Professional Documents
Culture Documents
04 Enteral Feeding PDF
04 Enteral Feeding PDF
Uploaded by
ckeshavaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
04 Enteral Feeding PDF
04 Enteral Feeding PDF
Uploaded by
ckeshavaCopyright:
Available Formats
Program Anestesiologi & Cawangan Kualiti Penjagaan Kesihatan BPP, KKM
ICU Management Protocol No. 4
ENTERAL FEEDING
General Points
1. All ventilated patients must receive a nasogastric or orogastric tube. It is
preferable to use 12FG in adults. The correct position of the tube should
be confirmed by 2 out of the following 3 criteria. The criteria are
(i) injecting 10-20 ml of air down the tube and auscultating the epigastric
area (ii) use of litmus paper and (iii) radiography.
2. Early enteral feeding should be commenced within 24-48 hours after
ICU admission whenever the gastrointestinal tract is deemed to be
functioning. This applies to all mechanically ventilated patients who
have been adequately resuscitated and haemodynamically stable.
3. Enteral feeding for patients who have undergone recent abdominal and
bowel surgeries may require prior discussion with the surgeon and ICU
specialist before commencement.
4. Patients should preferably receive feeding continuously during the acute
phase. They can be switched to intermittent bolus technique later.
(i) Continuous feeding
Start at 20-40ml/hr continuously. Aspirate the feeding tube every 4
hours.
(a) If aspirate < 200ml, return all aspirate. Increase rate by 20ml/hr every
3 cycles till a flow rate that meets the caloric needs of the patient. Once
target caloric needs are met, the feeds may be further diluted with water
to meet the fluid requirements of the patient.
(b) If aspirate >200ml, return 200ml aspirate to patient and reduce rate
by 50% of initial rate. Exclude bowel obstruction first. If there is no
clinical evidence of bowel obstruction, administer prokinetic agents (see
11). Once further aspirates are < 200ml, follow (i-a). If aspirates continue
to exceed 200 ml after the above has been carried out, consider the use of
small bowel feeding (see 10) and elemental formulas (see 9).
(ii) Intermittent bolus feeding
Start with 50ml every 3 hours. Aspirate before every feed.
(a) If aspirate < 200ml return aspirate to patient. Increase by 50ml after
every 4 feeds. Increase by 100 ml/feed every 24 hr till caloric needs are
met. Once target caloric needs are met, the feeds may be further diluted
with water to meet the fluid requirements of the patient.
NAICU/ Management Protocol/ Enteral Feeding /August 2006 1
Program Anestesiologi & Cawangan Kualiti Penjagaan Kesihatan BPP, KKM
(b) If aspirate >200ml, return 200ml aspirate to patient and reduce by
50ml per feed. Exclude bowel obstruction first. If there is no clinical
evidence of bowel obstruction, administer prokinetic agents (see 11).
Once further aspirates are < 200ml, follow (ii-a). If aspirates continue to
exceed 200 ml after the above has been carried out, consider the use of
continuous feeding (see 4).
5. Where feasible, enteral feeds can be administered via the closed system.
Closed system refers to the “ready to hang formulas”. Once connected
the duration of feeding is 24 hrs. During initiation of feeding, use the
open system (to reduce wastage) and where feasible, use the closed
system once target feeding has been achieved.
6. All patients receiving feeding must be placed in the semi-recumbent
position with the head of the bed elevated to 45 0. Head injured patients
will have head elevated to 30 0. Patients who have to be prone should be
in the anti-trendelenberg position (10-20 0)
7. Current recommendations suggest a target energy intake of 25
kcal/kg/day and at least 1.2-1.5 g/kg/day of protein.
For obese patients, use 120% of ideal body weight (IBW) or (Actual Body
Weight - IBW) X 0.25 + IBW.
For underweight patients, use actual body weight.
Energy intake should be adjusted according to the severity and type of
illness. Feeding should be administered via a stepwise gradual
introduction of feeds over first 48 hrs. Avoid overfeeding.
8. Use polymeric formulas (whole protein formula) for feeding.
9. Peptide based or elemental formulas (eg Peptamen, Alitrac) have been
shown to be useful in patients with gastrointestinal complications (short
bowel syndrome, pancreatitis). However, there is insufficient evidence
to demonstrate any favourable treatment effects.
10. Small bowel feeding (nasojejunal/nasoduodenal) can be considered for
patients who are intolerant to enteral feeding (high inotropic support,
continuous infusion of sedatives, or paralytic agents or with high gastric
residual volumes) or in pancreatitis
11. Motility agents such as IV metochlopramide 10-20mg 6-8 hourly and/or
IV erythromycin 125 mg QID or 250 mg BID to be used in patients who
experience feed intolerance (high gastric residuals, emesis).
12. Nutrient mixtures prepared in the kitchen (“blenderised diet”) should
not be used as this type of feed is unbalanced, causes feeding tube
occlusion and diarrhea secondary to bacterial contamination.
NAICU/ Management Protocol/ Enteral Feeding /August 2006 2
Program Anestesiologi & Cawangan Kualiti Penjagaan Kesihatan BPP, KKM
Types of enteral feeds
Type Energy Indications ** Suggested
maximum
volume/day
Polymeric
-Ensure 1kcal/ml Most patients 60-80 ml/hr
-Enercal or
-Isocal 200-250 ml 3 hourly
-Nutren
-Diabetic patients 60-80 ml/hr
-Glucerna 1kcal/ml -Stress induced or
-Nutren diabetic hyperglycemia 200-250 ml 3 hourly
Fiber-enriched -Patient who develop 60-80 ml/hr
-Jevity 1 kcal/ml diarrhea to non-fiber or
-Nutren fiber containing feeds 200-250 ml 3 hourly
Disease specific 2 kcal/ml -Renal failure with fluid 30-40 ml/hr
-Nepro restriction and on or
dialysis 100-120 ml 3 hourly
Disease specific 2 kcal/ml -Renal failure with fluid, 30-40 ml/hr
-Suplena protein, electrolytes or
restriction and not on 100-120 ml 3 hourly
dialysis
Disease specific 1.5 kcal/ml -Patients with 50-60 ml /hr
-Pulmocare hypercapnia (eg COAD) or
150-200 ml 3 hourly
Elemental 1 kcal/ml -Patients with
-Peptamen gastrointestinal 60-80 ml/hr
-Alitrac problems (pancreatitis,
short bowel syndrome)
** Please note that the suggested maximum volume is not restricted to the
examples given. It is important that the target caloric needs are eventually met
in whatever volume that is delivered to the patient. If the patient has increased
fluid requirements, supplemental fluids may be given as diluted feeds (the
maximum flow rates can be increased) or given intravenously.
References
1. Heyland DK J PEN 2003;27:355-373
2. Bongers T, Griffiths RD Crit Care Med 2006;12:131-135
3. Simpson F, Doig GS Inten Care Med 2005;31:12-23
4. McClave SA et al Crit Care Med 2005;33:324-330
5. Artinian et al Chest 2006;129(4):960-967
NAICU/ Management Protocol/ Enteral Feeding /August 2006 3
Program Anestesiologi & Cawangan Kualiti Penjagaan Kesihatan BPP, KKM
ALGORITHM FOR ENTERAL FEEDING (CONTINOUS METHOD)
ICU ADMISSION
No
Functioning GI tract
Consider PN
Yes
Start enteral feeding at 20-
40 ml/hr
Aspirate 4 hourly
Yes
-Return 200mls aspirate to
Aspirate > 200ml patient
-Exclude bowel obstruction
-Administer prokinetic agents
-Reduce rate by 50%
No
-Return aspirate to patient -Consider small bowel feeding
-Increase by 20ml/hr after 3 -Consider elemental feeds
cycles -Consider supplemental PN
Aspirate every 4 hours
Increase rate to whatever
volume as long as target
caloric needs are met
eg 60-80ml/hr
NAICU/ Management Protocol/ Enteral Feeding /August 2006 4
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Multiple Sclerosis Nursing Care PlanDocument4 pagesMultiple Sclerosis Nursing Care PlanCHRISTIE MONTANONo ratings yet
- Ch01 Medical Surgical NursingDocument8 pagesCh01 Medical Surgical Nursingmicky1121100% (1)
- Nursing Care Plan Case PreDocument3 pagesNursing Care Plan Case PreKhatzky MeiNo ratings yet
- Estradiol 10mcg (Vagifen)Document13 pagesEstradiol 10mcg (Vagifen)asdwasdNo ratings yet
- Speech Text - Mental HealthDocument2 pagesSpeech Text - Mental Healthjohnny suhNo ratings yet
- Living WillDocument3 pagesLiving WillBalkiss TouzriNo ratings yet
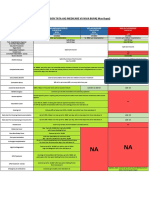
- Comparison Tata Aig Medicare Vs Niva BupaDocument1 pageComparison Tata Aig Medicare Vs Niva BupaTikekar ShubhamNo ratings yet
- 5 PPT Tle 7 Week 5Document51 pages5 PPT Tle 7 Week 5jerico juarezNo ratings yet
- Covid 19Document31 pagesCovid 19Lee BuelaNo ratings yet
- Learner's Activity Sheet: MAPEH Physical Education (Quarter I - Week 1)Document4 pagesLearner's Activity Sheet: MAPEH Physical Education (Quarter I - Week 1)She Ena Man UelNo ratings yet
- Punjab Healthcare Commission: CG-09RM-Ed2Document168 pagesPunjab Healthcare Commission: CG-09RM-Ed2saimaNo ratings yet
- What Can We Eat After Tooth ExtractionDocument4 pagesWhat Can We Eat After Tooth Extractionkings furyNo ratings yet
- Referat Rontgen Thorax Dan KelainannyaDocument31 pagesReferat Rontgen Thorax Dan KelainannyawindarhyngtysNo ratings yet
- EMJ EthicsReviewAAU AdamuDocument9 pagesEMJ EthicsReviewAAU AdamuJateni joteNo ratings yet
- Benign Paroxysmal Positional Vertigo (BPPV) - A Simple SolutionDocument5 pagesBenign Paroxysmal Positional Vertigo (BPPV) - A Simple SolutionagniosaiNo ratings yet
- PreeclampsiaDocument13 pagesPreeclampsiaAnamikaNo ratings yet
- Intake Form: Health Declaration For TravellersDocument1 pageIntake Form: Health Declaration For TravellersHekiXamNo ratings yet
- Chapter 01: Drug Regulation, Actions, and Responses Workman & Lacharity: Understanding Pharmacology: Essentials For Medication Safety, 2Nd EditionDocument13 pagesChapter 01: Drug Regulation, Actions, and Responses Workman & Lacharity: Understanding Pharmacology: Essentials For Medication Safety, 2Nd Editionleo chenNo ratings yet
- BHW Pocket HandbookDocument70 pagesBHW Pocket HandbookGa B B Orlongan100% (9)
- Form F Tule DOWNSDocument2 pagesForm F Tule DOWNSAnand ChineyNo ratings yet
- Chapter 5 Challenge Solution: Project Management FoundationsDocument2 pagesChapter 5 Challenge Solution: Project Management FoundationspraveenNo ratings yet
- Mini-PAT Paper Form - Updated June 18Document2 pagesMini-PAT Paper Form - Updated June 18Benjamin NgNo ratings yet
- Viral ShahDocument2 pagesViral ShahAkshay ShahNo ratings yet
- Research India - Google ScholarDocument1 pageResearch India - Google Scholarritesh jadhavNo ratings yet
- Dehydration in ChildrenDocument24 pagesDehydration in ChildrenDani AsmareNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanJoyce AnglubenNo ratings yet
- San Cristobal Elementary School School Clinic LogbookDocument3 pagesSan Cristobal Elementary School School Clinic LogbookLhenzky BernarteNo ratings yet
- 100 Item Exam On Fundamentals of Nursing - Pulse - Blood Pressure PDFDocument12 pages100 Item Exam On Fundamentals of Nursing - Pulse - Blood Pressure PDFJawad AkbarNo ratings yet
- NCPDocument4 pagesNCPDivine TejadaNo ratings yet
- Varicose VeinsDocument25 pagesVaricose VeinsByancaPredescu50% (2)