Professional Documents
Culture Documents
EBP Implementation Leadership of Frontline Nurse Managers: Validation of The Implementation Leadership Scale in Acute Care
Uploaded by
jamie carpioOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EBP Implementation Leadership of Frontline Nurse Managers: Validation of The Implementation Leadership Scale in Acute Care
Uploaded by
jamie carpioCopyright:
Available Formats
Original Article
EBP Implementation Leadership of
Frontline Nurse Managers: Validation of the
Implementation Leadership Scale in Acute
Care
Clayton J. Shuman, PhD, RN ● Mark G. Ehrhart, PhD ● Elisa M. Torres, MS, PhD ●
Philip Veliz, PhD ● Lisa M. Kath, PhD ● Katherine VanAntwerp, BSN, RN ●
Jane Banaszak-Holl, PhD ● Marita G. Titler, PhD, RN, FAAN ● Gregory A. Aarons, PhD
Key words ABSTRACT
nursing leadership, Background: Frontline nurse managers influence the implementation of evidence-based prac-
implementation, tices (EBP); however, there is a need for valid and reliable instruments to measure their leader-
evidence-based ship behaviors for EBP implementation in acute care settings.
practice, Aim: The aim of this study was to evaluate the validity and reliability of the Implementation
psychometrics, acute Leadership Scale (ILS) in acute care settings using two unique nurse samples.
care
Methods: This study is a secondary analysis of ILS data obtained through two distinct multisite
cross-sectional studies. Sample 1 included 200 registered nurses from one large Californian
health system. Sample 2 was 284 registered nurses from seven Midwest and Northeast U.S.
hospitals. Two separate studies by different research teams collected responses using written
and electronic questionnaires. We analyzed each sample independently. Descriptive statistics
described individual item, total, and subscale scores. We analyzed validity using confirmatory
factor analysis and within-unit agreement (awg). We evaluated factorial invariance using multi-
group confirmatory factor analyses and evaluating change in chi-square and comparative fit
index values. We evaluated reliability using Cronbach’s alpha.
Results: Confirmatory factor analyses in both samples provided strong support for first- and
second-order factor structure of the ILS. The factor structure did not differ between the two
samples. Across both samples, internal consistency reliability was strong (Cronbach’s alpha:
0.91–0.98), as was within-unit agreement (awg: 0.70–0.80).
Linking Evidence to Action: Frontline manager implementation leadership is a critical contex-
tual factor influencing EBP implementation. This study provides strong evidence supporting
the validity and reliability of the ILS to measure implementation leadership behaviors of nursing
frontline managers in acute care. The ILS can help clinicians, researchers, and leaders in nursing
contexts assess frontline manager implementation leadership, deliver interventions to target
areas needing improvement, and improve implementation of EBP.
BACKGROUND what is done at the point of care delivery (Titler, 2018;
Evidence-based practice (EBP) has received widespread Titler & Shuman, 2017).
attention over the last few decades and is a national pri- Implementation science addresses the evidence-to-prac-
ority for improving quality of care and population health tice gap by investigating the “processes and factors that are
(Agency for Healthcare Research & Quality, 2015; Institute associated with successful integration of evidence-based in-
of Medicine, 2001). Numerous EBP resources are available terventions within a particular setting” (Rabin & Brownson,
to clinicians and healthcare organizations, including EBP 2018, p. 26) and testing strategies targeting these processes
guidelines and recommendations, systematic reviews, evi- and factors. The effect of contextual factors on implemen-
dence-summary reports, and EBP education programs (e.g., tation processes and outcomes is important and may help
workshops, inservices, webinars, certificate programs). to explain variation in the effectiveness of implementa-
Despite the availability of these resources, there remains tion strategies across care settings (May, Johnson, & Finch,
a substantial gap between what is known (evidence) and 2016).
82 Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91.
© 2019 Sigma Theta Tau International
Original Article
Frontline unit leadership is an important contex- leadership; (c) supportive leadership; and (d) perseverant
tual factor that has emerged in implementation science. leadership. The ILS, originally developed and tested in men-
Although job title varies across healthcare institutions tal health settings, has been cross-validated in substance use
(e.g., nurse manager, unit director), frontline nurse man- facilities (Aarons, Ehrhart, Torres, Finn, & Roesch, 2016),
agers are leaders who supervise clinical staff and are re- child welfare service organizations (Finn, Torres, Ehrhart,
sponsible for the quality of care and outcomes achieved Roesch, & Aarons, 2016), and education sectors (Lyon et al.,
on their units. They are responsible for staffing, oversee- 2018). However, it has yet to be validated for use in nursing
ing budgets, supporting educational opportunities, hiring contexts.
and firing staff, and establishing positive work environ- The purpose of this study is to evaluate the psychomet-
ments (American Organization for Nursing Leadership & ric properties of the ILS when used in acute care settings
American Organization of Nurse Executives, 2015). In light and completed by registered nurses providing direct pa-
of these responsibilities, they are well-situated to promote tient care. Using data from two independent samples, this
implementation and sustainability of EBP. study evaluates the first- and second-order factor structure
Previous studies demonstrate critical attributes and in each study independently. We then compare the factor
behaviors of leaders that influence EBP implementation structure across the two studies. We hypothesized that
(Aarons, Ehrhart, Farahnak, & Sklar, 2014; Birken et al., the ILS would demonstrate strong first- and second-order
2018; Gifford et al., 2018). For example, Shuman, Liu, and factor structure and high reliability in both samples, and
colleagues (2018) suggest that frontline leaders play a key factor structure would not significantly differ between
role in creating practice climates that foster and promote the two samples. In addition, we hypothesized that the
EBP implementation. Additionally, frontline managers are ILS would have good-to-excellent support for agreement
pivotal in planning for implementation efforts. In a study aggregated to the unit level, consistent with the concep-
of 102 Veterans Health Administration facilities, Robinson tualization of implementation leadership as a unit-level
et al. (2010) found that including frontline managers in im- construct (Aarons, Ehrhart, & Farahnak, 2014).
plementation planning improved implementation of a team
training program for operating room clinical staff. During
implementation, leadership behaviors of support, en- METHODS
couragement, and engagement have been associated with Design
higher fidelity to implementation strategies (Augustsson, This is a secondary analysis of ILS data from two multisite
von Thiele Schwarz, Stenfors-Hayes, & Hasson, 2015). cross-sectional studies—the first conducted in Southern
Other leadership behaviors of frontline managers that in- California in 2016 and the second conducted in the Midwest
fluence EBP implementation include ongoing monitoring and Northeast U.S. in 2016 (Shuman, 2017; Shuman, et al.,
and feedback to staff regarding EBP use, role modeling, 2018; Shuman, Powers, Banaszak-Holl, & Titler, 2019).
relationship building, supporting implementation efforts,
and providing resources (e.g., EBP workshops; Gifford et al., Samples
2018; Reichenpfader, Carlfjord, & Nilsen, 2015; Sandström, Sample 1: Southern California nurses
Borglin, Nilsson, & Willman, 2011; Shuman, Ploutz-Snyder, Study 1 recruited a convenience sample of nurses from a
& Titler, 2018). Despite recent findings regarding the im- large community hospital system in Southern California.
portance of frontline managers to EBP implementation, The hospital system consisted of several acute care and
common measures of frontline implementation leadership specialty hospital sites. After gaining permission from sys-
are not used across studies. This hinders our understand- tem- and hospital-level leadership at four sites, we distrib-
ing of the mechanisms by which frontline leaders influ- uted invitations to participate to registered nurses via email
ence implementation processes and outcomes. Studies are and in-person recruitment presentations provided during
needed to demonstrate the validity and reliability of prag- monthly unit meetings. All nurses providing direct care in
matic measures of leadership behaviors specific to EBP im- one of 78 units from the four hospitals were eligible for
plementation (Gifford et al., 2018; Lewis et al., 2015). participation.
To be more fully comprehend and evaluate the role
of frontline managers in EBP implementation, Aarons Sample 2: Midwest and Northeast U.S. nurses
Ehrhart & Farahnak (2014) developed the Implementation Study 2 was conducted in 24 adult medical-surgical units
Leadership Scale (ILS). The scale is informed by relevant nested within seven acute care community hospitals in
implementation and organizational research literature, Iowa, Minnesota, New Hampshire, and Vermont. We ran-
as well as the Exploration, Preparation, Implementation, domly selected 30 eligible nurses from each study unit to
Sustainment framework (Aarons, Hurlburt, & Horwitz, receive electronic questionnaires. For units with fewer than
2011). The scale focuses on specific leadership behaviors 30 eligible nurses, we invited all eligible nurses. Nurses
enacted by frontline managers to influence implementa- met the following inclusion criteria: worked a minimum
tion, including: (a) proactive leadership; (b) knowledgeable of 0.40 FTE; designated as staff on a study unit (e.g., not
Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91. 83
© 2019 Sigma Theta Tau International
Testing the ILS in Nursing
float pool or agency); and provided direct patient care. We pilot tested with four nurse managers and 26 nurses at two
invited a total of 553 nurses to participate via email. Iowa hospitals (not participating in the current study) to
establish content validity and evaluate appropriateness, us-
Measure ability, and relevance to nursing. No changes were made to
For both samples, we administered the 12-item ILS. The the ILS except for changing “supervisor” to “nurse man-
ILS consists of four dimensions, each consisting of three ager” to reflect the nursing context. Next, executive nursing
items. The four dimensions are as follows: proactive lead- leadership (e.g., chief nursing officers) and other nursing
ership, knowledgeable leadership, supportive leadership, leaders (e.g., nursing education directors) from each hos-
and perseverant leadership. Proactive leadership involves pital participated in 1-hr conference calls with investiga-
developing a plan to implement EBP, addressing barriers to tors to discuss the study, establish buy-in, and identify site
implementation, and establishing clear unit standards for coordinators to assist in recruitment and data collection.
implementation. Knowledgeable leadership relates to the We trained site coordinators to study procedures using a
manager’s competency in EBP. Supportive leadership in- detailed study manual and 90-min teleconference train-
cludes recognizing staff who use EBP and supporting staff ing meetings (see Shuman, 2017). After receiving IRB ap-
education in EBP. Finally, perseverant leadership involves proval from the university and all study hospitals, up to 30
the manager’s ability to navigate implementation challenges randomly selected nurses from each study unit received an
and address implementation problems. Participants scored email invitation to participate, with a link to a web-based
their frontline manager’s EBP implementation leadership questionnaire inclusive of the ILS. We asked participants to
behaviors on each item. Response anchors ranged from 0 respond within 1 month. Weekly email reminders and a
(not at all) to 4 (to a very great extent). Subscale scores are lottery drawing incentive for a $100 cash gift card encour-
determined by calculating the mean of responses to items aged response.
loading on each subscale. The mean of the subscales is com-
puted to create the total mean score. Statistical Analysis
Descriptive statistics (mean and standard deviation) sum-
Procedures marized item, subscale, and total scale scores for each
Sample 1: Southern California nurses sample. We assessed internal consistency reliability using
The research team made initial contact with the research Cronbach’s alpha. To evaluate within-unit agreement of
leadership at the Southern California hospital system to the measures, we calculated awg values. Values for awg
describe the study’s purpose and establish buy-in. Upon range from −1.00 to 1.00, with values? 0.60 considered
approval to move forward, members of the research team acceptable agreement for aggregating to the unit level
met with a group of nurse managers and educators at the (Brown & Hauenstein, 2005). Pearson product moment
hospital system to review the items for appropriateness in correlations between factors for each sample were com-
the nursing setting. No changes were made beyond minor puted to evaluate the higher order implementation lead-
wording adjustments for the nursing context (e.g., use of ership factor. We conducted confirmatory factor analysis
the term “nurse” instead of “employee”). After receiving utilizing Mplus statistical software (Muthén & Muthén,
institutional review board (IRB) approval from the uni- 1998–2016). The estimation method was maximum like-
versity and the participating hospital system, we recruited lihood estimation with robust standard errors, which ap-
participants through general email announcements of the propriately adjust standard errors and chi-square values
study and through in-person recruitment at unit meetings. accounted for the nested data structure (multiple nurses
For the in-person recruitment, participants could complete within nursing units). We accounted for missing data
hard copies of the survey or an online version through through full information maximum likelihood estima-
a provided survey link. For paper-and-pencil surveys, a tion. We assessed model fit using the comparative fit
member of the research team left a batch of blank surveys index (CFI), the root mean square error of approxima-
during a regularly occurring team meeting, which could tion (RMSEA), and the standardized root mean square
then be mailed in preaddressed envelopes or left at the hos- residual (SRMR). CFI values greater than 0.95, RMSEA
pital for a member of the research team to collect. Overall, values less than 0.06, and SRMR values less than 0.08 in-
129 responded to the online version of the survey and 71 dicate model fit that is deemed acceptable (Hu & Bentler,
responded to the paper-and-pencil version. No signifi- 1999). In order to test for factorial invariance (Dimitrov,
cant differences were found in the measures based on the 2010) between the two samples (i.e., are the results simi-
method of survey completion. Participants received a $5 lar between the two samples), we used multiple group
gift certificate to a retail coffee shop for their participation. modeling in Mplus to assess the invariance in the first-
and second-order factors between the two samples. Chi-
Sample 2: Midwest and Northeast U.S. nurses square difference tests using the scaling correction factor
Prior to this study, the ILS was reviewed by a group of four assessed if the model fit significantly changed when the
EBP experts and two nursing scientists. It was subsequently first- and second-order factors were constrained to be
84 Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91.
© 2019 Sigma Theta Tau International
Original Article
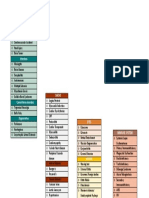
Table 1. Survey Respondent Characteristics for characteristics of Sample 2 are published elsewhere
Sample 1 (N = 200) and Sample 2 (N = 284) (Shuman et al., 2019).
Sample 1 Sample 2
n (%) n (%)
Psychometric Findings
Table 2 provides the ILS item means, standard deviations,
Age reliabilities, and aggregation statistics for each sample.
20–29 49 (24.5) 121 (42.6) Across both samples, the Cronbach’s alpha scores for all
30–39 65 (32.5) 64 (22.5) dimensions and overall scale ranged from 0.91 to 0.98,
demonstrating excellent internal consistency reliability.
40–49 44 (22.0) 38 (13.4)
Based on units with at least two respondents (Sample 1,
50+ 33 (16.5) 36 (12.7)
n = 40 units; Sample 2, n = 24 units), results of the awg
Missing 9 (4.5) 25 (8.8) ranged from 0.70 to 0.80, indicating support for within-
Race unit agreement and aggregation of participant responses to
White/ 107 (53.5) 237 (83.5) the unit level.
Caucasian Confirmatory factor analysis results in both samples
Black/African 30 (15.0) 3 (1.1) provided strong support for the ILS. In Sample 1, strong
American model fit statistics were found for the second-order factor
Asian/Pacific 33 (16.5) 2 (0.7) structure of the ILS (χ2(50) = 87.06, p < .001; CFI = 0.978,
Islander RMSEA = 0.061, 90% C.I. [.039, .082], probability
American 1 (.5) 2 (0.7) RMSEA ≤ .05 = .192; SRMR = 0.030). Similarly, the model
Indian/Alaskan fit statistics of Sample 2 supported the strong factor structure
Native (χ2(50) = 86.583, p < .001; CFI = 0.986, RMSEA = 0.051,
Other 19 (9.5) 10 (3.5) 90% C.I. [.032, .068], probability RMSEA ≤ .05 = .454;
Missing 10 (5.0) 30 (10.5) SRMR = 0.022). Thus, across both nursing samples there
was overall support for the ILS factor structure. As shown
Primary work shift
in Table 3, the standardized factor loadings for both sam-
Days 96 (48.0) 102 (35.9) ples are ≥ .83 and all are statistically significant (p < .001).
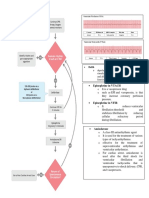
Evenings and 91 (45.5) 82 (28.9) Factor models for both samples are depicted in Figures 1
nights and 2. We found significant correlations (p < .05) among
Rotate – 82 (28.9) the four factors in both samples supporting a higher order
Missing 13 (6.5) 18 (6.3) implementation leadership factor (Table 4).
Table 5 provides the results testing for factorial invari-
ance for the first- and second-order factors between the
two samples. The results in Table 5 show evidence of in-
equal. Additionally, we also assessed the change in the variance with respect to both the first- and second-order
CFI as an additional step to assess model fit across the factor loadings between the two samples: the Chi-square
invariant and constrained models (Cheung & Rensvold, change statistic (∆χ2) is not statistically significant, and
2002). no change in the CFI was found across the models, in-
dicating that the factor structure is similar across both
samples. It should be noted here that the baseline model
RESULTS did have to constrain (to be invariant across the two
Participant Characteristics groups) three of the four first-order factor loadings to
Sample characteristics are provided in Table 1. Sample 1 estimate the baseline model without invariance (this was
included 200 nurses employed in 78 units in four hospi- due to the high correlation between items and factors in
tals from a regional hospital system located in Southern Sample 2; see Table 4). Despite this limitation in the an-
California. Sample 1 had an average age of 37.99 years alytic approach, the results do suggest high similarity in
(SD = 11.0) and average experience as a nurse of the first- and second-order factor loading between both
11.15 years (SD = 10.17). The majority of Sample 1 par- samples.
ticipants reported at least a bachelor’s degree or higher
in nursing (56.4%). Sample 2 included 284 nurses from
24 units in seven hospitals. The sample had an average DISCUSSION
age of 34.9 (SD = 11.94) and an average experience work- Frontline nurse leadership is an important context fac-
ing as a registered nurse of 7.84 (SD = 9.88). Most par- tor influencing EBP implementation; however, few vali-
ticipants had a baccalaureate degree (59.2%). Additional dated measures are available. Our study used data from
Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91. 85
© 2019 Sigma Theta Tau International
Testing the ILS in Nursing
Table 2. Descriptive Statistics for ILS Item and Dimensions for Sample 1 and Sample 2
Sample 1 Sample 2*
My direct
supervisor/nurse
manager… N Mean SD Alpha awg N Mean SD Alpha awg
Proactive leadership 198 2.32 1.05 .93 .80 280 2.67 .87 .90 .70
has developed a plan 199 2.30 1.15 281 2.68 .97
to facilitate
implementation of
EBPs
has removed 199 2.27 1.08 282 2.54 .95
obstacles to the
implementation of
EBPs
has established clear 198 2.40 1.12 283 2.80 .91
unit standards for
the implementation
of EBPs
Knowledgeable 198 2.70 .95 .96 .80 282 2.99 .80 .91 .79
leadership
is knowledgeable 198 2.72 1.00 284 3.12 .77
about EBPs
is able to answer my 198 2.67 1.00 282 2.89 .92
questions about
EBPs
knows what he or she 199 2.71 .97 283 2.98 .91
is talking about when
it comes to EBPs
Supportive leadership 198 2.75 .92 .95 .80 281 3.03 .80 .89 .77
recognizes and 198 2.73 .95 283 3.02 .85
appreciates nurses'
efforts toward
successful EBP
implementation
supports nurses' 200 2.73 .972 283 2.98 .95
efforts to learn more
about EBPs
supports nurses' 200 2.78 .98 283 3.09 .86
efforts to use EBPs
Perseverant 199 2.68 .97 .97 .80 282 2.84 .84 .91 .75
leadership
perseveres through- 199 2.70 1.01 283 2.81 .93
out the ups and
downs of implement-
ing EBPs
carries on through 199 2.68 1.01 282 2.83 .90
the challenges of
implementing EBPs
reacts to critical 199 2.68 .98 284 2.88 .91
issues regarding the
implementation of
EBPs
ILS total score 198 2.61 .90 .98 .80 275 2.88 .78 .97 .80
Note. SD = standard deviation; Alpha = Cronbach’s alpha; awg = average within-group agreement.
*Mean, standard deviation, and Cronbach’s alpha for Sample 2 have been previously published in Shuman et al., 2019.
86 Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91.
© 2019 Sigma Theta Tau International
Original Article
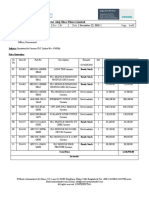
Table 3. Confirmatory Factor Analysis Results for Sample 1 and Sample 2
Sample 1 Sample 2
My direct supervisor/ Standardized factor Standardized factor
nurse manager… loading p Value loading p Value
Proactive leadership .86 <.001 .96 <.001
has developed a plan to .89 <.001 .89 <.001
facilitate implementation
of EBPs
has removed obstacles to .94 <.001 .88 <.001
the implementation of
EBPs
has established clear unit .90 <.001 .84 <.001
standards for the
implementation of EBPs
Knowledgeable leadership .88 <.001 .96 <.001
is knowledgeable about .93 <.001 .83 <.001
EBPs
is able to answer my .96 <.001 .90 <.001
questions about EBPs
knows what he or she is .94 <.001 .91 <.001
talking about when it
comes to EBPs
Supportive leadership .95 <.001 .94 <.001
recognizes and appreciates .91 <.001 .84 <.001
nurses' efforts toward
successful EBP
implementation
supports nurses' efforts to .92 <.001 .83 <.001
learn more about EBPs
supports nurses' efforts to .94 <.001 .90 <.001
use EBPs
Perseverant leadership .96 <.001 1.02 <.001
perseveres throughout the .98 <.001 .87 <.001
ups and downs of
implementing EBPs
carries on through the .97 <.001 .87 <.001
challenges of implement-
ing EBPs
reacts to critical issues .90 <.001 .87 <.001
regarding the implementa-
tion of EBPs
Note. EBP = evidence-based practice; standardized factor loading ≥1 due to high correlation among factors in Sample 2 (see Table 3).
two unique studies to validate the ILS in acute care nurs- factors that contribute to within-group agreement within
ing units. Both samples provide strong support for the units. Overall, the strength of these findings is notewor-
factor structure of the ILS, and factor loadings are simi- thy given that data were collected independently, by two
lar across samples. In addition, our results support aggre- different investigative teams, in very different geographic
gation of responses to the unit level, consistent with the areas of the U.S., and with broadly different nurse demo-
conceptualization of implementation leadership as a unit- graphics. Our results contribute to the strong record of the
level construct (Aarons et al., 2014). However, it should be scale’s validity and reliability in other contexts (Aarons
noted that Sample 2 aggregation values are not as strong et al., 2014; Aarons et al., 2016; Finn et al., 2016; Lyon et al.,
as Sample 1. Future studies are needed to determine the 2018; Torres et al., 2018).
Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91. 87
© 2019 Sigma Theta Tau International
Testing the ILS in Nursing
.26 ILS1 .21
.89
Proactive ILS2 .12
.94
leadership
.90
ILS3 .20
.22
ILS4 .14
.93
Knowledgeable .96
leadership
ILS5 .08
Implementation
leadership .95
ILS6 .10
.10
.91 ILS7 .18
Supportive
leadership .92
ILS8 .15
.94
ILS9 .12
.08
.98 ILS10 .04
Perseverant
leadership .97 ILS11 .16
.90
ILS12 .19
Figure 1. Sample 1 factor structure.
As a brief, pragmatic instrument of EBP implementa- Our study has some limitations worth noting. First,
tion leadership, the ILS is well-suited for inclusion in im- Sample 2 included adult medical-surgical units only,
plementation studies involving nurses in acute care. This and although Sample 1 included all units at one health
validation of the ILS allows for additional testing of the system, our sample may not include all types of nursing
effect of frontline nurse manager leadership behaviors units, thus affecting generalizability. Aggregation statis-
on implementation processes and outcomes. The four tics in Sample 2 are acceptable but not as strong as in
ILS domains (proactivity, knowledge, support, and per- Sample 1. Future studies are needed to explore intraunit
severance) can guide intervention work by highlighting alignment and its effect on EBP implementation. Finally,
areas for improvement in frontline leaders’ EBP imple- this study did not address the relationship of the ILS with
mentation leadership behaviors and testing interventions other implementation-related variables. Future stud-
targeted to these areas. For example, the Leadership and ies should address the interplay with other measures of
Organizational Change for Implementation program uses implementation context and implementation outcomes.
the ILS to help improve general and EBP implementa- Despite these limitations, our study, inclusive of two
tion-focused leadership of frontline managers and EBP unique samples, provides strong evidence supporting the
implementation climates in substance use treatment fa- validity and reliability of the ILS in acute care nursing
cilities (Aarons, Ehrhart, Moullin, Torres, & Green, 2017). settings.
88 Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91.
© 2019 Sigma Theta Tau International
Original Article
.09 ILS1 .21
.89
Proactive ILS2 .23
.88
leadership
.84
ILS3 .29
.09
ILS4 .31
.83
Knowledgeable .90
leadership
ILS5 .19
Implementation
leadership .91
ILS6 .18
.12
.84 ILS7 .29
Supportive
leadership .83
ILS8 .32
.90
ILS9 .20
–.04
.87 ILS10 .24
Perseverant
leadership .87 ILS11 .24
.87
ILS12 .24
Figure 2. Sample 2 factor structure.
IMPLICATIONS FOR RESEARCH AND Table 4. ILS Subscale Intercorrelation Matrix for
PRACTICE Sample 1 and Sample 2
Frontline nurse managers influence the implementation
and use of EBPs to improve care delivery and outcomes. 1 2 3 4
The ILS is a valid and reliable instrument that can be used
1. Proactive – .82 .80 .89
in future research to investigate frontline nurse managers’ leadership
leadership behaviors for EBP implementation in acute care.
2. Knowledgeable .79 – .83 .88
In addition to using the scale to address research questions leadership
important to implementation science, the ILS is a pragmatic
3. Supportive .74 .80 – .85
tool that frontline nurse managers can use for self-assess- leadership
ment, as well as for obtaining their staff perceptions re-
4. Perseverant .79 .81 .88 –
garding their leadership behaviors for EBP implementation. leadership
Identifying areas for improvement can guide nurse leaders
Note. All values significant at p < .01 level; correlations below the
in selection of programs or interventions to address prob-
diagonal correspond to Sample 1 and above the diagonal correla-
lem areas and improve their implementation leadership. tions correspond to Sample 2.
Improving their implementation leadership will contrib-
ute to more successful EBP implementation efforts on their
units, ultimately leading to improved care and outcomes.
Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91. 89
© 2019 Sigma Theta Tau International
Testing the ILS in Nursing
Table 5. Testing for Factorial Invariance of a Second-Order Factor Model Across the Two Samples
Model χ2 df Comparison ∆χ2 ∆df CFI ∆CFI RMSEA
M0 193.2 105 – – – .976 – –
M1 197.4 108 M0–M1 2.75 3 .976 .000 .058
M2 200.1 111 M2–M1 1.87 3 .976 .000 .058
Note. CFI = comparative fit index; RMSEA = root mean square error of approximation; ∆χ2 = Chi-square change using the scaling correction
factor (analyses use MLR); M0 = baseline model (without invariance. Note that factors for knowledgeable leadership, supportive leadership, and
perseverant leadership needed to be constrained to be invariant in order for the baseline model to estimate); M1 = first-order factor loadings
invariant; M2 = first-order and second-order factor loadings invariant.
CONCLUSIONS Research Professor, University of Michigan, Ann Arbor,
This study provides support for the use of the ILS in acute MI, USA; Lisa M. Kath, Associate Professor, San Diego State
care using nursing samples. Numerous studies have sup- University, San Diego, CA, USA; Katherine VanAntwerp,
ported the role of leadership in EBP implementation. DNP Student and Research Assistant, University of
Frontline leadership behaviors of proactivity, knowledge, Michigan, Ann Arbor, MI, USA; Jane Banaszak-Holl,
support, and perseverance are critically relevant to nursing. Professor, Monash University, Melbourne VIC, Australia;
Investigating and improving implementation leadership Marita G. Titler, Professor, University of Michigan, Ann
using the ILS can help nurse clinicians, researchers, and Arbor, MI, USA; Gregory A. Aarons, Professor, University
leaders improve implementation processes to improve de- of California San Diego, La Jolla, CA, USA
livery of evidence-based care and patient outcomes. WVN Address correspondence to Clayton J. Shuman,
University of Michigan, 400 N. Ingalls, Ste. 4162, Ann
Arbor, MI 48109, USA; clayshu@umich.edu
LINKING EVIDENCE TO ACTION
Accepted 20 July 2019
• Frontline manager implementation leadership is a critical © 2019 Sigma Theta Tau International
contextual factor influencing implementation but is often
ignored. There is a critical need for more research on the
influence of frontline nurse managers in acute care. References
Aarons, G. A., Ehrhart, M. G., & Farahnak, L. R. (2014).
• Few tools are available to measure the implementation
The implementation leadership scale (ILS): develop-
leadership behaviors of frontline nurse managers. The ILS ment of a brief measure of unit level implementa-
is a valid and reliable instrument that can be used in fu- tion leadership. Implementation Science, 9(1), https://doi.
ture research to investigate frontline nurse managers’ lead- org/10.1186/1748-5908-9-45.
ership behaviors for EBP implementation in acute care.
Aarons, G. A., Ehrhart, M. G., Farahnak, L. R., & Sklar, M. (2014).
• The ILS is a pragmatic tool that frontline nurse manag- Aligning leadership across systems and organizations to de-
ers can use for self-assessment, as well as for obtaining velop a strategic climate for evidence-based practice imple-
their staff perceptions regarding their leadership be- mentation. Annual Review of Public Health, 35, 255–274.
haviors for EBP implementation. Aarons, G. A., Ehrhart, M. G., Moullin, J. C., Torres, E. M.,
& Green, A. E. (2017). Testing the leadership and organi-
• Interventions to improve implementation leadership zational change for implementation (LOCI) intervention
behaviors for frontline nurse managers are needed. in substance abuse treatment: A cluster randomized trial
The ILS can be used to identify areas needing im- study protocol. Implementation Science, 12, Article 29. https://
provement and inform intervention development and doi.org/10.1186/s13012-017-0562-3
delivery targeting these areas. Aarons, G. A., Ehrhart, M. G., Torres, E. M., Finn, N. K., &
Roesch, S. C. (2016). Validation of the Implementation
Leadership Scale (ILS) in substance use disorder treatment
Author information organizations. Journal of Substance Abuse Treatment, 68, 31–35.
Clayton J. Shuman, Assistant Professor, University of Aarons, G. A., Hurlburt, M., & Horwitz, S. M. (2011).
Michigan, Ann Arbor, MI, USA; Mark G. Ehrhart, Professor, Advancing a conceptual model of evidence-based practice
University of Central Florida, Orlando, FL, USA; Elisa M. implementation in public service sectors. Administration and
Torres, Student and Graduate Research Assistant, George Policy in Mental Health and Mental Health Services Research, 38(1),
Mason University, Fairfax, VA, USA; Philip Veliz, Associate 4–23.
90 Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91.
© 2019 Sigma Theta Tau International
Original Article
Agency for Healthcare Research and Quality (2015). 2014 May, C. R., Johnson, M., & Finch, T. (2016). Implementation,
national healthcare quality and disparities report. Retrieved from context and complexity. Implementation Science, 11(1), Article
https://www.ahrq.gov/research/findings/nhqrdr/nhqdr14/ 141. https://doi.org/10.1186/s13012-016-0506-3
index.html Muthén, L. K., & Muthén, B. (1998–2016). Mplus user’s guide, 7th
American Organization for Nursing Leadership & American ed. Los Angeles, CA: Muthén & Muthén.
Organization of Nurse Executives (2015). AONL nurse man- Rabin, B. A., & Brownson, R. C. (2018). Terminology for dis-
ager competencies. Chicago, IL: AONL, AONE. Retrieved from semination and implementation research. In R. Brownson,
https://www.aonl.org/system/files/media/f ile/2019/06/ G. Colditz, & E. Proctor (Eds.), Dissemination and implementa-
nurse-manager-competencies.pdf tion research in health: Translating science to practice, 2nd ed. (pp.
Augustsson, H., Von Thiele Schwarz, U., Stenfors-Hayes, T., & 19–45). New York, NY: Oxford University Press.
Hasson, H. (2015). Investigating variations in implementa- Reichenpfader, U., Carlfjord, S., & Nilsen, P. (2015). Leadership
tion fidelity of an organizational-level occupational health in evidence-based practice: A systematic review. Leadership in
intervention. International Journal of Behavioral Medicine, 22(3), Health Services, 28, 298–316.
345–355.
Robinson, L. D., Paull, D. E., Mazzia, L. M., Falzetta, L., Hay, J.,
Birken, S., Clary, A., Tabriz, A. A., Turner, K., Meza, R., Zizzi, Neily, J., … Bagian, J. P. (2010). The role of the operating
A., … Charns, M. (2018). Middle managers’ role in imple- room nurse manager in the successful implementation of
menting evidence-based practices in healthcare: A system- preoperative briefings and postoperative debriefings in the
atic review. Implementation Science, 13, Article 149. https://doi. VHA Medical Team Training Program. Journal of PeriAnesthesia
org/10.1186/s13012-018-0843-5 Nursing, 25(5), 302–306.
Brown, R. D., & Hauenstein, N. M. (2005). Interrater agree- Sandström, B., Borglin, G., Nilsson, R., & Willman, A. (2011).
ment reconsidered: An alternative to the rwg indices. Promoting the implementation of evidence-based practice:
Organizational Research Methods, 8(2), 165–184. A literature review focusing on the role of nursing leader-
Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness- ship. Worldviews on Evidence-Based Nursing, 8(4), 212–223.
of-fit indexes for testing measurement invariance. Structural Shuman, C. (2017). Addressing the practice context in evi-
Equation Modeling, 9(2), 233–255. dence-based practice implementation: Leadership and cli-
Dimitrov, D. M. (2010). Testing for factorial invariance in the mate (Doctoral Dissertation). Retrieved from Deep Blue.
context of construct validation. Measurement and Evaluation in http://hdl.handle.net/2027.42/138458
Counseling and Development, 43(2), 121–149. Shuman, C. J., Liu, X., Aebersold, M. L., Tschannen, D.,
Finn, N. K., Torres, E. M., Ehrhart, M. G., Roesch, S. C., & Aarons, Banaszak-Holl, J., & Titler, M. G. (2018). Associations
G. A. (2016). Cross-validation of the Implementation among unit leadership and unit climates for implemen-
Leadership Scale (ILS) in child welfare service organiza- tation in acute care: A cross-sectional study. Implementation
tions. Child Maltreatment, 21(3), 250–255. Science, 13, Article 62.
Gifford, W. A., Squires, J. E., Angus, D. E., Ashley, L. A., Shuman, C. J., Ploutz-Snyder, R. J., & Titler, M. G. (2018).
Brosseau, L., Craik, J. M., … Wallin, L. (2018). Managerial Development and testing of the nurse manager EBP
leadership for research use in nursing and allied health competency scale. Western Journal of Nursing Research, 40(2),
care professions: A systematic review. Implementation Science, 175–190.
13, Article 127. https://doi.org/10.1186/s13012-018-0817-7 Shuman, C. J., Powers, K., Banaszak-Holl, J., & Titler, M. G.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit in- (2019). Unit leadership and climates for evidence-based
dexes in covariance structure analysis: Conventional cri- practice implementation in acute care: A cross-sec-
teria versus new alternatives. Structural Equation Modeling: A tional descriptive study. Journal of Nursing Scholarship, 51(1),
Multidisciplinary Journal, 6(1), 1–55. 114–124.
Institute of Medicine (2001). Crossing the quality chasm: A new Titler, M. G., & Shuman, C. (2017). Implementation Science
health system for the 21st century. Washington, DC: National and Policy. In P. Grady & A. S. Hinshaw (Eds.), Using Nursing
Academies Press. Research to Shape Health Policy (pp. 33–54). New York, NY:
Lewis, C. C., Fischer, S., Weiner, B. J., Stanick, C., Kim, M., Springer Publishing Company.
& Martinez, R. G. (2015). Outcomes for implementation Titler, M. G. (2018). Translation research in practice: An in-
science: An enhanced systematic review of instruments troduction. Online Journal of Issues in Nursing, 23(2). https://doi.
using evidence-based rating criteria. Implementation Science, org/0.3912/OJIN.Vol23No02Man01
10, Article 155. https://doi.org/10.1186/s13012-015-0342-x Torres, E. M., Ehrhart, M. G., Beidas, R. S., Farahnak, L. R.,
Lyon, A. R., Cook, C. R., Brown, E. C., Locke, J., Davis, C., Finn, N. K., & Aarons, G. A. (2018). Validation of the
Ehrhart, M., & Aarons, G. A. (2018). Assessing organiza- Implementation Leadership Scale (ILS) with supervisors’
tional implementation context in the education sector: self-ratings. Community Mental Health Journal, 54(1), 49–53.
Confirmatory factor analysis of measures of implementation
leadership, climate, and citizenship. Implementation Science, 13, 10.1111/wvn.12402
Article 5. https://doi.org/10.1186/s13012-017-0705-6 WVN 2020;17:82–91
Worldviews on Evidence-Based Nursing, 2020; 17:1, 82–91. 91
© 2019 Sigma Theta Tau International
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- National Interest Waiver Software EngineerDocument15 pagesNational Interest Waiver Software EngineerFaha JavedNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Darkle Slideshow by SlidesgoDocument53 pagesDarkle Slideshow by SlidesgoADITI GUPTANo ratings yet
- Drug Calculations WorkbookDocument32 pagesDrug Calculations Workbookvhon100% (1)
- Jake - MH TeamDocument1 pageJake - MH Teamjamie carpioNo ratings yet
- ABCDs During A Code Blue Response in An Adult PatientDocument23 pagesABCDs During A Code Blue Response in An Adult PatientChakra PuspitaNo ratings yet
- Bring Your Gear 2010: Safely, Easily and in StyleDocument76 pagesBring Your Gear 2010: Safely, Easily and in StyleAkoumpakoula TampaoulatoumpaNo ratings yet
- Passage To Abstract Mathematics 1st Edition Watkins Solutions ManualDocument25 pagesPassage To Abstract Mathematics 1st Edition Watkins Solutions ManualMichaelWilliamscnot100% (50)
- Culture and Sensitivity: InhalationDocument3 pagesCulture and Sensitivity: Inhalationjamie carpioNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6jamie carpioNo ratings yet
- MUST Malnutrition Universal Screening Tool PDFDocument6 pagesMUST Malnutrition Universal Screening Tool PDFHoria CostrutNo ratings yet
- Cardiovascular Disorders: Types of DysrythmiasDocument3 pagesCardiovascular Disorders: Types of Dysrythmiasjamie carpioNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4jamie carpioNo ratings yet
- Mari Andrew: Am I There Yet?: The Loop-De-Loop, Zigzagging Journey To AdulthoodDocument4 pagesMari Andrew: Am I There Yet?: The Loop-De-Loop, Zigzagging Journey To Adulthoodjamie carpioNo ratings yet
- Chart 1: The NEWS Scoring System: Physiological Score Parameter 3 2 1 0 1 2 3Document4 pagesChart 1: The NEWS Scoring System: Physiological Score Parameter 3 2 1 0 1 2 3jamie carpio100% (1)
- Abbey Pain Assessment Scale (Follow On Assessment) : Date AND Time Date AND Time Date AND Time Date AND Time Date AND TimeDocument2 pagesAbbey Pain Assessment Scale (Follow On Assessment) : Date AND Time Date AND Time Date AND Time Date AND Time Date AND TimeMuhammad RezgiaNo ratings yet
- Public Health Community Health Nursing: Goal: To Enable EveryDocument10 pagesPublic Health Community Health Nursing: Goal: To Enable Everyjamie carpioNo ratings yet
- Bob Dawson - PhysioDocument1 pageBob Dawson - Physiojamie carpioNo ratings yet
- RowariwudujiladekodazelaDocument3 pagesRowariwudujiladekodazelajamie carpioNo ratings yet
- Writing-General-Information-Tasks (Dragged)Document2 pagesWriting-General-Information-Tasks (Dragged)jamie carpioNo ratings yet
- Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis GDocument9 pagesHepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis Gjamie carpioNo ratings yet
- The ABCDE ApproachDocument8 pagesThe ABCDE ApproachAsmaa TahaNo ratings yet
- Jake PetersonDocument1 pageJake Petersonjamie carpioNo ratings yet
- Code MNGTDocument3 pagesCode MNGTjamie carpioNo ratings yet
- Nusing NCP Blood Transfusion NCP: Total Parenteral NutriDocument2 pagesNusing NCP Blood Transfusion NCP: Total Parenteral Nutrijamie carpioNo ratings yet
- OET Letter FormatDocument8 pagesOET Letter FormatHeba Zaher100% (4)
- Artery Bypass GraftDocument3 pagesArtery Bypass GraftJasmine ChuaNo ratings yet
- Paid Maternity Leave Claiming Personal Exemptions National Immunization DayDocument2 pagesPaid Maternity Leave Claiming Personal Exemptions National Immunization Dayjamie carpioNo ratings yet
- MS TopicsDocument1 pageMS Topicsjamie carpioNo ratings yet
- OBSTETRICSDocument4 pagesOBSTETRICSjamie carpioNo ratings yet
- Rapid Rehabilitation Nursing in Postoperative Patients With Colorectal Cancer and Quality of LifeDocument8 pagesRapid Rehabilitation Nursing in Postoperative Patients With Colorectal Cancer and Quality of Lifejamie carpioNo ratings yet
- CONCEPTSDocument1 pageCONCEPTSjamie carpioNo ratings yet
- POSITIONSDocument1 pagePOSITIONSjamie carpioNo ratings yet
- Ra 07305 FVR PDFDocument11 pagesRa 07305 FVR PDFjamie carpioNo ratings yet
- AMS ANALITICA-AIRFLOW TSP-HVS BrochureDocument1 pageAMS ANALITICA-AIRFLOW TSP-HVS BrochureShady HellaNo ratings yet
- Test On Real NumberaDocument1 pageTest On Real Numberaer.manalirathiNo ratings yet
- Rsi r2 Super Rsi FaqDocument14 pagesRsi r2 Super Rsi FaqChandrasekar Chandramohan100% (1)
- 53 English Work Book XDocument292 pages53 English Work Book XArun DhawanNo ratings yet
- Digital Systems Project: IITB CPUDocument7 pagesDigital Systems Project: IITB CPUAnoushka DeyNo ratings yet
- Arudha PDFDocument17 pagesArudha PDFRakesh Singh100% (1)
- FT2020Document7 pagesFT2020Sam SparksNo ratings yet
- Pyramid Type Plate Bending MachineDocument10 pagesPyramid Type Plate Bending MachineAswin JosephNo ratings yet
- AYUMJADocument1 pageAYUMJASoumet Das SoumetNo ratings yet
- Keeping Track of Your Time: Keep Track Challenge Welcome GuideDocument1 pageKeeping Track of Your Time: Keep Track Challenge Welcome GuideRizky NurdiansyahNo ratings yet
- AP8 Q4 Ip9 V.02Document7 pagesAP8 Q4 Ip9 V.02nikka suitadoNo ratings yet
- Man Bni PNT XXX 105 Z015 I17 Dok 886160 03 000Document36 pagesMan Bni PNT XXX 105 Z015 I17 Dok 886160 03 000Eozz JaorNo ratings yet
- Functions of Theory in ResearchDocument2 pagesFunctions of Theory in ResearchJomariMolejonNo ratings yet
- Michael Clapis Cylinder BlocksDocument5 pagesMichael Clapis Cylinder Blocksapi-734979884No ratings yet
- Service Quality Dimensions of A Philippine State UDocument10 pagesService Quality Dimensions of A Philippine State UVilma SottoNo ratings yet
- LC For Akij Biax Films Limited: CO2012102 0 December 22, 2020Document2 pagesLC For Akij Biax Films Limited: CO2012102 0 December 22, 2020Mahadi Hassan ShemulNo ratings yet
- Building Material Supplier in GurgaonDocument12 pagesBuilding Material Supplier in GurgaonRodidustNo ratings yet
- Vetoset CA541: Thickbed Cementitious Tile AdhesiveDocument2 pagesVetoset CA541: Thickbed Cementitious Tile Adhesivemus3b1985No ratings yet
- Topic: Grammatical Issues: What Are Parts of Speech?Document122 pagesTopic: Grammatical Issues: What Are Parts of Speech?AK AKASHNo ratings yet
- The Essence of Technology Is by No Means Anything TechnologicalDocument22 pagesThe Essence of Technology Is by No Means Anything TechnologicalJerstine Airah SumadsadNo ratings yet
- Topic One ProcurementDocument35 pagesTopic One ProcurementSaid Sabri KibwanaNo ratings yet
- SDS ERSA Rev 0Document156 pagesSDS ERSA Rev 0EdgarVelosoCastroNo ratings yet
- Load Chart Crane LiftingDocument25 pagesLoad Chart Crane LiftingLauren'sclub EnglishBimbel Sd-sma100% (1)
- solidworks ขั้นพื้นฐานDocument74 pagessolidworks ขั้นพื้นฐานChonTicha'No ratings yet
- TIA Guidelines SingaporeDocument24 pagesTIA Guidelines SingaporeTahmidSaanidNo ratings yet
- Aditya Academy Syllabus-II 2020Document7 pagesAditya Academy Syllabus-II 2020Tarun MajumdarNo ratings yet