Professional Documents
Culture Documents
SOP For Discharge Planning (Nursing)
Uploaded by
enumula kumarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SOP For Discharge Planning (Nursing)
Uploaded by
enumula kumarCopyright:
Available Formats
Logo HCS CARDIAC CARE CENTER SOP ID -GNSOP001
Version No: 01
Approved by DISCHARGE PLANNING Date of Approval
DISCHARGE PLANNING
1. Introduction:
Discharge planning begins at the time of admission. The discharge plan shall ensure that every
patient is assessed on admission for discharge needs. A discharge plan is developed for every
patient, documented, and initiated.
Discharge Planning is one such thing which provides information to the in regards to discharge
of the patient.
2. Objective:
This policy applies for all patients admitted as Inpatient to the hospital. Surgical and
Observation patients may require discharge planning.
To standardize the process for discharge planning
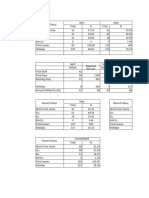
3. Workflow:
4. Detailed work instructions:
1. Discharge planning will begin on admission with the initial nursing assessment being
reviewed by the Case Manager to determine post-discharge needs of the patient.
A. Assessments will include:
1. Assessment of the patient ability to perform activities of daily living
(ADLs)
2. Assessment of whether or not the needs of the patient were being met
pre-admission.
3. Assessment of the patient ability to perform self-care.
4. Assessment of the patient’s support person to provide care.
5. Assessment of the possible need for medical equipment.
6. Assessment of need for home environment modifications.
7. Assessment of available community-based services that may be
needed.
8. Assessment of the patient’s insurance coverage (if applicable) and how
that coverage would or would not provide for post-discharge needs.
9. Was the patient’s family or support person included in the discussion
of post-discharge needs?
2. A plan of care will be developed, implemented and documented in the record identify
needs and plans to address those needs.
3. The physician will be consulted as needed to obtain necessary consults or orders to
meet other patient needs.
4. Patient and family education will be provided as needed during the patient’s stay and
will be documented in the record.
5. The discharge plan may change and/or be redefined during the patient’s stay and will
be a multi-discipline, collaborative effort.
6. Discharge planning can include but is not limited to the following:
a. Therapy consults
b. Home oxygen set-up and delivery
c. Post-discharge appointment planning
d. Medication education and assistance with obtaining home medications
e. DME set up and delivery at home i.e. hospital bed, walker, etc.
f. Social assistance
g. Nursing home or personal care home placement
h. Home Health care referral
i. Insurance authorization requests
j. Sending of necessary medical information to the post-discharge provider.
You might also like
- Code Blue Running SheetDocument2 pagesCode Blue Running Sheetenumula kumar100% (11)
- 28-Nursing Assessment For Admission ofDocument3 pages28-Nursing Assessment For Admission ofakositabon100% (1)
- Key Performance Indicators - Signposts To Loss PreventionDocument2 pagesKey Performance Indicators - Signposts To Loss PreventionSteve ForsterNo ratings yet
- Hospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsFrom EverandHospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsNo ratings yet
- Lourdes Hospital Discharge Process StudyDocument24 pagesLourdes Hospital Discharge Process StudyakinravNo ratings yet
- LATEST Draft of Nursing PoliciesDocument152 pagesLATEST Draft of Nursing PoliciesDe La Serna Mitz100% (2)
- Discharge Process at Adityavardhan HospitalDocument6 pagesDischarge Process at Adityavardhan HospitalSanjay Kadam100% (1)
- Preop ChecklistDocument2 pagesPreop ChecklistJan Federick BantayNo ratings yet
- Clinical Audit - RestraintDocument19 pagesClinical Audit - Restraintsanisani1020No ratings yet
- Admission, Discharge and Transfer PDFDocument3 pagesAdmission, Discharge and Transfer PDFAmank's Tamin EgpNo ratings yet
- Hospital Admission GuideDocument6 pagesHospital Admission GuideSandeep Kumar100% (1)
- Essential Roles of a Chief Nursing Officer (CNODocument4 pagesEssential Roles of a Chief Nursing Officer (CNOHazel LezahNo ratings yet
- Patient Transfer Policy v4.0Document34 pagesPatient Transfer Policy v4.0Kharisma Putra100% (1)
- 6-Cross Training As A Motivational and ProblemDocument3 pages6-Cross Training As A Motivational and Problemakositabon100% (1)
- ICU Procedures ManualDocument64 pagesICU Procedures Manualenumula kumar100% (1)
- SOP For Spilling ManagementDocument2 pagesSOP For Spilling Managementenumula kumar100% (2)
- Code Blue Management SOPDocument25 pagesCode Blue Management SOPenumula kumar100% (4)
- As 2214-2004 Certification of Welding Supervisors - Structural Steel WeldingDocument8 pagesAs 2214-2004 Certification of Welding Supervisors - Structural Steel WeldingSAI Global - APAC50% (2)
- In - Patient Service Ward 1Document12 pagesIn - Patient Service Ward 1mitchNo ratings yet
- Managing Outpatient CareDocument64 pagesManaging Outpatient CareDAD SHOTSNo ratings yet
- NABH Staff RatioDocument1 pageNABH Staff RatioRetteri KUMARANNo ratings yet
- Code NurseDocument2 pagesCode Nursenoreen ellie100% (2)
- DamaDocument2 pagesDamajerimiah_manzon100% (1)
- Verbal Order PolicyDocument4 pagesVerbal Order PolicyAruna HarikrishnanNo ratings yet
- Job Description - Deputy Nursing SuperintendentDocument5 pagesJob Description - Deputy Nursing SuperintendentSheen BelsylinNo ratings yet
- Job Description of Operating Room Nurse in IndiaDocument4 pagesJob Description of Operating Room Nurse in IndiaShine George100% (1)
- Admitting A Patient .: Prepared by Ayugi Winnyfred Patience Bsc. Midwifery StudentDocument10 pagesAdmitting A Patient .: Prepared by Ayugi Winnyfred Patience Bsc. Midwifery StudentAYO NELSONNo ratings yet
- Checklist of NursesDocument1 pageChecklist of NursesDhananjay Saini100% (4)
- Nursing Director JobDocument2 pagesNursing Director JobLeelaArunpal100% (1)
- Admission & Discharge (Autosaved)Document99 pagesAdmission & Discharge (Autosaved)Bhuvanya ParthasarathiNo ratings yet
- Procedure Manual HospitalDocument196 pagesProcedure Manual HospitalMarian StrihaNo ratings yet
- Sample Form of Quality Assurance Nursing AuditDocument2 pagesSample Form of Quality Assurance Nursing AuditgandhialpitNo ratings yet
- Ipsg # 2017 PDFDocument30 pagesIpsg # 2017 PDFDARRYLARANHA100% (1)
- Duties and Responsibilities of An RN: Lpns CnasDocument4 pagesDuties and Responsibilities of An RN: Lpns CnasSPTDNo ratings yet
- Job Responsibilities FoDocument4 pagesJob Responsibilities FoKumar BalramNo ratings yet
- TRIAGE POLICIES JuvyDocument6 pagesTRIAGE POLICIES JuvyCuyapo Infirmary Lying-In HospitalNo ratings yet
- Nurse Supervisor Job DescriptionDocument1 pageNurse Supervisor Job DescriptionCharm TanyaNo ratings yet
- Hospital Daily Census ReportDocument1 pageHospital Daily Census ReportGerald TalledoNo ratings yet
- JOB DESCRIPTION OF STAFF NURSE-NABH NewDocument2 pagesJOB DESCRIPTION OF STAFF NURSE-NABH NewGAGANJOT85100% (1)
- Triage in The HospitalDocument15 pagesTriage in The HospitalCarie Manarondong100% (1)
- Head Nurse - PrintDocument4 pagesHead Nurse - PrintMark Joseph Felicitas CuntapayNo ratings yet
- Emergency & Disaster ManagementDocument39 pagesEmergency & Disaster ManagementSanket Telang100% (1)
- CCUDocument82 pagesCCUSarah100% (1)
- Nursing Audit Tool ScorecardDocument2 pagesNursing Audit Tool Scorecardalaysa udok100% (2)
- Minor SurgeryDocument7 pagesMinor SurgeryBabylyn Purugganan100% (1)
- Job Description - Nursing SuperintendentDocument4 pagesJob Description - Nursing SuperintendentSheen BelsylinNo ratings yet
- Icu Design and SetupDocument9 pagesIcu Design and SetupNorfaidah AliNo ratings yet
- Zamboanga Del Sur General Hospital: Staff Nurse Performance Evaluation SheetDocument5 pagesZamboanga Del Sur General Hospital: Staff Nurse Performance Evaluation SheethahahahaaaaaaaNo ratings yet
- ICU Accomplishment Report and Improvement PlanDocument5 pagesICU Accomplishment Report and Improvement PlanMikhaelEarlSantosTacordaNo ratings yet
- ISBAR Communication ToolDocument16 pagesISBAR Communication ToolTni JolieNo ratings yet
- Admission and DischargeDocument35 pagesAdmission and DischargeKaren Arches100% (2)
- Nursing Shift HandoverDocument10 pagesNursing Shift HandoverYosepha Fortuna KristantiNo ratings yet
- Aspen Healthcare Online Interview QuestionDocument5 pagesAspen Healthcare Online Interview QuestionNad DionisioNo ratings yet
- Material ManagementDocument11 pagesMaterial ManagementBhoomika Pandey100% (1)
- Emergency Department PolicyDocument18 pagesEmergency Department PolicySt. Mary's HospitalNo ratings yet
- Preoperative Nursing CareDocument3 pagesPreoperative Nursing CareRaedel San MiguelNo ratings yet
- Protocol Hospital NurseDocument8 pagesProtocol Hospital NurseDeepak patelNo ratings yet
- Emergency Codes in A HospitalDocument19 pagesEmergency Codes in A Hospitalworkshoppe75% (4)
- Manpower planning in hospitalsDocument17 pagesManpower planning in hospitalsBhideVishwasNo ratings yet
- Patient SafetyDocument27 pagesPatient Safetyarahman168No ratings yet
- Self Assessment ToolkitDocument43 pagesSelf Assessment Toolkitshah007zaad100% (1)
- Hospital Food and Beverage ServicesDocument18 pagesHospital Food and Beverage ServicesKomal Sharma100% (1)
- MedicineDocument19 pagesMedicineSarah100% (1)
- Critical care nursing roles, functions, and qualificationsDocument3 pagesCritical care nursing roles, functions, and qualificationsMa Christina Herrera AntesNo ratings yet
- Handbook for Cssd Technicians: Understanding the Basics - Second EditionFrom EverandHandbook for Cssd Technicians: Understanding the Basics - Second EditionNo ratings yet
- The COAT & Review Approach: How to recognise and manage unwell patientsFrom EverandThe COAT & Review Approach: How to recognise and manage unwell patientsRating: 5 out of 5 stars5/5 (1)
- Covering Letter FormatDocument1 pageCovering Letter Formatenumula kumarNo ratings yet
- Recruitment Analysis Report Draft August 2023Document14 pagesRecruitment Analysis Report Draft August 2023enumula kumarNo ratings yet
- Updated kumar resume (1)Document8 pagesUpdated kumar resume (1)enumula kumarNo ratings yet
- 02 Mantra Aarti Nagara Elevator Etc AppsDocument3 pages02 Mantra Aarti Nagara Elevator Etc Appsenumula kumarNo ratings yet
- Study of Productivity Analysis of Tuff Offshore April and May 2023Document6 pagesStudy of Productivity Analysis of Tuff Offshore April and May 2023enumula kumarNo ratings yet
- Floater Health Insurance Analysis ReportDocument8 pagesFloater Health Insurance Analysis Reportenumula kumarNo ratings yet
- Advt-for-Consultant-in-L-T-NewDocument6 pagesAdvt-for-Consultant-in-L-T-Newenumula kumarNo ratings yet
- Leave Analysis excel sheetDocument7 pagesLeave Analysis excel sheetenumula kumarNo ratings yet
- SOP Drug AdministrationDocument4 pagesSOP Drug Administrationenumula kumarNo ratings yet
- SOP Drug AdministrationDocument4 pagesSOP Drug Administrationenumula kumarNo ratings yet
- Discharge Summary FormatDocument14 pagesDischarge Summary Formatenumula kumarNo ratings yet
- Social Challenges and Threats to Filipino FamiliesDocument24 pagesSocial Challenges and Threats to Filipino FamiliesKarlo Jayson AbilaNo ratings yet
- RVUN's Role in Power Generation in RajasthanDocument126 pagesRVUN's Role in Power Generation in Rajasthanvenka07No ratings yet
- Class Program 2023-2024Document1 pageClass Program 2023-2024Cheryl Jane A. MusaNo ratings yet
- Design & Development ISODocument6 pagesDesign & Development ISOمختار حنفىNo ratings yet
- Employee Stock Option SchemeDocument6 pagesEmployee Stock Option Schemezenith chhablaniNo ratings yet
- AMA - Australias Forest Industries at A GlanceDocument2 pagesAMA - Australias Forest Industries at A GlanceCarlos D. GuiradosNo ratings yet
- Assessing The Environmental Impact of Data Centres Part 1: Background, Energy Use and MetricsDocument10 pagesAssessing The Environmental Impact of Data Centres Part 1: Background, Energy Use and Metricsmarf123No ratings yet
- Programme VDZ CongressDocument2 pagesProgramme VDZ CongresssaeedhoseiniNo ratings yet
- The Divine ServitorDocument55 pagesThe Divine ServitorlevidinizNo ratings yet
- Forced Removal: The Division, Segregation, and Control of The People of South AfricaDocument96 pagesForced Removal: The Division, Segregation, and Control of The People of South Africas_annaNo ratings yet
- Finalplansw PDFDocument146 pagesFinalplansw PDFOffice of PlanningNo ratings yet
- Imu200 (Chapter 9 Principle of Harship (Branches)Document11 pagesImu200 (Chapter 9 Principle of Harship (Branches)zahirahnur2023No ratings yet
- Property rights in news, body parts, and wild animalsDocument22 pagesProperty rights in news, body parts, and wild animalskoreanmanNo ratings yet
- NATO Bombing of Yugoslavia (TEXT)Document4 pagesNATO Bombing of Yugoslavia (TEXT)ana milutinovicNo ratings yet
- Introduction: Mobile Phone and Mobile Banking: 1.1 Problems To Be Evaluated and AssessedDocument56 pagesIntroduction: Mobile Phone and Mobile Banking: 1.1 Problems To Be Evaluated and AssessedAbhay MalikNo ratings yet
- How To Activate Wondershare For Lifetime With Key and 127.0.0.1 Platform - Wondershare.com - 2019.mp4Document5 pagesHow To Activate Wondershare For Lifetime With Key and 127.0.0.1 Platform - Wondershare.com - 2019.mp4Rashid MahmoodNo ratings yet
- Bai Tap Ve Cac Thi Qua Khu Don Tiep Dien Hoan Thanh Co Dap AnDocument4 pagesBai Tap Ve Cac Thi Qua Khu Don Tiep Dien Hoan Thanh Co Dap AnNguyễn Gia KhangNo ratings yet
- 1NC RR FinalsDocument17 pages1NC RR FinalsTanish KothariNo ratings yet
- Smoke Values and Cut-Off Speeds Per Engine Type: en-GBDocument7 pagesSmoke Values and Cut-Off Speeds Per Engine Type: en-GBruanNo ratings yet
- ProCapture-T User Manual V1.1 - 20210903 PDFDocument65 pagesProCapture-T User Manual V1.1 - 20210903 PDFahmad khanNo ratings yet
- The Path of Kriya Yoga: An IntroductionDocument7 pagesThe Path of Kriya Yoga: An IntroductionGowthamanBalaNo ratings yet
- Choosing the Right Career and Job RequirementsDocument2 pagesChoosing the Right Career and Job RequirementsdinnahNo ratings yet
- An Interview with Novelist Anita BrooknerDocument12 pagesAn Interview with Novelist Anita BrooknerlupearriegueNo ratings yet
- Film&Broadcast MediaDocument39 pagesFilm&Broadcast MediaDo NotNo ratings yet
- CMC No. PRO13 PEACE AND SECURITY CAMPAIGN PLAN (M+K+K K) PDFDocument13 pagesCMC No. PRO13 PEACE AND SECURITY CAMPAIGN PLAN (M+K+K K) PDFDanielZamoraNo ratings yet
- Lgesp - Pura Neguma Reference Manual For Project StaffDocument62 pagesLgesp - Pura Neguma Reference Manual For Project StaffmuthunayakeNo ratings yet
- IpoDocument43 pagesIpoyogeshdhuri22100% (4)
- Tossa College of Economic DevelopmentDocument2 pagesTossa College of Economic DevelopmentAbdurohman80% (5)