Professional Documents
Culture Documents
Attenuation of Sepsis-Related Immunoparalysis by Continuous Veno-Venous Hemofiltration in Experimental Porcine Pancreatitis
Uploaded by
manuelantoniomenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Attenuation of Sepsis-Related Immunoparalysis by Continuous Veno-Venous Hemofiltration in Experimental Porcine Pancreatitis
Uploaded by
manuelantoniomenaCopyright:
Available Formats
Attenuation of sepsis-related immunoparalysis by continuous veno-
venous hemofiltration in experimental porcine pancreatitis
Emre F. Yekebas, MD; Claus F. Eisenberger, MD; Henning Ohnesorge, MD; Armin Saalmüller, MD;
Holger-Andreas Elsner, MD; Madelaine Engelhardt, MD; Andrea Gillesen, MD; Jan Meins, MD;
Marcel The, MD; Tim Strate, MD; Christoph Busch, MD; Wolfram T. Knoefel, MD; Christian Bloechle, MD;
Jakob R. Izbicki, MD
Objectives: In light of evidence suggesting that hemofiltration periodic filter change was significantly superior compared with less
favorably influences septic diseases by removing sepsis media- intensive treatment modalities (low-volume CVVH, no filter change) in
tors, the impact of different modalities of continuous veno-venous sepsis protection. Long-term survival (>60 hrs) was found in 67% of
hemofiltration (CVVH) on outcome and immunologic derange- group 4 and 33% of group 3 animals (p < .05), whereas in controls and
ments in porcine pancreatogenic sepsis was evaluated. group 2 no animal survived. CVVH ameliorated the initial serum tumor
Design: Randomized, controlled intervention trial. necrosis factor-␣ response and prevented sepsis-induced in vitro endo-
Subjects: Forty-eight minipigs of either sex. toxin hyporesponsiveness. Down-regulation of major histocompatibility
Interventions: Pancreatitis was induced by intraductal injec- complex II and CD14 expression on monocytes was significantly im-
tion of sodium taurocholate (4%, 1 mL/kg body weight [BW]) and proved by CVVH. Improved oxidative burst and phagocytosis capacity in
enterokinase (2 U/kg BW). Animals were allocated either to un- polymorphonuclear leukocytes suggested that leukocyte function was
treated controls— group 1— or to one of three treatment stabilized by CVVH. Also, CVVH significantly reduced bacterial translo-
groups— group 2: low-volume CVVH (20 mL/kg BW), no change of cation and endotoxemia.
hemofilters; group 3: low-volume CVVH, filters changed every 12 Conclusions: Hemofiltration reversed sepsis-induced immuno-
hrs; and group 4: high-volume CVVH (100 mL/kg BW), filters paralysis in a porcine model of bile acid–induced pancreatitis.
changed every 12 hrs. Survival represented the major parameter Implications for human pancreatitis must be validated in prospec-
of the study. Serum cytokine levels, sepsis-related down-regula- tive, clinical protocols. (Crit Care Med 2001; 29:1423–1430)
tion of major histocompatibility complex II and CD14 expression KEY WORDS: swine; physiopathology of pancreatitis; mediators
on leukocytes, bacterial translocation, and endotoxemia were of inflammation; tumor-necrosis-factor; cytokines; sepsis syn-
further parameters evaluated in the study. drome; immunoparalysis; immunology of monocytes; immunology
Measurements and Main Results: High-volume CVVH combined with of neutrophils; bacterial translocation
S evere pancreatitis leading to sep- cades. The final pathway of pancreatogenic atitis-related derangements in a porcine
sis-related multiple organ dys- sepsis shares many immunologic charac- model of necrotizing pancreatitis (14).
function is a devastating disease teristics with other septic diseases, includ- However, because the severity of the
that induces severe alterations ing the excessive release of cytokines (1– 4) model lead to an eventually lethal “toxin
of the immune system and triggers the and functional leukocyte disorders (5, 6). shock,” CVVH failed to result in long-
activation of numerous inflammatory cas- Treatments have been suggested aiming term survival. In contrast to that prelim-
symptomatically at the nonselective elimi- inary study, in the present series an ex-
nation of sepsis mediators thought to be perimental setting was established that
From the Departments of Surgery (EFY, CFE, ME, associated with systemic complications af- resulted in sepsis-associated multiple or-
AG, JM, MT, TS, CB, WTK, CB, JRI), Anesthesiology ter the onset of pancreatitis. This includes gan failure secondary to the onset of the
(HO), and Medical Microbiology and Immunology (HAE), continuous veno-venous hemofiltration disease, thus mimicking the clinical sit-
University Hospital Eppendorf, Hamburg, Germany; and (CVVH), reported to be of considerable ben- uation in humans better than previous
the Federal Research Center for Virus Diseases of
Animals, Tuebingen, Germany (AM). efit in the treatment of multiple organ dys- models. Based on this new setting, we
Supported, in part, by grants of the “Forschungs- function secondary to sepsis (7, 8) as well as examined whether CVVH, performed in
und Studienstiftung der Vereinigung Nordwestdeut- to severe pancreatitis (9, 10). This benefit of different modalities, would result in de-
scher Chirurgen,” “Verein zur Förderung der chirurgis- CVVH has been ascribed to its potential in finitive survival and provide protection
chen Forschung am UKE e.V.,” and Hospal Medizin-
technik GmbH, Nürnberg, Germany. removing sepsis mediators such as cyto- from sepsis. A postulated loss of efficiency
Address requests for reprints to: Jakob R. Izbicki, kines (9, 11, 12), activated complement fac- of filter membranes resulting from their
MD, Abteilung für Allgemeinchirurgie, Universitätsk- tors (7, 9), and platelet activating factor long-term application (13) was assessed
rankenhaus Eppendorf, Martinistr. 52, D-20246 Ham-
burg, Deutschland. E-mail: izbicki@uke.uni-ham-
(13). by periodic change of hemofilters. Vari-
burg.de In a pilot study, we proved CVVH- ous filtration rates were applied to eval-
Copyright © 2001 by Lippincott Williams & Wilkins induced improvement of several pancre- uate whether increasing plasma turnover
Crit Care Med 2001 Vol. 29, No. 7 1423
results in better outcome as reported in any treatment. In three treatment groups, dif- Microbiological Evaluation. Processing of
clinical trials (15). To examine whether ferent modalities of CVVH were applied after a swabs for microbiological analysis and differ-
CVVH favorably influences immunologic decline of the total peripheral resistance of entiation of isolates was performed using stan-
disorders, serum levels of pro- and anti- 30%. Group 2 animals (n ⫽ 12) underwent dard techniques classifying microbiological
CVVH without changing hemofilters. In samples as positive or negative. The following
inflammatory cytokines and sepsis-
groups 3 and 4 (n ⫽ 12 each), hemofilters subsets were assessed: 1) Gram-negative, en-
induced down-regulation of the mono- were changed every 12 hrs. Groups 2 and 3 dotoxin-containing Enterobacteriaceae/non-
cyte antigens major histocompatibility underwent a filtration turnover of 20 mL/kg/ fermentative rods (including Escherichia coli,
complex (MHC) II and CD14 were mea- hr; group 4, representing the most intensive Proteus mirabilis, and Klebsiella pneu-
sured. The immunologic screening in- treatment modality, underwent a filtration moniae); 2) Gram-positive cocci; and 3) Gram-
cluded oxidant burst and phagocytosis ca- turnover of 100 mL/kg/hr. After a maximal negative or -positive anaerobes.
pacity of polymorphonuclear leukocytes observation period of 60 hrs, animals were Flow Cytometric Analysis—Antibodies
(PMNs), which are known to be impaired killed. and Conjugates for Immunophenotyping. An-
in septic diseases (16, 17). Further, we Definition of Sepsis. Modifying generally ti-MHC class II (monoclonal antibody MSA3,
assessed whether CVVH prevents endo- accepted criteria (18, 19), the occurrence of contributed by Dr. Saalmüller, Tuebingen,
toxin hyporesponsiveness, which is a sepsis was assumed when bacteremia proved Germany) to assess monocyte and T-cell MHC
by positive blood cultures was associated with II expression (T-cells not reported); anti-CD14
common problem in advanced sepsis.
at least two of the following signs: 1) body (My 4, Coulter Immunotech Diagnostics,
temperature ⬎38.5°C or ⬍36°C in (nonhemo- Krefeld, Germany) to assess endotoxin recep-
MATERIALS AND METHODS filtrated) controls and an increase of ⬎1.5°C tor expression on monocytes; and anti-SWC3
compared with baseline values in treatment (Swine Workshop Cluster 1, 8/1a3, contrib-
Anesthesia and Surgical Preparation. The groups, respectively, because preliminary ex- uted by Dr. Glatthaar, Reutlingen, Germany),
study was approved by the Animal Care Com- periments had shown a CVVH-related decrease a specific porcine antigen without a human
mittee of the University of Hamburg. Forty- of body temperature of 1.4°C (range, 1.1–1.6; CD analog to differentiate SWC3⫺ lympho-
eight fasted minipigs (body weight [BW] n ⫽ 5); 2) heart rate ⬎120 beats/min; and 3) cytes from SWC3⫹ monocytes and granulo-
21–30 kg) were premedicated intramuscularly altered white blood cell count of ⬎12,000 or cytes, were used.
with flunitrazepam (0.1 mg/kg) and atropine ⬍4000 cells/mm3. Staining of cells for two-color flow cyto-
(0.06 mg/kg). Adequate anesthetic depth was Serum Lipase, C-Reactive Protein, metric analysis was performed in a two-step
achieved by continuous intravenous applica- Trypsinogen Activation Peptides, and White procedure: 1) incubation of whole peripheral
tion of propofol (6 mg/kg/hr) and fentanyl (10 Blood Cell Count. Lipase levels were measured blood (100 L) with the respective primary
g/kg/hr). After laparotomy, the pancreatic using a commercial assay kit (Delta Test Assay antibodies (50 L); and 2) incubation with the
duct was cannulated by a 5-Fr umbilical vein for pancreatic lipase, Sigma Chemical). Plas- respective isotype-specific conjugates. Cells
catheter. Before closing the laparotomy, two matic C-reactive protein (CRP) concentrations were shielded from light at 4°C before analy-
silicon drainage tubes were placed in the ab- were detected with an enzyme-linked immu- sis. Analysis was performed on a flow cytom-
dominal cavity for sampling peritoneal secre- nosorbent assay (ELISA) as previously de- eter with a four-decade, 1024-channel, loga-
tions for microbiological analysis. After the scribed (20). Urinary trypsinogen activation rithmic amplifier (FACS-Calibur, Becton
instrumentation of the animals by arterial and peptide (TAP) measurements were performed Dickinson, Heidelberg, Germany). A mini-
pulmonary catheters, mean arterial blood with an ELISA (Biotrin, Sinsheim, Germany). mum of 15,000 events was analyzed for each
pressure (MAP), central venous pressure, and White blood cell (WBC) counts were per- sample.
heart rate (HR) were monitored continuously. formed using a Coulter counter (Coulter Elec- Phagocytosis Activity and Oxidant Burst.
Total peripheral resistance (TPR) and cardiac tronics, Krefeld, Germany). The quantification of phagocytic and respira-
index (CI) were calculated intermittently. Cytokines. All cytokines evaluated in this tory burst activity in PMNs to assess pancre-
Hemofiltration. Zero-balanced CVVH was study were assessed both in serum (pre- and atitis-related alterations of leukocyte function
performed in a predilution mode using a poly- postfilter) and in hemofiltrate. The concentra- was performed using commercially available
acrylonitrile membrane (AN 69S, Prisma M tions of TNF-␣ (pig TNF-␣, Endogen, Eching, specific test kits (PHAGOTEST, PHAGO-
60, Hospal Medizintechnik, Nürnberg, Ger- Germany), and IL-10 (pig IL-10, BioSource, BURST, Orpegen Pharma, Heidelberg, Ger-
many) connected to a continuous blood pump Camarillo, CA) were measured by swine- many).
(Prisma, Hospal Medizintechnik). Ultrafiltrate specific ELISA kits. TGF-1, known to show For measurement of phagocytosis activity
rates were 20 mL/hr/kg BW in groups 2 and 3, high homology between the human and por- in PMNs, whole blood aliquots (100 L) were
and 100 mL/hr/kg in group 4. To provide in- cine protein (21), was detected using a human incubated with a fluorescein isothiocyanate–
formation about the elimination of pancreati- ELISA (Quantikine, R&D Systems, Wiesbaden, stained E. coli suspension (2– 4 ⫻ 106/L) for
tis-related cytokines (tumor necrosis factor Germany), detecting both human and porcine 10 mins at 37°C resulting in a bacteria/
[TNF]-␣, interleukin [IL]-10, and transform- TGF-1. Preliminary experiments had shown neutrophil ratio of 5:1. Fluorescence-activated
ing growth factor [TGF]-1), sieving coeffi- a cross-reactivity of human and recombinant cell-sorter analysis was performed within 60
cients (SC) were calculated with the following porcine TGF-1 of 96% (n ⫽ 5). mins.
equation: SC ⫽ 2 Cf /(Ci ⴙ Co), where Cf, Ci, In Vitro TNF-␣ Production by PMNs. PMNs The assessment of respiratory burst activ-
and Co, respectively, represent concentration were isolated by dextran sedimentation and ity is based on the measurable oxidation of the
in hemofiltrate, concentration in “inflow” Ficoll-Hypaque density gradient sedimenta- substrate dihydrorhodamine (DHR 123) in the
(prefilter), and concentration in “outflow” tion as previously described (22). Cell viability test reflecting the capability of PMNs to gen-
(postfilter) catheters, respectively. was ⬎95% as assessed by trypan blue exclu- erate oxygen radicals. Whole blood samples
Induction of Pancreatitis and Biometric sion. PMNs were incubated in RPMI 1640 me- were activated with 20 ng/mL phorbol myris-
Design. Pancreatitis was induced by pressure- dium (Seromed, Berlin, Germany) supple- tate acetate or formyl-methionyl-leucyl-
controlled (⬍20 mm Hg), intraductal infusion mented with 10% calf serum resulting in a phenylalanine.
of sodium taurocholate (4%, 1 mL/kg BW, final count of 2 ⫻ 106 cells/mL. TNF-␣ con- Statistics. Data are reported as mean ⫾ SD.
Sigma Chemical, Deisenhofen, Germany) and centrations in supernatants were measured af- Survival times were calculated by Kaplan-
enterokinase (2 U/kg BW, Sigma Chemical). ter exposure of suspensions to lipopolysaccha- Meier analysis and compared by the log-rank
Control animals (n ⫽ 12, group 1) underwent ride (5 g/mL Salmonella abortus equi, Sigma test. Differences of baseline values vs. changes
the spontaneous course of the disease without Chemical) for 4 hrs at 37°C. of parameters after pancreatitis were evaluated
1424 Crit Care Med 2001 Vol. 29, No. 7
by analysis of variance for repeated measures. 3: n ⫽ 4; group 4: n ⫽ 8), in definitive CRP concentrations were ⬍8 mg/L. In
Differences between treatment groups were long-term (60 hrs) survival. Both the ini- controls, pancreatitis resulted in a 20-
analyzed by analysis of variance, followed by tial elevation of body temperature up to fold increase in CRP concentrations
the Scheffé test to assess significance. Differ- almost 41°C and the hypothermia in the (baseline: 7.2 ⫾ 4.4 mg/L; 24 hrs postin-
ences in incidences of bacterial growth were
compared using Fisher’s exact test. Correla-
late course of experiments were signifi- duction: 148 ⫾ 31 mg/L). CVVH weak-
tion analysis was performed using the Pearson
cantly ameliorated by CVVH. The change ened distinctly the CRP response. In
correlation method. A p value ⬍ .05 was con- of hemofilters (group 3) and, notably, ad- group 2, this attenuation was only tran-
sidered statistically significant. ditional increase of filtration rate (group sient and CRP levels increased in the later
4) were distinctly superior in preventing course of experiments (48 hrs postinduc-
RESULTS sepsis-related hemodynamic impairment tion: 139 ⫾ 45 mg/L). In groups 3 and 4,
compared with group 2. This resulted in a even 60 hrs postinduction, CRP concen-
Clinical Data. After the onset of pan- definitive prevention of sepsis signs by trations were considerably lower than
creatitis, group 1 (control) animals ex- CVVH in a total of ten animals, seven of those detected 24 hrs postinduction in
hibited an early phase, hyperdynamic re- which belonged to group 4 and three to controls (group 3: 81 ⫾ 31; group 4: 72 ⫾
sponse characterized by increases in CI, group 3. No animals from group 2 sur- 28).
HR (not demonstrated), and body tem- vived.
WBC counts in controls showed a
perature, and decreases in MAP and TPR
characteristic biphasic course with an
(Table 1). In the late phase of septic Laboratory Parameters
macrocirculatory derangements, a dra- early phase increase from 8.2 ⫾ 1.8 ⫻
matic breakdown of the entire macrocir- Lipase, TAP, CRP, and WBC. The ac- 103/L (baseline) to 15.2 ⫾ 4.3 ⫻ 103/L
culation and a decrease in body temper- tivities of lipase in blood serum were be- (24 hrs) preceding severe leukopenia (3.4
ature occurred. The major reason for this low 50 U/L before the induction of pan- ⫾ 1.5 ⫻ 103/L, 36 hrs). Although peak
was a progressive cardiac insufficiency in- creatitis. Slight differences between and nadir values were reached later, the
dicated by a decrease in CI. In treatment groups in the rise of lipase activities up same tendency was observed in group 2
groups, the median time interval after 1500 U/L postinduction were not signifi- (baseline: 7.9 ⫾ 1.5 ⫻ 103/L; 36 hrs:
which animals had to be connected to cant. Comparable findings were observed 14.8 ⫾ 2.0 ⫻ 103/L; 48 hrs: 3.0 ⫾ 1.9 ⫻
CVVH according to the experimental pro- concerning urinary TAP concentrations 103/L). In animals undergoing filter
tocol (decrease in TPR of 30%) was 14.2 increasing from baseline values ⬍1 change, the increase in circulating WBC
hrs (range, 11.4 –16.6 hrs). CVVH led in nmol/L to peak values ⱕ230 nmol/L peaked 48 hrs postinduction (group 3:
all treatment groups to a reversal of he- without considerable differences between 13.9 ⫾ 2.4 ⫻ 103/L; group 4: 13.6 ⫾ 2.6
modynamic impairment that resulted the experimental groups (data not ⫻ 103/L). In group 3, the drop in WBC
eventually in significantly prolonged sur- shown). counts observed at the end of the exper-
vival and, in a total of 12 animals (group Before the induction of pancreatitis, iments was significantly attenuated (6.0
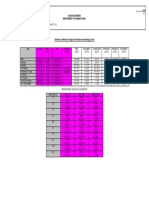
Table 1. Clinical outcome parameters
Parameter Group No. Baseline 12 hrs 24 hrs 36 hrs 48 hrs 60 hrs
Survival rate, % (survivors/ 1 100 100 83 (10/2) 33 (4/8) 0 (0/12) NC
nonsurvivors)
2 100 100 100 (12/0) 67 (8/4) 25 (3/9) 0 (0/12)a
3 100 100 92 (11/1) 92 (11/1) 50 (6/6) 33 (4/8)a,b
4 100 100 100 (12/0) 100 (12/0) 75 (9/3) 67 (8/4)a,b,c
MAP, mm Hg 1 97 ⫾ 12 72 ⫾ 14d 44 ⫾ 21d 36 ⫾ 18 NC NC
2 96 ⫾ 14 68 ⫾ 16d 86 ⫾ 18a 59 ⫾ 17d 40 ⫾ 19d NC
3 101 ⫾ 13 74 ⫾ 13d 85 ⫾ 17a,e 74 ⫾ 16e 62 ⫾ 17b,d 47 ⫾ 18d
4 99 ⫾ 15 71 ⫾ 15d 92 ⫾ 15a 91 ⫾ 18b,c 80 ⫾ 18b,c,d 66 ⫾ 18c,d
CI, L/min䡠m2 1 4.5 ⫾ 1.1 6.2 ⫾ 1.5d 9.8 ⫾ 2.8d 2.8 ⫾ 2.4 NC NC
2 4.2 ⫾ 1.5 6.0 ⫾ 1.4d 6.3 ⫾ 1.7a,d 11.8 ⫾ 2.8d 3.1 ⫾ 2.8 NC
3 4.4 ⫾ 1.2 5.8 ⫾ 1.6d 6.6 ⫾ 1.9a 5.9 ⫾ 2.5b,e 6.0 ⫾ 3.5b,e 7.6 ⫾ 3.7d
4 4.8 ⫾ 1.3 6.5 ⫾ 1.7d 5.9 ⫾ 1.9a,b,e 5.6 ⫾ 2.1b 5.4 ⫾ 2.6b 5.8 ⫾ 3.0c
TPR, dyn䡠sec䡠cm⫺5 1 1875 ⫾ 366 1485 ⫾ 429e 695 ⫾ 291d 574 ⫾ 203d NC NC
2 2025 ⫾ 214 1428 ⫾ 345e 1529 ⫾ 351a,e 820 ⫾ 385d 673 ⫾ 350d NC
3 1942 ⫾ 295 1549 ⫾ 262e 1673 ⫾ 273a 1495 ⫾ 462a,b,e 1148 ⫾ 429b,e 749 ⫾ 376d
4 1815 ⫾ 392 1334 ⫾ 385d 1592 ⫾ 304a 1631 ⫾ 481a,b 1521 ⫾ 458b,c,e 1111 ⫾ 317c,d
BT, °C 1 37.3 ⫾ 0.9 38.4 ⫾ 1.6d 40.9 ⫾ 1.4d 35.4 ⫾ 1.5 NC NC
2 37.0 ⫾ 0.7 38.6 ⫾ 1.2e 37.8 ⫾ 1.5a 39.3 ⫾ 2.1d 35.2 ⫾ 1.4d NC
3 37.5 ⫾ 0.9 38.9 ⫾ 1.3e 37.5 ⫾ 1.7a 37.7 ⫾ 1.3b 37.8 ⫾ 2.0b 37.4 ⫾ 2.9
4 37.2 ⫾ 0.6 38.3 ⫾ 0.9e 37.1 ⫾ 1.4a 37.2 ⫾ 1.5b 37.3 ⫾ 1.5b 38.0 ⫾ 1.9
Survival rates, mean arterial pressure (MAP), cardiac index (CI), total peripheral resistance (TPR), and body temperature (BT) after pancreatitis (mean ⫾
SD). Group 1: controls; group 2: continuous veno-venous hemofiltration (CVVH) without change of hemofilters; group 3: low-volume CVVH (20 mL/kg body
weight [BW]/hr) with change of hemofilters every 12 hrs; group 4: high-volume CVVH (100 mL/kg BW) with change of hemofilters every 12 hrs; NC, not
calculated (no survival).
a
p ⬍ .05 vs. the respective value in controls; bp ⬍ .05 vs. the respective value in group 2; cp ⬍ .05 vs. the respective difference in group 3; dp ⬍ .01
and ep ⬍ .05 vs. baseline values, respectively.
Crit Care Med 2001 Vol. 29, No. 7 1425
⫾ 4.3 ⫻ 103/L); in group 4, WBC counts more effective, increasing the filtration of endotoxin measurements (see below),
remained elevated (11.9 ⫾ 4.3 ⫻ 103/L, rate (group 4), led to an arrest of TNF-␣ the final decrease in TNF-␣ generation in
60 hrs postinduction). The subgroup of response (⬍200 pg/mL) that remained, in groups 1 and 2 suggested endotoxin hy-
nonseptic animals in groups 3 and 4 (n ⫽ contrast to group 2, definitively sup- poresponsiveness. This was either atten-
10) had significantly higher WBC counts pressed compared with peak values in uated or even completely prevented in
than the total of 38 septic animals at the controls. Furthermore, the attenuation of animals undergoing filter change in
last period of individual observation (11.2 TNF-␣ response in treatment groups was groups 3 and 4.
⫾ 4.0 vs. 3.7 ⫾ 3.3 ⫻ 103/L; p ⬍ .01). reciprocally associated with the removal TGF-1 and IL-10. Serum concentra-
TNF-␣. Pancreatitis resulted in a tre- of TNF-␣ in hemofiltrate (R ⫽ ⫺0.83, p tions of TGF-1 (11 ⫾ 7 to 19 ⫾ 8 pg/mL
mendous increase of TNF-␣ concentra- ⫽ .004). Highest hemofiltrate levels of preinduction) peaked 24 hrs postinduc-
tions, peaking 24 hrs postinduction in TNF-␣, and thereby highest sieving coef- tion and ranged from 846 ⫾ 238 (group
controls. The subgroup of four control ficients, were found in group 4 (data not 2) to 1102 ⫾ 415 pg/mL (group 4). In the
animals that were still alive 36 hrs postin- shown). The late-phase decrease in further course, TGF-1 serum levels de-
duction showed a reversal of the serum TNF-␣ serum concentrations in controls creased gradually. Despite considerable
TNF-␣ response (Fig. 1A). CVVH signifi- and, although in a delayed fashion, in removal in hemofiltrate indicated by high
cantly attenuated the increase of TNF-␣ group 2 was consistent with in vitro ex- sieving coefficients (0.51– 0.59) and sig-
levels in serum. In group 2, this effect periments showing progressive decrease nificant gradients of pre- and postfilter
was temporarily limited, resulting in ele- in TNF-␣ generation from isolated, endo- concentrations, TGF-1 levels in CVVH-
vated TNF-␣ levels 36 hrs postinduction. toxin-challenged PMNs in these groups treated groups tended to be rather ele-
Changing hemofilters (group 3) and, (Fig. 1B). Taking into account the results vated when compared with untreated
controls (not significant). IL-10 levels in
controls showed an overwhelming pri-
mary increase, but decreased in the later
course of experiments (Fig. 2). Sieving
coefficients of IL-10 were comparable
with those of TGF-1 (range, 0.48 – 0.55,
24 hrs postinduction). Interestingly, with
more effective IL-10 removal in hemofil-
trate (group 4 ⬎ group 3 ⬎ group 2),
serum IL-10 concentrations increased. In
the late experimental course, long-term
survivors protected from sepsis (n ⫽ 10)
had significantly higher IL-10 levels com-
pared with final values assessed in the
total of 38 septic animals (134 ⫾ 41 vs. 62
⫾ 30 pg/mL; p ⬍ .01).
Microbiology and Endotoxemia. None
of blood and ascites samples collected im-
mediately after instrumentation showed
bacterial growth. The near 100% inci-
dence of positive blood and ascites cul-
tures 24 hrs postinduction in controls
was significantly weakened by CVVH, re-
sulting in positive cultures of 43% of
ascites cultures (15/35) and 31% of blood
cultures (11/35) (p ⬍ .001 vs. controls for
each). High-volume CVVH reduced bac-
teremia better compared with groups 2
and 3 (data not shown). The microbiolog-
ical differentiation revealed a broad spec-
trum of bacteria with slightly elevated
prevalence (not significant) for E. coli,
Morganella morganii, Pseudomonas
aeruginosa, and Gram-negative anaer-
obes (i.e., Bacteroides fragilis). Bacteria
found in positive blood cultures were
without exception simultaneously
Figure 1. Plasma tumor necrosis factor (TNF)-␣ levels (A) and in vitro TNF-␣ generation by endotoxin-
stimulated polymorphonuclear leukocytes (PMNs) obtained at different points of time (B). Definitive present in ascites, too.
protection from overwhelming TNF-␣ response was only achieved by intensified continuous veno- CVVH succeeded in significantly sup-
venous hemofiltration (CVVH). Attenuation of endotoxin hyporesponsiveness was most effective in pressing the considerable increase of en-
animals undergoing high-volume CVVH. LPS, lipopolysaccharide. *p ⬍ .01 vs. 0 hrs; #p ⬍ .05 vs. dotoxin levels (Fig. 3). Both the periodic
control; §p ⬍ .05 vs. group 2; $p ⬍ .05 vs. group 3. change of hemofilters and the increase of
1426 Crit Care Med 2001 Vol. 29, No. 7
Phagocytosis and Oxidative Burst Ac-
tivity in PMNs. PMNs obtained from con-
trols showed initially a marked priming
response (maximum at 24 hrs) for phor-
bol myristate acetate–stimulated oxida-
tive burst activity when compared with
baseline PMNs (Fig. 5A). In contrast,
PMNs obtained at 36 hrs postinduction
demonstrated a breakdown of respiratory
burst orchestrated by decreased phagocy-
tosis of fluorescein isothiocyanate–
stained E. coli. Comparable findings were
observed in group 2 animals, although
both the initial enhancement and end-
stage breakdown of oxidative burst and
Figure 2. Plasma interleukin (IL)-10 concentrations. Continuous veno-venous hemofiltration (CVVH) PMN-related phagocytosis were delayed.
resulted in significantly increased IL-10 levels that peaked 24 hrs postinduction. Intensified CVVH with In animals undergoing intensified CVVH
filtrate turnover of 100 mL/kg body weight/hr arrested IL-10 levels at these levels, whereas those in (groups 3 and 4), this pattern of func-
animals undergoing low filtrate turnover, notably when filters were not changed, decreased in the tional alterations in PMNs was not ob-
further course of the observation period. *p ⬍ .01 vs. 0 hrs; #p ⬍ .05 vs. control; §p ⬍ .05 vs. group served. The change of hemofilters and,
2; $p ⬍ .05 vs. group 3. more effective, the increase of filtration
rate succeeded, in distinct contrast to
group 2, in attenuating the deterioration
of PMN function in the later course of
experiments.
DISCUSSION
Significant evidence has accumulated
from clinical studies suggesting that sec-
ondary multiple organ failure resulting
from septic complications is the cardinal
cause of mortality in severe pancreatitis.
Progress in the field of intensive care
therapy has led to the suggestion that
patients who seem to be at risk to develop
severe, systemic complications after the
onset of pancreatitis might profit from
Figure 3. Plasma endotoxin concentrations. Endotoxin levels surged during the first 24 hrs of the “early” application of CVVH (10). This
study, reaching peak levels by 36 hrs. Increase of endotoxin levels was significantly attenuated by implies a hypothetical indication of CVVH
continuous veno-venous hemofiltration (CVVH). Definitive prevention was only achieved by CVVH irrespective of the presence of acute renal
performed in high-volume modality. *p ⬍ .01 vs. 0 hrs; #p ⬍ .05 vs. control; §p ⬍ .05 vs. group 2; $p failure. The impetus of early application
⬍ .05 vs. group 3. of CVVH in nonanuric patients is thereby
to eliminate overwhelmingly released in-
flammatory mediators supposed to initi-
filtration rate weakened endotoxemia at genic sepsis on MHC class II antigen ex- ate a sequela of pathophysiologic de-
significantly lower levels compared with pression on monocytes are shown in rangements that finally results in sepsis-
group 2. Moreover, maximal endotoxin Figure 4. CVVH was highly effective in induced acute renal failure, uremia, and
levels in the entirety of ten nonseptic delaying or even preventing MHC class II multiple organ failure.
animals from groups 3 and 4 were signif- down-regulation. CD14 down-regulation In the present study, we investigated
icantly lower than those assessed in the on monocytes occurred in a similar fash- whether CVVH, performed in different
total of 38 septic animals (41 ⫾ 18 vs. 79 ion (data not shown). In controls, CD14 modalities, would prevent sepsis-induced
⫾ 27 pg/mL; p ⬍ .05). Preliminary exper- expression decreased from 68% (baseline) derangements following pancreatitis. Be-
iments (n ⫽ 4) performed to explore to 34% (36 hrs postinduction). This ten- cause a model of experimental pancreato-
whether endotoxin would be filtered or dency, which was only delayed in group 2, genic sepsis does not exist, we first estab-
adsorbed by the filter membranes re- was almost completely prevented in lished a new pancreatitis model sharing
vealed that the recovery of exogenous en- group 4 animals (baseline: 65%; 60 hrs many parallels with severe human pan-
dotoxin (5 g/mL) was ⬎90%. Also, en- postinduction: 54%). Moreover, a signif- creatitis, e.g., the nonbacterial onset of
dotoxin was not detectable in any of the icant, reciprocal correlation of CD14 the disease preceding secondary bacterial
hemofiltrate samples. down-regulation on monocytes and the translocation and endotoxemia, a hyper-
Changes in Leukocyte Immunophe- degree of endotoxemia was found (R ⫽ dynamic circulatory response, and char-
notypes. The adverse effects of pancreato- ⫺0.82, p ⫽ .007). acteristic laboratory and immunologic
Crit Care Med 2001 Vol. 29, No. 7 1427
C
ontinuous veno-
venous hemofil-
tration distinctly
improved outcome and de-
layed occurrence of sepsis in
experimental pancreato-
genic sepsis.
Figure 4. Major histocompatibility complex (MHC) II antigen expression in monocytes assessed by flow
cytometry. A total of 15,000 cells were analyzed for each sample. Down-regulation of MHC II
direct correlation between cumulative ul-
expression ⬍40% compared with baseline values indicating severe immunoparalysis occurred in
controls and, although being significantly delayed, in group 2 animals undergoing continuous
trafiltrate volume and survival rate in pa-
veno-venous hemofiltration (CVVH) without filter change. This was significantly improved when filters tients with sepsis-associated acute renal
were periodically changed. In animals undergoing high-volume CVVH (group 4), MHC II expression failure (15), we report significantly im-
was arrested at approximately control levels. *p ⬍ .05 vs. 0 hrs; #p ⬍ .05 vs. control; §p ⬍ .05 vs. group proved outcome and even considerable
2. long-term survival in animals undergo-
ing high-volume CVVH representing the
most intensified treatment modality per-
formed in this study. Furthermore, our
data provide evidence for a linkage be-
tween duration of filter application and
efficiency of CVVH. Although it has been
previously hypothesized that there may
be a need for periodic changes of hemo-
filters to prevent progressive loss of effi-
cacy of CVVH (13), this assumption has
not been proven in clinical or experimen-
tal studies to date. The significant im-
provement of outcome in animals under-
going filter change identifies the
prevention of filter “fouling,” in addition
to a sufficient filtration rate, as a second,
mandatory requirement for the efficacy of
CVVH.
The observation that both the eleva-
tion of CRP concentrations in plasma and
alterations of WBC counts were signifi-
cantly suppressed by CVVH is of great
importance because it reflects the capa-
bility of CVVH in attenuating the sys-
temic inflammatory response in the
course of pancreatitis. With regard to leu-
kocyte function, this attenuation was
Figure 5. Oxidative burst (A) assessed by oxidation of dihydrorhodamine 123 to rhodamine 123 by eventually orchestrated by improvement
polymorphonuclear leukocytes (PMNs) activated with 20 ng/mL phorbol myristate acetate (PMA) and of both oxidative burst and phagocytosis
phagocytosis capacity (B) for opsonized, fluorescein isothiocyanate–stained Escherichia coli (E. coli) capacity in PMNs. In contrast, CVVH did
(2– 4 ⫻ 106/L) in PMNs detected by flow cytometry (15,000 cells). The biphasic pattern of oxidative not have any impact on urinary TAP lev-
burst in response to PMA in controls and group 2 was attenuated by intensified continuous veno- els assayed as a parameter for pancreatic
venous hemofiltration (CVVH). Comparably, phagocytosis was arrested near baseline levels in animals necrosis and, therefore, being helpful in
undergoing high-volume CVVH, whereas low-volume CVVH was less effective, notably when filters re-
predicting the local severity of acute pan-
mained unchanged. *p ⬍ .05 vs. 0 hrs; #p ⬍ .05 vs. control; §p ⬍ .05 vs. group 2; $p ⬍ .05 vs. group 3.
creatitis (23, 24).
Previous studies suggest that the local
features found frequently in clinical sep- icantly more effective prevention of sep- pancreatic damage triggers the release of
sis. sis-related hemodynamic deterioration both proinflammatory (TNF-␣) and anti-
Of particular interest is the finding than does low-volume CVVH. In accor- inflammatory (IL-10 and TGF-) cyto-
that high-volume CVVH results in signif- dance with clinical studies suggesting a kines in the course of the disease (25).
1428 Crit Care Med 2001 Vol. 29, No. 7
TNF-␣ is known to be of crucial impor- CD14. CVVH delayed, in instances of sep- modulation. Gastroenterology 1996; 110:
tance in mediating systemic effects of sis protection over the whole observation 583–588
septic diseases, e.g., necrotizing pancre- period, and even definitively suppressed 2. Norman J, Franz M, Messina J, et al: Inter-
atitis. It was of striking interest that the down-regulation of MHC II known to oc- leukin-1 receptor antagonist decreases sever-
ity of acute experimental pancreatitis.
potential of CVVH in decreasing TNF-␣ cur in fatal, sepsis-induced immunopa-
Surgery 1994; 117:648 – 655
levels was temporarily limited when only ralysis (29 –32). In accord with studies
3. Heath DL, Cruickshank DH, Gudgeon M, et
one filter was used, whereas periodic fil- reporting a reduction of CD14 receptor al: Role of interleukin-6 in mediating the
ter change as well as the increase in density during sepsis (33), CVVH also at- acute phase protein response and potential as
plasma turnover prevented excessive tenuated CD14 down-regulation as long an early means in acute pancreatitis.
TNF-␣ levels more effectively. Also, the as it prevented sepsis. Most interestingly, Pancreas 1993; 66:41– 45
drop in TNF-␣ concentrations to near the latter finding was obviously the result 4. Gross V, Andreesen R, Leser HG, et al: Inter-
control levels in advanced sepsis was ab- of the close, reciprocal association of leukin-8 and neutrophil activation in acute
sent in nonseptic animals, most of which CD14 down-regulation with the extent of pancreatitis. Eur J Clin Invest 1992; 22:
were treated by intensified, high-volume endotoxemia. 200 –203
CVVH. In contrast, sepsis prevention was Finally, CVVH obviously improved the 5. Richter A, Nebe T, Kattermann R, et al: Im-
associated with an arrest of TNF-␣ re- mucosa barrier and thereby restrained both mune paralysis in acute pancreatitis—
sponse at elevated levels. This seemed to endotoxemia and bacteremia. This was HLA-DR antigen expression on CD14⫹DR⫹
monocytes. Langenbecks Arch Chir 1996;
be paradoxic, as the final, sepsis-related caused by mechanisms different from filtra-
381:38 – 41
TNF-␣ decrease was orchestrated by sig- tion/adsorption processes as evidenced, 6. Widdison AL, Karanjia ND, Alvarez C, et al:
nificantly higher endotoxin levels than first, by the finding that in no hemofiltrate Reticuloendothelial function and efficacy of
those in nonseptic animals. As endotoxin sample endotoxin was detectable. Further- levamisole for the treatment of pancreatic
is known to be one of the major stimula- more, preliminary experiments had re- infection in acute necrotizing pancreatitis.
tors of TNF-␣ generation, the dissocia- vealed that the filters used in our setting Am J Surg 1992; 163:100 –104
tion of TNF-␣ decrease and exorbitant are not able to remove endotoxin. The find- 7. Gotloib L, Barzilay E, Shustak A, et al: He-
endotoxin levels therefore suggested en- ing that bacteria assessed in positive blood mofiltration in septic ARDS. The artificial
dotoxin hyporesponsiveness in advanced cultures were, without exception, also kidney as an artificial endocrine lung.
sepsis. This assumption was strengthened present in ascites suggests that CVVH, by Resuscitation 1986; 13:123–132
by in vitro experiments showing sepsis- improving splanchnic perfusion, protects 8. Gomez A, Wang R, Unruh H, et al: Hemofil-
induced, disturbed TNF-␣ generation by the bloodstream from bacterial invasion tration reverses left ventricular dysfunction
during sepsis in dogs. Anesthesiology 1990;
PMNs subjected to exogenous endotoxin. from the abdominal cavity.
73:671– 685
CVVH attenuated or completely pre-
In summary, CVVH distinctly im- 9. Blinzler L, Hausser J, Bödeker H, et al: Con-
vented disturbed TNF-␣ generation in en- servative treatment of severe necrotizing
dotoxin-stimulated PMNs. proved outcome and delayed occur-
pancreatitis using early continuous veno-
Moreover, CVVH had considerable ef- rence of sepsis in experimental pancre-
venous hemofiltration. Contrib Nephrol
fects on serum levels of the anti-inflamma- atogenic sepsis. Intensifying CVVH by
1991; 93:234 –236
tory cytokines IL-10 and TGF-. Numerous periodically changing hemofilters and 10. Gebhardt C, Bödeker H, Blinzler L, et al:
reports underline the role of anti-inflam- increasing filtration rate resulted in Wandel in der Therapie der schweren akuten
matory cytokines, notably of IL-10, in both considerable sepsis protection and Pankreatitis. Chirurg 1994; 65:33– 41
sepsis and pancreatitis (25–28). In the long-term survival. These findings 11. Lee PA, Matson JR, Pryor RW, et al: Con-
present series, IL-10 and TGF- levels mea- identify both the integrity of filter tinuos arteriovenous hemofiltration therapy
sured in controls and CVVH-treated ani- membranes and a sufficient filtration for Staphylococcus aureus-induced septice-
mals developing sepsis showed a character- rate to be essential for the efficiency of mia in immature swine. Crit Care Med 1993;
CVVH. These results beg further exam- 21:914 –924
istic biphasic course: after an
ination in a prospective, clinical trial. 12. Bellomo R, Tipping P, Boyce N: Continuous
overwhelming primary response, serum veno-venous hemofiltration with dialysis re-
levels approximated baseline levels in the However, as most patients recover
spontaneously without interventional moves cytokines from the circulation of sep-
later course of sepsis. In contrast, animals tic patients. Crit Care Med 1993; 21:522–526
protected from sepsis by CVVH showed nei- and/or surgical treatments, the “pro-
13. Ronco C, Tetta C, Lupi A, et al: Removal of
ther this exorbitant primary increase nor a phylactic” application of CVVH in all platelet-activating factor in experimental
final drop in IL-10 and TGF- levels. Also, patients suffering from pancreatitis continuous arteriovenous hemofiltration.
in nonseptic animals, IL-10 and TGF- cannot be recommended. Evidence for Crit Care Med 1995; 23:99 –107
were removed from hemofiltrate in higher necrosis and clinical signs of a septic 14. Yekebas EF, Treede H, Knoefel WT, et al:
concentrations than in septic animals. course of the disease might be suitable Influence of zero-balanced hemofiltration on
Hence, we assume that CVVH restrained tools to discriminate patients who the course of severe experimental pancreati-
up-regulated anti-inflammatory cytokine might profit from CVVH from those in tis in pigs. Ann Surg 1999; 229:514 –522
response as long as it prevented sepsis. whom it would represent overtreat- 15. Storck M, Hartl WH, Zimmerer E, et al:
ment. Comparison of pump-driven and spontane-
Further evidence that CVVH improved
ous continuous haemofiltration in postoper-
immunologic alterations was obtained ative acute renal failure. Lancet 1991; 337:
from the screening of monocyte activa- REFERENCES 452– 455
tion markers. We particularly focused on 16. Kono K, Serikawa T, Matsumoto Y: Influence
the expression of the MHC II antigen 1. Curley P, Nestor M, Collins K, et al: De- of surgical stress on monocytes and compli-
corresponding to human leukocyte anti- creased interleukin-2 production in murine cations of infection in patients with esopha-
gen-DR and the endotoxin receptor acute pancreatitis: potential for immuno- geal cancer—monocyte HLA-DR antigen ex-
Crit Care Med 2001 Vol. 29, No. 7 1429
pression and respiratory burst capacity. 22. Boyum A: Isolation of mononuclear cells and rine experimental pancreatitis. Gastroenter-
J Surg Res 1995; 58:275–280 granulocytes from human blood. Scand ology 1995; 108:1917–1922
17. Windsor ACJ, Walsh CJ, Mullen PG, et al: J Clin Lab Invest 1968; 97:77– 89 29. Hershman MJ, Cheadle WG, Wellhausen SR,
Tumor necrosis factor-␣ blockade prevents 23. Karanjia ND, Widdison AL, Jehanli A, et al: et al: Monocyte HLA-DR antigen expression
neutrophil CD18 receptor upregulation and Assay of trypsinogen activation in the cat characterizes clinical outcome in the trauma
attenuates acute lung injury in porcine sep- experimental model of acute pancreatitis. patient. Br J Surg 1990; 77:204 –207
sis without inhibition of neutrophil oxygen Pancreas 1993; 8:189 –195 30. Birkenmaier C, Hong YS, Horn JK: Modula-
radical generation. J Clin Invest 1993; 91: 24. Gudgeon AM, Heath DI, Hurley P, et al: tion of the endotoxin receptor (CD14) in sep-
1459 –1468 Trypsinogen activation peptides assay in the tic patients. J Trauma 1991; 32:473– 479
18. American College of Chest Physicians/ early prediction of severity of acute pancre- 31. Lin RY, Astiz ME, Saxon JC, et al: Altered
Society of Critical Care Medicine Consensus
atitis. Lancet 1990; 335:4 – 8 leukocyte immunophenotypes in septic
Conference: Definition for sepsis and organ
25. Kusske AM, Rongione AJ, Ashley SW, et al: shock. Studies of HLA-DR, CD11b, CD14,
failure and guidelines for the use of innova-
Interleukin 10 (IL-10) prevents death in le- and IL-2R expression. Chest 1993; 104:
tive therapies in sepsis. Crit Care Med 1992;
thal necrotizing pancreatitis in mice. Sur- 847– 853
1992:20:864 – 874
gery 1996; 120:284 –288 32. Volk HD, Reinke P, Krausch D, et al: Mono-
19. Bone RC: Toward an epidemiology and nat-
ural history of SIRS (systemic inflammatory 26. Bean AGD, Freiberg RA, Andrade S, et al: cyte deactivation—Rationale for a new ther-
response syndrome). JAMA 1992; 268: Interleukin 10 protects mice against staphy- apeutic strategy in sepsis. Intensive Care
3452–3455 lococcal enterotoxin B-induced lethal shock. Med 1996; 22:474 – 481
20. Schroedl W: Diagnostische Verwendbarkeit Infect Immun 1993; 61:4937– 4939 33. Larsen NE, Sullivan R: Interaction between
ausgewählter immunologischer Parameter 27. Howard M, Muchamel T, Andrade S, et al: endotoxin and human monocytes: Charac-
in Seren von Schweinen und Pferden. Doc- Interleukin 10 protects mice from lethal teristics of the binding of 3H-labeled lipo-
toral thesis. University of Leipzig, Leipzig, endotoxaemia. J Exp Med 1993; 177: polysaccharide and 51C-labeled lipid A before
Germany, 1994. 1205–1208 and after the induction of endotoxin toler-
21. Murtaugh MP: Porcine cytokines. Vet Immu- 28. Van Laethem JV, Marchant A, Delvaux A, et ance. Proc Natl Acad Sci U S A 1984; 81:
nol Immunopathol 1994; 43:37– 44 al: Interleukin 10 prevents necrosis in mu- 3491–3495
1430 Crit Care Med 2001 Vol. 29, No. 7
You might also like
- Thomas' Hematopoietic Cell Transplantation: Stem Cell TransplantationFrom EverandThomas' Hematopoietic Cell Transplantation: Stem Cell TransplantationStephen J. FormanNo ratings yet
- Physicians Approach to Biotoxin IllnessDocument81 pagesPhysicians Approach to Biotoxin IllnessCody ThomasNo ratings yet
- Oet Test Material: Occupational English Test Reading Sub-Test NursingDocument13 pagesOet Test Material: Occupational English Test Reading Sub-Test NursingRyu Tse33% (3)
- Non Hodgkin LymphomaDocument37 pagesNon Hodgkin LymphomaYulanda Gusti CibiNo ratings yet
- Jci Ssi ToolkitDocument191 pagesJci Ssi ToolkitMr. Jonathan Hudson O.T. Manager, Justice K.S. Hegde Charitable Hospital100% (3)
- CYTOKINESDocument31 pagesCYTOKINESSaifi Alam100% (4)
- Psychoneuroimmunology PDFDocument10 pagesPsychoneuroimmunology PDFRatu Nurul FadhilahNo ratings yet
- Immunology MCQ DrNaeem PDFDocument163 pagesImmunology MCQ DrNaeem PDFA-Naeem To'mah Al-sawaieNo ratings yet
- Quantifying The Clinical Virulence of Klebsiella Pneumoniae Producing Carbapenemase Klebsiella Pneumoniae With A Galleria Mellonella Model and A Pilot Study To Translate To Patient OutcomesDocument10 pagesQuantifying The Clinical Virulence of Klebsiella Pneumoniae Producing Carbapenemase Klebsiella Pneumoniae With A Galleria Mellonella Model and A Pilot Study To Translate To Patient OutcomesJuwita PratiwiNo ratings yet
- Nebulized Colistin in The Treatment of Pneumonia Due To Multidrug-Resistant Acinetobacter Baumannii and Pseudomonas AeruginosaDocument4 pagesNebulized Colistin in The Treatment of Pneumonia Due To Multidrug-Resistant Acinetobacter Baumannii and Pseudomonas AeruginosaPhan Tấn TàiNo ratings yet
- Cytomegalovirus:: Clinical Virological Correlations in Renal Transplant RecipientsDocument10 pagesCytomegalovirus:: Clinical Virological Correlations in Renal Transplant RecipientsRaffaharianggaraNo ratings yet
- TMP C0 BADocument12 pagesTMP C0 BAFrontiersNo ratings yet
- Gu2014 Article AllogeneicMesenchymalStemCellTDocument9 pagesGu2014 Article AllogeneicMesenchymalStemCellTLily ChandraNo ratings yet
- Pi Is 1083879118313909Document2 pagesPi Is 1083879118313909Ljc JaslinNo ratings yet
- 2 Koldehoff 2004Document5 pages2 Koldehoff 2004Sergio SampaioNo ratings yet
- Clinical Review: Blood Purifi Cation For SepsisDocument10 pagesClinical Review: Blood Purifi Cation For SepsisVlady78No ratings yet
- Journal SDocument6 pagesJournal SLyla SandyNo ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- Severe Systemic Cytomegalovirus Infection in An Immunocompetent Patient Outside The Intensive Care Unit: A Case ReportDocument4 pagesSevere Systemic Cytomegalovirus Infection in An Immunocompetent Patient Outside The Intensive Care Unit: A Case ReportSebastián Garay HuertasNo ratings yet
- 0300060520925693Document11 pages0300060520925693Narjes Sharif AskariNo ratings yet
- Braz Jr. Infect Dis 2021Document4 pagesBraz Jr. Infect Dis 2021cdsaludNo ratings yet
- Mannose-Binding Lectin Levels and Variation During Invasive CandidiasisDocument7 pagesMannose-Binding Lectin Levels and Variation During Invasive CandidiasisNaili N S NuhriawangsaNo ratings yet
- Mesothelioma Environment Comprises Cytokines and T-Regulatory Cells That Suppress Immune ResponsesDocument10 pagesMesothelioma Environment Comprises Cytokines and T-Regulatory Cells That Suppress Immune ResponseshariompriyNo ratings yet
- 8 Pathogenesis of Viral HepatitisDocument5 pages8 Pathogenesis of Viral HepatitisMedhumanNo ratings yet
- Jiao PDFDocument7 pagesJiao PDFRodrigo GarciaNo ratings yet
- Maggi 1999Document7 pagesMaggi 1999Araceli Enríquez OvandoNo ratings yet
- Klebsiella Pneumoniae ThesisDocument6 pagesKlebsiella Pneumoniae Thesisaprillaceyjackson100% (1)
- Hep 510240406Document6 pagesHep 510240406Faisal JamshedNo ratings yet
- Sun 2012Document6 pagesSun 2012ntnquynhproNo ratings yet
- Fine-Needle Aspiration Evaluation of Lymphoproliferative Lesions in Human Immunodeficiency Virus-Positive PatientsDocument11 pagesFine-Needle Aspiration Evaluation of Lymphoproliferative Lesions in Human Immunodeficiency Virus-Positive PatientsNidhi JaisNo ratings yet
- Chaves 2005 PDFDocument5 pagesChaves 2005 PDFWa Nur Arlin RahmadhantyNo ratings yet
- A Novel Oncolytic Viral Therapy and Imaging Technique For Gastric Cancer Using A Genetically Engineered Vaccinia Virus Carrying The Human Sodium Iodide SymporterDocument7 pagesA Novel Oncolytic Viral Therapy and Imaging Technique For Gastric Cancer Using A Genetically Engineered Vaccinia Virus Carrying The Human Sodium Iodide SymporterkNo ratings yet
- Cytomegalovirus Triggering Autoimmune Hepatitis: Case Report and Literature ReviewDocument3 pagesCytomegalovirus Triggering Autoimmune Hepatitis: Case Report and Literature ReviewRabiatul 'raney' AdawiyahNo ratings yet
- Application of Real-Time PCR For Determination of Antiviral Drug Susceptibility of Herpes Simplex VirusDocument5 pagesApplication of Real-Time PCR For Determination of Antiviral Drug Susceptibility of Herpes Simplex VirusMinh TriếtNo ratings yet
- Alloimmunization To Red Blood Cell Antigens After Universal Leucodepletion. A Regional Multicentre Retrospective StudyDocument6 pagesAlloimmunization To Red Blood Cell Antigens After Universal Leucodepletion. A Regional Multicentre Retrospective Studymy accountNo ratings yet
- Serum Procalcitonin Levels in Bacterial and Abacterial MeningitisDocument5 pagesSerum Procalcitonin Levels in Bacterial and Abacterial MeningitisSaul Gonzalez HernandezNo ratings yet
- High Rates of Resistance To Cephalosporins Among Viridans-Group Streptococci Causing Bacteraemia in Neutropenic Cancer PatientsDocument6 pagesHigh Rates of Resistance To Cephalosporins Among Viridans-Group Streptococci Causing Bacteraemia in Neutropenic Cancer PatientsJohnree A. EvangelistaNo ratings yet
- White Paper CPD Sepsis AJCP 2005Document5 pagesWhite Paper CPD Sepsis AJCP 2005jtmchughNo ratings yet
- Fulminant Hemophagocytic Lymphohistiocytosis Induced by Pandemic A (H1N1) Influenza: A Case ReportDocument4 pagesFulminant Hemophagocytic Lymphohistiocytosis Induced by Pandemic A (H1N1) Influenza: A Case ReportrahNo ratings yet
- 2023_Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage_ A Dose-Escalation Safety and Tolerability TrialDocument11 pages2023_Mesenchymal Stem Cell Therapy in Acute Intracerebral Hemorrhage_ A Dose-Escalation Safety and Tolerability TrialOlga Manco GuzmánNo ratings yet
- A Review of GM-CSF Therapy in Sepsis: S R M - ADocument10 pagesA Review of GM-CSF Therapy in Sepsis: S R M - AAnonymous SMLzNANo ratings yet
- Kjuo009 02 03Document7 pagesKjuo009 02 03Gambit Marvel FanNo ratings yet
- Human Immunodeficiency Virus Jejunal Enteropathy Associated WithDocument8 pagesHuman Immunodeficiency Virus Jejunal Enteropathy Associated Withihatecrooks8308No ratings yet
- COHORT - TB MenigealDocument11 pagesCOHORT - TB MenigealYA MAAPNo ratings yet
- Risk Factors of Cytomegalovirus Reactivation in UlcerativeDocument15 pagesRisk Factors of Cytomegalovirus Reactivation in UlcerativeNatalyFuertesNo ratings yet
- Influenzae, and Streptococcus Pneumoniae in Suspected CasesDocument6 pagesInfluenzae, and Streptococcus Pneumoniae in Suspected CasesMatiasNo ratings yet
- Jhe2021 6455659Document5 pagesJhe2021 6455659Septi MuninggarNo ratings yet
- Clinical Relevance and Contemporary Methods For Counting Blood Cells in Body Fluids Suspected of Inflammatory DiseaseDocument18 pagesClinical Relevance and Contemporary Methods For Counting Blood Cells in Body Fluids Suspected of Inflammatory DiseaseVanessa Diez de Medina GarcíaNo ratings yet
- Arthritis Rheumatism - 2002 - Houssiau - Immunosuppressive Therapy in Lupus Nephritis The Euro Lupus Nephritis Trial A (1) - 220727 - 183333Document11 pagesArthritis Rheumatism - 2002 - Houssiau - Immunosuppressive Therapy in Lupus Nephritis The Euro Lupus Nephritis Trial A (1) - 220727 - 183333HPNo ratings yet
- Catater Ventriuclar Impregndados en Ab Sep 2010Document6 pagesCatater Ventriuclar Impregndados en Ab Sep 2010Felipe Anduquia GarayNo ratings yet
- Hep Chiv Renal DZDocument9 pagesHep Chiv Renal DZSundar RamanathanNo ratings yet
- 2011 Koc - MPV InflameDocument4 pages2011 Koc - MPV Inflamenermal93No ratings yet
- Tosca 1996Document7 pagesTosca 1996HEARTJUGGLERNo ratings yet
- Successful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolDocument2 pagesSuccessful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolHawin NurdianaNo ratings yet
- Sakka TherapyDocument2 pagesSakka TherapyMohammed Khair BashirNo ratings yet
- Changes in the co-expressions of interleukin 29 (IL-29), IFN-inducible protein 10 (IP-10) and monokine induced by IFNγ (MIG) genes in chronic hepatitis C Egyptian patients untreated and treated with DAAsDocument8 pagesChanges in the co-expressions of interleukin 29 (IL-29), IFN-inducible protein 10 (IP-10) and monokine induced by IFNγ (MIG) genes in chronic hepatitis C Egyptian patients untreated and treated with DAAsAhmed AmerNo ratings yet
- Practice Guidelines For The Diagnosis and Management of Skin and Soft-Tissue InfectionsDocument34 pagesPractice Guidelines For The Diagnosis and Management of Skin and Soft-Tissue InfectionsNatalia MoranNo ratings yet
- Journal Club Terapia Con Células T Del Receptor de Antígeno Quimérico anti-CD19 para El Lupus Eritematoso Sistémico RefractarioDocument5 pagesJournal Club Terapia Con Células T Del Receptor de Antígeno Quimérico anti-CD19 para El Lupus Eritematoso Sistémico RefractarioCristhian RodriguezNo ratings yet
- First - in - Man Observation of Talaromyces Marneffei-Transmission by Organ TransplantationDocument5 pagesFirst - in - Man Observation of Talaromyces Marneffei-Transmission by Organ TransplantationAnonymous oQtve4oNo ratings yet
- Human Infection With Delftia Tsuruhatensis Isolated From A Central Venous CatheterDocument3 pagesHuman Infection With Delftia Tsuruhatensis Isolated From A Central Venous CatheterRENE RIVASNo ratings yet
- Rheumatology-2014-Liu-rheumatology-keu316 HormonaDocument11 pagesRheumatology-2014-Liu-rheumatology-keu316 HormonaBluna0291No ratings yet
- 3 Saritanayak EtalDocument7 pages3 Saritanayak EtaleditorijmrhsNo ratings yet
- Rodolfo TI 2022Document8 pagesRodolfo TI 2022rodolfodepaulavieiraNo ratings yet
- VasculitisDocument12 pagesVasculitisMaite OrellanaNo ratings yet
- Sepsis - Eval and MGMTDocument62 pagesSepsis - Eval and MGMTDr Ankit SharmaNo ratings yet
- Infections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumFrom EverandInfections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumNo ratings yet
- Tectonic Plates (Grade 8)Document2 pagesTectonic Plates (Grade 8)manuelantoniomenaNo ratings yet
- Prime Numbers PDFDocument1 pagePrime Numbers PDFmanuelantoniomenaNo ratings yet
- Adding Decimals: Instructions: Find The SumDocument2 pagesAdding Decimals: Instructions: Find The SummanuelantoniomenaNo ratings yet
- Travelmate 6592 6592gDocument148 pagesTravelmate 6592 6592gmanuelantoniomenaNo ratings yet
- Algebraic TerminologyDocument1 pageAlgebraic TerminologymanuelantoniomenaNo ratings yet
- Time Kids 1 PDFDocument4 pagesTime Kids 1 PDFmanuelantoniomenaNo ratings yet
- Travelmate 6592 6592gDocument148 pagesTravelmate 6592 6592gmanuelantoniomenaNo ratings yet
- Uno r3 Driver FaqDocument13 pagesUno r3 Driver FaqazuldevoNo ratings yet
- Algebraic TerminologyDocument1 pageAlgebraic TerminologymanuelantoniomenaNo ratings yet
- Multiplying and Dividing FractionsDocument4 pagesMultiplying and Dividing FractionsmanuelantoniomenaNo ratings yet
- Time Kids 1Document4 pagesTime Kids 1manuelantoniomenaNo ratings yet
- What Time Is ItDocument4 pagesWhat Time Is ItmanuelantoniomenaNo ratings yet
- Diving by 2-Digit Numbers - Word Problems (Document2 pagesDiving by 2-Digit Numbers - Word Problems (manuelantoniomenaNo ratings yet
- Multiplying and Dividing Decimals To HundredthsDocument6 pagesMultiplying and Dividing Decimals To HundredthsmanuelantoniomenaNo ratings yet
- Numerical Expression Word ProblemsDocument3 pagesNumerical Expression Word ProblemsmanuelantoniomenaNo ratings yet
- Number & Operations in Base Ten Review - Grade 5Document8 pagesNumber & Operations in Base Ten Review - Grade 5manuelantoniomenaNo ratings yet
- Problem Solving With Negative NumbersDocument2 pagesProblem Solving With Negative NumbersmanuelantoniomenaNo ratings yet
- PercentsDocument3 pagesPercentsmanuelantoniomenaNo ratings yet
- Prime Numbers PDFDocument1 pagePrime Numbers PDFmanuelantoniomenaNo ratings yet
- Prime NumbersDocument1 pagePrime NumbersmanuelantoniomenaNo ratings yet
- Prime Numbers PDFDocument1 pagePrime Numbers PDFmanuelantoniomenaNo ratings yet
- Proportions: Instructions: Solve Each ProportionDocument1 pageProportions: Instructions: Solve Each ProportionmanuelantoniomenaNo ratings yet
- Long Division: Instructions: Solve The Division Problems Below. Show The Remainder If There Is OneDocument2 pagesLong Division: Instructions: Solve The Division Problems Below. Show The Remainder If There Is OnemanuelantoniomenaNo ratings yet
- Positive and Negative Number CalculationsDocument2 pagesPositive and Negative Number CalculationsmanuelantoniomenaNo ratings yet
- Adding Decimals: Instructions: Find The SumDocument2 pagesAdding Decimals: Instructions: Find The SummanuelantoniomenaNo ratings yet
- Identifying Number PropertiesDocument2 pagesIdentifying Number PropertiesmanuelantoniomenaNo ratings yet
- Long Division: Instructions: Solve The Division Problems Below. Show The Remainder If There Is OneDocument2 pagesLong Division: Instructions: Solve The Division Problems Below. Show The Remainder If There Is OnemanuelantoniomenaNo ratings yet
- Identifying Number PropertiesDocument2 pagesIdentifying Number PropertiesmanuelantoniomenaNo ratings yet
- Adding Decimals: Instructions: Find The SumDocument2 pagesAdding Decimals: Instructions: Find The SummanuelantoniomenaNo ratings yet
- Lypm Immunity SystemDocument22 pagesLypm Immunity SystemPhoenix JudgeNo ratings yet
- Mcqs - Biochemistry - Immune Response - PFMSG ForumDocument4 pagesMcqs - Biochemistry - Immune Response - PFMSG ForumDillu SahuNo ratings yet
- Vaccination Preference of Philippines Position PaperDocument3 pagesVaccination Preference of Philippines Position PaperJuan Leandro MaglonzoNo ratings yet
- Vaccination in PregnancyDocument7 pagesVaccination in PregnancyNoraNo ratings yet
- Stage One: 2020/2019: Leukopenia: Symptoms, Causes, and TreatmentDocument5 pagesStage One: 2020/2019: Leukopenia: Symptoms, Causes, and Treatmentعـَــٻاس مَـــشتاق عـَــليNo ratings yet
- BSC BioinformaticsDocument31 pagesBSC BioinformaticsAjay KumarNo ratings yet
- Human Histology Midterms: Blood and HemopoesisDocument3 pagesHuman Histology Midterms: Blood and Hemopoesisabi dimatulacNo ratings yet
- 201227 박사학위논문 서슬아 수정Document166 pages201227 박사학위논문 서슬아 수정Quynh NguyenNo ratings yet
- Complement Fixation Test (CFT) : Microbiology PharmacyDocument11 pagesComplement Fixation Test (CFT) : Microbiology PharmacyAisya Amalia MuslimaNo ratings yet
- Uncovering the mystery behind the coronavirus pandemicDocument7 pagesUncovering the mystery behind the coronavirus pandemickim VERGARANo ratings yet
- Inhibitory B7 Family Molecules in Tumour MicroenvironmentDocument12 pagesInhibitory B7 Family Molecules in Tumour MicroenvironmentJoanne LeungNo ratings yet
- Microbiology (M.SC II) - 05092022Document80 pagesMicrobiology (M.SC II) - 05092022RohittitansinghNo ratings yet
- Steel connection analysisDocument7 pagesSteel connection analysisErick HurtadoNo ratings yet
- Enterotoxin-Producing Staphylococcus AureusDocument17 pagesEnterotoxin-Producing Staphylococcus Aureusvignesh9489No ratings yet
- Engineered Antibodies for Disease TreatmentDocument14 pagesEngineered Antibodies for Disease TreatmentJholina Aure ReyesNo ratings yet
- Childrens FBC Reference Ranges PDFDocument1 pageChildrens FBC Reference Ranges PDFCerianne BodionganNo ratings yet
- BVSC & AH - SyllabusDocument36 pagesBVSC & AH - SyllabusAnomalous suriya addictzNo ratings yet
- Malignant LymphomaDocument3 pagesMalignant LymphomaKakaa KakaNo ratings yet
- Bisc 1111 Introductory Biology - Cells and MoleculesDocument4 pagesBisc 1111 Introductory Biology - Cells and MoleculesKarthik S. IyerNo ratings yet
- Potential Benefits and Challenges of MRNA Cancer VaccinesDocument3 pagesPotential Benefits and Challenges of MRNA Cancer VaccinesAthenaeum Scientific PublishersNo ratings yet
- Biochemistry syllabusDocument3 pagesBiochemistry syllabusSATISH SINGHNo ratings yet
- Clinical Case Studies: Interpretation Guide 5-DIFF Hematology AnalyzersDocument48 pagesClinical Case Studies: Interpretation Guide 5-DIFF Hematology Analyzersnurliah armandNo ratings yet
- Unit 11 Human Body PPTDocument34 pagesUnit 11 Human Body PPTEllhai Caliwan100% (1)