Professional Documents
Culture Documents
Pityriasis Rosea - StatPearls - NCBI Bookshelf PDF
Pityriasis Rosea - StatPearls - NCBI Bookshelf PDF
Uploaded by
Endah SOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pityriasis Rosea - StatPearls - NCBI Bookshelf PDF
Pityriasis Rosea - StatPearls - NCBI Bookshelf PDF
Uploaded by
Endah SCopyright:
Available Formats
Pityriasis Rosea
Litchman G, Nair PA, Le JK.
Introduction
Pityriasis rosea is an acute self-limiting papulosquamous disorder. It is characterized by a herald patch followed by scaly oval
patches on the trunk and proximal extremities in a "Christmas-tree" appearance. Pityriasis rosea means rose-colored scale.
Pityriasis rosea is also known as pityriasis circinata, roseola annulata, and herpes tonsurans maculosus. The skin eruption
usually lasts 6-8 weeks and begins with a 'herald patch.' [1][2][3]
Etiology
The exact cause of pityriasis rosea is not known, but features like seasonal variation and clustering in communities suggest
that it is an infectious disease. Infections like viruses, bacteria, spirochetes, and noninfective causes like atopy and
autoimmunity are known causes. Upper respiratory tract infections that precede pityriasis rosea suggest a role of
Streptococcus. Recently, reactivation of latent human herpesvirus-6 and human herpesvirus-7 infection have been found as the
possible etiologic agents. Pityriasis rosea-like eruptions have been reported after vaccinations such as Bacillus Calmette-
Guerin, influenza, H1N1, diphtheria, smallpox, hepatitis B, and Pneumococcus. Eruptions have also been seen with drugs like
gold, captopril, barbiturates, D-penicillamine, and clonidine. In temperate regions, it is more common in the winter season,
while in tropical areas some seasonal variation is noted.[4][5][6]
Epidemiology
The approximate incidence of pityriasis rosea is 0.5% to 2%. It affects people of both genders between 15 and 30 years of age,
but it also affects older adults and children.[7]
Pathophysiology
A lack of natural killer (NK) cell and B-cell activity in pityriasis rosea lesions has been noted, suggesting a predominantly T-
cell mediated immunity. Increased amounts of CD4 T-cells and Langerhans cells are present in the dermis, possibly reflecting
viral antigen processing and presentation. Anti-immunoglobulin M (IgM) keratinocytes have been found in patients with
pityriasis rosea. This may be associated with the exanthem phase of viral infection.
Histopathology
Skin biopsy is not necessary but if performed will reveal non-specific features similar to those seen in chronic dermatitis.
History and Physical
Pityriasis rosea is clinically characterized by a herald patch or mother patch followed by scaly oval plaques on the trunk and
proximal extremities along the Langer’s lines of cleavage giving characteristic “Christmas-tree" appearance. Collarette scaling
is common. The eruption is usually preceded by a prodrome of a sore throat, gastrointestinal disturbance, fever, and arthralgia.
Pruritus is severe in 25% of cases. Herald patch is seen in 50% to 90% cases and is located on the trunk followed by the neck
or proximal extremity.
A generalized eruption then occurs, in which numerous lesions develop in crops over a period of one to two weeks after the
onset of the herald patch. The eruptions are symmetric and most commonly involve the thorax, back, abdomen, and adjoining
areas of the neck and extremities. These secondary lesions occur as macules and papules that are elliptical or ovular in shape.
https://www.ncbi.nlm.nih.gov/books/NBK448091/ 01/03/20 13.46
Halaman 1 dari 4
Fine scaling and central wrinkling, with a cigarette paper aspect, are seen. A characteristic feature is the collarette appearance
of the scale, with edges peripherally attached and lifted up near the center of the lesion. The distribution of the lesions is
usually bilateral and diffuse, with the long axis running parallel to skin tension lines.
The incidence of atypical pityriasis rosea is 20% which maybe regard morphology, size, distribution, course, or symptoms.
The various atypical morphologies include:
Vesicular Pityriasis Rosea presents as a generalized eruption of 2 mm to 6 mm vesicles or as a rosette of vesicles
mainly over the head, palms, and soles. It needs to be differentiated from varicella and dyshidrosis. It is commonly
seen in children.
Purpuric (hemorrhagic) Pityriasis Rosea presents as macular purpura on skin or oral mucosa.
Urticarial Pityriasis Rosea
Generalized Papular Pityriasis Rosea is rare and is seen in young children, pregnant women, and African Caribbeans.
It presents as multiple papules which occur along with classic patches and plaques.
Lichenoid Pityriasis Rosea is observed in the course of atypical Pityriasis Rosea, but it is more commonly caused by
drugs such as gold, captopril, barbiturates, D-penicillamine, and clonidine.
Erythema multiforme-like Pityriasis Rosea: It presents with targetoid lesions along with the classical lesions of
pityriasis rosea. Histopathologically, erythema multiform and pityriasis rosea may show similar features except
satellite cell necrosis which is a distinguishing feature seen only in erythema multiform where lymphocytes are seen
attached to scattered necrotic keratinocytes.
Follicular Pityriasis Rosea: The secondary lesions are typically follicular and present discrete or in groups associated
classical lesions.Differential diagnoses includes follicular lichen planus and keratosis pilaris ad atopic dermatitis with
a follicular element.
Giant Pityriasis Rosea is rarely reported and was named after Darier. It consists of plaques and circles of very large
size ranging from 5 cm to 7 cm with individual lesions reaching the size of the palm of the patient.
Pityriasis Rosea presenting as exfoliative dermatitis
Pityriasis Rosea with atypical herald patch may be absent in 20% of patients or present with secondary eruptions or
occur at unusual sites such as the face, scalp, genitalia, or other sites.
Inverse Pityriasis Rosea: Lesions are predominantly present in acral and flexural areas involving axilla, groin, and
face.
Acral Pityriasis Rosea: Lesions are more concentrated over acral parts of body ie palms and soles, where EM,
syphilis, necrolytic acral erythema, and drug eruptions should be kept as differentials.
Unilateral Pityriasis Rosea is a rare variant that can be seen in both children and adults, and the lesions are located on
one side of the body. The patient has a herald patch with classical secondary lesions.
Blaschkoid Pityriasis Rosea: Lesions of Pityriasis Rose follows the lines of Blaschko.
Limb-Girdle Pityriasis Rosea: Also known as Pityriasis Rosea of Vidal where eruptions are limited to shoulders or
pelvic girdle, thus involving axilla and groin. Lesions are usually larger and more annular.
Mucosal involvement in pityriasis rosea is seen in 16% of patients affecting oral mucosa, with punctuate, erosive,
bullous, hemorrhages, ulcers (with or without raised borders), petechiae, papulovesicular, bullae, and erythematous
plaques.
Localized pityriasis rosea: Eruptions are localized to one part of the body.
The rashes of pityriasis rosea usually last for five weeks and resolve by 8 weeks in more than 80% of patients. Pityriasis rosea
needs to be differentiated from secondary syphilis, dermatophytosis, guttate psoriasis, nummular eczema, pityriasis lichenoid
chronic, cutaneous T-cell lymphoma, erythema annular centrifugal and erythema chronic migrans.
Evaluation
https://www.ncbi.nlm.nih.gov/books/NBK448091/ 01/03/20 13.46
Halaman 2 dari 4
Dermatoscopy helps to differentiate pityriasis rosea from other conditions. It shows a yellowish background color, peripheral
arrangement of the scales, and patchy distribution of loosely arranged dotted vessels.
Histopathology shows superficial perivascular dermatitis. Focal parakeratosis in mounds, hyperplasia, and focal spongiosis are
observed in the epidermis. The epidermis may show exocytosis of lymphocytes, variable spongiosis, mild acanthosis, and a
thinned granular layer. Extravasated red blood cells along with a perivascular infiltrate of lymphocytes, histiocytes, and
eosinophils are seen in the dermis.[2][8][9]
Treatment / Management
Pityriasis rosea is a self-limiting, exanthematous disease. Most patients need emollients, antihistaminics, and topical steroids.
Macrolides and acyclovir lead to faster resolution of lesions and help to relieve pruritus. Narrowband ultraviolet B therapy is
also used. It works by altering the immunology in the skin.[10]
Pearls and Other Issues
Atopy is associated with pityriasis rosea. Pityriasis rosea during pregnancy, within the first 15 weeks of gestation, may cause
premature delivery and fetal demise.
Enhancing Healthcare Team Outcomes
In the majority of patients, pityriasis is a self-limited condition with an excellent prognosis. However, about 2-3% of patients
will experience a recurrence. The skin disorder is benign, non-contagious and does not require any special precautions. Since
the majority of patients first present to their primary care provider when the skin lesions appear, it is important for the nurse,
pharmacist and primary care provider to educate the patient that the condition is benign and will not last for more than 2
months. For cases that are severe, a dermatology referral should be made. The biggest morbidity is due to pigmentation
changes, especially in dark-skinned individuals. However, scarring does not occur. There are reports that pityriasis during
pregnancy may be associated with premature birth- but it is not known if this is just a coincidental observation. Patients
should be told to avoid applying irritants to the skin and avoid tanning. The itching is mild and usually resolves with a
moisturizer. Exposure to the sun may induce pigmentary changes and should be avoided. [11][12] (Level V)
Questions
To access free multiple choice questions on this topic, click here.
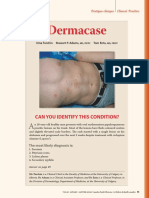
Figure
Pityriasis Rosea. Contributed by DermNetNZ
References
1. Drago F, Ciccarese G, Parodi A. Pityriasis rosea and pityriasis rosea-like eruptions: How to distinguish them? JAAD Case
Rep. 2018 Sep;4(8):800-801. [PMC free article: PMC6142012] [PubMed: 30246131]
2. Trayes KP, Savage K, Studdiford JS. Annular Lesions: Diagnosis and Treatment. Am Fam Physician. 2018 Sep
01;98(5):283-291. [PubMed: 30216021]
3. Chang HC, Sung CW, Lin MH. The efficacy of oral acyclovir during early course of pityriasis rosea: a systematic review
and meta-analysis. J Dermatolog Treat. 2019 May;30(3):288-293. [PubMed: 30109959]
https://www.ncbi.nlm.nih.gov/books/NBK448091/ 01/03/20 13.46
Halaman 3 dari 4
4. Gay JT, Gross GP. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 6, 2019. Herald Patch.
[PubMed: 30020673]
5. Engelmann I, Ogiez J, Ogiez L, Alidjinou EK, Lazrek M, Dewilde A, Hober D. Relapsing Pityriasis Rosea With HHV-7
Reactivation in an 11-Year-Old Girl. Pediatrics. 2018 May;141(5) [PubMed: 29674359]
6. Alame MM, Chamsy DJ, Zaraket H. Pityriasis rosea-like eruption associated with ondansetron use in pregnancy. Br J Clin
Pharmacol. 2018 May;84(5):1077-1080. [PMC free article: PMC5903224] [PubMed: 29520857]
7. VanRavenstein K, Edlund BJ. Diagnosis and management of pityriasis rosea. Nurse Pract. 2017 Jan 20;42(1):8-11.
[PubMed: 28002142]
8. Rodriguez-Zuniga M, Torres N, Garcia-Perdomo H. Effectiveness of acyclovir in the treatment of pityriasis rosea. A
systematic review and meta-analysis. An Bras Dermatol. 2018 Sep-Oct;93(5):686-695. [PMC free article: PMC6106661]
[PubMed: 30156618]
9. Sonthalia S, Kumar A, Zawar V, Priya A, Yadav P, Srivastava S, Gupta A. Double-blind randomized placebo-controlled
trial to evaluate the efficacy and safety of short-course low-dose oral prednisolone in pityriasis rosea. J Dermatolog Treat.
2018 Sep;29(6):617-622. [PubMed: 29363373]
10. Krishnamurthy K, Walker A, Gropper CA, Hoffman C. To treat or not to treat? Management of guttate psoriasis and
pityriasis rosea in patients with evidence of group A Streptococcal infection. J Drugs Dermatol. 2010 Mar;9(3):241-50.
[PubMed: 20232586]
11. Cook B, Crutchfield CE. Pityriasis rosea. Dermatol Nurs. 2006 Aug;18(4):370. [PubMed: 16948385]
12. Black JB, Pellett PE. Human herpesvirus 7. Rev. Med. Virol. 1999 Oct-Dec;9(4):245-62. [PubMed: 10578120]
Publication Details
Author Information
Authors
Graham Litchman; Pragya A. Nair; Jacqueline K. Le1.
A!liations
1 Desert Regional Medical Center
Publication History
Last Update: June 10, 2019.
Copyright
Copyright © 2020, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/),
which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
Publisher
StatPearls Publishing, Treasure Island (FL)
NLM Citation
Litchman G, Nair PA, Le JK. Pityriasis Rosea. [Updated 2019 Jun 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
https://www.ncbi.nlm.nih.gov/books/NBK448091/ 01/03/20 13.46
Halaman 4 dari 4
You might also like
- Anatomy and Physiology 9th Edition Patton Solutions Manual Full Chapter PDFDocument7 pagesAnatomy and Physiology 9th Edition Patton Solutions Manual Full Chapter PDFserenafinnodx100% (13)
- Speaker NotesDocument21 pagesSpeaker Noteschinnupepsi4allNo ratings yet
- Determination of Sun Protection Factor by Uvvis Spectrophotometry - hccr.1000108Document4 pagesDetermination of Sun Protection Factor by Uvvis Spectrophotometry - hccr.1000108rnd labNo ratings yet
- Ptyriasis Rosea: Clinical FeaturesDocument3 pagesPtyriasis Rosea: Clinical FeaturesRizky FajriNo ratings yet
- Chapter 11 Pityriasis Rosea, Pityriasis Rubra Pilaris, and Other Papulosquamous and Hyperkeratotic DiseasesDocument10 pagesChapter 11 Pityriasis Rosea, Pityriasis Rubra Pilaris, and Other Papulosquamous and Hyperkeratotic DiseasesErika KusumawatiNo ratings yet
- Pomfoliks JurnalDocument4 pagesPomfoliks JurnalTri RatnawatiNo ratings yet
- Fungal Infections-MlcDocument31 pagesFungal Infections-Mlcsamuel gathenyaNo ratings yet
- Dermacase. Pityriasis Rosea.Document3 pagesDermacase. Pityriasis Rosea.Brenda Ruth PanjaitanNo ratings yet
- Psoriasis - StatPearls - NCBI BookshelfDocument8 pagesPsoriasis - StatPearls - NCBI BookshelfMehmet TaşçıNo ratings yet
- Pediatric Tinea Versicolor: BackgroundDocument16 pagesPediatric Tinea Versicolor: BackgroundlolNo ratings yet
- Physical Trauma (Koebner's Phenomenon) Is A Major Factor in Eliciting LesionsDocument12 pagesPhysical Trauma (Koebner's Phenomenon) Is A Major Factor in Eliciting LesionsNaomi AnastacioNo ratings yet
- Mikimos,+09 +lisi 56 60Document5 pagesMikimos,+09 +lisi 56 60MaylafaizaNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document3 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Santomi PratamaNo ratings yet
- XXXXXX 121Document16 pagesXXXXXX 121AndriantkNo ratings yet
- Pityriasis RoseaDocument29 pagesPityriasis RoseaAsressieNo ratings yet
- Superficial Mycoses 3Document8 pagesSuperficial Mycoses 3Mohammad KaifNo ratings yet
- Handbook of Skin DiseasesDocument43 pagesHandbook of Skin DiseasesTrixDelaCruzNo ratings yet
- Pityriasis RoseaDocument13 pagesPityriasis Roseagagauzne196950% (2)
- Localized Pityriasis RoseaDocument4 pagesLocalized Pityriasis RoseaFenni OktoberryNo ratings yet
- Seborrheic DermatitisDocument34 pagesSeborrheic DermatitisRizky Takdir RamadhanNo ratings yet
- Tinea Kruris BahanDocument11 pagesTinea Kruris BahanFebridayanti Nur FitriannisaNo ratings yet
- Primary SyphilisDocument6 pagesPrimary Syphilisnicolas joshuNo ratings yet
- Superficial Mycoses Group 4Document38 pagesSuperficial Mycoses Group 4prudence azenaborNo ratings yet
- Annular LesionsDocument8 pagesAnnular LesionshpmcentreNo ratings yet
- Pityriasis Rosea - Background, Pathophysiology, EtiologyDocument4 pagesPityriasis Rosea - Background, Pathophysiology, EtiologysyahrulroziNo ratings yet
- Referat Kulit KakayDocument26 pagesReferat Kulit KakayRezky Dwiputra FellanysNo ratings yet
- Verruga Peruana - Bartonellosis: VisitDocument2 pagesVerruga Peruana - Bartonellosis: VisitErika Pilco GuerraNo ratings yet
- Pics MCQSDocument22 pagesPics MCQStania100% (1)
- Fungal InfectionsDocument29 pagesFungal InfectionsKaran MassNo ratings yet
- Meth Elab Topic N2Document19 pagesMeth Elab Topic N2Group M1869No ratings yet
- Fungus IdDocument6 pagesFungus Idmajid4uonlyNo ratings yet
- DR - Ali's Uworld Notes For Step 2 CKDocument19 pagesDR - Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- The Diagnosis and Management of Tinea CapitisDocument4 pagesThe Diagnosis and Management of Tinea CapitisKeyla Kehara PutriNo ratings yet
- PITYRIASIS ROSEA eisman2015-DIPLOMADO DERMATOLOGIA CLINICA 2023Document6 pagesPITYRIASIS ROSEA eisman2015-DIPLOMADO DERMATOLOGIA CLINICA 2023taniasolisNo ratings yet
- ROSACEADocument19 pagesROSACEAAs Syarif50% (2)
- Rosacea SystemicDocument7 pagesRosacea SystemicSalud Los UribeNo ratings yet
- Papular UrticariaDocument10 pagesPapular UrticariaNuri Sakina SuhartoNo ratings yet
- Dermatology OSCE Pictures 1Document208 pagesDermatology OSCE Pictures 1medt80No ratings yet
- Tinea Versicolor (Pityriasis Versicolor) - UpToDateDocument47 pagesTinea Versicolor (Pityriasis Versicolor) - UpToDatejotaere RobNo ratings yet
- PsoriasisDocument40 pagesPsoriasisAmrit Preet KaurNo ratings yet
- Defi Nition and NomenclatureDocument4 pagesDefi Nition and NomenclatureintanphNo ratings yet
- Lecture 3Document25 pagesLecture 3Sucdi CabdiNo ratings yet
- 17.pityriasis RoseaDocument5 pages17.pityriasis RoseahaidarTRVNo ratings yet
- 10 1016@j Clindermatol 2019 01 007 PDFDocument10 pages10 1016@j Clindermatol 2019 01 007 PDFMira GNo ratings yet
- Int. Medicine: Batch 2014-College of MedicineDocument14 pagesInt. Medicine: Batch 2014-College of MedicineGabriel Gerardo N. CortezNo ratings yet
- Pityrosporum FolliculitisDocument6 pagesPityrosporum FolliculitisAndy Sugiharto WonodiharjoNo ratings yet
- Epidemiology: FilariasisDocument10 pagesEpidemiology: Filariasisketty putriNo ratings yet
- A. Psoriasis Affects 2% Population. B. Oral Involvement Is Uncommon. C. Ultraviolet Exposure (Phototherapy) Is TherapeuticDocument3 pagesA. Psoriasis Affects 2% Population. B. Oral Involvement Is Uncommon. C. Ultraviolet Exposure (Phototherapy) Is Therapeuticrvar839No ratings yet
- Hydradinitis SupparativaDocument46 pagesHydradinitis SupparativaSaqib SaeedNo ratings yet
- Kawasaki Disease What Is Kawasaki Disease?Document6 pagesKawasaki Disease What Is Kawasaki Disease?Arafat Masud NiloyNo ratings yet
- Genodermatosis: The IchthyosisDocument4 pagesGenodermatosis: The IchthyosisOman ArifNo ratings yet
- Fungal InfectionsDocument9 pagesFungal InfectionsCoral Srinivasa RamaluNo ratings yet
- Pityriasis RoseaDocument20 pagesPityriasis RoseaMendy Herianto100% (1)
- 2.papulosquamous DiseasesDocument65 pages2.papulosquamous DiseasesThesa TagalogNo ratings yet
- Haider OralllllllllllllllllllllllDocument13 pagesHaider OralllllllllllllllllllllllAli YehyaNo ratings yet
- LP 160610182350Document25 pagesLP 160610182350Karthik TNo ratings yet
- Derma Signs of Systemic DiseaseDocument84 pagesDerma Signs of Systemic DiseaseNaba YusraNo ratings yet
- Oral PathologyDocument18 pagesOral Pathologyمنتظر منشد دعاشNo ratings yet
- Dermatology Atlas for Medical StudentsFrom EverandDermatology Atlas for Medical StudentsRating: 4 out of 5 stars4/5 (6)
- Chicken Wing DissectionDocument4 pagesChicken Wing DissectionclaireNo ratings yet
- ENERPEEL SA - Rev - 0 - 2011Document48 pagesENERPEEL SA - Rev - 0 - 2011CHONG WEI SHENGNo ratings yet
- SKIN, HAIR, NAILS NewDocument35 pagesSKIN, HAIR, NAILS NewHind Sabahaldin100% (1)
- DERM Resource Common+Skin+Diseases+in+Africa-1Document94 pagesDERM Resource Common+Skin+Diseases+in+Africa-1OlaNo ratings yet
- By Komal Sharma Assistant ProfessorDocument14 pagesBy Komal Sharma Assistant ProfessorOphthalmology DiscussionNo ratings yet
- Pomadasys MagranthansDocument11 pagesPomadasys Magranthanspheonix_0381713No ratings yet
- Glow Up To Do ListDocument13 pagesGlow Up To Do ListMarianne R. Gutib100% (4)
- DermatologyDocument93 pagesDermatologyneha100% (5)
- Ichthyosis Hystrix CurthDocument4 pagesIchthyosis Hystrix Curtheby_3tamaNo ratings yet
- Tosp Booklet With MSP (3 Jan 2017) WordDocument112 pagesTosp Booklet With MSP (3 Jan 2017) WordArif Tri Prasetyo HarunNo ratings yet
- Estimasi PO LenteraDocument6 pagesEstimasi PO Lenteraarie wijayaNo ratings yet
- SyllabusDocument8 pagesSyllabusहुडदंग हास्य कवि सम्मलेनNo ratings yet
- Papers Cimentaciones ProfundasDocument822 pagesPapers Cimentaciones Profundasjimmy Andres100% (1)
- Freckles and Solar Lentigines Have Different Risk Factors in Caucasian WomenDocument12 pagesFreckles and Solar Lentigines Have Different Risk Factors in Caucasian WomenagityaNo ratings yet
- Skin CareDocument24 pagesSkin Careveren100% (5)
- Modul Kulit SsDocument22 pagesModul Kulit Ssshafiraa29No ratings yet
- Application Note: Tissue Reconstruction Using ThinCert™Document6 pagesApplication Note: Tissue Reconstruction Using ThinCert™Greiner Bio-OneNo ratings yet
- 2poultices and CompressesDocument73 pages2poultices and CompressesVictor IjadunminiyiNo ratings yet
- EpsDocument24 pagesEpsRosaldy MuhamadNo ratings yet
- TattooDocument24 pagesTattooElianeOliveira0% (1)
- Pioneer Institute OF Professional Studies: Decision Making For Purchasing OF Herbal Face PackDocument12 pagesPioneer Institute OF Professional Studies: Decision Making For Purchasing OF Herbal Face PackSangamesh KumashiNo ratings yet
- AcneDocument4 pagesAcnekingwinston ombionNo ratings yet
- SCIENCE - 6 - TG - Q2.docx Filename - UTF-8''SCIENCE 6 TG Q2Document103 pagesSCIENCE - 6 - TG - Q2.docx Filename - UTF-8''SCIENCE 6 TG Q2אנג' ליקהNo ratings yet
- CDI 5 Prelim ExamDocument4 pagesCDI 5 Prelim ExamHarold GaraoNo ratings yet
- Lab Report #5: Integumentary System: /40 MarksDocument10 pagesLab Report #5: Integumentary System: /40 Marksapi-535408818No ratings yet
- Cosmelan Home Pack ProtocolDocument1 pageCosmelan Home Pack ProtocolPutri IndahNo ratings yet
- 1Document1 page1Fathiyah NuramadhaniNo ratings yet
- Burns SeminarDocument66 pagesBurns SeminarPratibha Thakur100% (1)