Professional Documents
Culture Documents
[1479683X - European Journal of Endocrinology] A clinical study on the short-term effect of berberine in comparison to metformin on the metabolic characteristics of women with polycystic ovary syndrome
Uploaded by
Trần Hồ Thạnh PhúCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
[1479683X - European Journal of Endocrinology] A clinical study on the short-term effect of berberine in comparison to metformin on the metabolic characteristics of women with polycystic ovary syndrome
Uploaded by
Trần Hồ Thạnh PhúCopyright:
Available Formats
European Journal of Endocrinology (2012) 166 99–105 ISSN 0804-4643
CLINICAL STUDY
A clinical study on the short-term effect of berberine in
comparison to metformin on the metabolic characteristics
of women with polycystic ovary syndrome
Wei Wei1,*, Hongmin Zhao1,*, Aili Wang1, Ming Sui1, Kun Liang1, Haiyun Deng1, Yukun Ma1, Yajuan Zhang1,
Hongxiu Zhang1 and Yuanyuan Guan1,2
1
Department of Gynecology and Obstetrics, Clinical Center of Reproductive Medicine, the First Affiliated Hospital of Harbin Medical University, Harbin
Medical University, 23 Youzheng Street, Nangang District, Harbin, Heilongjiang 150001, People’s Republic of China and 2Clinical Center of Reproductive
Medicine, Peking Union Medical College Hospital, Beijin 100001, People’s Republic of China
(Correspondence should be addressed to Y Guan at Department of Gynecology and Obstetrics, Clinical Center of Reproductive Medicine, the First Affiliated
Hospital of Harbin Medical University, Harbin Medical University; Email: guanyuanyuan63@yahoo.cn)
*(W Wei and H Zhao contributed equally to this work)
Abstract
Objective: Polycystic ovary syndrome (PCOS) is a frequent reproductive and metabolic disorder
associated with insulin resistance (IR). Berberine (BBR) is an isoquinoline derivative alkaloid extracted
from Chinese medicinal herbs that has been used as an insulin sensitizer. BBR may have a potential
therapeutic value for PCOS. The aim of this study was to evaluate the effects of BBR in comparison
to metformin (MET) on the metabolic features of women with PCOS.
Design and methods: Eighty-nine subjects with PCOS and IR subjects were randomized into one of
three treatment groups: BBRCcompound cyproterone acetate (CPA; nZ31), METCCPA (nZ30), and
placeboCCPA (nZ28) for 3 months. Clinical characteristics of the women and metabolic and
hormonal parameters were assessed before and after the period of treatment.
Results: Treatment with BBR in comparison to MET showed decrease in waist circumference and waist-
to-hip ratio (WHR; P!0.01), total cholesterol (TC), triglycerides (TG), and low-density lipoprotein
cholesterol (LDLC; P!0.05) as well as increase in high-density lipoprotein cholesterol (HDLC) and sex
hormone-binding globulin (SHBG; P!0.05). Similarly, treatment with BBR in comparison to placebo
showed decrease in WHR, fasting plasma glucose, fasting insulin, homeostasis model assessment
for IR, area under the curve of insulin, TC, LDLC, and TG (P!0.05) as well as increase in HDLC and
SHBG (P!0.01).
Conclusions: Intake of BBR improved some of the metabolic and hormonal derangements in a group of
treated Chinese women with PCOS. Main effects could be related to the changes in body composition in
obesity and dyslipidemia. Further controlled studies are needed for the assessment of the potential
favorable metabolic effects of BBR in women with PCOS.
European Journal of Endocrinology 166 99–105
Introduction for many metabolic and reproductive dysregulations
characteristic of women with PCOS (8–13).
Polycystic ovary syndrome (PCOS) is a common Berberine (BBR, [C20H18NO4]) is a type of isoquino-
endocrine and metabolic disorder afflicting 3–8% of line derivative alkaloid extracted from Chinese medic-
women of reproductive age. PCOS is characterized by inal herbs, such as Coptidis Rhizoma (Huanglian),
chronic anovulation, hyperandrogenism, and/or the Cortex Phellodendri (Huangbai), and Hydrastis Cana-
presence of polycystic ovary morphology (1). A wide densis (goldenseal). In China, BBR is a non-prescription
variety of risk factors have been investigated in relation oral drug for the treatment of gastrointestinal infec-
to PCOS, including obesity, glucose intolerance, and tions and diabetes. BBR possesses a wide range of
dyslipidemia, which lead to a significantly increased risk biochemical and pharmacological activities, including
for long-term type 2 diabetes mellitus (T2DM) and anti-obesity and anti-dyslipidemia (14–16). A large
cardiovascular disease (2–5). Insulin resistance (IR) is body of evidence has demonstrated that BBR is an
known to play a critical role in the pathophysiology of effective insulin sensitizer and has a comparable activity
PCOS (6, 7). The administration of insulin sensitizer to MET in reducing IR (15, 17–19). However, before we
metformin (MET) is recognized as a successful treatment can draw conclusions regarding the pharmacological
q 2012 European Society of Endocrinology DOI: 10.1530/EJE-11-0616
Online version via www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
100 W Wei, H Zhao and others EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166
properties of BBR and their applicability to the Methods
pathophysiological changes observed in PCOS, trials
examining the therapeutic value of BBR in patients with All subjects received lifestyle modification and antian-
PCOS are required. drogen compound cyproterone acetate (CPA) in the
form of combined pill with ethinyl estradiol, randomly
This study aimed to assess whether use of BBR,
assigned to the BBR, MET, or placebo groups for a
considered to be an insulin sensing agent, is effective in
3-month treatment course. Randomization was based
the treatment of endocrine characteristics of PCOS and
on a computer-generated code in blocks of six. A copy of
to compare these effects with MET therapy. The outcome
the code was stored in a sealed envelope by personnel
measures in this study included change in anthropo-
not involved in the trial.
metric measures and hormonal and metabolic indices in
All subjects received advice from a nutritionist on
a group of insulin-resistant Chinese women with PCOS. nutrition and exercise. They were instructed to limit fat
and carbohydrate intake and improve dietary behavior
without the application of a calorie-restricted diet
program. Exercise was also recommended to include
Subjects and methods 30 min/day of moderate to intense activity and was not
monitored. CPA (Diane 35, Bayer Schering Pharma)
Subjects containing 35 mg ethinyl estradiol and 2.0 mg cypro-
terone acetate were also taken in a cyclic fashion. BBR
A total of 100 subjects with PCOS and insulin resistance
(BBR hydrochloride, Northeast General Pharmaceutical
(IR) were included in this study. They were recruited Factory, Harbin, China) was administered at a dosage of
from the Clinical Centre of Reproductive Medicine of the 3!500 mg daily, MET (Bristol-Myers Squibb Company,
First Affiliated Hospital of Harbin Medical University Shanghai, China) was administered at a dosage of 3!
(Harbin, China). The diagnostic criteria for PCOS 500 mg daily, except for the first week of treatment
followed the 2003 Rotterdam ESHRE/ASRM criteria. when 500 mg was given only twice a day to reduce the
Oligomenorrhea (interval between menstrual periods incidence and severity of gastrointestinal side effects.
R35 days) or amenorrhea (absence of vaginal bleeding Placebo (provided by pharmaceutical preparation
for at least 6 months) (20) and clinical (a Ferriman– section) was administered as one tablet twice a day.
Gallwey score R6) (21) and/or biochemical hyperandro-
genism (total testosterone (TT) R58 ng/dl (2 nmol/l))
were used to assess PCOS. Normal range of TT in healthy Clinical and endocrine examination
Chinese women is no more than 2 nmol/l (22). The Clinical assessments included anthropometric measure-
phenotype of polycystic ovaries was detected by vaginal ments (height (m), weight (kg), body mass index (BMI),
ultrasound examination presenting 12 follicles or more and waist-to-hip ratio (WHR)). BMI was calculated as
in one or both ovaries and/or increased ovarian volume weight divided by height squared. WHR was defined as
(O10 ml) (23). All subjects fulfilled at least two of the ratio between the circumference of waist and hip.
the three diagnostic criteria. IR was assessed by Blood pressure was measured in the seated position in
homeostasis model assessment for IR (HOMA-IR) R3.8 the right arm after a 30 min rest period and averaged
(24) or fasting glucose insulin ratio (FGIR) %4.5 (25). over three measurements.
Exclusion conditions included the following systemic In the baseline study, vaginal bleeding in the absence
and endocrine disorders: late-onset congenital adrenal of spontaneous bleeding was induced by progesterone
hyperplasia, Cushing’s syndrome, thyroid dysfunction, withdrawal. After a 12 h overnight fast, a venous blood
hyperprolactinemia, diabetes mellitus, coronary artery sample was obtained in the morning between 0800 and
disease, and spontaneous abortion. Furthermore, 0900 h during the early follicular phase (days 2–3). In
subjects accepting treatment with medications known all subjects, circulating concentrations of the reproduc-
to alter insulin hemodynamics, ovulation induction, tive hormones TT and sex hormone-binding globulin
anti-obesity, or oral contraceptives (OCs) within 3 (SHBG) were measured. The free androgen index (FAI)Z
months were excluded from the study. All subjects (testosterone (nmol/l)/SHBG (nmol/l))!100 (26) was
were nonsmokers, and none reported chronic alcohol also calculated. Other parameters included fasting
consumption. plasma glucose (FPG) and insulin (FIN), total cholesterol
The study was conducted according to the Helsinki (TC), triglycerides (TG), high-density lipoprotein choles-
Declaration on human experimentation. The study terol (HDLC), and low-density lipoprotein cholesterol
protocol was approved by the ethics committee of the (LDLC). Immediately after obtaining the basal blood
First Affiliated Hospital of Harbin Medical University. sample, a 2 h, 75 g oral glucose tolerance test (OGTT)
The registration number of the trial is 200907. The was performed, and blood samples were obtained after
purpose, procedure, and potential risks of the study 30, 60, and 120 min to measure serum glucose and
were carefully explained to each subject, and written insulin concentrations. The degree of IR was estimated
consent was obtained before beginning the study. by a number of different methods, including calculated
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166 Effect of berberine in patients with PCOS 101
FGIR, HOMA-IR, and area under the insulin curve Results
(AUCINS). Impaired glucose tolerance (IGT) was defined
as fasting glucose O5.6 mmol/l and/or 2–h glucose All subjects were reproductive-aged Chinese females
O7.8 mmol/l (27). living in the Heilongjiang Province. Complete data from
FGIRZFPG (mg/dl)/FIN (mIU/ml) (24). 89 of the 100 subjects were analyzed. One subject from
HOMA-IRZFIN (mIU/ml)!FPG (mmol/l)/22.5 (23). the BBR group, two from the MET group, and two from
AUCINSZinsulin 0 0 !0.25Cinsulin 30 0 !0.5Cinsu- the placebo group were lost to follow-up after
lin 60 0 !0.75Cinsulin 120 0 !0.5 (28). randomization without any visits. Two subjects from
After 3 months of treatment, each subject underwent the BBR group and one from the MET group left for
the same procedures as described above. personal reasons. Two subjects from the MET group and
one from the placebo group left because of travel
difficulties. The final number of subjects in the three
Assays groups were similar (BBR 30, MET 31, and placebo 28).
Serum concentrations of TT, SHBG, and insulin were Nine subjects who received MET complained of transient
measured using the electro-chemiluminescent immuno- abdominal discomfort (nausea, vomiting, mild diarrhea,
assay method by auto-analyzer (Abbott I2000). and flatulence) and three subjects who received BBR
Plasma glucose, TC, TG, HDLC, and LDLC levels were complained of a bitter taste in their mouth.
determined using the electro-chemiluminescent
immunoassay method by auto-analyzer (Abbott V51). Clinical characteristics of the studied subjects
At baseline, there were no significant differences in
Statistical analysis any parameter among the groups (Table 1). After 3
months of treatment, body weight and BMI decreased
SPSS 13.0 (SPSS Inc., Chicago, IL, USA) was used for the significantly in all three groups; however, compared to
data analysis. A repeated measures ANOVA was used to placebo, no significant differences in body weight and
estimate the statistical difference between treatment BMI were observed in the BBR (PZ0.928, PZ0.161)
groups, including pre- and post-treatment and within and the MET groups (PZ0.146, PZ0.975). BBR and
one group between pre- and post-treatment. Logar- MET had no additive effect on decreasing weight and
ithmic transformations of FGIR, HOMA-IR, and AUCINS BMI. Waist circumference (WC) and WHR also decreased
were applied before ANOVA to ensure homogeneity of in all of the groups after 3 months of treatment.
variances. Data are presented as meanGS.D. with a value However, a greater reduction in WC was observed in
of P!0.05 considered as statistically significant. the BBR group (88.38G5.84 vs 80.22G5.17) than in
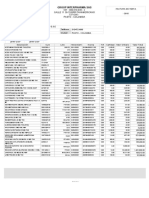
Table 1 Clinical characteristics and metabolic parameters of all subjects before and after treatment.
BBRCCA (nZ31; METCCA (nZ30; PLCCA (nZ28;
ageZ25.74G2.66) ageZ26.03G2.82) ageZ26.75G2.62)
Parameters Pre Post Pre Post Pre Post
Weight (kg) 65.11G4.06 60.06G3.61 62.98G5.21 58.58G4.66 65.13G5.10 60.16G3.95
WC (cm) 88.38G5.84 80.22G5.17 89.12G7.06 85.03G6.53s 85.23G6.18 80.75G5.28¶
BMI (kg/m2) 25.57G1.60 23.64G1.45 24.74G1.85 23.03G1.72 24.91G1.66 23.01G1.27
WHR 0.89G0.03 0.82G0.04§ 0.9G0.04 0.87G0.03 0.89G0.05 0.87G0.44¶
FPG (mmol/l) 4.97G0.67 4.36G0.53§ 5.10G0.69 4.61G0.55 5.07G0.67 4.63G0.73
FIN (mU/l) 19.77G5.80 13.07G2.45§ 21.94G12.43 13.81G4.92s 21.04G10.71 17.80G4.60
OGTT (nmol/l) 7.82G0.58 6.93G0.93 7.76G0.46 7.06G0.92 7.71G0.42 7.53G0.53
HOMA-IR 4.38G1.49 2.55G0.65§ 4.92G2.61 2.82G1.02s 4.78G2.57 3.76G0.92
FGIR 4.81G1.19 6.19G1.25§ 4.85G1.50 6.60G2.10s 4.82G1.23 5.09G1.21
AUCINS 231.55G61.72 121.66G14.72§ 258.84G90.59 122.43G11.80s 238.69G59.97 134.74G16.39
TC (mmol/l) 5.85G0.39 4.65G0.52§ 5.70G0.51 5.01G0.42 5.71G0.47 5.03G0.39‡
TG (mmol/l) 2.35G0.27 1.95G0.24* 2.26G0.25 2.09G0.22 2.30G0.24 2.10G0.23‡
LDLC (mmol/l) 4.22G0.56 3.62G0.60§ 4.25G0.51 3.95G0.48 4.28G0.52 4.05G0.51‡
HDLC (mmol/l) 1.11G0.12 1.24G0.09§ 1.13G0.13 1.19G0.10† 1.11G0.12 1.13G0.11‡
TT (nmol/l) 1.89G0.14 1.47G0.22* 1.88G0.13 1.53G0.20 1.85G0.12 1.59G0.17
SHBG (nmol/l) 25.37G4.31 58.70G11.03§ 24.20G3.52 51.98G9.66s 24.19G4.01 45.01G8.32¶
FAI (%) 7.69G1.55 2.59G1.12§ 7.92G1.22 3.16G0.98† 7.81G1.15 3.77G1.38
*P!0.05, BBR vs placebo; †P!0.05, MET vs placebo; ‡P!0.05, BBR vs MET; §P!0.01, BBR vs placebo; sP!0.01, MET vs placebo; ¶P!0.01, BBR vs
MET. CA, cyproterone acetate; PL, placebo; CPA, compound cyproterone acetate; WC, waist circumference; BMI, body mass index; WHR, waist-to-hip ratio;
FPG, fasting glucose; FIN, fasting insulin; OGTT, oral glucose tolerance test; HOMA-IR, homeostasis model assessment for insulin resistance; AUCINS, area
under the curve of insulin; TC, total cholesterol; TG, triglycerides; LDLC, low-density lipoprotein cholesterol; HDLC, high-density lipoprotein cholesterol;
TT, total testosterone; SHBG, sex hormone-binding globulin; FAI, free androgen index.
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
102 W Wei, H Zhao and others EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166
the MET group (89.12G7.06 vs 85.03G6.53; 2.59G1.12, which were significantly different from
PZ0.001). WHR decreased from 0.89G0.03 to the changes in the placebo group (PZ0.017,
0.82G0.04 in the BBR group, a significantly greater PZ0.0002). However, the changes in TT and FAI after
reduction than that observed in the MET (0.9G0.04 vs BBR treatment were not significantly different from the
0.87G0.03; P!0.001) and the placebo groups (0.89 changes observed following MET treatment (PZ0.15,
G0.05 vs 0.87G0.44; P!0.001) (Table 1). PZ0.06) (Table 1).
Carbohydrate metabolic parameter of the
studied subjects Discussion
After 3 months of treatment, the placebo group, FIN, In recent years, the recommended management
HOMA-IR, and AUCINS showed a significant reduction strategy for long-term treatment of PCOS includes
compared with the baseline (Table 1). Other markers of lifestyle modification, insulin sensitizers, and OC. This
IR, such as FGIR and FPG, remained unchanged; comprehensive intervention protocol results in better
however, compared with the subjects who received regularity of menses and fertility potential (10, 29, 30).
placebo, subjects receiving BBR or MET had a significant In this study, OC and lifestyle modification remained the
improvement in insulin sensitivity. FPG decreased from first-line therapy choice and every subject received CPA
4.97G0.67 to 4.36G0.53 with BBR (PZ0.005). FIN in the form of a combined pill during the 3-month
significantly decreased after treatment with BBR treatment period. Furthermore, BBR, MET, and placebo
(19.77G5.80 vs 13.07G2.45) or MET (21.94 were administered randomly in order to evaluate the
G12.43 vs 13.81G4.92). Moreover, a significant effects of BBR in comparison to MET in a group of
decrease in HOMA-IR and AUCINS was also detected in women with PCOS. However, this study had two
the BBR and MET groups. Conversely, FGIR was signi- limitations: small subgroups were studied and the
ficantly increased after treatment with BBR (4.81G1.19 study population was under the treatment of OC.
vs 6.19G1.25; PZ0.004) or MET (4.85G1.50 vs Compared with the baseline, significant improvement
6.60G2.10; PZ0.001). However, no significant vari- in biochemical indices of hyperandrogenemia like TT
ation in FPG, FIN, FGIR, HOMA-IR, and AUCINS was and FAI, were observed in all of the groups after 3
noted between the BBR and MET groups (Table 1). months of treatment. Our data suggest that both BBR
and MET have similar effects on reduction of concen-
trations of androgens, which are in agreement with
Lipid profile parameters of the studied subjects the results of other studies analyzing effects of MET in
After 3 months of treatment, reductions in TC and TG PCOS (9, 31).
were observed in all of the groups. In the placebo group, MET as the most commonly used insulin sensitizer
exerts favorable metabolic outcomes in women with
the level of LDLC showed a decreasing trend but was not
PCOS, such as decrease in insulin and androgen
statistically significant, and the level of HDLC remained
concentrations, normalization of menstrual cycles, and
unchanged. The BBR group demonstrated a significant
improvement ovulation rates (10, 32, 33). Although, our
decrease in TG from 2.35G0.27 to 1.95G0.24, TC from
3-month treatment period led to decrease in concen-
5.58G0.39 to 4.65G0.52, and LDLC from 4.22G0.56
trations of insulin and androgens as it was reported
to 3.62G0.60. Compared with the MET group, the
elsewhere (11, 12, 32, 33), we could not confirm sig-
differences of TG, TC, and LDLC were statistically nificant effect of MET on weight change and lipid profile
significant (PZ0.034, PZ0.012, PZ0.016). Addition- as it was shown by others (11, 12, 34). Three months
ally, BBR therapy caused a significant increase in the may be too short a time to demonstrate the effect of MET
plasma level of HDLC from 1.11G0.12 to 1.24G0.09, on metabolic abnormalities sufficiently. Furthermore,
whereas MET treatment only increased HDLC from MET is associated with a higher incidence of nausea,
1.13G0.13 to 1.19G0.10 (PZ0.039) (Table 1). vomiting, and other gastrointestinal disturbances.
BBR, as the main constituent of traditional Chinese
Reproductive hormone levels of the studied medicine, displays good potential in the prevention and
subjects treatment of metabolic disorders, including weight
control, cholesterol reduction, and antilipogenic and
TT and FAI decreased, whereas SHBG increased hypoglycemic effects (35). Several trials have reported
significantly in all of the groups after 3 months of that BBR treatment can not only reduce body weight
treatment. The level of SHBG increased significantly in and the ratio of white adipose tissue to body weight
the BBR group (25.37G4.31 vs 58.70G11.03) (7, 14) but also increase energy expenditure and the
compared with the MET (PZ0.008) and placebo groups consumption of lipid metabolites as the primary energy
(PZ0.006). BBR treatment resulted in a significant source in obese animals (36). In our study, body weight
decline in TT from 1.89G0.14 to 1.47G0.22 and a and BMI decreased in all three groups after treatment.
corresponding decline of FAI from 7.69G1.55 to Compared with the placebo group, subjects treated with
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166 Effect of berberine in patients with PCOS 103
BBR showed no significant differences in body weight With regard to safety, BBR is not considered toxic at
and BMI. Therefore, losing weight may be attributed to present doses used in clinical situations (37). Recent
lifestyle modifications rather than BBR therapy, which studies reported that by treatment with BBR (0.5 g
conflicts with previous results that demonstrated BBR’s t.i.d.) none of the subjects were observed to have marked
anti-obesity activity (14, 37). It is possible that the changes in renal and hepatic function. The pharmaco-
treatment period did not last long enough for the effect kinetics of BBR studied in rats also suggests that blood
of BBR on body weight to be observed. However, WC and clearance of BBR is very quick and that its biotrans-
WHR in the BBR group decreased significantly formation in the liver is rapid (44). The major side
compared with the MET and placebo groups, which effects of BBR can result from overdose, including
supports the notion of BBR-induced adipose tissue diarrhea, constipation, flatulence, and abdominal pain
redistribution and ameliorated central fat distribution in rare cases (7). Subjects in this clinical study tolerated
in PCOS, with significantly decreased WC and WHR of BBR well and none had mild gastrointestinal discomfort.
the subjects in the absence of weight changes. No data are available regarding the safety of BBR in
BBR has been reported to exert hypoglycemic effect in long-term use in young women and on its safety in early
either animal models or on humans and has a pregnancy.
comparable activity to MET as an insulin sensitizer. In conclusion, we showed that BBR in comparison
Moreover, BBR improves IGT and reduces blood glucose to MET showed similar metabolic effects presumably on
without increased insulin release and synthesis (38). amelioration of insulin sensitivity and reduction of
A growing body of evidence suggests that BBR improves hyperandrogenemia. BBR also appeared to have a
insulin sensitivity and stimulates glucose uptake via greater effect on the changes in body composition and
activation of the AMP-activated protein kinase pathway dyslipidemia. However, the underlying mechanisms of
(14, 39–41), which may be the target for BBR-induced its action remain to be clarified in longer term clinical
regulation of glucose and lipid metabolism. Our study trials that are required to evaluate therapeutic efficacy
confirmed that administration of BBR (0.5 g t.i.d.) was and safety of BBR in women with PCOS.
able to reduce FBG, FIN, HOMA-IR, and AUCINS in
patients with PCOS, and the outcomes were consistent
Declaration of interest
with previous reports. However, no significant vari-
ations in glycemic parameters were noted between the The authors declare that there is no conflict of interest that could be
BBR and the MET groups. It could be demonstrated that perceived as prejudicing the impartiality of the research reported.
BBR and MET exerted comparable effects on improving
glucose metabolism in PCOS.
In addition to the hypoglycemic action, a beneficial Funding
effect of BBR on lipid metabolism was also observed This research did not receive any specific grant from any funding
in animals and human subjects (7, 14, 15, 37, 42). agency in the public, commercial, or not-for-profit sector.
The mechanism of BBR-moderated lipid metabolism is
related to upregulation of LDL receptor in both mRNA
and protein in liver (7). In this study, the effect of BBR on
lipid metabolic parameters was demonstrated by the References
significant decrease in serum concentrations of TC, TG,
and LDLC and the HDLC increase after 3 months of 1 Rotterdam ESHRE/ASRM Sponsored PCOS Consensus Workshop
Group. Revised 2003 consensus on diagnostic criteria and long-
treatment. Although BBR and MET both improved term health risks related to polycystic ovary syndrome. Fertility and
glycemic parameters, their effects on lipid metabolism Sterility 2004 81 19–252.
were different. Compared with BBR, MET was less 2 Orio F Jr, Palomba S, Spinelli L, Cascella T, Tauchmanova L, Zullo F,
effective on the lipid parameters. BBR-induced allevia- Lombardi G & Colao A. The cardiovascular risk of young women
with polycystic ovary syndrome: an observational, analytical,
tion of lipid dysregulation surpassed those obtained by prospective case–control study. Journal of Clinical Endocrinology
MET in this study. and Metabolism 2004 89 3696–3701. (doi:10.1210/jc.2003-
Until now, there have been few reports concerning 032049)
the effect of BBR use on reproductive hormones. A 3 Robert A. Wild. Long-term health consequences of PCOS. Human
recent study with dexamethasone-induced IR on theca Reproduction Update 2002 8 231–241. (doi:10.1093/humupd/8.
3.231)
cells showed an excessive testosterone production and 4 Manneras-Holm L, Baghaei F, Holm G, Janson PO, Ohlsson C, Lonn M
that was effectively antagonized by BBR (43). In our & Stener-Victorin E. Coagulation and fibrinolytic disturbances in
study, level of testosterone and FAI significantly women with polycystic ovary syndrome. Journal of Clinical
decreased in the group treated with BBR in comparison Endocrinology and Metabolism 2011 96 1068–1076. (doi:10.1210/
to the placebo group. Although the mechanism of BBR- jc.2010-2279)
5 Legro RS, Castracane VD & Kauffman RP. Detecting insulin
reducing hyperandrogenism remains to be clarified, it resistance in polycystic ovary syndrome: purposes and pitfalls.
may be partially related to the remarkable effect of BBR Obstetrical and Gynecological Survey 2004 59 141–154. (doi:10.
on amelioration of IR. 1097/01.OGX.0000109523.25076.E2)
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
104 W Wei, H Zhao and others EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166
6 DeUgarte CM, Bartolucci AA & Azziz R. Prevalence of insulin 21 Laven JS, Imani B, Eijkemans MJ & Fauser BC. New approach
resistance in the polycystic ovary syndrome using the homeostasis to polycystic ovary syndrome and other forms of anovulatory
model assessment. Fertility and Sterility 2005 83 1454–1460. infertility. Obstetrical and Gynecological Survey 2002 57 755–767.
(doi:10.1016/j.fertnstert.2004.11.070) (doi:10.1097/00006254-200211000-00022)
7 Kong W, Wei J, Abidi P, Lin M, Inaba S, Li C, Wang Y, Wang Z, Si S, 22 Yue J. Obstetrics and gynecology. People’s Medical Publishing House,
Pan H, Wang S, Wu J, Wang Y, Li Z, Liu J & Jiang JD. 6th edn, ch 46, p 418. Peking: Xinhua Book Store, 2004.
Berberine is a novel cholesterol-lowering drug working through 23 Balen AH, Laven JS, Tan SL & Dewailly D. Ultrasound assessment
a unique mechanism distinct from statins. Nature Medicine 2004 of the polycystic ovary: international consensus definitions.
10 1344–1351. (doi:10.1038/nm1135) Human Reproduction Update 2003 9 505–514. (doi:10.1093/
8 Eisenhardt S, Schwarzmann N, Henschel V, Germeyer A, Wolff M, humupd/dmg044)
Hamann A & Strowitzki T. Early effects of metformin in 24 Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF &
women with polycystic ovary syndrome: a prospective random- Turner RC. Homeostasis model assessment: insulin resistance
ized, double-blind, placebo-controlled trial. Journal of Clinical and beta-cell function from fasting plasma glucose and insulin
Endocrinology and Metabolism 2006 91 946–952. (doi:10.1210/ concentrations in man. Diabetologia 1985 28 412–419. (doi:10.
jc.2005-1994) 1007/BF00280883)
9 Hoeger K, Davidson K, Kochman L, Cherry T, Kopin L & 25 Legro RS, Finegood D & Dunaif A. A fasting glucose to insulin ratio
David SG. The impact of metformin, oral contraceptives, and is a useful measure of insulin sensitivity in women with polycystic
lifestyle modification on polycystic ovary syndrome in obese ovary syndrome. Journal of Clinical Endocrinology and Metabolism
adolescent women in two randomized, placebo-controlled clinical 1998 83 2694–2698. (doi:10.1210/jc.83.8.2694)
trials. Journal of Clinical Endocrinology and Metabolism 2008 93 26 Mathur S, Baker ER, Williamson HO, Derrick FC, Teague KJ &
4299–4306. (doi:10.1210/jc.2008-0461) Fudenberg HH. Clinical significance of sperm antibodies in
10 Diamanti-Kandarakis E, Paterakis T, Alexandraki K, Piperi C, infertility. Fertility and Sterility 1981 36 486–495.
Aessopos A, Katsikis I, Katsilambros N, Kreatsas G & Panidis D. 27 WHO Technical Report Series, No. 646, 1980 (Second report of
Indices of low-grade chronic inflammation in polycystic ovary the WHO Expert Committee on Diabetes Mellitus).
syndrome and the beneficial effect of metformin. Human 28 Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA &
Reproduction 2006 21 1426–1431. (doi:10.1093/humrep/de Stern MP. Prospective analysis of the insulin resistance syndrome
l003) (syndrome X). Diabetes 1992 41 715–722. (doi:10.2337/
11 Trolle B, Flyvbjerg A, Kesmodel U & Lauszus FF. Efficacy of diabetes.41.6.715)
metformin in obese and non-obese women with polycystic ovary 29 Pasquali R, Gambineri A, Cavazza C, Ibarra Gasparini D,
syndrome: a randomized, double-blinded, placebo-controlled Ciampaglia W, Cognigni GE & Pagotto U. Heterogeneity in the
cross-over trial. Human Reproduction 2007 22 2967–2973. responsiveness to long-term lifestyle intervention and predict-
(doi:10.1093/humrep/dem271)
ability in obese women with polycystic ovary syndrome. European
12 Harborne LR, Sattar N, Norman JE & Fleming R. Metformin and
Journal of Endocrinology 2011 164 53–60. (doi:10.1530/EJE-10-
weight loss in obese women with polycystic ovary syndrome:
0692)
comparison of doses. Journal of Clinical Endocrinology and
30 Hoeger KM, Kochman L, Wixom N, Craig K, Miller RK &
Metabolism 2005 90 4593–4598. (doi:10.1210/jc.2004-2283)
Guzick DS. A randomized, 48-week, placebo-controlled trial
13 Macut D, Panidis D, Glisic B, Spanos N, Petakov M, Bjekic J,
of intensive lifestyle modification and/or metformin therapy in
Stanojlovic O, Rousso D, Kourtis A, Bozic I & Damjanovic S.
overweight women with polycystic ovary syndrome: a pilot study.
Lipid and lipoprotein profile in women with polycystic ovary
Fertility and Sterility 2004 82 421–429. (doi:10.1016/j.fertnstert.
syndrome. Canadian Journal of Physiology and Pharmacology 2008
86 199–204. (doi:10.1139/Y08-014) 2004.02.104)
14 Lee YS, Kim WS, Kim KH, Yoon MJ, Cho HJ, Shen Y, Ye JM, Lee CH, 31 Norman RJ, Davies MJ, Lord J & Moran LJ. The role of lifestyle
Oh WK, Kim CT, Hohnen-Behrens C, Gosby A, Kraegen EW, modification in polycystic ovary syndrome. Trends in Endocrinology
James DE & Kim JB. Berberine, a natural plant product, activates and Metabolism 2002 13 1630–1635.
AMP-activated protein kinase with beneficial metabolic effects 32 Luque-Ramirez M & Escobar-Morreale HF. Treatment of poly-
in diabetic and insulin-resistant states. Diabetes Care 2006 55 cystic ovary syndrome (PCOS) with metformin ameliorates
2256–2264. insulin resistance in parallel with the decrease of serum inter-
15 Yin J, Xing H & Ye J. Efficacy of berberine in patients with type 2 leukin-6 concentrations. Hormone and Metabolic Research 2010 42
diabetes mellitus. Metabolism 2008 57 712–717. (doi:10.1016/ 815–820. (doi:10.1055/s-0030-1262855)
j.metabol.2008.01.013) 33 Lord J, Thomas R, Fox B, Acharya U & Wilkin T. The effect of
16 Gu Y, Shi X, Li X, Hong J, Chen J, Gu W, Lu X, Xu G & Ning G. Effect metformin on fat distribution and the metabolic syndrome in
of traditional Chinese medicine berberine on type 2 diabetes based women with polycystic ovary syndrome – a randomised, double-
on comprehensive metabonomics. Talanta 2010 81 766–772. blind, placebo-controlled trial. British Journal of Obstetrics and
(doi:10.1016/j.talanta.2010.01.015) Gynaecology 2006 113 817–824. (doi:10.1111/j.1471-0528.
17 Yin J, Gao Z, Liu D, Liu Z & Ye J. Berberine improves glucose 2006.00966.x)
metabolism through induction of glycolysis. American Journal of 34 Kim WS, Lee YS, Cha SH, Jeong HW, Choe SS, Lee MR, Oh GT,
Physiology. Endocrinology and Metabolism 2008 294 E148–E156. Park HS, Lee KU, Lane MD & Kim JB. Berberine improves lipid
(doi:10.1152/ajpendo.00211.2007) dysregulation in obesity by controlling central and peripheral
18 Ascaso JF, Romero P, Real JT, Lorente RI, Martinez-Valls J & AMPK activity. American Journal of Physiology. Endocrinology and
Carmena R. Abdominal obesity, insulin resistance, and meta- Metabolism 2009 296 E812–E819. (doi:10.1152/ajpendo.
bolic syndrome in a southern European population. European 90710.2008)
Journal of Internal Medicine 2003 14 101–106. (doi:10.1016/ 35 Vuddanda PR, Chakraborty S & Singh S. Berberine: a potential
S0953-6205(03)00022-0) phytochemical with multispectrum therapeutic activities. Expert
19 Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Opinion on Investigational Drugs 2010 19 1297–1307. (doi:10.
Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ & Rimm EB. 1517/13543784.2010.517745)
Inflammatory markers and the risk of coronary heart disease in 36 Chen C, Zhang Y & Huang C. Berberine inhibits PTP1B activity
men and women. New England Journal of Medicine 2004 351 and mimics insulin action. Biochemical and Biophysical Research
2599–2610. (doi:10.1056/NEJMoa040967) Communications 2010 397 543–547. (doi:10.1016/j.bbrc.2010.
20 Hatch R, Rosenfield RL, Kim MH & Tredway D. Hirsutism: 05.153)
implications, etiology, and management. American Journal of 37 Zhang YF, Li XY, Zou DJ, Liu W, Yang JL, Zhu N, Huo L, Wang M,
Obstetrics and Gynecology 1981 140 815–830. Hong J, Wu PH, Ren GG & Ning G. Treatment of type 2 diabetes and
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2012) 166 Effect of berberine in patients with PCOS 105
dyslipidemia with the natural plant alkaloid berberine. Journal of 42 Brusq JM, Ancellin N, Grondin P, Guillard R, Martin S, Saintillan Y
Clinical Endocrinology and Metabolism 2008 93 2559–2565. (doi:10. & Issandou M. Inhibition of lipid synthesis through activation of
1210/jc.2007-2404) AMP kinase: an additional mechanism for the hypolipidemic
38 Zhou L, Yang Y, Wang X, Liu S, Shang W, Yuan G, Li F, Tang J, effects of berberine. Journal of Lipid Research 2006 47 1281–1288.
Chen M & Chen J. Berberine stimulates glucose transport (doi:10.1194/jlr.M600020-JLR200)
through a mechanism distinct from insulin. Metabolism 2007 43 Zhao L, Han F, Hou L, Baillargeon JP, Kuang H, Wang Y & Wu X.
56 405–412. (doi:10.1016/j.metabol.2006.10.025) Berberine reduces insulin resistance induced by dexamethasone in
39 Cheng Z, Pang T, Gu M, Gao AH, Xie CM, Li JY, Nan FJ & Li J. theca cells in vitro. Fertility and Sterility 2011 95 461–463.
Berberine-stimulated glucose uptake in L6 myotubes involves (doi:10.1016/j.fertnstert.2010.07.1090)
both AMPK and p38 MAPK. Biochimica et Biophysica Acta 2006 44 Zuo F, Nakamura N, Akao T & Hattori M. Pharmacokinetics of
760 1682–1689. berberine and its main metabolites in conventional and pseudo
40 Yin J, Hu R, Chen M, Tang J, Li F, Yang Y & Chen J. Effects of germ-free rats determined by liquid chromatography/ion trap
berberine on glucose metabolism in vitro. Metabolism 2002 51 mass spectrometry. Drug Metabolism and Disposition 2006 34
1439–1443. (doi:10.1053/meta.2002.34715)
2064–2072. (doi:10.1124/dmd.106.011361)
41 Turner N, Li JY, Gosby A, To SW, Cheng Z, Miyoshi H,
Taketo MM, Cooney GJ, Kraegen EW, James DE, Hu LH, Li J &
Ye JM. Berberine and its more biologically available derivative,
dihydroberberine, inhibit mitochondrial respiratory complex I: a
mechanism for the action of berberine to activate AMP-activated Received 9 May 2011
protein kinase and improve insulin action. Diabetes 2008 57 Revised version received 12 October 2011
1414–1418. (doi:10.2337/db07-1552) Accepted 21 October 2011
www.eje-online.org
Downloaded from Bioscientifica.com at 06/27/2019 08:15:29AM
via free access
You might also like
- Complementary and Alternative Medical Lab Testing Part 18: PsychiatryFrom EverandComplementary and Alternative Medical Lab Testing Part 18: PsychiatryRating: 5 out of 5 stars5/5 (1)
- Clinical StudyDocument5 pagesClinical StudysilvanaNo ratings yet
- Effect of Diet On Insulin Resistance in PCOSDocument15 pagesEffect of Diet On Insulin Resistance in PCOSRocío Vivancos NavarroNo ratings yet
- Effects of Probiotic Supplementation On Hormonal PDocument7 pagesEffects of Probiotic Supplementation On Hormonal PSafara WairoyNo ratings yet
- Research PaperDocument11 pagesResearch PapersilvanaNo ratings yet
- The Combined Therapy With Myo-Inositol and D-Chiro-inositol Reduces The Risk of Metabolic Disease in PCOS Overweight Patients Compared To Myo-Inositol Supplementation AloneDocument7 pagesThe Combined Therapy With Myo-Inositol and D-Chiro-inositol Reduces The Risk of Metabolic Disease in PCOS Overweight Patients Compared To Myo-Inositol Supplementation AloneFeernandaRangeelNo ratings yet
- Graessler 2012Document9 pagesGraessler 2012dora guzmanNo ratings yet
- Effect of Hypocaloric High-Protein, Low-Carbohydrate Diet Supplemented With Fennel On Androgenic and Anthropometric Indices in Overweight and Obese Women With PCOSDocument8 pagesEffect of Hypocaloric High-Protein, Low-Carbohydrate Diet Supplemented With Fennel On Androgenic and Anthropometric Indices in Overweight and Obese Women With PCOSRocío Vivancos NavarroNo ratings yet
- Artigo Pics 4 PDFDocument9 pagesArtigo Pics 4 PDFGabriela Brito de Lima SilvaNo ratings yet
- The Combined Therapy With Myo-Inositol and D-ChiroDocument8 pagesThe Combined Therapy With Myo-Inositol and D-ChirosajantkNo ratings yet
- Pcos 12 GoodDocument9 pagesPcos 12 GoodDeepak KumarNo ratings yet
- Esmaeilinezhad Et Al 2019Document8 pagesEsmaeilinezhad Et Al 2019ahmad azhar marzuqiNo ratings yet
- Biomedicine & Pharmacotherapy: SciencedirectDocument7 pagesBiomedicine & Pharmacotherapy: SciencedirectMirja AdiyaksaNo ratings yet
- (1479683X - European Journal of Endocrinology) Metformin Improves Polycystic Ovary Syndrome Symptoms Irrespective of Pre-Treatment Insulin ResistanceDocument8 pages(1479683X - European Journal of Endocrinology) Metformin Improves Polycystic Ovary Syndrome Symptoms Irrespective of Pre-Treatment Insulin ResistanceLương LýNo ratings yet
- Complementary Therapies in Medicine: SciencedirectDocument7 pagesComplementary Therapies in Medicine: SciencedirectAna Raíza OliveiraNo ratings yet
- 1 s2.0 S0039128X13000901 MainDocument5 pages1 s2.0 S0039128X13000901 MainA NNo ratings yet
- Metformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyDocument9 pagesMetformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyIam MaryamNo ratings yet
- Original Article An Observational Study of Yasmin in The Management of Women With Polycystic Ovary SyndromeDocument4 pagesOriginal Article An Observational Study of Yasmin in The Management of Women With Polycystic Ovary SyndromeBob IrsanNo ratings yet
- Li 2021Document8 pagesLi 2021Neil Patrick AngelesNo ratings yet
- Ron Danelli 2014Document14 pagesRon Danelli 2014Anisa Sekar WidhiNo ratings yet
- 1 s2.0 S2225411022000591 MainDocument9 pages1 s2.0 S2225411022000591 MaindanielwongtsNo ratings yet
- Decreased Serum Ghrelin Following Helicobacter Pylori EradicationDocument10 pagesDecreased Serum Ghrelin Following Helicobacter Pylori Eradicationps piasNo ratings yet
- Archive of SID: Leptin, Ghrelin, Adiponectin, Homocysteine and Insulin Resistance Related To Polycystic Ovary SyndromeDocument4 pagesArchive of SID: Leptin, Ghrelin, Adiponectin, Homocysteine and Insulin Resistance Related To Polycystic Ovary SyndromeherryNo ratings yet
- Effect of Pleurotus Tuber-Regium Polysaccharides Supplementation On The Progression of Diabetes Complications in Obese-Diabetic RatsDocument11 pagesEffect of Pleurotus Tuber-Regium Polysaccharides Supplementation On The Progression of Diabetes Complications in Obese-Diabetic RatsAlmaNo ratings yet
- 1 s2.0 S2589936821000475 MainDocument8 pages1 s2.0 S2589936821000475 MainA NNo ratings yet
- PJMS 38 992Document6 pagesPJMS 38 992Nur WahyuniNo ratings yet
- Artículo de SOPDocument13 pagesArtículo de SOPLili VillarroelNo ratings yet
- Medicine: Chinese Herbal Medicine On Treating Obese Women With Polycystic Ovary SyndromeDocument5 pagesMedicine: Chinese Herbal Medicine On Treating Obese Women With Polycystic Ovary SyndromeNur AwaliyaNo ratings yet
- The Role of The FODMAP Diet in IBSDocument24 pagesThe Role of The FODMAP Diet in IBSMércia FiuzaNo ratings yet
- Myo-Inositol Effects in Women With PCOS: A Meta-Analysis of Randomized Controlled TrialsDocument13 pagesMyo-Inositol Effects in Women With PCOS: A Meta-Analysis of Randomized Controlled TrialsSandeep SAmudreNo ratings yet
- Karimzadeh 2010Document5 pagesKarimzadeh 2010Derevie Hendryan MoulinaNo ratings yet
- BMC Complementary and Alternative MedicineDocument8 pagesBMC Complementary and Alternative MedicineThiago NunesNo ratings yet
- Tsai 2013 Dietary Intake Glucose Metabolism ADocument9 pagesTsai 2013 Dietary Intake Glucose Metabolism ANasrin SharifiNo ratings yet
- Austin Journal of Obesity & Metabolic SyndromeDocument6 pagesAustin Journal of Obesity & Metabolic SyndromeAustin Publishing GroupNo ratings yet
- Prebiotics Reduce Body Fat and Alter Intestinal Microbiota in Children Who Are Overweight or With ObesityDocument12 pagesPrebiotics Reduce Body Fat and Alter Intestinal Microbiota in Children Who Are Overweight or With ObesityJUAN SEBASTIAN AVELLANEDA MARTINEZNo ratings yet
- Jpe 3 E05Document6 pagesJpe 3 E05amirreza jmNo ratings yet
- Dr. Arti-POGI 001Document66 pagesDr. Arti-POGI 001sidah fatimahNo ratings yet
- Effect of Metformin On FSH, LH and Prolactin Levels in Patients With Polycystic Ovarian SyndromeDocument4 pagesEffect of Metformin On FSH, LH and Prolactin Levels in Patients With Polycystic Ovarian SyndromeTatjana Nikolić MilivojevićNo ratings yet
- Jurnal DMDocument8 pagesJurnal DMNana MuktiNo ratings yet
- Bazedoxifane Dan IbuprofenDocument7 pagesBazedoxifane Dan Ibuprofendita novia maharaniNo ratings yet
- Probioticos IBS 1Document15 pagesProbioticos IBS 1Freddy SquellaNo ratings yet
- Shahad 3Document5 pagesShahad 3Mohammed OmarNo ratings yet
- Effects of Probiotic Supplementation On Lipid Profile of Women With Rheumatoid Arthritis: A Randomized Placebo-Controlled Clinical TrialDocument7 pagesEffects of Probiotic Supplementation On Lipid Profile of Women With Rheumatoid Arthritis: A Randomized Placebo-Controlled Clinical Trialsufiah istthyNo ratings yet
- 10 1210@clinem@dgaa336 PDFDocument37 pages10 1210@clinem@dgaa336 PDFAuliya BintanNo ratings yet
- Ijcem 3 126Document5 pagesIjcem 3 126sajantkNo ratings yet
- Microbiome 3Document10 pagesMicrobiome 3Sagung Ayuska GandhariNo ratings yet
- The Effects of Polyphenol Supplementation in Addition To Calorie Restricted Diets And:or Physical Activity On Body Composition Parameters A Systematic Review of Randomized TrialsDocument13 pagesThe Effects of Polyphenol Supplementation in Addition To Calorie Restricted Diets And:or Physical Activity On Body Composition Parameters A Systematic Review of Randomized TrialsAli FaqihNo ratings yet
- Metabolic Syndrome XDocument11 pagesMetabolic Syndrome XAndres RiveraNo ratings yet
- BMCDocument12 pagesBMCManuel RomeroNo ratings yet
- Effects of Metronidazole On The Fecal Microbiome and Metabolome in Healthy DogsDocument14 pagesEffects of Metronidazole On The Fecal Microbiome and Metabolome in Healthy DogsKarin Groot JebbinkNo ratings yet
- Outcomes of Obese, Clozapine-Treated Inpatients With Schizophrenia Placed On A Six-Month Diet and Physical Activity ProgramDocument7 pagesOutcomes of Obese, Clozapine-Treated Inpatients With Schizophrenia Placed On A Six-Month Diet and Physical Activity ProgramnajibrendraNo ratings yet
- Metformin Monotherapy in Lean Women With Polycystic Ovary SyndromeDocument5 pagesMetformin Monotherapy in Lean Women With Polycystic Ovary SyndromeQuratul AyunNo ratings yet
- Effects of Thyroid Hormone and Depression On Common Components of Central ObesityDocument10 pagesEffects of Thyroid Hormone and Depression On Common Components of Central ObesitylolaNo ratings yet
- 2019 Article 480Document8 pages2019 Article 480Luisa Fernanda Zambrano DuranNo ratings yet
- The Additional Effects of A Probiotic Mix On Abdominal Adiposity and Antioxidant Status: A Double-Blind, Randomized TrialDocument9 pagesThe Additional Effects of A Probiotic Mix On Abdominal Adiposity and Antioxidant Status: A Double-Blind, Randomized TrialLeonardo AzevedoNo ratings yet
- Lee 2012Document6 pagesLee 2012jhomarlaiNo ratings yet
- Berberine SilymarinDocument6 pagesBerberine SilymarinANDRADANo ratings yet
- Pcos TreatmentDocument13 pagesPcos TreatmentAnonymous PuaFsusNo ratings yet
- Efectos de La Fibra en ObDocument15 pagesEfectos de La Fibra en ObFabiola Polo ToledoNo ratings yet
- Drisko 2006Document10 pagesDrisko 2006Elton MatsushimaNo ratings yet
- JP17 Rev 1 PDFDocument2,643 pagesJP17 Rev 1 PDFduc89100% (1)
- Susan Johnson Tungs Mu Points 04 2012Document3 pagesSusan Johnson Tungs Mu Points 04 2012Pedro Maia100% (1)
- Using Master Tung's Gallbladder Points For Diseases of The Head and NeckDocument2 pagesUsing Master Tung's Gallbladder Points For Diseases of The Head and NeckTrần Hồ Thạnh Phú100% (1)
- Dieu Tri Hoc Ket Hop Y Hien Dai Va Y Co Truyen Y Ha Noi NXB Y Hoc 2006 PDFDocument256 pagesDieu Tri Hoc Ket Hop Y Hien Dai Va Y Co Truyen Y Ha Noi NXB Y Hoc 2006 PDFTrần Hồ Thạnh PhúNo ratings yet
- Sach Tieng Anh - Bai ThuocDocument8 pagesSach Tieng Anh - Bai ThuocTrần Hồ Thạnh PhúNo ratings yet
- Susan Johnson Master Kidney Point Article 2017 PDFDocument2 pagesSusan Johnson Master Kidney Point Article 2017 PDFTrần Hồ Thạnh PhúNo ratings yet
- Bunch, Darin PDFDocument71 pagesBunch, Darin PDFJose Gregorio Parra100% (1)
- Using Master Tung's Gallbladder Points For Diseases of The Head and NeckDocument2 pagesUsing Master Tung's Gallbladder Points For Diseases of The Head and NeckTrần Hồ Thạnh Phú100% (1)
- The Miracle of Master Tung's Magic Points:: Correct Tendons' Amazing For Neck PainDocument2 pagesThe Miracle of Master Tung's Magic Points:: Correct Tendons' Amazing For Neck PainMarcin SowNo ratings yet
- Acupuntura - Pulso Tornozelo - InglêsDocument40 pagesAcupuntura - Pulso Tornozelo - InglêsAntonio de AlexandreNo ratings yet
- The Miracle of Master Tung's Magic Points:: Correct Tendons' Amazing For Neck PainDocument2 pagesThe Miracle of Master Tung's Magic Points:: Correct Tendons' Amazing For Neck PainMarcin SowNo ratings yet
- Susan Johnson Master Kidney Point Article 2017 PDFDocument2 pagesSusan Johnson Master Kidney Point Article 2017 PDFTrần Hồ Thạnh PhúNo ratings yet
- Susan Johnson Tungs Mu Points 04 2012Document3 pagesSusan Johnson Tungs Mu Points 04 2012Pedro Maia100% (1)
- Acupuntura - Pulso Tornozelo - InglêsDocument40 pagesAcupuntura - Pulso Tornozelo - InglêsAntonio de AlexandreNo ratings yet
- Bunch, Darin PDFDocument71 pagesBunch, Darin PDFJose Gregorio Parra100% (1)
- De Con Duoc Om PDFDocument4 pagesDe Con Duoc Om PDFTrần Hồ Thạnh PhúNo ratings yet
- Cham Cuu Sau Dai Hoc Nguyen Tai Thu Va Tran ThuyDocument10 pagesCham Cuu Sau Dai Hoc Nguyen Tai Thu Va Tran ThuyTrần Hồ Thạnh PhúNo ratings yet
- 10 Chapter 4Document15 pages10 Chapter 4Trần Hồ Thạnh PhúNo ratings yet
- Antidiabetic Properties Bioactive Constituents and PDFDocument12 pagesAntidiabetic Properties Bioactive Constituents and PDFTrần Hồ Thạnh PhúNo ratings yet
- De Con Duoc Om PDFDocument4 pagesDe Con Duoc Om PDFTrần Hồ Thạnh PhúNo ratings yet
- Anti-Inflammatory and Antioxidant Effects of Ethanol Extract ofDocument9 pagesAnti-Inflammatory and Antioxidant Effects of Ethanol Extract ofTrần Hồ Thạnh PhúNo ratings yet
- Antidiabetic Activity of Helicteres Angustifolia RootDocument8 pagesAntidiabetic Activity of Helicteres Angustifolia RootTrần Hồ Thạnh PhúNo ratings yet
- Herbal Medicine of The Republic of ChinaDocument255 pagesHerbal Medicine of The Republic of ChinaarielighNo ratings yet
- Cu Lao Pho Lich Su Va Van Hoa IIIDocument33 pagesCu Lao Pho Lich Su Va Van Hoa IIITrần Hồ Thạnh PhúNo ratings yet
- Antidiabetic Activity of Helicteres Angustifolia RootDocument8 pagesAntidiabetic Activity of Helicteres Angustifolia RootTrần Hồ Thạnh PhúNo ratings yet
- A-Pdf Merger DemoDocument216 pagesA-Pdf Merger DemoTrần Hồ Thạnh PhúNo ratings yet
- A Review On Phytosome Technology As A Novel Approach To Improve The Bioavailability of Nutraceuticals PDFDocument15 pagesA Review On Phytosome Technology As A Novel Approach To Improve The Bioavailability of Nutraceuticals PDFTrần Hồ Thạnh PhúNo ratings yet
- Bam Huyet Chua Benh 1156Document185 pagesBam Huyet Chua Benh 1156Trần Hồ Thạnh PhúNo ratings yet
- Full TextDocument5 pagesFull TextTrần Hồ Thạnh PhúNo ratings yet
- 3rd Periodic Test Science 10Document2 pages3rd Periodic Test Science 10Anonymous xagGSIdNo ratings yet
- Gluconeogenesis Group6Document9 pagesGluconeogenesis Group6JasneetaNo ratings yet
- Sistem Organ Reproduksi Wanita & Gangguan Haid: Jimmy Yanuar AnnasDocument110 pagesSistem Organ Reproduksi Wanita & Gangguan Haid: Jimmy Yanuar AnnasYudha SatriaNo ratings yet
- The Sistrunk ProcedureDocument4 pagesThe Sistrunk ProcedureDrTarek Mahmoud Abo Kammer100% (1)
- Final Bionformatics Practical - 17034103Document28 pagesFinal Bionformatics Practical - 17034103Manpreet KaurNo ratings yet
- Caroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesDocument15 pagesCaroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesFarid RakhmanNo ratings yet
- Carbohydrates: Biochemistry and Clinical Significance: Prof. Fritz Von T. Gella, RMT, MD October 5, 2021Document10 pagesCarbohydrates: Biochemistry and Clinical Significance: Prof. Fritz Von T. Gella, RMT, MD October 5, 2021May Ann EnoserioNo ratings yet
- Hormones and Related DrugsDocument42 pagesHormones and Related DrugsRamya PrabhuNo ratings yet
- Chapter 19 HomeostasisDocument11 pagesChapter 19 HomeostasisKiu yu LiuNo ratings yet
- DALLALhead Nurse AutosavedDocument77 pagesDALLALhead Nurse AutosavedmulanNo ratings yet
- Anabolic Steroids in A Contest Preparation of The Top World-Class BodybuilderDocument9 pagesAnabolic Steroids in A Contest Preparation of The Top World-Class BodybuilderDaddy SlvehNo ratings yet
- 5 Day Water Fast What To Expect On The Healing JourneyDocument26 pages5 Day Water Fast What To Expect On The Healing JourneysiesmannNo ratings yet
- Exam QuestionsDocument4 pagesExam QuestionsAlyssa Mariae CodornizNo ratings yet
- NEET MDS Mock TestDocument158 pagesNEET MDS Mock TestAysha NazrinNo ratings yet
- Basic Metabolic PathwaysDocument20 pagesBasic Metabolic PathwaysMapple Hernandez Belen75% (4)
- Rheumatology Case 1Document6 pagesRheumatology Case 1ALMIRA GUANNo ratings yet
- Storage Tank Design For Lactic Acid ProductionDocument30 pagesStorage Tank Design For Lactic Acid ProductionPrabuddha GopeNo ratings yet
- Group Interpharma Sas: NIT: 900,619,038 - 2 Calle 11 38-78 BRR Panamericano 7371395 - Pasto - ColombiaDocument4 pagesGroup Interpharma Sas: NIT: 900,619,038 - 2 Calle 11 38-78 BRR Panamericano 7371395 - Pasto - ColombiaBrayan Obando CalvachiNo ratings yet
- 2 EtiologyDocument9 pages2 EtiologyCatedra 2018No ratings yet
- Biochemistry - Lipid Transport & Cholesterol TransportDocument10 pagesBiochemistry - Lipid Transport & Cholesterol TransportainiNo ratings yet
- Solitary Nodule of Thyroid Gland: An Overview and Case StudyDocument3 pagesSolitary Nodule of Thyroid Gland: An Overview and Case StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Ctoij MS Id 556077Document24 pagesCtoij MS Id 556077Rakesh InnovationsAnd SolutionsInstituteNo ratings yet
- A Critical Evaluation of The Biological ConstructDocument23 pagesA Critical Evaluation of The Biological ConstructRosaneLacerdaNo ratings yet
- D.Pharm CODocument32 pagesD.Pharm COPrakash NargattiNo ratings yet
- Histiocyte Society LCH Treatment GuidelinesDocument21 pagesHistiocyte Society LCH Treatment GuidelinesAshok KumarNo ratings yet
- Minister of Health Kafue College of Nursing and Midwifery Public Health NursingDocument9 pagesMinister of Health Kafue College of Nursing and Midwifery Public Health NursingLawrence Favor SilungweNo ratings yet
- Celery JuiceDocument13 pagesCelery JuiceSilvia C. MarcelleNo ratings yet
- Hysterectomy: Max Brinsmead MB Bs PHD June 2015Document19 pagesHysterectomy: Max Brinsmead MB Bs PHD June 2015DrChauhan0% (1)
- 19-20 Spring PS10Document2 pages19-20 Spring PS10GG MMNo ratings yet
- Personal DevelopmentDocument13 pagesPersonal DevelopmentLyza PacibeNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (23)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)