Professional Documents
Culture Documents
Conflict of Interests: Subscripts
Uploaded by
StevepallmerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Conflict of Interests: Subscripts
Uploaded by
StevepallmerCopyright:
Available Formats
8 Computational and Mathematical Methods in Medicine
pressure dynamics of the lung simulator were done and the Subscripts
conclusions are summed up as follows. 1: Equivalent throttle 1
(1) The measured data has a good consistency with the 2: Equivalent throttle 2
ventilator report, and the experiment is authentic and 𝑑: Downstream side
reliable. 𝑒: Exhalation valve
lung: Parameter of lung
(2) The simulation results are consistent with the experi- loss: Pressure loss
mental results, which verify the mathematical model. 𝑢: Upstream side
(3) The air pressure in the lung simulator rises with a 𝑡: Tube.
growth in the output pressure of the ventilator and
declines with a decrease in the output pressure of Conflict of Interests
the ventilator. The air pressure in the lung simulator
always lags behind the output pressure of the ventila- The authors declare that there is no conflict of interests
tor. regarding the publication of this paper.
(4) Increasing IPAP may lead to a distinct rise in max-
imum pressure of the lung simulator. The EPAP Acknowledgment
elevation may result in a significant rise in minimum
pressure of the lung simulator. Influences of BPM, the The research is funded by Open Foundation of the State Key
inspiration time (𝑇𝑖 ), and the pressure rise time (𝑇𝑟 ) Laboratory of Fluid Power Transmission and Control.
on the pressure dynamics of the lung simulator are
very slight. References
(5) When the respiratory compliance (𝐶) is smaller than
10 mL/cm H2 O, the air pressure in the lung simulator [1] F. T. Tehrani, “A control system for mechanical ventilation of
can reach IPAP. However, when the 𝐶 is bigger passive and active subjects,” Computer Methods and Programs
in Biomedicine, vol. 110, no. 3, pp. 511–518, 2013.
than 10 mL/cm H2 O, the peak pressure of the lung
simulator is inversely proportional to the respiratory [2] S. P. Pilbeam and J. M. Cairo, Mechanical Ventilation, Physio-
logical and Clinical Application, Mosby Elsevier, St. Louis, Mo,
compliance (𝐶).
USA, 4th edition, 2006.
(6) When the diameter (𝑑) of the equivalent effective area [3] R. L. Chatburn, “Classification of ventilator modes: update and
is larger than 3.2 mm, the air pressure in the lung proposal for implementation,” Respiratory Care, vol. 52, no. 3,
simulator can get to IPAP. But when the diameter (𝑑) pp. 301–323, 2007.
of the effective area is smaller than 3.2 mm, the peak [4] M. Tuǧrul, E. Çamci, H. Karadeniz, M. Şentürk, K. Pembeci,
pressure of the lung simulator increases with a rise in and K. Akpir, “Comparison of volume controlled with pressure
the diameter (𝑑) of the effective area. controlled ventilation during one-lung anaesthesia,” British
Journal of Anaesthesia, vol. 79, no. 3, pp. 306–310, 1997.
The study can be referred to in the respiratory diagnostics, [5] M. M. James and G. J. Beilman, “Mechanical Ventilation,”
treatment, and design of various medical devices or diagnos- Surgical Clinics of North America, vol. 92, no. 6, pp. 1463–1474,
tic systems. In addition, it may accelerate research on the 2012.
development of new diagnostic and treatments. [6] A. J. Garneroa, H. Abbonab, F. Gordo-Vidalc et al., “Pressure
versus volume controlled modes in invasive mechanical venti-
Nomenclature lation,” Medicina Intensive, vol. 37, no. 4, pp. 292–298, 2013.
[7] V. Jounieaux and C. Andréjak, “Pressure-controlled ventilation
𝐴 𝑒: Effective area of throttle (m2 ) and sleep in COPD patients in the intensive care unit: the role
𝑏: Critical pressure ratio = 0.528 of tidal volume?” Respiratory Medicine, vol. 107, no. 10, pp. 1633–
𝐶: Respiratory compliance (L/cm H2 O) 1634, 2013.
𝑑: Diameter of effective area (m) [8] C. Andréjak, J. Monconduit, D. Rose et al., “Does using
𝑙: Length (m) pressure-controlled ventilation to rest respiratory muscles
𝑚: Mass of air (kg) improve sleep in ICU patients?” Respiratory Medicine, vol. 107,
𝑝: Pressure (pa) no. 4, pp. 534–541, 2013.
𝑞: Air mass flow (kg/s) [9] A. W. Thille, B. Cabello, F. Galia, A. Lyazidi, and L. Brochard,
“Reduction of patient-ventilator asynchrony by reducing tidal
𝑄: Air volume flow (m3 /s)
volume during pressure-support ventilation,” Intensive Care
𝑅: Gas constant = 287 (J/(kg⋅K)) Medicine, vol. 34, no. 8, pp. 1477–1486, 2008.
𝑅𝑟 : Respiratory resistance (cm H2 O/L/s)
[10] B. Cabello, S. Parthasarathy, and J. Mancebo, “Mechanical ven-
𝑇: Temperature (K) tilation: let us minimize sleep disturbances,” Current Opinion in
𝑡: Time (s) Critical Care, vol. 13, no. 1, pp. 20–26, 2007.
𝑉: Volume (m3 ) [11] N. Jaimchariyatam, R. A. Dweik, R. Kaw, and L. S. Aboussouan,
𝜆: Friction coefficient “Polysomnographic determinants of nocturnal hypercapnia in
𝜌: Density (kg/m3 ) patients with sleep apnea,” Journal of Clinical Sleep Medicine,
𝜅: Specific heat ratio = 1.4. vol. 9, no. 3, pp. 209–215, 2013.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- (A. McLuckie) Respiratory Disease and Its Manageme PDFDocument169 pages(A. McLuckie) Respiratory Disease and Its Manageme PDFDerison MarsinovaNo ratings yet
- Neonatal Resuscitation: BY DR Babatunde O.TDocument20 pagesNeonatal Resuscitation: BY DR Babatunde O.Tijojo elizabethNo ratings yet
- Encyclopedia of Clinical Pharmacy by Joseph T. DiPiroDocument958 pagesEncyclopedia of Clinical Pharmacy by Joseph T. DiPiroAlex Pieces100% (1)
- Care For Mechanical VentilationDocument14 pagesCare For Mechanical Ventilationmaeya186135100% (3)
- Mechanical VentilatorDocument9 pagesMechanical VentilatorAnusha Verghese100% (2)
- Step by Step Neonatal Ventilation PDFDocument99 pagesStep by Step Neonatal Ventilation PDFUtuh Kalambuai50% (2)
- Introduction To Pediatric VentilationDocument41 pagesIntroduction To Pediatric Ventilationedderj2585No ratings yet
- Nursing Management of Patient With Mechanical VentilationDocument77 pagesNursing Management of Patient With Mechanical Ventilationrojina poudel0% (1)
- Service Manual - 731 VentilatorsDocument228 pagesService Manual - 731 VentilatorsChris HA100% (1)
- Dräger Flow Acceleration Feature v5.5.21Document4 pagesDräger Flow Acceleration Feature v5.5.21Marlon PokeNo ratings yet
- Schematic of Experimental Span of JSC "STC FGC UES" For Testing of Vibration Dampers On Wire EfficiencyDocument5 pagesSchematic of Experimental Span of JSC "STC FGC UES" For Testing of Vibration Dampers On Wire EfficiencyStevepallmerNo ratings yet
- Seventh Natural Waveform of AC 120/19 Wire Sample With Damper GPG-1,6-11-450Document5 pagesSeventh Natural Waveform of AC 120/19 Wire Sample With Damper GPG-1,6-11-450StevepallmerNo ratings yet
- Maximum Bending Stresses in AC 150/24 Wire Sections With and Without Dampers HVT-1,6-11-800, GPG-1,6-11-450Document5 pagesMaximum Bending Stresses in AC 150/24 Wire Sections With and Without Dampers HVT-1,6-11-800, GPG-1,6-11-450StevepallmerNo ratings yet
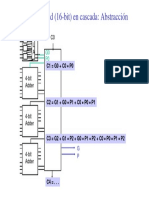
- Clase6 2014-7 PDFDocument1 pageClase6 2014-7 PDFStevepallmerNo ratings yet
- Thirteenth Proper Form of Vibration of The Sample Wire AC 120/19 With Dampener GPH-1,6-11-450Document5 pagesThirteenth Proper Form of Vibration of The Sample Wire AC 120/19 With Dampener GPH-1,6-11-450StevepallmerNo ratings yet
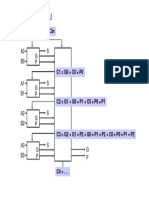
- Clase6 2014-5 PDFDocument1 pageClase6 2014-5 PDFStevepallmerNo ratings yet
- Fig. 5. Sample Selection of Random Action.: Z. Xiang, Et AlDocument1 pageFig. 5. Sample Selection of Random Action.: Z. Xiang, Et AlStevepallmerNo ratings yet
- Mediators: The Scientific World JournalDocument1 pageMediators: The Scientific World JournalStevepallmerNo ratings yet
- 10 PDFDocument1 page10 PDFStevepallmerNo ratings yet
- BF 02129047Document14 pagesBF 02129047StevepallmerNo ratings yet
- View PDFDocument135 pagesView PDFStevepallmerNo ratings yet
- 6 PDFDocument1 page6 PDFStevepallmerNo ratings yet
- Introduction and Modeling of Mechanical Ventilation SystemDocument1 pageIntroduction and Modeling of Mechanical Ventilation SystemStevepallmerNo ratings yet
- Tube Lung: 3. Experimental and Simulation StudyDocument1 pageTube Lung: 3. Experimental and Simulation StudyStevepallmerNo ratings yet
- Section 2.2.4: 5. ConclusionsDocument1 pageSection 2.2.4: 5. ConclusionsStevepallmerNo ratings yet
- 3.4. Analysis and Discussions. The Curve and Fitted Curve ofDocument1 page3.4. Analysis and Discussions. The Curve and Fitted Curve ofStevepallmerNo ratings yet
- Influence On Air Pressure Dynamic Characteristics: Figure 5: Respiratory Resistance of The SystemDocument1 pageInfluence On Air Pressure Dynamic Characteristics: Figure 5: Respiratory Resistance of The SystemStevepallmerNo ratings yet
- Research Article: Pressure Dynamic Characteristics of Pressure Controlled Ventilation System of A Lung SimulatorDocument1 pageResearch Article: Pressure Dynamic Characteristics of Pressure Controlled Ventilation System of A Lung SimulatorStevepallmerNo ratings yet
- 10 PDFDocument1 page10 PDFStevepallmerNo ratings yet
- Computational and Mathematical Methods in Medicine 9Document1 pageComputational and Mathematical Methods in Medicine 9StevepallmerNo ratings yet
- MSN LEC GROUP 2 Oxygenation Ventilation Additional InfosDocument16 pagesMSN LEC GROUP 2 Oxygenation Ventilation Additional InfosJohn MalkovicNo ratings yet
- Mechanical Ventilation 101: DR Paul Healey ICU Fellow John Hunter Hospital NewcastleDocument95 pagesMechanical Ventilation 101: DR Paul Healey ICU Fellow John Hunter Hospital NewcastlePatrick ValentinoNo ratings yet
- Dräger Savina 300 Classic: Technical DataDocument4 pagesDräger Savina 300 Classic: Technical DataIZAL100% (1)
- Mechanical Ventilation Training 3Document13 pagesMechanical Ventilation Training 3Nakato ShadiaNo ratings yet
- Kaynar2018 Medscape PDFDocument29 pagesKaynar2018 Medscape PDFberlianNo ratings yet
- Infant Ventilator For Conventional Ventilation (Also Available With Optional HFO)Document8 pagesInfant Ventilator For Conventional Ventilation (Also Available With Optional HFO)ROHIT KHANNANo ratings yet
- Complet Cardoio Pulmonary - Brochure NEW0.2 PDFDocument39 pagesComplet Cardoio Pulmonary - Brochure NEW0.2 PDFgladyannNo ratings yet
- MechanicalVentilation PrintPDFDocument261 pagesMechanicalVentilation PrintPDFIvulik87No ratings yet
- Horus 4Document6 pagesHorus 4Juan carlos100% (1)
- 222 MIDTERM Central Philippine UniversityDocument7 pages222 MIDTERM Central Philippine Universitygwen pencerNo ratings yet
- Chapter 6. Operation: Before Operation, Prepare The Ventilator As Instructed inDocument18 pagesChapter 6. Operation: Before Operation, Prepare The Ventilator As Instructed indeboraNo ratings yet
- Mechanical Ventilation Basic ModesDocument37 pagesMechanical Ventilation Basic ModesAmr El TaherNo ratings yet
- New Insights in Mechanical Ventilation and Adjunctive Therapies in ARDSDocument11 pagesNew Insights in Mechanical Ventilation and Adjunctive Therapies in ARDSKarina Vanessa María Llanos YupanquiNo ratings yet
- Chapter 03Document23 pagesChapter 03alqahtaniabdullah271No ratings yet
- Nasal IMV - Gatot PDFDocument43 pagesNasal IMV - Gatot PDFtutiarlyNo ratings yet
- Indications For Mechanical VentilationDocument25 pagesIndications For Mechanical VentilationKenneth Jay EdnacoNo ratings yet
- Test Bank For Pilbeams Mechanical Ventilation 6th Edition J M CairoDocument35 pagesTest Bank For Pilbeams Mechanical Ventilation 6th Edition J M Cairoacholiaquacha.v575100% (46)
- Trilogy Ev300 Clinical PresentationDocument40 pagesTrilogy Ev300 Clinical PresentationMojahid HamidNo ratings yet
- Renal Failure, Acute (Acute Kidney Injury) : Selected ReferencesDocument10 pagesRenal Failure, Acute (Acute Kidney Injury) : Selected ReferencesputriarumNo ratings yet
- Bipap 3Document13 pagesBipap 3Dayana EscobedoNo ratings yet