Professional Documents
Culture Documents
13 Subacromial PDF
Uploaded by
Luis de Gonzaga Botía GarcíaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
13 Subacromial PDF
Uploaded by
Luis de Gonzaga Botía GarcíaCopyright:
Available Formats
Neuromodulation: Technology at the Neural Interface
Received: September 3, 2013 Revised: November 20, 2013 Accepted: December 2, 2013
(onlinelibrary.wiley.com) DOI: 10.1111/ner.12152
Percutaneous Peripheral Nerve Stimulation for
Chronic Pain in Subacromial Impingement
Syndrome: A Case Series
Richard D. Wilson, MD, MS*†; Michael A. Harris, MD†; Douglas D. Gunzler,
PhD‡; Maria E. Bennett, MS§; John Chae, MD*†¶
Objective: The objective of this study was to determine the effect of peripheral nerve stimulation (PNS) on pain reduction for
those with refractory subacromial impingement syndrome (SIS) and to evaluate the association with reduced disability, impair-
ment, and safety. Our hypotheses are that PNS will be associated with a reduction in pain, impairment and disability, and
improvement in quality of life while demonstrating safety.
Material and Methods: Adults with shoulder pain of at least six months duration were recruited for a three-week treatment of
percutaneous PNS applied through a percutaneous electrode to the axillary motor points of the deltoid muscle. Subjects were
followed for 12 weeks after treatment. The primary outcome was the worst pain in the last week, and secondary outcomes
included pain interference, the Disabilities of the Arm, Shoulder, and Hand questionnaire, shoulder abduction range of motion,
and safety. Analysis was with a linear mixed model.
Results: Ten subjects were recruited. Longitudinal analysis demonstrated significant reduction in pain relative to baseline
(F(1, 66) = 12.9, p < 0.01). After correcting for multiple comparisons, there were significant reductions at explantation and all
follow-up time points when compared with baseline. There were also significant improvements in pain interference (F(1,65) = 15.0,
p < 0.01), the Disabilities of the Arm, Shoulder, and Hand questionnaire (F(1,35) = 7.0, p = 0.01), and shoulder abduction range of
motion (F(1,35) = 6.3, p = 0.02).
Conclusion: Intramuscular PNS for chronic shoulder pain due to SIS is a safe treatment associated with pain reduction, lower pain
interference with activities of daily living, reduced disability, and improved shoulder abduction. Pain reduction is maintained for
at least 12 weeks after treatment.
Keywords: Chronic pain, electrode placement, nonmalignant pain, percutaneous nerve stimulation, peripheral nerve stimulation
Conflict of Interest: Richard D. Wilson is a consultant to SPR Therapeutics, LLC. Maria Bennett is an employee of and owns equity
in SPR Therapeutics, LLC. John Chae is a consultant and Chief Medical Advisor to SPR Therapeutics, LLC. Dr. Chae owns equity in SPR
Therapeutics, LLC. Dr. Chae and Mrs. Bennett are patent holders for intramuscular peripheral nerve stimulation for the treatment
of chronic pain. SPR Therapeutics, LLC. has a commercial interest in the device presented in this article.
INTRODUCTION
Shoulder pain is a common problem in the healthy adult popu-
lation, accounting for 16% of musculoskeletal complaints (1) and 12 Address correspondence to: Richard D. Wilson MD, MS, MetroHealth Medical
million physician visits annually in the United States (2). The point Center, MetroHealth Rehabilitation Institute of Ohio, N5-36, 4229 Pearl Rd.,
prevalence of shoulder pain has been estimated to be 7–27% in Cleveland, OH 44109, USA. Email: rwilson@metrohealth.org
adults less than 70 years old, with 12-month prevalence being up to * Cleveland FES Center, Case Western Reserve University, Cleveland, OH (Wilson,
47% (3). While there are multiple causes of shoulder pain, subacro- Chae), USA
mial impingement syndrome (SIS) is the most common cause, esti- †
Department of Physical Medicine and Rehabilitation, Case Western Reserve
mated to comprise up to 48% of incident cases (4). University at MetroHealth Medical Center, Cleveland, OH (Wilson, Harris, Chae),
USA
The clinical syndrome of SIS is typically associated with pain with ‡
Center for Healthcare Research and Policy, Case Western Reserve University/
movement of the shoulder, most commonly when raising the arm MetroHealth Medical Center, Cleveland, OH (Gunzler), USA
overhead. Anatomically, SIS refers to the supraspinatus tendon §
SPR Therapeutics (subsidiary of NDI Medical), Cleveland, OH (Bennett), USA
¶
impinging on the undersurface of the anterior acromion as the Department of Biomedical Engineering, Case Western Reserve University,
shoulder is abducted or flexed. Multiple pathologies, such as sub- Cleveland, OH (Chae), USA
acromial bursitis, rotator cuff tendinopathy, partial rotator cuff tears, For more information on author guidelines, an explanation of our peer review
and even small tears, either in isolation or through a combination, process, and conflict of interest informed consent policies, please go to http://
1
can create the syndrome of subacromial impingement. Regardless of www.wiley.com/bw/submit.asp?ref=1094-7159&site=1
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
WILSON ET AL.
the exact pathology, conservative treatment is aimed at controlling
pain with rest, nonsteroidal anti-inflammatory drugs, corticosteroid
injections, and improving biomechanics of the shoulder through
physical therapy. Approximately half of the patients will respond
acutely to conservative management (5).
When conservative treatment has failed and chronic pain persists,
patients are often referred for surgical management of subacromial
decompression (6,7). Unfortunately, randomized controlled trials
have not shown surgical management of SIS to be better than con-
servative therapy (8–11). Presently, there are no established treat-
ments for those with SIS who have failed conservative treatment.
We previously published a case report of successful treatment of
chronic pain due to SIS in a participant who had failed treatment of
physical therapy and corticosteroid injection, with treatment by
percutaneous peripheral nerve stimulation (PNS) (12). The treat-
ment of SIS with PNS involves the temporary placement of a single,
percutaneously placed electrode that provides stimulation to the
terminal branches of the axillary nerve to the deltoid muscle for
three weeks. This study presents the results of a complete case Figure 1. Percutaneous PNS Smartpatch System. Top: Percutaneous Electrode
loaded in a 20-gauge introducer. Bottom-left: External stimulator mounted on
series of ten participants with refractory SIS treated with PNS for the pad (anode electrode-embedded battery). Bottom-right: Configuration on
pain relief. The objective is to determine the effect of PNS on pain participant. PNS, peripheral nerve stimulation.
reduction for those with refractory SIS and to evaluate the associa-
tion with reduced disability, impairment, and safety. Our hypoth-
heart disease including artificial valves, or compromised immune
eses are that PNS will be associated with a reduction in pain,
system.
impairment and disability, and improvement in quality of life while
The study took place at an urban, academic rehabilitation center
demonstrating safety.
in the United States from April 2011 through March 2013. The pro-
tocol was approved by the local institutional review board.
METHODS
Participants Treatment and Evaluation
This was a single-center, unblinded case series of percutaneous After obtaining informed consent, all participants received a per-
PNS for SIS. Eligible participants were adults aged 21 years and older cutaneously placed lead to stimulate the terminal branches of the
with shoulder pain subjectively rated at least a 4 out of 10 on the axillary nerve to the middle and posterior deltoids. The procedure
11-point numeric rating scale of the Brief Pain Inventory Short Form, was previously described (see Fig. 1) (12). The electrode remained in
question 3 (BPI-SF3) (13,14). The pain had to be present six months place for a one-week stabilization period without delivery of stimu-
or longer, and the participant had to have previously participated in lation. The lead was then connected to the stimulator, and param-
physical or occupational therapy for shoulder pain and previous eters were set to stimulate the middle and posterior deltoids at
subacromial corticosteroid injection at the affected shoulder. Par- 12 Hz and 20 mA. Pulse duration, with a range of 20–200 μsec, was
ticipants had to have a positive response to Neer’s test (15) (sub- adjusted to produce the strongest muscle contraction of the middle
acromial injection of 5 cc 2% lidocaine), defined as 50% or greater and posterior deltoids without causing discomfort to the partici-
reduction in pain with shoulder flexion and external rotation. To pant. Participants were prescribed 6 hours of stimulation per day for
exclude large rotator cuff tears, participants had to have a muscle 3 weeks, to be completed in single or divided doses, for a total of
strength of at least a 4 out of 5 grading (Medical Research Council 126 hours of stimulation. The rationale for three weeks of treatment
Scale (16)) in shoulder abduction, internal rotation, and external came from review of data from a prior trial of PNS in hemiplegic
rotation after subacromial lidocaine injection. Participants were shoulder pain (18), in which the data suggested that many of those
required to have the ability to check their skin or have the availabil- subjects who experienced pain reduction did so after three weeks of
ity of the assistance of a reliable adult. Exclusion criteria included treatment. Two subsequent studies in which three weeks of stimu-
evidence of joint or overlying skin infection or history of recurrent lation was prescribed for hemiplegic shoulder pain found an asso-
skin infections, the need for sustained release opioid analgesics for ciation with successful pain relief (19,20). The stimulator completed
shoulder pain or other chronic pain syndrome, subacromial cortico- a cycle every 30 seconds consisting of 5 seconds to ramp up, 10
steroid injections to the shoulder in the previous eight weeks, cur- seconds at maximum stimulation, 5 seconds to ramp down, and 10
rently receiving physical or occupational therapies for shoulder seconds of no stimulation. At the conclusion of the three-week
pain, bleeding disorder or international normalized ratio >3.0 for stimulation period, the lead was removed by gently pulling on its
those on Coumadin, medical instability, pregnancy, uncontrolled exposed end. Afterward, participants underwent anterior–posterior
seizures (>1 per month for the last six months), evidence of pain and scapular-Y view radiographs of the shoulder for surveillance for
(local tenderness or from provocative testing) at the long-head retained lead fragments.
biceps tendon or acromioclavicular joint that contributed signifi- The electrical stimulation was provided by a small (58 × 36 ×
cantly to pain in the affected shoulder, moderate to severe depres- 14 mm) body-worn device (Smartpatch, SPR Therapeutics, Cleve-
sion (Beck Depression Inventory-Fast Screen (17) 13 or above), other land, OH, USA). The stimulator was attached to the skin using the
confounding neurological conditions involving the affected upper Smartpatch Pad, a custom surface electrode that includes an
limb, allergy to skin-surface electrodes or lidocaine, an implanted embedded battery (see Fig. 1). The device has a compliance monitor
2
electronic device such as cardiac pacemaker or defibrillator, valvular that records the total time of stimulator usage.
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
PNS FOR SUBACROMIAL IMPINGEMENT
Participants underwent outcome assessments by a physical points, the same model was used with the dependent variable
therapist at implantation (week 0), start of stimulation (week 1), end week (ordinal). Pairwise comparisons between baseline and the
of stimulation (week 4), and follow-up assessments at weeks 5, 8, discrete time points of EOT (week 4) and follow-up time points
and 16. Two telephone assessments also were completed at weeks 2 (weeks 5, 8, and 16) of the least squares means were computed
and 3 to assess the primary (BPI-SF3) and one secondary outcome from the model with discrete time points, and significance levels
(BPI-SF question 9 [BPI-SF9]). were interpreted using a Bonferroni correction (alpha = 0.0125). In
The primary outcome measure was BPI-SF3 (13,14), which asks both models, missing data were handled by a maximum likelihood
participants to rate their worst shoulder pain in the last week on a 0 algorithm, and the analyses were conducted by the available-case,
to 10 numeric rating scale, where 0 indicates “No pain” and 10 indi- intention-to-treat method.
cates “Pain as bad as you can imagine.” Secondary outcomes The association of changes in PPTs with a successful outcome was
included 1) pain interference with activities of daily living, BPI-SF9 evaluated in a similar fashion but with the dependent variable being
(13,14), which assesses the degree to which pain interferes with an indicator for group (success or not) and variables for week (con-
general activity, mood, walking ability, normal work, interpersonal tinuous, ordinal), a group interaction by week interaction, and a
relationships, sleep and enjoyment of life on a 0–10 numeric rating covariate for gender, which is known to affect PPTs (28).
scale, where 0 indicates no interference and 10 indicates complete All statistical analyses were made with SAS/STAT® 9.3 software
interference; 2) the Disabilities of the Arm, Shoulder, and Hand (SAS Institute Inc., Cary, NC, USA).
questionnaire (DASH) (21,22), a 30-item questionnaire measuring
physical function and symptoms in people with musculoskeletal
disorders of the upper limb on a scale of 0 to 100, with 0 indicating RESULTS
least disability and 100 indicating most disability; 3) active, pain-free
abduction range of motion (23) measured with a standard goniom- Ten participants were recruited. Demographics are shown in
eter from a standing position; 4) the Patient Global Impression of Table 1. Three participants did not complete all outcomes assess-
Change (PGIC) Scale (24), in which participants rate how much their ments. One was lost to follow-up after completing the five-week
quality of life has changed since the beginning of the study; and 5) assessment. Two withdrew after having a corticosteroid injection,
and a measure of secondary hyperalgesia, the pressure pain thresh- one of the subacromial space and the other of the long-head biceps
old (PPT). The PPTs were measured at the deltoid of the affected tendon, both occurring after the eight-week assessment. Overall,
shoulder, unaffected shoulder, and the tibialis anterior muscle on seven participants completed all outcomes assessments.
the unaffected side. The PPT is a measure of deep somatic tissue Pain. There was a significant reduction in pain in the longitudinal
sensitivity, indicated by the amount of pressure (kg/cm2) from a analysis (BPI-SF3, F(1, 66) = 12.9, p < 0.01, Table 2, Fig. 2). Compared
handheld algometer where a sensation of pressure first changes to with baseline and taking into account multiple comparisons (alpha
pain (25). The average of three measurements at each location is = 0.0125), there were significant reductions in pain at EOT (36.6%,
reported. p < 0.01), at week 5 (35.4%, p < 0.01), at week 8 (40.2%, p < 0.01),
Treatment success was defined as a reduction in the worst pain in and at week 16 (48.8%, p < 0.01). Treatment success (a 2-point or
the past week (BPI-SF3) of two points or 30% at end of treatment 30% reduction in pain at EOT) was met for 60% (six out of ten) of
(EOT). A two-point or 30% reduction has been shown to be a clini- the participants. Disability. There was a significant reduction in
cally relevant reduction in pain and has been recommended as an shoulder-related disability in the longitudinal analysis (DASH,
outcome in chronic pain trials (26,27).
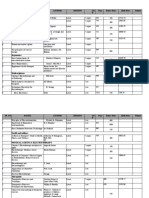
Table 1. Baseline Demographics.
Statistical Analysis
Because of the exploratory nature of this study, a formal power N 10
analysis was not completed. The effect of treatment group over Age (year, ± SD) 52.2 (±7.6)
time was analyzed using a linear mixed model for repeated mea- Female 6
sures with random effects for intercept and a first-order ante- White 5
dependent covariance structure, because it is reasonable to Black 4
assume that for each individual there is a greater correlation Hispanic 1
between assessments that are closer together and that variance Worst pain in 7 days (baseline, ±SD) 8.5 (±1.9)
might be different at different assessments. The dependent vari- Duration of pain (year, ±SD) 4.3 (±5.6)
able was week (continuous), representing a change over the course SD, standard deviation.
of the study. To evaluate the dependent variables at discrete time
Table 2. Outcomes.
Week 0 Week 1 Week 2 Week 3 Week 4 Week 5 Week 8 Week 16
Pain (±SE) 8.2 (1.1) 7.6 (1.1) 6.2 (1.1) 5.1 (1.1) 5.2 (1.1) 5.3 (1.1) 4.9 (1.1) 4.2 (1.1)
Pain interference (±SE) 5.0 (0.8) 4.7 (0.8) 3.9 (0.8) 3 (0.8) 2.4 (0.8) 2.7 (0.8) 2.0 (0.6) 2.1 (0.8)
DASH (±SE) 48.4 (6.9) 26.4 (6.9) 30.3 (6.9) 22.4 (7.4) 25.4 (7.4)
Range of motion (degrees) (±SE) 84.6 (14.6) 116.1 (14.6) 119.0 (14.6) 124.9 (15.6) 125.7 (15.6)
DASH, Disabilities of the Arm, Shoulder, and Hand questionnaire; SE, standard error.
3
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
WILSON ET AL.
F(1,35) = 7.0, p = 0.01, Table 2). Compared with baseline, there were electrodes implanted in ten participants. Seven participants (70%)
significant reductions at EOT (45.5%, p < 0.01), week 5 (37.4%, p = developed a granuloma at the electrode site that resolved by the
0.01), week 8 (53.7%, p < 0.01), and week 16 (47.5%, p < 0.01). Pain end of the follow-up period. No electrodes fractured during treat-
Interference. There was a significant reduction in pain interference ment, although five (50%) fractured on explantation. No adverse
in the longitudinal analysis (BPI-SF9, F(1,65) = 15.0, p < 0.01, Table 2). events were experienced as a result of the retained electrodes
Compared with baseline, there were significant reductions at EOT during the 12-week follow-up period. No participant experienced
(52.0%, p < 0.01), week 5 (46.0%, p < 0.01), week 8 (60.0%, p < 0.01), an infection at the electrode site.
and week 16 (58.0%, p < 0.01). Range of Motion. The longitudinal
analysis showed a significant increase in pain-free active range of
motion (aROM, F(1,35) = 6.3, p = 0.02, Table 2). Compared with base- DISCUSSION
line, there were significant increases in aROM at week 8 (47.6%, p <
0.01) and week 16 (48.6%, p < 0.01). Quality of Life. The PGIC also This case series supports the findings of the prior case report that
showed an improvement in quality of life (minimally improved, PNS may be an effective treatment for SIS. In general, there was a
much improved, or very much improved) for 80% (eight of ten) at reduction in pain associated with PNS treatment that was main-
EOT and 62.5% (five of eight) at week 16 (Fig. 3). PPTs. While the tained for 12 weeks after treatment. The reduction in pain was also
PPTs for participants who met the criteria for Global Success of Pain accompanied by a reduction in impairment and an improvement in
Relief appear to differ when compared with those who did not have use of the affected arm. These changes may be responsible for the
successful treatment (Fig. 4), there was not a statistically significant improvement in quality of life documented for most participants. It
difference in the longitudinal analysis at the affected shoulder is notable that the participants in this study were those who did not
(F(1,44) = 0.1, p = 0.7), non-affected shoulder (F(1,44) = 0.1, p = 0.8), find sustained relief with a subacromial corticosteroid injection and
or tibialis anterior (F(1,44) < 0.1, p = 0.8.) Safety. There were ten physical therapy. Such participants have limited options for treat-
ment of their shoulder pain, often being referred for surgery, which
has not been shown to result in better outcomes than conservative
10 treatment (8).
9 The mechanism of action of PNS is unknown. The stimulation
provided by PNS is different than the electrical stimulation provided
8
* * * * by transcutaneous electrical nerve stimulation, which is thought to
7 improve pain by providing paresthesias in the area of pain (29). No
6 paresthesias are experienced with percutaneous PNS because the
Pain
5 insulated electrode allows the electrical current to bypass the cuta-
4 neous sensory receptors. There is also no discomfort with the use of
percutaneous PNS because the large-diameter motor nerves are
3
stimulated at a lower intensity than the small-diameter sensory
2
nerves, allowing a comfortable muscle contraction. This is one
1 advantage of percutaneous PNS to surface neuromuscular electrical
0 stimulation, which is often limited by the discomfort created by the
0 2 4 6 8 10 12 14 16 high intensity needed to cause muscle contraction through the skin
Week (30).
It is possible that PNS affects chronic pain through central mecha-
Figure 2. Worst pain in the last week (0–10), BPI-SF3. Longitudinal analysis nisms. Prior work has shown that chronic pain due to SIS is associ-
revealed a significant changed over time (BPI-SF3, F(1,66) = 12.9, p < 0.01).
Compared with baseline, there were significant reductions at weeks 4, 5, 8, and
ated with central sensitization (31,32), an alteration in the function
16. Stimulation was provided during time represented by shaded area. BPI-SF3, of the central nervous system that can result in hyperalgesia and
Brief Pain Inventory, Short Form question 3. allodynia due to augmentation of nociceptive pathways in the
45
40
35
30
25
%
20
15 EOT
10
Week 16
5
0
Very Much Minimally No Minimally Much Very
Much Worse Worse Change Improved Improved Much
Worse Improved
Patient Global Impression of Change Scale
Figure 3. Patient Global Impression of Change Scale. Participants rated how much their quality of life has changed since the beginning of the study to end of
4
treatment (EOT) and at the end of the follow-up period (Week 16).
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
PNS FOR SUBACROMIAL IMPINGEMENT
(a) (b) (c)
10 10 10
8 8 8
PPT kg/cm2
PPT kg/cm2
PPT kg/cm2
6 6 6
4 4 4
2 2 2
0 0 0
1357911131517
0 2 4 6 8 10 12 14 16 1357911131517
0 2 4 6 8 10 12 14 16 01357911131517
2 44 6 88 10 10 12 14 16
Week Week Week
Responder Nonresponder Responder Nonresponder Responder Nonresponder
Figure 4. [Correction made on April 17, 2014 after first online publication: Figure b and c were updated.] a. Unaffected shoulder. b. Affected shoulder. c. Tibialis
anterior. Pressure pain thresholds (PPT) of responders (2-point or 30% reduction at end of treatment) compared with nonresponders. The period of stimulation is
represented by the shaded area.
central nervous system (33–35). In this study, those who experi- shoulder occurred in association with successful treatment. It is also
enced successful pain relief also experienced a nonsignificant notable that this study included a relatively short follow-up period
increase in PPTs, or a lower sensitivity to pain, at sites remote from for a chronic pain condition where long-term pain relief is an impor-
the area of stimulation that was more pronounced during the tant outcome. Unfortunately, the level of funding that was obtained
period of stimulation (Fig. 4). The differences at EOT in the PPTs, for for this study did not allow a longer follow-up period, although we
responders and nonresponders, at the affected shoulder of 3.8 kg/ plan to increase the duration of follow-up in future studies. It is also
cm2 (95% confidence interval [CI] 1.0–6.6) and at the non-affected possible that all subjects who continued to have pain after the
shoulder of 3.2 kg/cm2 (95% CI 0.9–5.5), are greater than the differ- three-week treatment period would respond more favorably to a
ences in PPTs for those with chronic SIS and the pain-free popula- longer period of stimulation, whether on the order of weeks or with
tion (31). That the changes in PPTs were seen in the non-affected a fully implanted PNS system, although this possibility was not
shoulder, an area not near the point of stimulation, suggests that an explored in this trial. Finally, because of the small sample size, it is
alteration of a central process was associated with pain relief from possible that the differences in PPTs between subgroups are spuri-
PNS. ous, although the patterns were consistent across multiple
Treatment of chronic shoulder pain due to SIS with PNS was safe measurements.
in this sample. Granulomas are a common reaction to an inert
foreign body (36) and all of those that were experienced in this
study resolved within the follow-up period. Those participants who CONCLUSION
experienced a retained electrode did not have any adverse events
as a result during the 12-week follow-up period. In our randomized PNS may be an efficacious treatment for chronic shoulder pain
controlled trial of percutaneous PNS for the treatment of hemiplegic due to SIS. Treatment with percutaneous PNS is also associated with
shoulder pain, there were no retained electrode-related complica- reduced shoulder disability, reduced pain interference, improved
tions after an average follow-up period of 18.8 months (37). The rate range of motion, and improved quality of life. Treatment with PNS is
in this study is higher than studies of PNS in hemiplegic shoulder safe and may be a new treatment for those with chronic SIS. A
pain, which range from 0–21.4% (18–20,38). It is not clear why the blinded randomized controlled trial is the next step in the contin-
rate of retained electrodes was higher in this study, although it is ued development and evaluation of this treatment modality for
possible that a difference exists between the granulation tissue that chronic shoulder pain due to SIS.
forms around the electrode in the able-bodied, who likely use their
shoulder to a greater extent than those with hemiplegia, or the
greater activity may weaken the electrode and increase the likeli- Authorship Statement
hood of fracture. Subjects with retained electrodes will continue to
be monitored per routine clinical care. Drs. Wilson, Harris, Gunzler, and Chae, and Mrs. Bennett designed
There are limitations to this study. First, this is a case series and conducted the study, including patient recruitment, data col-
without a control group to which the outcomes of the treatment lection, and data analysis. Dr. Wilson prepared the manuscript draft
group can be compared. It is possible that the improvement was a with important intellectual input from Drs. Harris, Gunzler, and
placebo response or natural recovery, although natural recovery Chae, and Mrs. Bennett. All authors approved the final manuscript.
seems less likely given that the average duration of shoulder pain in This publication was, in part, made possible by the Case Western
this study was 4.3 years (+/−standard deviation 5.6 years). There is Reserve University/Cleveland Clinic CTSA Grant Number UL1
also a limitation due to the lack of accounting for daily analgesic RR024989 from the National Center for Research Resources (NCRR),
consumption, which could affect the outcomes measured in this a component of the National Institutes of Health and NIH roadmap
study. There is a limitation in the inference that can be made about for Medical Research. Secure data storage was made possible
the mechanism of action of PNS treatment because of lack of through grants M01 RR00080 and UL1 RR024989 from NCRR/NIH.
5
outcome measures to show whether any anatomical changes at the Funding was also provided, in part, by SPR Therapeutics, LLC.
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
WILSON ET AL.
How to Cite this Article: 17. Beck AT, Steer RA, Brown GK. BDI-Fastscreen for medical patients: manual. San
Antonio, TX: The Psychological Corporation, 2000.
Wilson R.D., Harris M.A., Gunzler D.D., Bennett M.E., Chae 18. Yu DT, Chae J, Walker ME et al. Intramuscular neuromuscular electrical stimulation
for post-stroke shoulder pain: a multi-center randomized clinical trial. Arch Phys Med
J. 2014. Percutaneous Peripheral Nerve Stimulation for Rehabil 2004;85:695–704.
Chronic Pain in Subacromial Impingement Syndrome: 19. Chae J, Wilson RD, Bennett ME, Lechman TE, Stager KW. Single-lead percutaneous
A Case Series. peripheral nerve stimulation for the treatment of hemiplegic shoulder pain: a case
Neuromodulation 2014; E-pub ahead of print. DOI: series. Pain Pract 2013;13:59–67.
20. Wilson RD, Gunzler DD, Bennett ME, Chae J. Intramuscular peripheral nerve stimu-
10.1111/ner.12152 lation compared to usual care for pain relief of hemiplegic shoulder pain: a random-
ized controlled trial. Am J Phys Med Rehabil 2014;93(1):17–28.
21. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the
whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the
REFERENCES Arm, Shoulder and Hand outcome measure in different regions of the upper
extremity. J Hand Ther 2001;14:128–146.
22. Kitis A, Celik E, Aslan UB, Zencir M. DASH questionnaire for the analysis of musculo-
1. Urwin M, Symmons D, Allison T et al. Estimating the burden of musculoskeletal skeletal symptoms in industry workers: a validity and reliability study. Appl Ergon
disorders in the community: the comparative prevalence of symptoms at different 2009;40:251–255.
anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649– 23. Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing
655. shoulder range of motion. Aust J Physiother 2001;47:289–294.
2. Johnson MP, Crossley KL, O’Neil ME, Al-Zakwani IS. Estimates of direct health care 24. Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of
expenditures among individuals with shoulder dysfunction in the United States. J changes in chronic pain intensity measured on an 11-point numerical pain rating
Ortho Sports Phys Ther 2005;35 (1):A1–A26. scale. Pain 2001;94:149–158.
3. Luime JJ, Koes BW, Hendriksen IJ et al. Prevalence and incidence of shoulder pain in 25. Vanderweeen L, Oostendorp RA, Vaes P, Duquet W. Pressure algometry in manual
the general population; a systematic review. Scand J Rheumatol 2004;33:73–81. therapy. Man Ther 1996;1:258–265.
4. van der Windt DA, Koes BW, de Jong BA, Boulter LM. Shoulder disorders in general 26. Dworkin RH, Turk DC, Farrar JT et al. Core outcome measures for chronic pain clinical
practice: incidence, patient characteristics and management. Ann Rheum Dis trials: IMMPACT recommendations. Pain 2005;113:9–19.
1995;54:959–964. 27. Dworkin RH, Turk DC, Wyrwich KW et al. Interpreting the clinical importance of
5. van der Heijden GJ. Shoulder disorders: a state-of-the-art review. Baillieres Clin treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J
Rheumatol 1999;13:287–309. Pain 2008;9:105–121.
6. Codsi MJ. The painful shoulder: when to inject and when to refer. Cleve Clin J Med 28. Chesterton LS, Barlas P, Foster NE, Baxter GD, Wright CC. Gender differences in
2007;74:473–474. 7–8, 80–2 passim. pressure pain threshold in healthy humans. Pain 2003;101:259–266.
7. Cummins CA, Sasso LM, Nicholson D. Impingement syndrome: temporal outcomes 29. Melzack R. Prolonged relief of pain by brief, intense transcutaneous somatic stimu-
of nonoperative treatment. J Shoulder Elbow Surg 2009;18:172–177. lation. Pain 1975;1:357–373.
8. Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or 30. Yu DT, Chae J, Walker ME, Hart RL, Petroski GF. Comparing stimulation-induced pain
surgical treatment for subacromial impingement syndrome? A systematic review. J during percutaneous (intramuscular) and transcutaneous neuromuscular electric
Shoulder Elbow Surg 2009;18:652–660. stimulation for treating shoulder subluxation in hemiplegia. Arch Phys Med Rehabil
9. Ketola S, Lehtinen J, Arnala I et al. Does arthroscopic acromioplasty provide any 2001;82:756–760.
additional value in the treatment of shoulder impingement syndrome?: a two-year 31. Paul TM, Soo Hoo J, Chae J, Wilson RD. Central hypersensitivity in patients
randomised controlled trial. J Bone Joint Surg Br 2009;91:1326–1334. with subacromial impingement syndrome. Arch Phys Med Rehabil 2012;93:2206–
10. Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression 2209.
in patients with subacromial stage II impingement: 4–8-years’ follow-up in a pro- 32. Hidalgo-Lozano A, Fernandez-de-las-Penas C, Alonso-Blanco C, Ge HY,
spective, randomized study. Scand J Rheumatol 2006;35:224–228. Arendt-Nielsen L, Arroyo-Morales M. Muscle trigger points and pressure pain hyper-
11. Haahr JP, Ostergaard S, Dalsgaard J et al. Exercises versus arthroscopic decompres- algesia in the shoulder muscles in patients with unilateral shoulder impingement: a
sion in patients with subacromial impingement: a randomised, controlled study in blinded, controlled study. Exp Brain Res 2010;202:915–925.
90 cases with a one year follow up. Ann Rheum Dis 2005;64:760–764. 33. Petersen-Felix S, Curatolo M. Neuroplasticity–an important factor in acute and
12. Wilson RD, Harris MA, Bennett ME, Chae J. Single-lead percutaneous peripheral chronic pain. Swiss Med Wkly 2002;132:273–278.
nerve stimulation for the treatment of shoulder pain from subacromial impinge- 34. Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity
ment syndrome. Pm R 2012;4:624–628. by central neural plasticity. J Pain 2009;10:895–926.
13. Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for 35. Curatolo M, Arendt-Nielsen L, Petersen-Felix S. Central hypersensitivity in chronic
chronic nonmalignant pain. J Pain 2004;5:133–137. pain: mechanisms and clinical implications. Phys Med Rehabil Clin N Am
14. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann 2006;17:287–302.
Acad Med Singapore 1994;23:129–138. 36. Cotran RS, Kumar V, Collins T, Robbins SL. Robbins pathologic basis of disease, 6th ed.
15. Neer CS, 2nd. Anterior acromioplasty for the chronic impingement syndrome in the Philadelphia, PA: Saunders, 1999.
shoulder: a preliminary report. J Bone Joint Surg Am 1972;54:41–50. 37. Chae J, Yu DT, Walker ME et al. Intramuscular electrical stimulation for hemiplegic
16. Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research shoulder pain: a 12-month follow-up of a multiple-center, randomized clinical trial.
Council: Nerve Injuries Research Committee. His Majesty’s Stationery Office: 1942; Am J Phys Med Rehabil 2005;84:832–842.
pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the 38. Renzenbrink GJ, Ijzerman M. Percutaneous neuromuscular electrical stimulation
peripheral nervous system. By Michael O’Brien for the Guarantors of Brain. Saunders (P-NMES) for treating shoulder pain in chronic hemiplegia. Effects on shoulder pain
Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain 2010;133:2838–2844. and quality of life. Clin Rehabil 2004;18:359–365.
6
www.neuromodulationjournal.com © 2014 International Neuromodulation Society Neuromodulation 2014; ••: ••–••
You might also like
- Complex Regional Pain Syndrome: A Clinical GuideFrom EverandComplex Regional Pain Syndrome: A Clinical GuideErin F. LawsonNo ratings yet
- Delirium: Acute Brain Dysfunction in the Critically IllFrom EverandDelirium: Acute Brain Dysfunction in the Critically IllChristopher G. HughesNo ratings yet
- Dolor Sacro IliacoDocument6 pagesDolor Sacro Iliacomaria antonieta0102No ratings yet
- CRPS 1Document18 pagesCRPS 1mozi neyNo ratings yet
- m02-aula-02-historia-natural-da-dor-cervicalDocument6 pagesm02-aula-02-historia-natural-da-dor-cervicalgguida0No ratings yet
- 1 s2.0 S101595842100292X MainDocument7 pages1 s2.0 S101595842100292X MainNUR HAMIDAHNo ratings yet
- Jurnal 9 Neuropatic Pain On HIVDocument22 pagesJurnal 9 Neuropatic Pain On HIVKukuhWibisonoNo ratings yet
- Evidence-Based PT for Cervical RadiculopathyDocument9 pagesEvidence-Based PT for Cervical RadiculopathyDr Abdallah BahaaNo ratings yet
- Reduction of Pain-Related Fear and Disability in Post-Traumatic Neck Pain: A Replicated Single-Case Experimental Study of Exposure in VivoDocument12 pagesReduction of Pain-Related Fear and Disability in Post-Traumatic Neck Pain: A Replicated Single-Case Experimental Study of Exposure in VivoJazz SumanoNo ratings yet
- Disrupted Self-Perception in People With Chronic LDocument12 pagesDisrupted Self-Perception in People With Chronic L杨钦杰No ratings yet
- 2017 Low Back Pain Patients Learn To Adapt Motor Behavior With Advense Secondary ConsequencesDocument30 pages2017 Low Back Pain Patients Learn To Adapt Motor Behavior With Advense Secondary ConsequencesjaimeNo ratings yet
- Advances in The Diagnosis & Management of Neck Pain - Article.Document19 pagesAdvances in The Diagnosis & Management of Neck Pain - Article.salmankhan09215No ratings yet
- Nejmcp 2032396Document10 pagesNejmcp 2032396juan carlosNo ratings yet
- PIIS1526590018304565Document18 pagesPIIS1526590018304565gguida0No ratings yet
- Advances in The Diagnosis and Management of Neck PainDocument19 pagesAdvances in The Diagnosis and Management of Neck PainJose Fernando DiezNo ratings yet
- Review Article: Best Practice Management of Neck Pain in The Emergency Department (Part 6 of The Musculoskeletal Injuries Rapid Review Series)Document19 pagesReview Article: Best Practice Management of Neck Pain in The Emergency Department (Part 6 of The Musculoskeletal Injuries Rapid Review Series)Eduardo BarreraNo ratings yet
- Maik SLR and Slump Stretching With LBP Neural TensionDocument9 pagesMaik SLR and Slump Stretching With LBP Neural TensionFallahPhysioNo ratings yet
- Effects of Kinesio Taping For Stroke Patients WithDocument8 pagesEffects of Kinesio Taping For Stroke Patients WithBias HerkawentarNo ratings yet
- Multidisciplinary Manual Therapy Management of Cervicogenic Headache: A Case ReportDocument9 pagesMultidisciplinary Manual Therapy Management of Cervicogenic Headache: A Case ReportChirag MunjalNo ratings yet
- Vlaeyen 2021 Low Back PainDocument16 pagesVlaeyen 2021 Low Back PainThawanny de CarvalhoNo ratings yet
- Exercise in The Management of Chronic Back Pain: Thomas E. Dreisinger, PHD, FacsmDocument7 pagesExercise in The Management of Chronic Back Pain: Thomas E. Dreisinger, PHD, FacsmmazanNo ratings yet
- Editorial: Depression and OutcomeDocument3 pagesEditorial: Depression and OutcomepingusNo ratings yet
- Cervical Proprioception Impairment in Neck Pain-Pathophysiology, Clinical Evaluation, and Management: A Narrative ReviewDocument22 pagesCervical Proprioception Impairment in Neck Pain-Pathophysiology, Clinical Evaluation, and Management: A Narrative ReviewsoylahijadeunvampiroNo ratings yet
- Kristenen, NeckmusclebalanceDocument9 pagesKristenen, NeckmusclebalancePhooi Yee LauNo ratings yet
- Kwah Dan Diong, 2014Document1 pageKwah Dan Diong, 2014heruNo ratings yet
- Lumbar Epidural Steriods 2012Document42 pagesLumbar Epidural Steriods 2012m.lagruaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofnaufal12345No ratings yet
- Spondylysis in Young AthletesDocument15 pagesSpondylysis in Young AthletesFer NandoNo ratings yet
- Low Back Pain 2018Document18 pagesLow Back Pain 2018Salazar Ángel100% (1)
- Adult Spine 2015Document103 pagesAdult Spine 2015SHARMIN UrmiNo ratings yet
- Cognitive Functional Therapy An Integrated Behavioral Approach For Targeted Management of Disabling Low Back PainDocument16 pagesCognitive Functional Therapy An Integrated Behavioral Approach For Targeted Management of Disabling Low Back PainMário Márcio da Matta LopesNo ratings yet
- Birth Brachial Plexus Palsy UpdateDocument8 pagesBirth Brachial Plexus Palsy UpdateDyah SafitriNo ratings yet
- Abcdef en Cuidado CriticoDocument19 pagesAbcdef en Cuidado CriticoFernando FernándezNo ratings yet
- A Comparison of Osteopathic Spinal Manipulation With Standard Nejm199911043411903Document6 pagesA Comparison of Osteopathic Spinal Manipulation With Standard Nejm199911043411903Paola GuerraNo ratings yet
- 201705gillespie 1Document9 pages201705gillespie 1Jose PerezNo ratings yet
- Low Back PainDocument15 pagesLow Back PainwidiaNo ratings yet
- Physiotherapy Rehabilitation for Spinal Cord InjuriesDocument8 pagesPhysiotherapy Rehabilitation for Spinal Cord Injuriesdruketo vndmatNo ratings yet
- Nonspecific Low Back Pain: Clinical PracticeDocument9 pagesNonspecific Low Back Pain: Clinical PracticeandhikahadiNo ratings yet
- Chronic LumbagoDocument8 pagesChronic LumbagoOscar FrizziNo ratings yet
- 1 s2.0 S0003999319303892 MainDocument8 pages1 s2.0 S0003999319303892 MainRizkyrafiqoh afdinNo ratings yet
- Lumbar Spinal Stenosis: Syndrome, Diagnostics and Treatment: Nature Reviews Neurology August 2009Document13 pagesLumbar Spinal Stenosis: Syndrome, Diagnostics and Treatment: Nature Reviews Neurology August 2009Surya PangeranNo ratings yet
- A Systematic Evaluation of Prevalence and Diagnostic Accuracy of Sacroiliac Joint InterventionsDocument40 pagesA Systematic Evaluation of Prevalence and Diagnostic Accuracy of Sacroiliac Joint InterventionsmansyahNo ratings yet
- Telerehabilitation 5Document6 pagesTelerehabilitation 5Jerrin JacobNo ratings yet
- Alvin 2018 CervicalDocument7 pagesAlvin 2018 CervicalikhwanNo ratings yet
- Frozen Shoulder - Evidence and A Proposed Model Guiding RehabilitationDocument14 pagesFrozen Shoulder - Evidence and A Proposed Model Guiding RehabilitationMarlene RodriguezNo ratings yet
- Hair-Normalized Cortisol Waking Response As A Novel Biomarker of HPA Axis Activity Following Acute TraumaDocument9 pagesHair-Normalized Cortisol Waking Response As A Novel Biomarker of HPA Axis Activity Following Acute TraumawgNo ratings yet
- Facet Joint Pain-Advances in Patient Selection and TreatmentDocument16 pagesFacet Joint Pain-Advances in Patient Selection and TreatmentthiagoNo ratings yet
- Six-Month Follow-Up of Kinesitherapy For Cerebral Motor Disorders in Early ChildhoodDocument8 pagesSix-Month Follow-Up of Kinesitherapy For Cerebral Motor Disorders in Early ChildhoodIJAR JOURNALNo ratings yet
- Abstracts of The 2018 AANS/CNS Joint Section On Disorders of The Spine and Peripheral Nerves Annual MeetingDocument109 pagesAbstracts of The 2018 AANS/CNS Joint Section On Disorders of The Spine and Peripheral Nerves Annual MeetingEka Wahyu HerdiyantiNo ratings yet
- Diagnosis and Treatment of Sciatica: Data SupplementDocument12 pagesDiagnosis and Treatment of Sciatica: Data SupplementAstie NomleniNo ratings yet
- The Treatment of Acute Low Back Pain - Bed Rest, Exercises, or Ordinary Activity?Document5 pagesThe Treatment of Acute Low Back Pain - Bed Rest, Exercises, or Ordinary Activity?Arya Maulana NugrohoNo ratings yet
- Gray 2014Document10 pagesGray 2014Nada MachichNo ratings yet
- LSS Fritz Pain 2016Document10 pagesLSS Fritz Pain 2016Bia DiasNo ratings yet
- Thailand Anest,+02-Raviwan-FinalDocument8 pagesThailand Anest,+02-Raviwan-FinalAldaherlen BangunNo ratings yet
- BMC Musculoskeletal DisordersDocument8 pagesBMC Musculoskeletal DisordersGabriela Corrales CerdeiraNo ratings yet
- Comparison of sleep measures in ICD and CAD patientsDocument7 pagesComparison of sleep measures in ICD and CAD patientsFerdy LainsamputtyNo ratings yet
- Persistent Low Back PainDocument8 pagesPersistent Low Back PainAffan MsflNo ratings yet
- Depauw 2014Document9 pagesDepauw 2014CarolinaNo ratings yet
- Treatment Options For Patellar Tendinopathy A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy A Systematic ReviewRonny Araya AbarcaNo ratings yet
- ABO Incompatibility PDFDocument57 pagesABO Incompatibility PDFPachieNo ratings yet
- Pico Salax - Google SearchDocument1 pagePico Salax - Google SearchSZNo ratings yet
- Chapter 12 Organophosphate PoisoningDocument13 pagesChapter 12 Organophosphate Poisoningarief muhammadNo ratings yet
- Prince Price Alide Price Printer Sr. No Books Author Edition QT Y KinesiologyDocument9 pagesPrince Price Alide Price Printer Sr. No Books Author Edition QT Y KinesiologyNaveed AkhterNo ratings yet
- NSAIDs: Non-steroidal Anti-inflammatory DrugsDocument45 pagesNSAIDs: Non-steroidal Anti-inflammatory DrugsArvi KhanNo ratings yet
- Nursing Care Plan for Malaria PatientDocument2 pagesNursing Care Plan for Malaria PatientBethrice MelegritoNo ratings yet
- Guillain-Barré Syndrome in Children - Treatment and Prognosis - UpToDateDocument10 pagesGuillain-Barré Syndrome in Children - Treatment and Prognosis - UpToDateImanuel Far-FarNo ratings yet
- Virtualreal Psychotherapeutic ToolDocument29 pagesVirtualreal Psychotherapeutic Toollic.evelincincottaNo ratings yet
- S4C Human Health and DiseaseDocument6 pagesS4C Human Health and Diseasejiya singhNo ratings yet
- National Programme For Prevention and Control of DeafnessDocument5 pagesNational Programme For Prevention and Control of DeafnessMANISH MAMIDINo ratings yet
- Palliative Care: Palliative Care (Derived From The Latin Root Palliare, or "To Cloak") Is An Interdisciplinary MedicalDocument2 pagesPalliative Care: Palliative Care (Derived From The Latin Root Palliare, or "To Cloak") Is An Interdisciplinary MedicalLNo ratings yet
- Writing OetDocument3 pagesWriting OetWalid Uchiha50% (2)
- HematologyDocument69 pagesHematologyakshitaNo ratings yet
- Encyclopedia of Diseases and Disorders (Gnv64)Document482 pagesEncyclopedia of Diseases and Disorders (Gnv64)Florin Ciobanu100% (12)
- Kinesitherapie Et Covid 19 Tristan BonnevieDocument82 pagesKinesitherapie Et Covid 19 Tristan BonnevieSteveNo ratings yet
- Diseases of Renal Parenchyma - M. Sahay (Intech, 2012) WW PDFDocument314 pagesDiseases of Renal Parenchyma - M. Sahay (Intech, 2012) WW PDFMoldovan TiberiuNo ratings yet
- Nursing Advanced Skills 1684126397. - PrintDocument421 pagesNursing Advanced Skills 1684126397. - PrintFahir ÖZBAYNo ratings yet
- 5 6217311614496932277Document81 pages5 6217311614496932277DR.SANJOY GHOSHNo ratings yet
- FibromyelgiaDocument3 pagesFibromyelgiaTapash NathNo ratings yet
- Tympanoplasty - Surgical Repair of The Perforated EardrumDocument1 pageTympanoplasty - Surgical Repair of The Perforated EardrumMelly Selvia ANo ratings yet
- Rko Puskesmas 2022 Fix OkeDocument39 pagesRko Puskesmas 2022 Fix OkeFormanNo ratings yet
- Low Back Pain Guidelines-Reduced2Document26 pagesLow Back Pain Guidelines-Reduced2ranggadr100% (1)
- Oral Revalida Round 2Document63 pagesOral Revalida Round 2Mercy Anne EcatNo ratings yet
- Sleep Pattern DisturbanceDocument4 pagesSleep Pattern DisturbanceVirusNo ratings yet
- Breast Pain - UpToDateDocument22 pagesBreast Pain - UpToDateSalo MarianoNo ratings yet
- Ch2012.Decompressive Craniectomy - Operative TechniqueDocument22 pagesCh2012.Decompressive Craniectomy - Operative TechniqueKysy CodonNo ratings yet
- Sepmate ProtocolDocument2 pagesSepmate ProtocolZil PatelNo ratings yet
- The Clinical Significance of Subclinical Thyroid Dysfunction Bernadette Biondi and David S. Cooper PDFDocument56 pagesThe Clinical Significance of Subclinical Thyroid Dysfunction Bernadette Biondi and David S. Cooper PDFLorena IbarrolaNo ratings yet
- X. Comprehensive Pathophysiology and Management of Ovarian CancerDocument3 pagesX. Comprehensive Pathophysiology and Management of Ovarian CancerlieselannjacobNo ratings yet
- The Facts On Sleep Apnea SecretsDocument63 pagesThe Facts On Sleep Apnea SecretsClariceikoNo ratings yet