Professional Documents
Culture Documents
Lesions of The Corpus Callosum: Residents
Uploaded by
Ingrid AykeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lesions of The Corpus Callosum: Residents
Uploaded by
Ingrid AykeCopyright:
Available Formats
Residents’ Section • Pat tern of the Month
Ho et al.
Lesions of the Corpus Callosum
Residents’ Section
Pattern of the Month
Residents
inRadiology Lesions of the Corpus Callosum
Mai-Lan Ho1
T
his article reviews the causes and imaging appearances of lesions involving the cor-
Gul Moonis1 pus callosum (Table 1). The corpus callosum consists of densely bundled white mat-
Daniel T. Ginat 2 ter tracts connecting the two cerebral hemispheres, with a compact structure that
Ronald L. Eisenberg1 largely blocks interstitial edema and tumor spread. Isolated lesions of the corpus
callosum are rare and may represent transient responses to injury or myelination abnormalities.
Ho ML, Moonis G, Eisenberg RL More common butterfly lesions involve the corpus callosum and both cerebral hemispheres—a
pattern associated with aggressive tumors, demyelination, and traumatic brain injury.
American Journal of Roentgenology 2013.200:W1-W16.
Unenhanced CT is a first-line neuroimaging modality. Although soft-tissue contrast enhance-
ment is limited, CT can help characterize hemorrhage, edema, mass effect, calcification, and ne-
crosis. MRI provides more detailed informa-
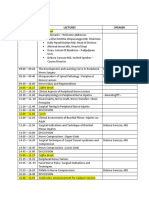
tion regarding tissue structure and composi- TABLE 1: Lesions Involving the
tion, using various pulse excitation sequences, Corpus Callosum
such as FLAIR, to distinguish abnormal signal
Neoplastic
in the corpus callosum from adjacent CSF in
the lateral ventricles. Administration of IV Glioma
contrast material is useful for characterization Lymphoma
of neoplastic and vascular lesions, which may Meningioma
show characteristic patterns of enhancement.
Metastases
Neoplastic Lesions Neurodystrophic
Glioma Demyelinating diseases
Glioblastoma multiforme (GBM) is the most Hereditary leukoencephalopathies
common and aggressive primary brain tumor
Wallerian degeneration
in adults, classified histologically as World
Health Organization (WHO) grade IV, with a Trauma or exposure
Keywords: brain, corpus callosum
median survival time of 14 months. Tumors Traumatic brain injury
DOI:10.2214/AJR.11.8080 can involve both cerebral hemispheres, with Hypoxic-ischemic encephalopathy
extension across the corpus callosum produc-
Received October 7, 2011; accepted after revision Marchiafava-Bignami disease
May 8, 2012.
ing a classic butterfly appearance. On CT,
GBM appears as an irregular, heterogeneous CSF shunting
1
All authors: Department of Radiology, Beth Israel mass with peritumoral vasogenic edema or Congenital
Deaconess Medical Center and Harvard Medical School, mass effect and possible internal areas of ne-
330 Brookline Ave, Boston, MA 02115. Address Callosal malformations
crosis, calcification, and hemorrhage (Fig. 1A).
correspondence to R. L. Eisenberg Lipoma
(rleisenb@bidmc.harvard.edu). On MRI, tumor is heterogeneously T1 hypoin-
tense and T2 hyperintense, with possible foci Vascular
2
Department of Radiology, Massachusetts General of susceptibility, vascular flow voids, and ir- Infarct
Hospital, Boston, MA. regular contrast enhancement (Fig. 1B). Aneurysm
WEB Gliomatosis cerebri is a slow-growing,
Arteriovenous malformation
This is a Web exclusive article. diffuse form of glioma, classified as WHO
grade III. By definition, it infiltrates two or Callosal gliosis
AJR 2013; 200:W1–W16 more lobes and shows minimal contrast en- Periventricular leukomalacia
0361–803X/13/2001–W1
hancement (Fig. 2). The prognosis is slightly Virchow-Robin spaces
better than GBM, with a median survival
Infection or inflammation
© American Roentgen Ray Society time of 12 months.
AJR:200, January 2013 W1
Ho et al.
A B
Fig. 1—Glioblastoma multiforme.
American Journal of Roentgenology 2013.200:W1-W16.
A, Unenhanced CT image shows heterogeneously hypodense mass with surrounding vasogenic edema. This
involves both frontal lobes and crosses genu (G) of corpus callosum, producing butterfly appearance. There is
compression and distortion of frontal horns of both lateral ventricles.
B, Contrast-enhanced T1-weighted MR image shows involvement of genu (G). Lesion shows rim enhancement
and central hypointensity, compatible with necrosis.
Fig. 2—Gliomatosis cerebri. FLAIR MR image
shows amorphous signal abnormalities infiltrating
both cerebral hemispheres, and extending across
midline (arrow).
Lymphoma
Primary CNS lymphoma is a rare and aggressive neoplasm that preferentially affects im-
munocompromised patients and can involve or extend through the corpus callosum. The hy-
percellular histology manifests with increased density on unenhanced CT. Lesions are multi-
focal and nodular, tending to show less mass effect and peritumoral edema than expected for
the size [1, 2] (Fig. 3A). MR signal is generally T1 iso- to hypointense and T2 iso- to hyper-
intense to gray matter (Fig. 3B). There is usually slow internal diffusion and mild homoge-
neous contrast enhancement (Fig. 3C). An important variant is HIV-associated lymphoma,
which is more likely to produce significant surrounding edema as well as central necrosis
with characteristic ring enhancement. Lymphoma is highly radiosensitive and regresses rap-
idly with steroid treatment (so-called “vanishing lesions”) [3].
W2 AJR:200, January 2013
Lesions of the Corpus Callosum
A B
Fig. 3—Primary CNS lymphoma.
A, Unenhanced CT image shows multiple hyperdense
American Journal of Roentgenology 2013.200:W1-W16.
masses, consistent with hypercellular malignancy.
There is involvement of right caudate nucleus (C) and
thalamus (T), extending into corpus callosum (arrow).
B, Contrast-enhanced CT image in different patient
reveals butterfly lesion with increased signal in
splenium (arrow) and extension into both parietal
lobes. (Courtesy of Ginat DT, Massachusetts General
Hospital, Boston, MA)
C, Contrast-enhanced T1-weighted MR image in
same patient as in B confirms mild homogeneous
enhancement within mass (arrow). (Courtesy of Ginat
DT, Massachusetts General Hospital, Boston, MA)
Meningioma
Meningioma is the second most common primary CNS neoplasm and the most common
nonglial tumor. In less than 10% of cases, lesions arise from midline and parasagittal dural
surfaces, and can secondarily involve the corpus callosum. On CT, there is increased attenu-
ation due to hypercellularity as well as coarse internal calcifications. On MRI, contrast en-
hancement is avid and generally homogeneous, although hemorrhage, cavitation, and necro-
sis may be seen in larger lesions (Fig. 4).
Metastasis
Metastasis to the corpus callosum is rare. More frequently, there is contiguous extension of
tumor from adjacent structures. Imaging characteristics depend largely on the primary malig-
nancy but generally involve mass effect, vasogenic edema, and heterogeneous contrast en-
hancement (Fig. 5).
Neurodystrophic
Demyelinating Diseases
Demyelinating diseases are acquired disorders of adulthood in which formerly normal
white matter is progressively destroyed by infectious, inflammatory, autoimmune, genetic,
toxic, or metabolic causes.
AJR:200, January 2013 W3
Ho et al.
A B
Fig. 4—Meningioma.
A, Unenhanced CT image shows round well-
circumscribed hyperdense mass (asterisk) centered
American Journal of Roentgenology 2013.200:W1-W16.
in falx cerebri (arrow) and extending across midline.
There is subtle surrounding edema that involves
bilateral temporooccipital regions.
B, T1-weighted contrast-enhanced MR image shows
relatively homogeneous contrast enhancement
within mass, which deviates surrounding pial vessels
(arrows).
C, FLAIR MR image shows vasogenic edema
extending into both parietal lobes, creating butterfly
pattern (arrows).
A B
Fig. 5—Intracranial metastases from primary lung cancer.
A and B, Contrast-enhanced CT (A) and contrast-enhanced T1-weighted MR (B) images show heterogeneously
enhancing dominant metastasis in left frontal lobe (asterisk). Additional enhancing foci are noted in splenium
(S), genu (G), and periventricular regions (arrows).
W4 AJR:200, January 2013
Lesions of the Corpus Callosum
Multiple sclerosis—Multiple sclerosis (MS) is the most common demyelinating disorder,
with presumed autoimmune and inflammatory causes. CT has a low positive predictive value
for detection of MS lesions. On MRI, the disease is T2 and FLAIR hyperintense, with con-
trast enhancement in the acute stage. The presence of subcallosal striations or callosal-septal
interface lesions, which are thin bands along the undersurface of the corpus callosum, is
highly sensitive and specific (Fig. 6A). Dawson fingers are ovoid lesions that radiate perpen-
dicularly from the lateral ventricles in a pattern thought to reflect perivenular demyelination
(Fig. 6B). In the chronic phase, T1-hypointense lesions (dark spots or black holes) reflect in-
creased water content secondary to extreme demyelination and axonal loss. Susceptibility
artifact on gradient recalled-echo/susceptibility-weighted imaging sequences indicates mac-
rophage and iron deposition in areas of permanent tissue destruction [4, 5].
Progressive multifocal leukoencephalopathy—Progressive multifocal leukoencephalopathy
is a rare demyelinating disease caused by John Cunningham virus replication in immunocom-
promised patients. There is resulting destruction of subcortical white matter, showing T1 hypo-
intensity and T2 hyperintensity on MRI. Lesions are typically multifocal and asymmetric, with
progressive enlargement and confluence over time. Corpus callosal involvement has been de-
scribed in 10–15% of published studies [1, 6–8]. There is no or minimal peripheral contrast
enhancement because of the patient’s inability to mount an adequate inflammatory response.
Hereditary Leukoencephalopathies
Hereditary leukoencephalopathies are congenital disorders of myelin formation or mainte-
American Journal of Roentgenology 2013.200:W1-W16.
nance, which may affect the corpus callosum. Metachromatic leukodystrophy is the most
common form and is caused by arylsulfatase A deficiency. Diffuse symmetric demyelination
results, with increased T2/FLAIR signal and global cerebral atrophy. Adrenoleukodystrophy
is a peroxisomal disorder due to acyl-CoA synthetase deficiency, which produces cerebral and
adrenal cortical dysfunction. Demyelination typically progresses from the parietooccipital to
frontotemporal lobes and involves the corpus callosum from posterior to anterior. Affected
regions appear hyperintense on T2-weighted FLAIR images and hypointense on T1-weighted
images with variable enhancement (Fig. 7). In certain cases, lesions may calcify or produce
mass effect. Other hereditary leukoencephalopathies include Alexander disease, Krabbe dis-
ease, and Sudanophilic leukodystrophy.
Wallerian Degeneration
Wallerian degeneration is a process of antegrade neural disintegration that develops after
injury to the proximal axon or cell body. For example, bilateral cerebral infarction can pro-
duce atrophy of the intervening corpus callosum due to Wallerian degeneration of the com-
missural fibers. Diffusion-weighted imaging is sensitive for early detection and quantification
of callosal degeneration [9–12] (Fig. 8).
A B
Fig. 6—Multiple sclerosis (MS).
A, Midline sagittal FLAIR MR image shows hyperintensity at interface between posteroinferior corpus
callosum (C) and septum pellucidum of lateral ventricles (S). Callosal-septal interface lesions are highly
sensitive and specific for MS.
B, Parasagittal FLAIR image shows radiating periventricular hyperintensities (subcallosal striations or Dawson
fingers), consistent with perivenular demyelination. Scattered nodular foci in deep white matter (arrows) are
also reflective of MS plaques.
AJR:200, January 2013 W5
Ho et al.
A B
Fig. 7—Hereditary leukoencephalopathies.
A and B, FLAIR MR images show signal abnormalities in bilateral parietal lobes and intervening splenium of
corpus callosum (arrows): metachromatic leukodystrophy (A) and adrenoleukodystrophy (B). (Courtesy of
American Journal of Roentgenology 2013.200:W1-W16.
Prabhu SP, Boston Children’s Hospital, Boston, MA)
Fig. 8—Wallerian degeneration. Apparent diffusion
coefficient MR image shows areas of reduced
diffusivity in bilateral occipital lobes (thin arrows),
as well as intervening splenium of corpus callosum
(thick arrow). This likely represents acute Wallerian
degeneration of crossing white matter tracts.
(Courtesy of Bhadelia R, Beth Israel Deaconess
Medical Center, Boston, MA)
Trauma and Exposures
Traumatic Brain Injury
Traumatic brain injury (TBI) is a primary cause of neurologic deficits in patients with se-
vere head trauma, most commonly high-speed motor vehicle accidents. The corpus callosum,
particularly the posterior body and splenium, are preferentially involved because of their
fixation to the overlying dura, with resulting torque injury. CT is not sensitive for TBI, but
shows hyperdense petechial foci of hemorrhage in 20% of cases (Figs. 9A and 9B). MRI is a
much more sensitive technique, with microhemorrhage detected as foci of magnetic suscepti-
bility on T2*-weighted gradient-recalled echo or susceptibility-weighted imaging sequences
(Figs. 9C and 9D). Nonhemorrhagic lesions show reduced diffusivity on diffusion-weighted
imaging, possibly with surrounding edema. Chronic lesions are associated with hemosiderin
and encephalomalacia. Diffusion-tensor imaging with tractography also holds promise for
detailed assessment of axonal injury [13–17].
Hypoxic-ischemic encephalopathy—Hypoxic-ischemic encephalopathy is a pattern of
brain injury resulting from partial oxygen deprivation due to hypoxic, hypoxemic, ischemic,
W6 AJR:200, January 2013
Lesions of the Corpus Callosum
A B
American Journal of Roentgenology 2013.200:W1-W16.
C D
Fig. 9—Traumatic brain injury.
A and B, Unenhanced CT images at level of lateral (A) and third (B) ventricles show hyperdense areas of acute
hemorrhage in splenium (S) and genu (G).
C and D, T2* gradient recalled-echo MR images at same levels confirm magnetic susceptibility in these areas.
There are multiple additional foci of microhemorrhage throughout gray-white matter junction and basal ganglia
(arrows).
or histotoxic causes. Lesions appear hypodense on CT and T1-hypointense and T2-hyperin-
tense on MRI (Fig. 10A) because of associated edema and encephalomalacia. Reduced dif-
fusivity (Fig. 10B) and contrast enhancement vary with the stage of injury. The corpus cal-
losum is affected in severe or advanced cases.
Marchiafava-Bignami disease—Marchiafava-Bignami disease is primary demyelination
of the corpus callosum after severe vitamin B12 deficiency. Usually seen in chronic alcoholic
patients, the clinical course may be acute and fulminant, affecting the genu and splenium; or
subacute to chronic, involving the body of the corpus callosum. In the early phase, affected
areas are edematous with T2 FLAIR hyperintensity, T1 hypointensity, reduced diffusivity,
and variable contrast enhancement (Fig. 11). There is selective involvement of the central
layer of the corpus callosum, resulting in a sandwich-like appearance. In the chronic stages,
affected regions become necrotic and atrophic, with minimal contrast enhancement. There
may be associated hemorrhage with susceptibility on gradient recalled-echo or susceptibility-
weighted imaging sequences.
AJR:200, January 2013 W7
Ho et al.
A B
Fig. 10—Hypoxic-ischemic encephalopathy.
A, T2-weighted MR image shows increased signal in globus pallidi (arrows) as well as in genu (G) and splenium
(S) of corpus callosum.
B, Diffusion-weighted MR image confirms reduced diffusivity within these same areas (arrows).
American Journal of Roentgenology 2013.200:W1-W16.
CSF Shunting
In patients with chronic hydrocephalus, placement of a new ventriculostomy catheter may
yield T1-hypointense and T2-hyperintense MR signal abnormalities in the corpus callosum.
The mechanism is incompletely understood and may involve biomechanical compression,
edema, ischemia, or demyelination or a combination. This entity should be considered when
new enlargement and signal changes are seen in the body of the corpus callosum. Often, there
is a scalloped appearance of the dorsal surface due to segmental tethering by pericallosal
artery branches (Fig. 12). No associated clinical symptoms have been reported [18].
Congenital
Callosal Malformations
Embryologically, the corpus callosum develops between the eighth and 20th weeks of gesta-
tion. Growth is primarily from anterior to posterior with the genu forming first, followed by the
anterior body, posterior body, and splenium. The rostrum is the last to form at 18–20 weeks [19].
A B
Fig. 11—Marchiafava-Bignami disease. (Courtesy of Ginat DT, Massachusetts General Hospital, Boston, MA)
A, FLAIR MR image shows increased signal in splenium (arrow).
B, Apparent diffusion coefficient map confirms reduced diffusivity in this region (arrow).
W8 AJR:200, January 2013
Lesions of the Corpus Callosum
Fig. 12—CSF shunting
in patient with chronic
hydrocephalus due to
tectal glioma. Sagittal
FLAIR MR image
shows enlargement
and characteristic
dorsal scalloping
of body of corpus
callosum (thin arrows).
Note hyperintense
mass involving tectal
plate (thick arrow).
(Courtesy of Ginat DT,
Massachusetts General
Hospital, Boston, MA)
Embryonic insults at different stages of development result in varying degrees of callosal dys-
genesis. On midline sagittal T1-weighted MRI, a radiating sunburst gyral pattern may be seen
American Journal of Roentgenology 2013.200:W1-W16.
because of nonconvergence of the major fissures. Absence of the splenium is associated with
posterior cerebral hypoplasia and ventricular colpocephaly. Complete agenesis produces paral-
lel “racecar” lateral ventricles and white matter tracts known as “Probst bundles.” The third
ventricle is also high riding and may form an interhemispheric arachnoid cyst at the level of the
absent corpus callosum (Fig. 13).
Fig. 13—Agenesis of corpus callosum.
A, Sagittal midline T1-weighted image shows
complete absence of corpus callosum (arrows).
B, Axial T2-weighted image shows colpocephalic
configuration with dilated occipital horns, right greater
than left (asterisks), and parallel (racecar) orientation of
lateral ventricles. Third ventricle (arrow) is high riding
and forms interhemispheric arachnoid cyst.
C, Axial T2-weighted image at higher level illustrates
crescentic (teardrop) morphology of frontal horns
(arrows).
B C
AJR:200, January 2013 W9
Ho et al.
Fig. 14—Callosal lipoma. (Courtesy of Ginat DT,
Massachusetts General Hospital, Boston, MA)
A, Axial T1-weighted unenhanced MR image shows
midline hyperintense mass (arrow), compatible with
lipoma.
B, Sagittal T1-weighted MR image shows curvilinear
lipoma along with mild dysgenesis of corpus callosum
(arrow).
A B
Lipoma
American Journal of Roentgenology 2013.200:W1-W16.
Intracranial lipomas are rare callosal or pericallosal lesions associated with persistence and
maldifferentiation of the meninx primitiva, which is the embryonic precursor of the meninges.
The morphology may be tubulonodular or curvilinear. Tubulonodular lipomas have a round or
cylindrical shape, are larger in diameter, and are usually located in the anterior brain. There is a
high association with frontal lobe anomalies, encephaloceles, and callosal dysgenesis. Curvilin-
ear lipomas are thin lesions that curve posteriorly around the splenium. Associated callosal mal-
formations are rarer and less severe [20].
On CT, lesions are homogeneous and well circumscribed, showing internal fat density (less
than −30 HU) and occasional rim calcification. On MRI, lesions are homogeneously T1 hyper-
intense and T2 hyperintense, following the signal of subcutaneous fat, and without appreciable
contrast enhancement (Fig. 14). Opposed-phase images may reveal chemical-shift artifact due
to macroscopic (bulk) fat. Loss of signal on fat-suppressed or STIR images confirms the pres-
ence of internal fat.
Vascular
The corpus callosum is supplied by multiple small penetrating vessels arising from the
anterior and posterior pericallosal arteries, which branch respectively from the anterior and
posterior cerebral arteries. Additional branches may arise from the anterior communicating
arteries, including subcallosal and median callosal arteries.
Infarct
Because of a rich collateral blood supply, corpus callosal infarcts are rare and associated
with systemic vasculitides, shower emboli, major ischemic stroke, or subfalcine herniation
with mass effect. The splenium is most commonly affected, followed by the body and genu.
CT lacks the necessary contrast resolution to identify mild edema associated with callosal
infarcts. On MRI, reduced diffusivity on diffusion-weighted imaging is the earliest sign, fol-
lowed by edema with T2 hyperintensity and T1 hypointensity (Fig. 15). Contrast enhance-
ment is variable but more likely in the acute phase. In the subacute to chronic stages, edema
evolves into gliosis or atrophy, with corresponding normalization of diffusivity. Hemorrhagic
transformation may manifest as magnetic susceptibility and chronic hemosiderin on gradient
recalled-echo and susceptibility-weighted imaging sequences.
Aneurysm
Midline and parasagittal cerebral aneurysms can occasionally rupture into the corpus cal-
losum. These usually arise from the distal anterior cerebral (Fig. 16A) or anterior communicat-
ing arteries (Figs. 16B–16E). Unenhanced CT is useful for localizing areas of hemorrhage, but
W10 AJR:200, January 2013
Lesions of the Corpus Callosum
A
American Journal of Roentgenology 2013.200:W1-W16.
B
Fig. 15—Callosal infarcts.
A, Left anterior cerebral artery infarct (thick arrow) with extension into genu (thin arrow) is seen on diffusion-
weighted (left) and apparent diffusion coefficient (ADC) (right) images, which confirm reduced diffusivity in
these areas.
B, Splenial infarct after evacuation of left epidural hematoma. Susceptibility artifact is noted in left occipital
lobe. There is postoperative subdural hygroma along left cerebral convexity (asterisk), resulting in mild
rightward subfalcine herniation. Diffusion-weighted (left) and ADC (right) images show acute splenial infarct
(arrow) secondary to compression of corpus callosum during herniation.
patients should be promptly evaluated with CT or MR angiography to assess the status of the
intracranial circulation. Treatment depends on aneurysm size and location and may involve
transarterial coil embolization or surgical craniotomy with clipping of the aneurysm neck.
Cerebral vasospasm, a feared complication of aneurysm rupture, may produce additional is-
chemia or infarction.
Arteriovenous malformation—Cerebral arteriovenous malformations (AVMs) involve the
corpus callosum in 10% of cases, with vascular involvement of both cerebral hemispheres.
Unenhanced CT is useful for identifying callosal hemorrhage, edema, mass effect, and calci-
fied phleboliths. Contrast-enhanced CT angiography or time-of-flight MR angiography can
help delineate the feeding arteries, central nidus, and draining veins. MRI may also show flow-
associated signal voids and magnetic susceptibility artifact in regions of calcification.
Small asymptomatic AVMs can be managed expectantly. Therapies for symptomatic lesions
include endovascular coil embolization, surgical resection, and stereotactic radiosurgery directed
at the central nidus. Outcomes correlate with the Spetzler-Martin grading system, which includes
AJR:200, January 2013 W11
Ho et al.
A B
American Journal of Roentgenology 2013.200:W1-W16.
C D
Fig. 16—Aneurysms.
A, CT angiogram of head shows right pericallosal
artery aneurysm (arrow) abutting anterior corpus
callosum, with coarse peripheral calcification.
B, Unenhanced CT image in different patient who
had ruptured anterior communicating artery
aneurysm. Lobulated hyperdense collection (asterisk)
suggestive of acute hematoma is visualized in
midfrontal region, involving genu of corpus callosum.
C, T2* gradient recalled-echo MR image verifies
magnetic susceptibility in region.
D, Sagittal contrast-enhanced magnetization-
prepared 180° radiofrequency pulses and rapid
gradient-echo (MP RAGE) image show lobulated rim-
enhancing collection (asterisk) involving genu.
E, Time-of-flight maximum-intensity-projection
image of circle of Willis depicts T1-hyperintense
hematoma (asterisk) surrounding ruptured anterior
communicating artery aneurysm.
E
W12 AJR:200, January 2013
Lesions of the Corpus Callosum
the size of the nidus, eloquence (degree of
functional importance) of adjacent brain, and
depth of venous drainage.
Callosal gliosis—Focally increased T2 signal
in the anteroinferior portion of the splenium
commonly occurs in patients with small-vessel
ischemic disease secondary to aging, subcorti-
cal arteriosclerotic encephalopathy (Binswanger
disease), or radiation therapy. Best appreciat-
ed on FLAIR MRI, this condition corresponds
pathologically to subependymal gliosis. There
is an association with periventricular white
matter disease (leukoaraiosis), which appears
hypodense on CT and hyperintense on T2-
weighted MRI (Fig. 17).
Periventricular leukomalacia—Periventric-
ular leukomalacia frequently affects premature
infants and is thought to represent watershed
infarction in the setting of low flow or decreased
Fig. 17—Callosal gliosis. Axial FLAIR image in patient
oxygen states. Severe cases may involve the
with left frontotemporal glioma after radiation shows corpus callosum, with cystic changes or hem-
American Journal of Roentgenology 2013.200:W1-W16.
vasogenic edema surrounding lesion as well as white orrhage reflecting ischemic damage to hemi-
matter hyperintensities in splenium (arrow) and spheric white matter tracts. MRI is useful for
periventricular regions.
identifying abnormal areas of signal change,
magnetic susceptibility, and reduced diffusivity
(Fig. 18).
Virchow-Robin spaces—Virchow-Robin spaces are dilated perivascular spaces that can occur
throughout the cerebral white matter, including the corpus callosum. They appear as well-circum-
scribed ovoid lesions isointense to CSF on all sequences. These lesions have no known clinical
significance but increase in size and frequency with age. There is an association with mucopolysac-
charidosis, in which accumulation of glycosoaminoglycans dilates the Virchow-Robin spaces and
produces a cribriform (état criblé) appearance in the white matter, corpus callosum, and basal
ganglia (Fig. 19).
A B
Fig. 18—Periventricular leukomalacia.
A, T2-weighted MR image shows periventricular white matter abnormalities, with increased signal in both
frontal and parietal lobes as well as genu (G) and splenium (S) of corpus callosum. Susceptibility artifact within
choroid plexus of occipital horns (asterisks) confirms presence of hemorrhage.
B, Diffusion-weighted MR image identifies reduced diffusivity within splenium (arrows) and multiple other areas.
AJR:200, January 2013 W13
Ho et al.
A B
Fig. 19—Virchow-Robin spaces in Hunter syndrome (mucopolysaccharidosis type 2). (Courtesy of Prabhu SP,
American Journal of Roentgenology 2013.200:W1-W16.
Boston Children’s Hospital, Boston, MA)
A, Axial FLAIR image shows diffusely enlarged perivascular spaces, which are isointense to CSF and involve
body of corpus callosum (arrows).
B, Sagittal T1 FLAIR contrast-enhanced image shows large Virchow-Robin spaces within corpus callosum
(arrow) and brain parenchyma.
Infection and Inflammation
Transient splenial signal changes have been reported in a wide variety of conditions, includ-
ing seizures, antiepileptic drug toxicity or withdrawal, sympathomimetic-induced kaleidoscop-
ic visual illusions, viral encephalitis, bacterial and parasitic meningitis, hypoglycemia, hyper-
natremia, osmotic myelinolysis, Wernicke encephalopathy, and hemolytic-uremic syndrome.
Lesions are well circumscribed and located in the central splenium, with T2 and FLAIR hyper-
intense and T1 hypointense signal. In the acute phase, contrast enhancement and reduced dif-
fusivity may be seen (Fig. 20). After disease recovery or withdrawal of the offending agent,
imaging abnormalities resolve over several weeks to months. The pathophysiology is poorly
A
Fig. 20—Transient splenial intensity changes.
A–C, Example images in migraine and visual scotomas (A), adenovirus encephalitis (B), and metronidazole
toxicity (C) show FLAIR hyperintensity and reduced diffusivity in splenium (arrows), which resolved on follow-
up imaging.
(Fig. 20 continues on next page)
W14 AJR:200, January 2013
Lesions of the Corpus Callosum
B
American Journal of Roentgenology 2013.200:W1-W16.
C
Fig. 20 (continued)—Transient splenial intensity changes.
A–C, Example images in migraine and visual scotomas (A), adenovirus encephalitis (B), and metronidazole
toxicity (C) show FLAIR hyperintensity and reduced diffusivity in splenium (arrows), which resolved on follow-
up imaging.
understood but is thought to reflect reversible demyelination and intracellular edema secondary
to infectious, inflammatory, or metabolic disturbances.
References of T1 black holes in patients with multiple sclero-
1. Bourekas EC, Varakis K, Bruns D. Lesions of the sis imaged monthly for 4 years. Brain 2003;
corpus callosum: MR imaging and differential 126:1782–1789
considerations in adults and children. AJR 2002; 5. Lassmann H. The pathologic substrate of mag-
179:251–257 netic resonance alterations in multiple sclerosis.
2. Castillo M. Lymphoma, primary. In: Castillo M. Neuroimaging Clin N Am 2008; 18:563–576
Neuroradiology companion: methods, guidelines, 6. Whiteman ML, Post MJ, Berger JR, et al. Pro-
and imaging fundamentals, 3rd ed. Philadelphia, gressive multifocal leukoencephalopathy in 47
PA: Lippincott Williams & Wilkins, 2005:146 HIV-seropositive patients: neuroimaging with
3. Slone HW, Blake JJ, Shah R, et al. CT and MRI clinical and pathologic correlation. Radiology
findings of intracranial lymphoma. AJR 2005; 1993; 187:233–240
184:1679–1685 7. Mark AS, Atlas SW. Progressive multifocal leuko-
4. Bagnato F, Jeffries N, Richert ND, et al. Evolution encephalopathy in patients with AIDS: appearance
AJR:200, January 2013 W15
Ho et al.
on MR images. Radiology 1989; 173:517–520 matic axonal injury. Neurology 2011; 77:818–826
8. Tartaglione T, Colosimo C, Antinori A, et al. Pro- 16. Newcombe V, Chatfield D, Outtrim J, et al. Map-
gressive multifocal leukoencephalopathy in patients ping traumatic axonal injury using diffusion ten-
with AIDS: findings with computerized tomogra- sor imaging: correlations with functional out-
phy and magnetic resonance. Radiol Med (Torino) come. PLoS One 2011; 6:e19214
1995; 90:8–15 17. Gasparetto EL, Rueda Lopes FC, Domingues RC,
9. Mukherjee P. Diffusion tensor imaging and fiber et al. Diffusion imaging in traumatic brain injury.
tractography in acute stroke. Neuroimaging Clin Neuroimaging Clin N Am 2011; 21:115–125
N Am 2005; 15:655–665 18. Lane JI, Luetmer PH, Atkinson JL. Corpus callo-
10. Thomalla G, Glauche V, Weiller C, et al. Time sal signal changes in patients with obstructive hy-
course of wallerian degeneration after ischaemic drocephalus after ventriculoperitoneal shunting.
stroke revealed by diffusion tensor imaging. J Am J Neuroradiol 2001; 22:158–162
Neurol Neurosurg Psychiatry 2005; 76:266–268 19. Barkovich AJ, Norman D. Anomalies of the cor-
11. Bianchi MT, Sims JR. Restricted diffusion in the pus callosum: correlation with further anomalies
splenium of the corpus callosum after cardiac ar- of the brain. AJR 1988; 151:171–179
rest. Open Neuroimag J 2008; 2:1–4 20. Ginat DT, Meyers SP. Intracranial lesions with high
12. Sylaja RN, Goyal M, Watson T, et al. Wallerian- signal intensity on T1-weighted MR images: differ-
like degeneration after ischemic stroke revealed ential diagnosis. RadioGraphics 2012; 32:499–516
by diffusion-weighted imaging. Can J Neurol Sci
2007; 34:243–244 Suggested Reading
13. Chang MC, Jang SH. Corpus callosum injury in 1. Gallucci M, Limbucci N, Paonessa A, Caranci F.
American Journal of Roentgenology 2013.200:W1-W16.
patients with diffuse axonal injury: a diffusion Reversible focal splenial lesions. Neuroradiology
tensor imaging study. NeuroRehabilitation 2010; 2007; 49:541–544
26:339–345 2. Shaikh R, Muttikkal TJ, Chavan VK. Callosal
14. Ljungqvist J, Nilsson D, Ljungberg M, et al. Longi- holes: an unusual imaging appearance in systemic
tudinal study of the diffusion tensor imaging prop- lupus erythematosus. Neuroradiol J 2009; 22:
erties of the corpus callosum in acute and chronic 165–168
diffuse axonal injury. Brain Inj 2011; 25:370–378 3. Uchino A, Takase Y, Nomivama K, Egashira R,
15. Wang JY, Bakhadirov K, Abdi H, et al. Longitu- Kudo S. Acquired lesions of the corpus callosum:
dinal changes of structural connectivity in trau- MR imaging. Eur Radiol 2006; 16:905–914
W16 AJR:200, January 2013
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Chapter 52 - Drugs Affecting The Urinary Tract and The BladderDocument12 pagesChapter 52 - Drugs Affecting The Urinary Tract and The BladderJonathonNo ratings yet
- Feng 2008Document3 pagesFeng 2008Ingrid AykeNo ratings yet
- Feng 2008Document3 pagesFeng 2008Ingrid AykeNo ratings yet
- Natural History of Chronic Subdural Haematoma: K.-S.LEEDocument8 pagesNatural History of Chronic Subdural Haematoma: K.-S.LEEAngelSosaNo ratings yet
- Natural History of Chronic Subdural Haematoma: K.-S.LEEDocument8 pagesNatural History of Chronic Subdural Haematoma: K.-S.LEEAngelSosaNo ratings yet
- Vezina 2009Document5 pagesVezina 2009Ingrid AykeNo ratings yet
- Vezina 2009Document5 pagesVezina 2009Ingrid AykeNo ratings yet
- Giant Invasive Spinal Schwannomas: Definition and Surgical ManagementDocument6 pagesGiant Invasive Spinal Schwannomas: Definition and Surgical ManagementIngrid AykeNo ratings yet
- Algattas 2020Document13 pagesAlgattas 2020Ingrid AykeNo ratings yet
- Giant Invasive Spinal Schwannomas: Definition and Surgical ManagementDocument6 pagesGiant Invasive Spinal Schwannomas: Definition and Surgical ManagementIngrid AykeNo ratings yet
- Asha 2020Document8 pagesAsha 2020Ingrid AykeNo ratings yet
- Asha 2020Document8 pagesAsha 2020Ingrid AykeNo ratings yet
- Ijss Oct Oa27 - 2018 PDFDocument6 pagesIjss Oct Oa27 - 2018 PDFIngrid AykeNo ratings yet
- Algattas 2020Document13 pagesAlgattas 2020Ingrid AykeNo ratings yet
- Cerebral Infarction Following Traumatic Carotid Cavernous Fistula in Adolescent Male A Case ReportDocument5 pagesCerebral Infarction Following Traumatic Carotid Cavernous Fistula in Adolescent Male A Case ReportIngrid AykeNo ratings yet
- Cerebral Infarction Following Traumatic Carotid Cavernous Fistula in Adolescent Male A Case ReportDocument5 pagesCerebral Infarction Following Traumatic Carotid Cavernous Fistula in Adolescent Male A Case ReportIngrid AykeNo ratings yet
- 5 6149941315837624367 PDFDocument4 pages5 6149941315837624367 PDFIde Bagoes InsaniNo ratings yet
- EU - WEST - 1 Prod s3 Ucmdata Evise C - O6293533 - 3249515Document16 pagesEU - WEST - 1 Prod s3 Ucmdata Evise C - O6293533 - 3249515Ingrid AykeNo ratings yet
- Neurosurgical Review 2020 PDFDocument538 pagesNeurosurgical Review 2020 PDFIngrid AykeNo ratings yet
- Strokeaha 110 591008 PDFDocument4 pagesStrokeaha 110 591008 PDFIngrid AykeNo ratings yet
- Neurosurgical Review 2020 PDFDocument10 pagesNeurosurgical Review 2020 PDFIngrid AykeNo ratings yet
- GCS PDFDocument1 pageGCS PDFFrincia100% (1)
- Peripheral Nerve Schedule PDFDocument3 pagesPeripheral Nerve Schedule PDFIngrid AykeNo ratings yet
- COVID 19 Pediatric Neurosurgery GuidelinesDocument1 pageCOVID 19 Pediatric Neurosurgery GuidelinesIngrid AykeNo ratings yet
- ACNSDocument1 pageACNSIngrid AykeNo ratings yet
- Virtual Memorial James T. Goodrich FB-1Document1 pageVirtual Memorial James T. Goodrich FB-1Ingrid AykeNo ratings yet
- Craniometrics and Ventricular Access PDFDocument9 pagesCraniometrics and Ventricular Access PDFIngrid AykeNo ratings yet
- Management of Multiply Injured Pediatric Trauma Patients in The Emergency Department Trauma CME Calculators PDFDocument5 pagesManagement of Multiply Injured Pediatric Trauma Patients in The Emergency Department Trauma CME Calculators PDFIngrid AykeNo ratings yet
- Furoshiki: Back in The Age ofDocument2 pagesFuroshiki: Back in The Age ofIngrid AykeNo ratings yet
- Ijss Oct Oa27 - 2018Document6 pagesIjss Oct Oa27 - 2018Ingrid AykeNo ratings yet
- Casali 2009Document6 pagesCasali 2009Giancarlo Maruri MunarettoNo ratings yet
- Mitral Valve ProlapseDocument7 pagesMitral Valve ProlapsehracakNo ratings yet
- Vector Borne DiseasesDocument3 pagesVector Borne DiseasesGo PrepNo ratings yet
- Jonathan C. Lubag Unintentional Injuries Q3M1 W1-3Document26 pagesJonathan C. Lubag Unintentional Injuries Q3M1 W1-3Jonathan LubagNo ratings yet
- Obat TeratogenikDocument24 pagesObat TeratogenikHidayat BazeherNo ratings yet
- Laporan GiziDocument11 pagesLaporan GiziEfrata MadridistaNo ratings yet
- Jama Echouffotcheugui 2023 RV 230007 1680895578.04302Document11 pagesJama Echouffotcheugui 2023 RV 230007 1680895578.04302Buton InspirasiNo ratings yet
- Yoga For Back PainDocument8 pagesYoga For Back Paingiorgino100% (1)
- FHP SampleDocument8 pagesFHP SampleJade GordoncilloNo ratings yet
- Lesson Plan: S.No Objectives Content Method of Teaching/ Teaching Aid Time in Min EvaluationDocument2 pagesLesson Plan: S.No Objectives Content Method of Teaching/ Teaching Aid Time in Min EvaluationNaqash HamayunNo ratings yet
- DOLICHOCOLONDocument6 pagesDOLICHOCOLONCassNo ratings yet
- Psyche 4 AnxietyDocument37 pagesPsyche 4 AnxietysimplyrosalynNo ratings yet
- Makassed Experience in Management of Placenta AccretaDocument39 pagesMakassed Experience in Management of Placenta AccretaRaluca HabaNo ratings yet
- MAPEHDocument3 pagesMAPEHGermaine Guimbarda MiguelesNo ratings yet
- HIV AwarenessDocument35 pagesHIV AwarenessCadine DavisNo ratings yet
- MINOR DISORDER IN PREGNANCY MaterialDocument8 pagesMINOR DISORDER IN PREGNANCY MaterialAnuradha MauryaNo ratings yet
- Health Certificate: Personal Details: Section ADocument3 pagesHealth Certificate: Personal Details: Section APrashob SugathanNo ratings yet
- AXR Made EasyDocument13 pagesAXR Made EasycswathikanNo ratings yet
- Parkinsons Disease FinalDocument2 pagesParkinsons Disease Finalapi-266655633No ratings yet
- Puerperal SepsisDocument4 pagesPuerperal SepsisSonali NayakNo ratings yet
- Neonatal HypertensionDocument21 pagesNeonatal HypertensionMuhammad Ammar Abdul WahabNo ratings yet
- Pep 2021 - October QuestionsDocument4 pagesPep 2021 - October QuestionsCynthia ObiNo ratings yet
- Daftar Pustaka PDFDocument3 pagesDaftar Pustaka PDFRatih Ayu PNo ratings yet
- Association Between Helicobacter Pylori Infection and Iron Deficiency Anemia: A Cross Sectional StudyDocument11 pagesAssociation Between Helicobacter Pylori Infection and Iron Deficiency Anemia: A Cross Sectional StudyHuỳnh Phương DuyNo ratings yet
- Abpsych Chapter 1Document4 pagesAbpsych Chapter 1Renz ReyesNo ratings yet
- Psychosurgery, Epilepsy Surgery, or Surgical Psychiatry: The Tangled Web of Epilepsy and Psychiatry As Revealed by Surgical OutcomesDocument2 pagesPsychosurgery, Epilepsy Surgery, or Surgical Psychiatry: The Tangled Web of Epilepsy and Psychiatry As Revealed by Surgical Outcomesximena sanchezNo ratings yet
- Guia 6. Trastorno Motor y SensitivoDocument47 pagesGuia 6. Trastorno Motor y SensitivoLorna Varela ArquinNo ratings yet
- Case History - 5Document8 pagesCase History - 5avnishNo ratings yet
- Modul Semester 1-1Document44 pagesModul Semester 1-1yuriNo ratings yet