Professional Documents
Culture Documents
Needle Electrode Insertion Into The Tibialis Posterior
Needle Electrode Insertion Into The Tibialis Posterior
Uploaded by
emilio9fernandez9gatOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Needle Electrode Insertion Into The Tibialis Posterior
Needle Electrode Insertion Into The Tibialis Posterior
Uploaded by
emilio9fernandez9gatCopyright:
Available Formats
1816
ORIGINAL ARTICLE
Needle Electrode Insertion Into the Tibialis Posterior: A
Comparison of the Anterior and Posterior Approaches
Seung-Nam Yang, MD, Sang-Heon Lee, MD, PhD, Hee-Kyu Kwon, MD, PhD
ABSTRACT. Yang S-N, Lee S-H, Kwon H-K. Needle elec- L5 radiculopathy. A careful approach is needed because the
trode insertion into the tibialis posterior: a comparison of the tibialis posterior muscle is located deep within the area of the
anterior and posterior approaches. Arch Phys Med Rehabil lower extremity and because the neurovascular bundle is lo-
20082008;89:1816-8. cated near the tibialis posterior muscle.
There are 2 methods currently used to place the needle
Objectives: To analyze and compare the safety of the ante- electrode. One is the traditionally used posterior approach, and
rior and posterior approaches for needle electrode placement the other is the anterior approach. In the posterior approach, the
and to examine the method for inserting the needle electrode electrode is inserted under the medial tibial shaft and directed
using the anterior approach. deep along the bone, where the muscle lies against the in-
Design: Cross-sectional study. terosseous membrane at the junction of the middle and lower
Setting: University hospital. thirds of the leg.3 In the anterior approach, the electrode is
Participants: Lower-extremity radiographs and magnetic inserted at the midpoint between the tibia and fibula at the
resonance images of 22 patients (13 men, 9 women). mid-third of the leg penetrating either the anterior tibial muscle
Interventions: Not applicable. or the extensor digitorum longus posteriorly and is advanced
Main Outcome Measure: Measurement of lower-extremity toward the interosseous membrane connecting the tibia and
radiographs and magnetic resonance imaging. fibula. The tibialis posterior is reached after passing the in-
Results: The anterior approach offers the advantage of a terosseous membrane.4
larger safe window for needle insertion into the upper third of According to a study based on 6 cadavers, access to the
the leg than the posterior approach. No significant differences tibialis posterior muscle for electrode insertion is safer with
were observed between the anterior and posterior approaches in the anterior approach than with the posterior approach because
terms of safety of needle insertion into the midpoint. The safe the anterior approach has a larger safe access window.5
zone of the overlying skin for needle insertion was found to be Little is known about the method for placing the needle
approximately 40% to 80% of the width of the tibia away from electrode, the depth of insertion, or the location in the muscle.
the lateral margin of the tibia shaft on the upper third of the leg Moreover, there is no confirmed technique for the location of
and 32% to 58% of the width of the tibia at the midpoint of the the needle insertion into the tibialis posterior muscle.
leg in the anterior approach. The aim of this study was to determine whether the anterior
Conclusions: The method suggested in this article can be or posterior approach is the safest approach to needle electrode
used for needle electromyography and deserves more wide- insertion. We also attempted to standardize the method of
spread use in clinical practice. needle electrode insertion through the anterior approaches.
Key Words: Electromyography; Magnetic resonance imag- MRI was used in this study to examine the insertion of the
ing; Needles; Rehabilitation; Tibia. needle electrode into the muscle using both approaches.
© 2008 by the American Congress of Rehabilitation Medi-
cine and the American Academy of Physical Medicine and METHODS
Rehabilitation
Two different techniques for electrode placement into the
tibialis posterior muscle were reviewed and compared using
HE TIBIALIS POSTERIOR originates from the proximal lower-extremity MRI.
T two thirds of the lateral side of the tibia, the medial side of
the fibula, and the interosseous membrane between these 2
Between 2002 and 2005, a total of 124 lower-extremity
magnetic resonance images were reviewed. Those with ana-
bones. It is inserted into the tarsal bones, mainly the navicular tomic abnormalities of the lower extremity such as tumor and
bone, and receives innervation from the tibial nerve.1,2 inflammation swelling were excluded from the study. Twenty-
The tibialis posterior is a useful muscle in the electrodiag- two patients (13 men, 9 women) were selected after reviewing
nosis of lumbosacral plexopathy, lumbosacral radiculopathy, both lower-extremity radiographs and magnetic resonance im-
tibial neuropathy, and sciatic neuropathy. It is particularly ages. Ten cases were on the left side, and 12 cases were on the
useful for the differential diagnosis of peroneal neuropathy and right side. The participants were between the ages of 18 and 65
years (mean age, 45.73y). This study protocol was approved by
the Korea University Institutional Review Board.
Several anatomic landmarks were defined, including the
anterior and posterior tibial artery and vein as well as the
From the Department of Rehabilitation Medicine, Korea University Anam Hospi- anterior border of the tibia on MRI, and the tibial tubercle and
tal, Korea University College of Medicine, Seoul, Republic of Korea.
No commercial party having a direct financial interest in the results of the research bimalleolar line on the simple radiograph.6
supporting this article has or will confer a benefit upon the authors or upon any After the length of the tibia (from the tibial tubercle to the
organization with which the authors are associated. bimalleolar line) was measured using simple radiograph, the
Reprint requests to Hee-Kyu Kwon, MD, PhD, Dept of Rehabilitation Medicine,
Korea University Anam Hospital, Korea University College of Medicine, 5 ga 126-1,
Anam-dong, Seongbuk-gu, Seoul 136-705, Republic of Korea, e-mail: hkkwon@
List of Abbreviations
korea.ac.kr.
0003-9993/08/8909-00927$34.00/0 MRI magnetic resonance imaging
doi:10.1016/j.apmr.2008.01.027
Arch Phys Med Rehabil Vol 89, September 2008
NEEDLE INSERTION IN TIBIALIS POSTERIOR, Yang 1817
Table 2: Safety Zone Overlying Skin for Needle Insertion in
Anterior Approach
Variable Upper Third of Tibia (mm) Mid-Third of Tibia (mm)
Safety zone
overlying
skin* 12.85⫺25.19 (40%⫺80%) 9.65⫺17.36 (32%⫺58%)
NOTE. Percentages are ratio to width of tibia.
*Distance from the lateral margin to tibia.
depths from the skin to the tibialis posterior muscle using the
anterior and posterior approaches were 36.19mm (range,
27.07– 45.58mm) and 35.67mm (range, 23.90 –50.42mm), re-
spectively, which corresponds to 116.17% and 118.38% of
the width of the tibial shaft at the skin using the anterior
and posterior approach, respectively. The safe window of the
anterior approach was significantly larger than that of the
posterior approach (P⬍.05). The safe zone of overlying skin
for insertion using the anterior approach was located be-
tween 12.85mm (range, 5.09 –20.45mm) and 25.19mm (range,
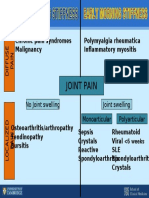
Fig 1. Parameters measured in MRI. Abbreviations: DA, depth to the 17.14 –32.97mm) from the lateral margin of the tibia, which
tibialis posterior in anterior approach; DP, depth to the tibialis corresponds to approximately 40% to 80% of the width of the
posterior in posterior approach; SWA, safety window in anterior
approach; SWP, safety window in posterior approach; SZA, safety tibia (tables 1, 2).
zone of overlying skin in anterior approach; WP, width of tibia. The mean width of the tibia at the midpoint was 30.05mm
(range, 23.94 –37.32mm). The mean safe windows for needle
insertion using the anterior and posterior approaches ⫾ SD
upper one third, the midpoint, and the lower one third of the leg were 7.71⫾2.62mm and 7.58⫾2.25mm, respectively. There
were marked. These points were chosen based on the findings was no significant difference in the safety window between the
of a previous study in which the anterior approach was used to 2 methods at the midpoint of the tibia. The safe zone of
insert the needle electrode into the tibialis posterior in the overlying skin for needle insertion using the anterior approach
mid-third of the lower leg.3,4 The width of the tibia and the was located between 9.65mm (range, 5.87–15.36mm) and
depth to the tibialis posterior by both the anterior and posterior 17.36mm (range, 10.01–26.12mm) from the lateral margin of
approaches were measured using MRI. The perpendicular dis- the tibia, which corresponds to 32% to 58% of the width of the
tance from the overlying skin to the tibialis posterior was tibia. At the midpoint along the length of the tibia, the mean
measured as the depth to the tibialis posterior in each of the 2 depth from the skin to the tibialis posterior muscle using the
approaches. anterior and posterior approach were 35.01mm (range, 25.17–
A safe window (tibia to neurovascular bundle) was measured 42.5mm) and 33.5mm (range, 25.86 – 47.83mm), respectively,
on the coronal MRI scan to avoid the neurovascular bundle in which corresponds to approximately 113.7% and 114.24% of
the anterior and posterior approaches. A safe zone of overlying the width of the anterior tibia using the anterior and posterior
skin for needle insertion into the safe window was measured approach, respectively.
using the anterior approach (fig 1). The safety window in the upper third and at the midpoint of
Four legs from fresh cadavers were used to validate our the tibia were compared during needle insertion using the
results. The standardized method for needle insertion into the anterior approach. The safety window of the upper third of the
upper third and midpoint of the leg was carried out using the leg was larger than that of the midpoint of the leg (tables 2, 3).
anterior approach. In the lower third along the length of tibia, the tibialis
posterior was a tendon in several cases. Therefore, this point
Statistical Analysis was determined to be an inappropriate needle insertion point.
We used the paired t test to compare the anterior and pos- In 4 fresh cadavers, the needle did not puncture the neuro-
terior approaches. Data were analyzed by SPSS.a vascular bundle and was well placed in the tibialis posterior
muscle using the standardized method of anterior approach in
RESULTS all cases.
In the upper third of the tibia, the mean width of the tibia was DISCUSSION
31.71mm (range, 24.77– 44.77mm). The mean safe windows
for insertion through the anterior and posterior approaches ⫾ These results confirmed the findings of a previous cadaver
SD were 12.34⫾3.59 and 6.76⫾4.67, respectively. The mean study by Lee et al,5 who reported that the anterior approach was
Table 1: Results in the Upper Third of the Tibia Table 3: Results in the Midpoint of the Tibia
Variables Anterior Approach (mm) Posterior Approach (mm) Variables Anterior Approach (mm) Posterior Approach (mm)
Safety window 12.34* 6.76 Safety window 7.71* 7.58
Depth 36.19 (116.17%) 35.67 (118.38%) Depth 35.01 (113.70%) 33.50 (114.24%)
NOTE. Percentages are ratio to width of tibia. NOTE. Percentages are ratio to width of tibia.
*P⬍.05. *P⬎.05.
Arch Phys Med Rehabil Vol 89, September 2008
1818 NEEDLE INSERTION IN TIBIALIS POSTERIOR, Yang
safer than the posterior approach for needle insertion into the Because the tibialis posterior is the principal inverter of the
upper third of the leg. We also evaluated the safety of insertion foot, it needs to be blocked in patients with an equinovarus
into the midpoint of the leg but found no significant differences deformity. The method suggested herein can also be applied to
in the safety window between the anterior and posterior ap- these cases.
proaches for needle insertion. Needle insertion into the lower
third of the leg was not considered because it was deemed to be CONCLUSIONS
an unsuitable site. The use of MRI is becoming increasingly more widespread,
MRI was used to evaluate the safety of the needle electrode which makes it relatively easy to obtain subjects. Thus, we
insertion technique and to identify the insertion point. The conclude that the method suggested in this study can be used
utility of MRI was verified by applying the same measure to for needle electromyography and deserves more widespread
cadavers. Because MRI is among the most widely used ad- use in clinical practice.
vanced techniques, it is a useful tool for determining the
appropriate technique for needle electrode insertion into the Acknowledgment: We thank Hang Lee, MD, for his kind help
muscles. Measurement using MRI applied directly to a living and support for this study.
person has the benefit of not having a loss in volume or
distance, which is often the case when taking measurements in References
cadavers. Therefore, all of the measurements obtained from 1. Gray H, Standring S, Ellis H, Berkovitz BK. Gray’s anatomy: the
living subjects may be more accurate than those obtained from anatomical basis of clinical practice. 39th ed. Edinburgh: Elsevier
cadavers. In the present study, the standardized method of Churchill Livingstone; 2005.
anterior approach obtained from this study was confirmed 2. Jenkins DB, Hollinshead WH. Hollinshead’s functional anatomy of
using fresh cadavers. the limbs and back. 8th ed. Philadelphia: WB Saunders; 2002.
The safety window for needle electrode insertion is closely 3. Geiringer SR, Davidson S. Anatomic localization for needle elec-
related to the muscle volume. A small leg volume is associated tromyography. Philadelphia: Hanley & Belfus; 1994.
with a small safety zone. In the case of a patient with progres- 4. Lee HJ, DeLisa JA. Surface anatomy for clinical needle electro-
sive severe muscle atrophy over a short period or a very thin myography. New York: Demos; 2000.
patient, the safety window for needle insertion may be smaller 5. Lee HJ, Bach JR, DeLisa JA. Needle electrode insertion into tibialis
than in general cases. Careful attention is needed in these cases. posterior: a new approach. Am J Phys Med Rehabil 1990;69:126-7.
The distance from the skin to the tibialis posterior varies 6. Manaster BJ. Diagnostic and surgical imaging anatomy: musculo-
from patient to patient. Therefore, regarding the depth of nee- skeletal. Salt Lake City: Amirsys; 2006.
dle insertion, the mean length and muscle action need to be
considered in each patient. In addition, it is important that the Supplier
practitioner is familiar with the proper feeling when puncturing a. Version 10; SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL
the interosseous membrane. 60606.
Arch Phys Med Rehabil Vol 89, September 2008
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- I Alone Level-Up (Full) (01-270) PDFDocument3,040 pagesI Alone Level-Up (Full) (01-270) PDFJC Tamayo86% (7)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Global Auto IndustryDocument200 pagesGlobal Auto IndustryPRADITYO PUTRA PURNOMO ,100% (1)
- EEG Signals and Wireless Transfer of EEG PDFDocument3 pagesEEG Signals and Wireless Transfer of EEG PDFemilio9fernandez9gatNo ratings yet
- Stable EEG Features: V. Stefanidis, G. Anogiannakis, A. Evangelou, and M. PoulosDocument9 pagesStable EEG Features: V. Stefanidis, G. Anogiannakis, A. Evangelou, and M. Poulosemilio9fernandez9gatNo ratings yet
- Differential Diagnosis SlideDocument1 pageDifferential Diagnosis Slideemilio9fernandez9gatNo ratings yet
- Computerized EEG Monitoring PDFDocument8 pagesComputerized EEG Monitoring PDFemilio9fernandez9gatNo ratings yet
- Clinical: Section 3 of 7Document13 pagesClinical: Section 3 of 7emilio9fernandez9gatNo ratings yet
- Cerebrovascular Disease Residents 2Document29 pagesCerebrovascular Disease Residents 2emilio9fernandez9gatNo ratings yet
- An EEG Study of The Neurodevelopmental H PDFDocument1 pageAn EEG Study of The Neurodevelopmental H PDFemilio9fernandez9gatNo ratings yet
- Cerebrovascular Disease ResidentsDocument14 pagesCerebrovascular Disease Residentsemilio9fernandez9gatNo ratings yet
- Complications of Posterior Cranial Fossa PDFDocument7 pagesComplications of Posterior Cranial Fossa PDFemilio9fernandez9gatNo ratings yet
- EEG - Basic Principles and Application in EpilepsyDocument19 pagesEEG - Basic Principles and Application in Epilepsyemilio9fernandez9gatNo ratings yet
- Cerebrovascular Disease Residents 1Document20 pagesCerebrovascular Disease Residents 1emilio9fernandez9gatNo ratings yet
- EMG Findings of Facial Muscles in ALS PDFDocument3 pagesEMG Findings of Facial Muscles in ALS PDFemilio9fernandez9gatNo ratings yet
- Comparison of Four Different Nerve Condu PDFDocument19 pagesComparison of Four Different Nerve Condu PDFemilio9fernandez9gatNo ratings yet
- Electrodiagnostic Reference Values For U PDFDocument7 pagesElectrodiagnostic Reference Values For U PDFemilio9fernandez9gatNo ratings yet
- The Medial Calcaneal Nerve Anatomy and N PDFDocument7 pagesThe Medial Calcaneal Nerve Anatomy and N PDFemilio9fernandez9gatNo ratings yet
- Clinical/Scientific Notes: Schwab & England: Standardization of AdministrationDocument25 pagesClinical/Scientific Notes: Schwab & England: Standardization of Administrationemilio9fernandez9gatNo ratings yet
- A Correlative Study of Quantitative EMG PDFDocument5 pagesA Correlative Study of Quantitative EMG PDFemilio9fernandez9gatNo ratings yet
- Needle EMG Muscle IdentificationDocument13 pagesNeedle EMG Muscle Identificationemilio9fernandez9gat100% (1)
- Utility of Elec Testing - ReaffirmedDocument7 pagesUtility of Elec Testing - Reaffirmedemilio9fernandez9gatNo ratings yet
- EMG GMed y Psoas1 PDFDocument10 pagesEMG GMed y Psoas1 PDFemilio9fernandez9gatNo ratings yet
- EMGLAB An Interactive EMG DecompositionDocument13 pagesEMGLAB An Interactive EMG Decompositionemilio9fernandez9gatNo ratings yet
- Saphenous Nerve EntrapmentDocument2 pagesSaphenous Nerve Entrapmentemilio9fernandez9gatNo ratings yet
- Nerves of Median Nerve (Proper Volar Digital Nerves)Document3 pagesNerves of Median Nerve (Proper Volar Digital Nerves)emilio9fernandez9gatNo ratings yet
- Order Form CTS and Ulnar N PMRJ - 1020 - OofDocument1 pageOrder Form CTS and Ulnar N PMRJ - 1020 - Oofemilio9fernandez9gatNo ratings yet
- Testimony Workshop HandoutDocument7 pagesTestimony Workshop HandoutEquipping CoursesNo ratings yet
- SD-AREE: An Advanced Modified Caesar Cipher Method To Exclude Repetition From A MessageDocument10 pagesSD-AREE: An Advanced Modified Caesar Cipher Method To Exclude Repetition From A MessageInternational Journal of Information and Network Security (IJINS)No ratings yet
- Nycy Power CableDocument3 pagesNycy Power CablePalash DahakeNo ratings yet
- Iocl ProjectDocument59 pagesIocl ProjectSeemi Halim50% (2)
- History of Indian AdvertisingDocument13 pagesHistory of Indian AdvertisingdheepaNo ratings yet
- Mefenamic AcidDocument5 pagesMefenamic AcidBeeBee SethNo ratings yet
- What Makes A Quality CurriculumDocument41 pagesWhat Makes A Quality CurriculumOana Ionescu PopaNo ratings yet
- Sample Letter Invitation To Attend Meeting To Discuss Putting in Place A Performance Improvement PlanDocument2 pagesSample Letter Invitation To Attend Meeting To Discuss Putting in Place A Performance Improvement PlanhenryNo ratings yet
- Sample Paper YTSE 2013 Class VIIDocument12 pagesSample Paper YTSE 2013 Class VIIsamridh guptaNo ratings yet
- Commercialization of New Technology-Based Product: Unit 8Document35 pagesCommercialization of New Technology-Based Product: Unit 8terlojitanNo ratings yet
- Pinyin+character Stroke OrderDocument4 pagesPinyin+character Stroke OrderAlexandra SmlNo ratings yet
- D155ax 8Document16 pagesD155ax 8eliasNo ratings yet
- Appendix 3 Study On The Impact On Stress and Anxiety Through Yoga Nidra Indian Journal of Traditional Knowledge Vol. 7 No 3Document4 pagesAppendix 3 Study On The Impact On Stress and Anxiety Through Yoga Nidra Indian Journal of Traditional Knowledge Vol. 7 No 3blanquiloNo ratings yet
- Tipaimukh Dam Presentation by NargisDocument4 pagesTipaimukh Dam Presentation by Nargisnoman13bd100% (2)
- About Myself: - StrenghtsDocument2 pagesAbout Myself: - StrenghtsGabriela MoNo ratings yet
- Unit 1-5 NEP (UNDERSTANDING POLITICAL THEORY)Document78 pagesUnit 1-5 NEP (UNDERSTANDING POLITICAL THEORY)GAGAN ANAND100% (1)
- Aggregate Planning in The Supply ChainDocument15 pagesAggregate Planning in The Supply ChainPrasad GantiNo ratings yet
- WorldCom Accounting ScandalDocument30 pagesWorldCom Accounting ScandalLari Jean Gallos100% (1)
- Thesis Report On Ad Hoc NetworkDocument6 pagesThesis Report On Ad Hoc Networkqpftgehig100% (2)
- Darwin WorksheetDocument2 pagesDarwin WorksheetjcrawlinsNo ratings yet
- Criterion D: Applying Math in Real-World Contexts: Angles & ClocksDocument7 pagesCriterion D: Applying Math in Real-World Contexts: Angles & ClockskatenerdypooNo ratings yet
- Is 1726 1991Document17 pagesIs 1726 1991RaykochiNo ratings yet
- Scoring Rubric OutputDocument1 pageScoring Rubric OutputNathaniel JuanNo ratings yet
- Relevel Test ProposalDocument6 pagesRelevel Test ProposalMonika AcharyaNo ratings yet
- Guidelines On Methods On Livestock ProductivityDocument173 pagesGuidelines On Methods On Livestock ProductivityMonaliz NagrampaNo ratings yet
- Service Manual: XM-222MK2Document4 pagesService Manual: XM-222MK2Gonzalo BrancoNo ratings yet
- The Return From One Investment Is 0.711 More Than The Other (Your Answer Is Incorrect)Document6 pagesThe Return From One Investment Is 0.711 More Than The Other (Your Answer Is Incorrect)Dolly TrivediNo ratings yet
- Anthropology: Gio Pabualan Jerome Quitoriano Ralf PlacidoDocument14 pagesAnthropology: Gio Pabualan Jerome Quitoriano Ralf PlacidoYannel VillaberNo ratings yet