Professional Documents
Culture Documents
Acute Periodontal Conditions: Sheet 11
Acute Periodontal Conditions: Sheet 11
Uploaded by
Jwana MahafzaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Periodontal Conditions: Sheet 11
Acute Periodontal Conditions: Sheet 11
Uploaded by
Jwana MahafzaCopyright:
Available Formats
• Sudden onset Present diagnostic problems to the
clinician.
• Limited duration
Sheet 11: Acute Periodontal Conditions
• Well defined clinical criteria
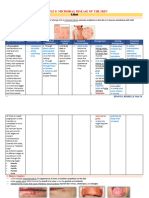
Causes of gingival Subtypes Clinical Causes Manegment Extra notes
& periodontal acute presentation
lesions:
1. Traumatic a) Physical* -keratosis - chronic forceful 1. Remove the cause. -taking good history is
Lesions (chronic) brushing 2. Mild mouthwashes. very important
- Factitious nail 3. Topical remedies. (Oragel
biting habit ,Sulcoseryl and Orabase)
b) Thermal - flat erythematous - burn They only cover the ulcers and
area (desquamated promote healing.
tissue). 4. Secondary infection
antibacterial mouthwashes.
c) Chemical - Aspirin
2. Infectious a) Viral - Ulcers that present - Primary herpetic Subsides within 4-5 days -The recurrent herpes in
as vesicles gingivostomatitis. - if there’s fever/malaise a severe form happens
lesions usually after tiring
- red lesions on - The recurrent Provides the pt supportive
gingiva, mucosa, lips herpes in a severe treatments like(
and the palate. form
treatment: extractions, matrix band
1. Bed rest fluid, cool and soft retainer placements,
food. rubber dam clamps...
2. Acyclovir in severe cases. etc.).
3. Paracetamol.
b) Fungal Lesions - white -Differentiated from
/Erythematous 1. Nystatin. plaque by :
lesions 2. Amphptericin B. 1.their creamy
- Cribriform redness consistency
growing deep into the 2. After wipe it away
tissues. you see redness.
Done by: Mais Rihani Page 1
C) Bacterial -Bacterial infections are
chronic.
Lesions - Necrotizing ulcerative
✓ Necrotizing gingivitis is an ACUTE
lesions: NUG, form of bacterial
NUP, NUS. infection.
✓ Abscesses of the -site: marginal gingiva - impacted -remove the foreign body. -can occur in people
periodontium: or interdental papilla foreign body -not removed :rupture with periodontitis
1. Localized, painful, -iatrogenic spontaneously/ becomes
1. Gingival and rapidly expanding causes recurrent lesion
swelling with red,
abscess.
smooth shiny surface.
2. Fluctuant and
pointed.
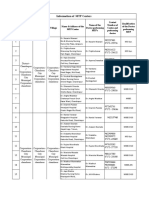
-Sudden onset of: - Obstruction of 1. Incision & drainage the second most
2. Periodontal 1. Pain. 2. Red, bluish opening of through sulcus. common dental
abscess.(not swelling 3.lateral to deep pockets 2. Scaling & root planning. emergency after
apical) affected teeth. by: 3. Irrigation with saline or endodontic/periapical
4. Tooth is mobile, 1. Foreign body H2O2 (3%). abscesses
extruded “high” on impaction. 4. Periodontal surgery if -Vitality test is v.imp
occlusion. 2. Partial healing inaccessible. for DDX
5. Pus drain through of a deep pocket. 5. Antibiotics for 5 days - postoperative care is
pocket or sinus tracts 6. -other factors : followed by instrumentation. needed
Systemic involvement if root morphology/ (Only if the infection is -Complications:
infection disseminated. immune response spreading or if the patient is 1. Tooth loss.
immunocompromised). 2. Cellulitis
✓ Extraction if prognosis is -(there is detailed
poor. information about this
✓ We don’t take biopsy. subject in the sheet
refers to inflammation of Unless it didn’t respond to pages 7+8+11+12)
conventional tx
the gingiva in relation to
3. Pericoronal 1. Red, swollen -the space 1. Gently flushing the area -mostly in mand.3rd
the crown of an tenderness with warm water to remove molar.
abscess. between the
incompletely erupted 2. . Radiating pains to crown of the debris - Once the acute
(Pericoronitis)
tooth.
Done by: Mais Rihani Page 2
the ear, the throat, tooth and the 2. Swabbing with antiseptic. symptoms have
and floor of the overlying gingival 3. The occlusion is evaluated. subsided, the prognosis
mouth. flap (operculum) 4.Pericoronal flap: It may be of the tooth can be
3. Foul taste. is an ideal area necessary to reduce soft tissue evaluated.
4. Inability to close for the surgically and/or to
the jaws. accumulation of 5. Adjust the opposing tooth
5. Swelling of the food debris and ----------------------------------------
cheek in the region bacterial growth. 6. Antibiotics can be
of the angle of the prescribed in severe.
jaw. 7. If the gingival flap is swollen
6. Trismus. and fluctuant, an incision may
be necessary to
7. Systemic
8. Establish drainage and
involvement.
relieve pressure.
✓ Combined A) Primary a) start from a PA -always start with RCT pathways endodontic
periodontal- endodontic- origin (necrotic and periodontic lesions
endodontic secondary pulp)& spread communicate through:
lesions periodontic. to periodontal 1. Apex.
B) Primary periodontic- tissue 2. lateral canals +
secondary b) Start as pockets.
endodontic. periodontitis 3. accessory canals.
C) Combined pulp may be ( mainly found apically
periodontic- vital &in the furcation area)
endodontic lesion. c) periodontium 4. Rarely, through the
and pulp are exposed dentinal
diseased tubules.
independently
from each
other that are
combined at
some point.
Done by: Mais Rihani Page 3
You might also like
- How To Start A Niche Staffing or Recruiting Business - Discover Your NicheDocument30 pagesHow To Start A Niche Staffing or Recruiting Business - Discover Your NicheDee Williams67% (3)
- NCP DMDocument4 pagesNCP DMAarav (мя Ρєяfєт)No ratings yet
- Fluor - Risk ManagementDocument37 pagesFluor - Risk ManagementromadhinhoNo ratings yet
- Mayo Clinic Infectious Diseases Board Review Mayo Clinic Scientific PRDocument581 pagesMayo Clinic Infectious Diseases Board Review Mayo Clinic Scientific PRarahman16877% (13)
- Pre and Post PregnancyDocument23 pagesPre and Post PregnancyJitendra ChaudharyNo ratings yet
- Superficial and Cutaneous Mycoses: 2. Disease CharacteristicsDocument4 pagesSuperficial and Cutaneous Mycoses: 2. Disease CharacteristicsMA. ANGELI DELA CRUZNo ratings yet
- Drug Study - Hyoscine Butylbromide IVDocument1 pageDrug Study - Hyoscine Butylbromide IVJet Bautista80% (5)
- Nursing Test 5 (NP Iii)Document12 pagesNursing Test 5 (NP Iii)Yuxin LiuNo ratings yet
- Risk For InfectionDocument3 pagesRisk For Infectionprickybiik100% (1)
- Yellow Print VDA Volume Process Description Special Characteristics SCDocument98 pagesYellow Print VDA Volume Process Description Special Characteristics SCesivaks200078% (9)
- Wound Care, Suture Materials & Suturing TechniquesDocument80 pagesWound Care, Suture Materials & Suturing TechniquesAlwin PrasetyaNo ratings yet
- WOUNDDocument52 pagesWOUNDIrfan Ritonga100% (6)
- Nursing Care Plan - RabiesDocument2 pagesNursing Care Plan - Rabiesderic89% (9)
- Assignment Trends and IssuesDocument16 pagesAssignment Trends and IssuesVarna MohanNo ratings yet
- Atestat EnglezaDocument14 pagesAtestat EnglezaClaudia SmaduNo ratings yet
- Mock ScenarioDocument35 pagesMock ScenarioCarla Catrina EstradaNo ratings yet
- Tissue Response To Complete DentureDocument7 pagesTissue Response To Complete DentureEVA MONSERRATNo ratings yet
- Bacterial Infection ReviewerDocument5 pagesBacterial Infection ReviewerJAMIE E. EULLARANNo ratings yet
- ConjunctivitisDocument4 pagesConjunctivitisKumar ShivamNo ratings yet
- Endophthalmitis: Current Trends, Drugs and Protocols: Aditya Verma, Vinata Muralidharan and Eesh NigamDocument10 pagesEndophthalmitis: Current Trends, Drugs and Protocols: Aditya Verma, Vinata Muralidharan and Eesh NigamHerman Kurt Ludvik100% (1)
- Endodontic Emergency (Dr. Imran)Document2 pagesEndodontic Emergency (Dr. Imran)aelessyaNo ratings yet
- Bacterial Skin InfectionDocument4 pagesBacterial Skin InfectionAngeline TaghapNo ratings yet
- 3) Bacterial Skin Infections Semi NotesDocument2 pages3) Bacterial Skin Infections Semi NotesIssa MoodNo ratings yet
- Module 2 Vettech325Document31 pagesModule 2 Vettech325cejproiloNo ratings yet
- Etiology of Periodontal DiseaseDocument3 pagesEtiology of Periodontal DiseaseKelly YeowNo ratings yet
- Etiology of Periodontal DiseaseDocument3 pagesEtiology of Periodontal DiseaseKelly YeowNo ratings yet
- PERIO Midterm NotesDocument7 pagesPERIO Midterm Notesabsjob1No ratings yet
- Classification of Wounds: Definition: It Is A Bruise, Usually Produced by AnDocument3 pagesClassification of Wounds: Definition: It Is A Bruise, Usually Produced by AnIvyLove CatalanNo ratings yet
- Assessment Nursing Diagnosis Expected Outcomes Intervention Evaluation Nursing Interventions Rationale Resources RequiredDocument3 pagesAssessment Nursing Diagnosis Expected Outcomes Intervention Evaluation Nursing Interventions Rationale Resources RequiredSiena KaleiNo ratings yet
- 1.02 Sugical Conditions of The Skin and Subcutaneous Tissue (Part2)Document6 pages1.02 Sugical Conditions of The Skin and Subcutaneous Tissue (Part2)Klyn Agagon GayodanNo ratings yet
- Candidiasis: 1. Thrush-Causes Curd-Like White Patches Inside TheDocument2 pagesCandidiasis: 1. Thrush-Causes Curd-Like White Patches Inside ThekyawNo ratings yet
- ENT Trans Disorders of The External EarDocument4 pagesENT Trans Disorders of The External EarJared Ezrach Cacal SanidadNo ratings yet
- Orofacial Infections PDFDocument19 pagesOrofacial Infections PDFMai TNo ratings yet
- Systemic Mycoses: A. BlastomycosisDocument3 pagesSystemic Mycoses: A. Blastomycosisbaihern24No ratings yet
- Subjective: Independent:: Nursing Care PlanDocument2 pagesSubjective: Independent:: Nursing Care PlanJade HemmingsNo ratings yet
- A Seb Előadásom HonlapraDocument52 pagesA Seb Előadásom HonlapraChristabella Natalia WijayaNo ratings yet
- Bacterial Infections 1Document2 pagesBacterial Infections 1jihanNo ratings yet
- 7a. Caria Complicata-PulpotomiaDocument64 pages7a. Caria Complicata-PulpotomiaNia AdibNo ratings yet
- Ncp-Case Pre Impaired Tissue Integrity-1Document2 pagesNcp-Case Pre Impaired Tissue Integrity-1Jade HemmingsNo ratings yet
- Clinical AND ADVANCE Pathology: TopicDocument7 pagesClinical AND ADVANCE Pathology: TopicNestley TiongsonNo ratings yet
- Oral Medicin Before The MidDocument48 pagesOral Medicin Before The MidNoura RihanNo ratings yet
- A Seb Előadásom HonlapraDocument52 pagesA Seb Előadásom HonlapraAliyah Tofani PawelloiNo ratings yet
- Classification and Management of Wound, Principle of Wound Healing, Haemorrhage and Bleeding ControlDocument39 pagesClassification and Management of Wound, Principle of Wound Healing, Haemorrhage and Bleeding ControlrohitNo ratings yet
- CorneaDocument5 pagesCorneaMohamed GhanemNo ratings yet
- Derma ReviewerDocument22 pagesDerma ReviewerAlyssandra LucenoNo ratings yet
- Actinomycosis and NOMADocument10 pagesActinomycosis and NOMASOUMYA A DR, DEPT.OF DENTAL SCIENCES,SRIHERNo ratings yet
- CD Additional LessonsDocument13 pagesCD Additional LessonsAlma Janella TOSINONo ratings yet
- 2.06 - Bacterial InfectionsDocument8 pages2.06 - Bacterial InfectionsMaria CanabeNo ratings yet
- Bruise: Wounds and Injuries of The Soft Tissues of The Facial AreaDocument12 pagesBruise: Wounds and Injuries of The Soft Tissues of The Facial AreaCharlene LunaNo ratings yet
- Actinomyecytes PrintDocument3 pagesActinomyecytes PrintSifat DewanNo ratings yet
- Micro Chart Test 3Document8 pagesMicro Chart Test 3api-26938624No ratings yet
- NCP ImpairedDocument3 pagesNCP ImpairedLyka NgayanNo ratings yet
- ch.2 (Deep Carious Lesion Management)Document19 pagesch.2 (Deep Carious Lesion Management)Nasser HashimNo ratings yet
- MetronidazoleDocument2 pagesMetronidazoleMartha Glorie Manalo WallisNo ratings yet
- Act 2-Criticalthinking CDDocument3 pagesAct 2-Criticalthinking CDWILJOHN DE LA CRUZNo ratings yet
- Occupational Hazards in Dental, Textile Industry and MechanicDocument20 pagesOccupational Hazards in Dental, Textile Industry and MechanicimtahifNo ratings yet
- Inflammation Introduction - Acute InflammationDocument12 pagesInflammation Introduction - Acute Inflammationlunijenn37No ratings yet
- Lecture 18 Cellular SpacesDocument7 pagesLecture 18 Cellular SpacesSara Abdul RahmanNo ratings yet
- Candidiasis 161115175237Document1 pageCandidiasis 161115175237Cikw KuzhaNo ratings yet
- Microbial Disease On SkinDocument19 pagesMicrobial Disease On SkinrishellemaepilonesNo ratings yet
- Dermatology Revision E6.5 'Document35 pagesDermatology Revision E6.5 'Riya SharmaNo ratings yet
- WK 3b Immune System 2023Document18 pagesWK 3b Immune System 2023Basmala HebaNo ratings yet
- Predisposing Factors: CandidiasisDocument4 pagesPredisposing Factors: CandidiasisMary ChristelleNo ratings yet
- NCP 1Document2 pagesNCP 1SienaNo ratings yet
- Graph and Treatment Lecture 2Document6 pagesGraph and Treatment Lecture 2Mateusz RadwańskiNo ratings yet
- Integumentary Disoder: Nursing Care PlanDocument3 pagesIntegumentary Disoder: Nursing Care PlanFrancise Elyn OcubilloNo ratings yet
- LSD Facts Sheet PDFDocument5 pagesLSD Facts Sheet PDFwebmaster@drugpolicy.orgNo ratings yet
- Carbon DioxideDocument4 pagesCarbon DioxideAndri PrastianNo ratings yet
- Role of Exercise Treatment of Low Back Pain in PregnancyDocument7 pagesRole of Exercise Treatment of Low Back Pain in Pregnancysansu3265No ratings yet
- Q3 English 8 ExaminationDocument3 pagesQ3 English 8 ExaminationMark Phil SaluyaNo ratings yet
- Neonatal PneumoniaDocument2 pagesNeonatal PneumoniaJustin EduardoNo ratings yet
- Domestic Workers ActDocument5 pagesDomestic Workers ActTroy San MarNo ratings yet
- Places and Spaces Rough Draft EssayDocument7 pagesPlaces and Spaces Rough Draft Essayapi-273002979No ratings yet
- Simpson AffidavitDocument55 pagesSimpson AffidavitCalgary HeraldNo ratings yet
- Macro Calculator - Anna VictoriaDocument2 pagesMacro Calculator - Anna VictoriaDonnaNo ratings yet
- Estimating R 2 Shrinkage in RegressionDocument6 pagesEstimating R 2 Shrinkage in RegressionInternational Jpurnal Of Technical Research And ApplicationsNo ratings yet
- Safety and Reference: Owner'S ManualDocument304 pagesSafety and Reference: Owner'S ManualDragsNo ratings yet
- MOH ChandrapurDocument3 pagesMOH ChandrapurAbhishek Motiram JagtapNo ratings yet
- HPHT 1Document59 pagesHPHT 1Jesus VargasNo ratings yet
- Anorectal Malformations: DR BenakDocument22 pagesAnorectal Malformations: DR Benakbenak shivalingappaNo ratings yet
- Biomolecules 09 00551 With CoverDocument122 pagesBiomolecules 09 00551 With Coverprabhakar beeravelliNo ratings yet
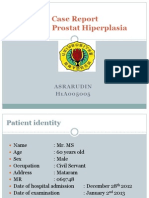
- Lapsus - Asrarudin - BPHDocument18 pagesLapsus - Asrarudin - BPHAsrarudin HamidNo ratings yet
- Centurion Lead Acid Battery, Wet, Non Spillable Sds 01898 03042018Document7 pagesCenturion Lead Acid Battery, Wet, Non Spillable Sds 01898 03042018Munya BengezaNo ratings yet
- Ascoli's Thermo Precipitin TestDocument8 pagesAscoli's Thermo Precipitin TestAbhijith SPNo ratings yet
- Comparison of Polymerization ShrinkageDocument6 pagesComparison of Polymerization ShrinkageYeison HidalgoNo ratings yet
- Moringa Breastfeeding Study PDFDocument4 pagesMoringa Breastfeeding Study PDFCisco Silva100% (1)