing
○ Seasonal occurrence ○ Eczema
*Release of mast cell vasoactive and bronchospastic mediators ○ Allergic rhinitis (Hay fever)
- Upper airway infection - Clinical Features
- Exercise ○ Mild wheezing progressing to severe dyspnea
- Anxiety ○ Audible wheezing
- Rarely, coughing or laughing ▪ Initial wheezing can be heard through auscultation
- Paroxysmal airway obstruction associated nasal polyps ○ Chest tightness (feeling not able to breathe)
○ Seen in response to aspirin or indomethacin ingestion ○ Cough productive of thick mucus
Airway obstruction from spasm of bronchial smooth muscle narrows - Other signs
airways; inflammatory edema of the bronchial wall and inspissation of ○ Prolonged expiration
tenacious mucoid secretions are important, particularly in status ○ Intercostal and supraclavicular retraction on inspiration
asthmaticus ○ Use of accessory muscle of respiration
○ Nasal flaring
○ Tachypnea
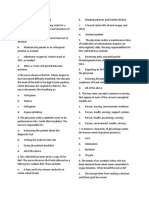
Confirming Diagnostic Measures ○ Tachycardia
- Physical Examination ○ Perspiration
○ Rhonchi and wheezing throughout the lung fields on expiration, at ○ Flushing
times, inspiration ○ Hay fever (allergic rhinitis)
○ Absent or diminished breath sounds during severe obstruction ○ Eczema
○ Loud bilateral wheezes may be grossly audible
○ Chest is hyperinflated
- Chest X-ray
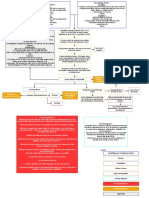
Therapeutic Management
○ Hyperinflated lungs with air tapping during attack - 4 components
○ Normal during remission ○ Measure asthma assessment and monitoring
- Sputum ▪ History and physical examination
○ Presence of Curschmann's spirals (cast of airways) ▪ Objective testing for asthma severity and control
○ Education for home self-management
○ Charcot-Leyden crystals (microscopic crystals composed of eosinophil
○ Control of environmental factors
protein)
○ Eosinophils ○ Pharmacologic therapy
- Pulmonary Test Function ▪ Beta-adrenergic agents
○ During attacks ▪ Methylxantines
▪ Decreased forced expiratory volumes ▪ Corticosteroids
▪ Increased residual volume - Emergency Treatment
▪ Occasionally, increased total lung capacity; may be normal ○ O2 therapy
between attacks ○ Corticosteroids
- Arterial Blood Gases ○ Bronchodilators
○ Decreased PO2 - Monitor for deteriorating respiratory status
○ Increased PCO2 (in severe attacks) - Note sputum characteristics
- EKG - Provide adequate fluid intake and oxygen, as ordered
○ Sinus tachycardia during attacks - Prevention
○ In severe attacks, cor pulmonae (right axis deviation, peaked p wave) ○ Avoid possible allergens
- Skin Test ○ Use antihistamines, decongestants, cromolyn powder and
○ Identify allergen bronchodilators
○ Explain the influence of stress and anxiety on asthma and frequent
association with exercise (particularly running) and cold air
Diseases Page 1
You might also like
- Psychia Practice QuestionsDocument13 pagesPsychia Practice QuestionsSophia FulacheNo ratings yet
- Psychiatric NursingDocument7 pagesPsychiatric NursingSophia FulacheNo ratings yet
- Community Health NursingDocument20 pagesCommunity Health NursingSophia FulacheNo ratings yet
- Fundamentals of Nursing Care for PatientsDocument7 pagesFundamentals of Nursing Care for PatientsSophia FulacheNo ratings yet
- Maternal and Child Nursing Signs and StagesDocument22 pagesMaternal and Child Nursing Signs and StagesSophia FulacheNo ratings yet
- Ob Drug StudyDocument3 pagesOb Drug StudySophia FulacheNo ratings yet
- Antivirals (E.g. Acyclovir, Famiciclovir)Document2 pagesAntivirals (E.g. Acyclovir, Famiciclovir)Sophia FulacheNo ratings yet
- Contact and Atopic DermatitsDocument1 pageContact and Atopic DermatitsSophia FulacheNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- AR 40-8 Effective 16 June 2007Document10 pagesAR 40-8 Effective 16 June 2007kbin3838No ratings yet
- Sports Injuries ManagementDocument94 pagesSports Injuries ManagementSaha DirllahNo ratings yet
- A Cure For Cancer Hidden in Plain Sight July 2019 DR David WilliamsDocument8 pagesA Cure For Cancer Hidden in Plain Sight July 2019 DR David WilliamsThomas Van Beek100% (2)
- Stomach CancerDocument14 pagesStomach CancerLamy SNo ratings yet
- Antiarrhythmic Drugs 1Document32 pagesAntiarrhythmic Drugs 1AliImadAlKhasakiNo ratings yet
- Erectile DysfunctionDocument31 pagesErectile Dysfunctionrahuldtc100% (1)
- Homeopathic Materia Medica by Dunham Sulphur (Sulph) : Aloes GraphitesDocument17 pagesHomeopathic Materia Medica by Dunham Sulphur (Sulph) : Aloes GraphiteskivuNo ratings yet
- AHA Elearning - ACLS Precourse Self-Assessment and Precourse WorkDocument3 pagesAHA Elearning - ACLS Precourse Self-Assessment and Precourse WorkAmmar bushraNo ratings yet
- Signs in MedicineDocument25 pagesSigns in MedicinepavanNo ratings yet
- Holistic Perspective of Physical TherapyDocument31 pagesHolistic Perspective of Physical TherapyShimmering MoonNo ratings yet
- 12 SP Physical Edu CbseDocument9 pages12 SP Physical Edu CbseshivamNo ratings yet
- Post Op InstructionsDocument5 pagesPost Op InstructionsAmar Bhochhibhoya0% (1)
- PHARMA BulletsDocument6 pagesPHARMA BulletsRhea Anne VeraNo ratings yet
- Ayurved TerminologiesDocument30 pagesAyurved TerminologiesVipul RaichuraNo ratings yet
- CTR Master Class CourseDocument15 pagesCTR Master Class CourseCool N CoolNo ratings yet
- Platelet Rich FibrinDocument7 pagesPlatelet Rich FibrinNelly AndriescuNo ratings yet
- InflammationDocument17 pagesInflammationNajwa AbdualgaderNo ratings yet
- NBME Answer With Explanation in DepthDocument10 pagesNBME Answer With Explanation in DepthDejan Zolak100% (3)
- Chapter 10 - Immune Responses Against Tumors and TransplantsDocument11 pagesChapter 10 - Immune Responses Against Tumors and TransplantsFYMNo ratings yet
- Dimension EXL 200/EXL With LM Integrated Chemistry Systems: Global Test MenuDocument2 pagesDimension EXL 200/EXL With LM Integrated Chemistry Systems: Global Test MenuGuneyden GuneydenNo ratings yet
- DM GerontikDocument15 pagesDM GerontikPuji Affan Dwi MiriyantoNo ratings yet
- Mandala Coloring For Children With Symptoms of Attention Deficit Hyperactivity Disorder - A Case SeriesDocument7 pagesMandala Coloring For Children With Symptoms of Attention Deficit Hyperactivity Disorder - A Case Seriesindex PubNo ratings yet
- AIIMS (MBBS) Solved Question Paper 2010Document34 pagesAIIMS (MBBS) Solved Question Paper 2010cbsestudymaterialsNo ratings yet
- CostipitationDocument4 pagesCostipitationashmi akberNo ratings yet
- Sinusitis LectureDocument66 pagesSinusitis LectureDada Doni100% (2)
- OB Power Point Presentation 002Document57 pagesOB Power Point Presentation 002RitamariaNo ratings yet
- Is Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsDocument11 pagesIs Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsClaudia FreyonaNo ratings yet
- Jazel Ibon Galon PDFDocument2 pagesJazel Ibon Galon PDFJazel GalonNo ratings yet
- Prevention of Adverse ReactionsDocument15 pagesPrevention of Adverse Reactionscupuwatie cahyaniNo ratings yet
- Jurnal Kesehatan Gigi: Perilaku Dan Keterampilan Menyikat Gigi Terhadap Timbulnya Karies Gigi Pada Anak Di Kota JambiDocument7 pagesJurnal Kesehatan Gigi: Perilaku Dan Keterampilan Menyikat Gigi Terhadap Timbulnya Karies Gigi Pada Anak Di Kota JambiUntuk TugasNo ratings yet