Professional Documents
Culture Documents
Sample Medical History Form77576
Uploaded by
Sheila Judd0 ratings0% found this document useful (0 votes)
8 views1 pageOriginal Title
Sample-Medical-History-Form77576
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views1 pageSample Medical History Form77576
Uploaded by
Sheila JuddCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
CONFIDENTIAL MEDICAL HISTORY Patient___________________________ Dr.
___________________
Physician’s name___________________________________________ Phone #_______________________________
1. Are you in good health? Yes ____ No ____ If no, please provide details____________________________________
_____________________________________________________________________________________________
2. When was the last time you had a medical examination?________________________________________________
3. Are you presently receiving treatment for any illness? If yes, please provide details:___________________________
_____________________________________________________________________________________________
4. Have you ever been hospitalized? If yes, please provide details___________________________________________
_____________________________________________________________________________________________
5. Do you have any heart or circulatory problems? Yes ____ No ____ Do you have a pacemaker? Yes ____ No ____
6. Have you ever had rheumatic fever? Yes ____ No ____ If yes, when________________
7. Have you ever been advised to take antibiotic pre-medication prior to dental treatment? Yes ____ No ____
8. Do you have allergies? Seasonal/hayfever ____ Food _____________________ Medication___________________
_____________________________________________ Other___________________________________________
9. Are you presently taking any kind of medication? If yes, please specify:
Drug ________________________________ Reason ______________________________________________
Drug ________________________________ Reason ______________________________________________
Drug ________________________________ Reason ______________________________________________
10. Have you ever had a reaction to any kind of medicine or dental local anaesthetic? If yes, please provide details:
_____________________________________________________________________________________________
11. Female patients – Are you pregnant or think you may be pregnant? Yes ___ No ___ Breastfeeding? Yes ___No ___
12. Please indicate below (√) if you presently have or have ever had any of the following:
AIDS/HIV Diabetes Liver disease (Hepatitis/Jaundice)
Alcohol or chemical dependency Eating disorders Lung disease/chest pains
Arthritis or Rheumatism Epilepsy/seizures Mental or nervous disorder
Artificial joints or valves Fainting/dizzy spells Stomach ulcers
Asthma High/low blood pressure Stroke
Blood transfusion Hyper/hypo glycemia Tuberculosis
Cancer/radiotherapy/chemotherapy Kidney disease Venereal/communicable disease
12. Do you smoke? If yes, how much per day?___________________ per week? __________________________
13. Do you grind or clench your teeth? Yes ___ No ___
14. Do you suffer from headaches____ earaches_____ or neck aches_____?
15. Is there any additional information related to your health that has not been addressed above? ___________________
______________________________________________________________________________________________
________________________________ ____________ _____________________________ _________
Patient or guardian’s signature Date Reviewed by Date
Medical history update:
__________________________________________________________________________ Date_________________By____________________
__________________________________________________________________________ Date_________________By____________________
__________________________________________________________________________ Date_________________By____________________
__________________________________________________________________________ Date_________________By____________________
You might also like
- SHD Form 1 Medical History-DepEdDocument1 pageSHD Form 1 Medical History-DepEdDivh BoquecozNo ratings yet
- Bipolar Concept MapDocument3 pagesBipolar Concept MapMeghan Cannon57% (7)
- Pre-Employment Medical FormDocument2 pagesPre-Employment Medical FormSourin NandiNo ratings yet
- PEDIATRIC ASSESSMENTDocument11 pagesPEDIATRIC ASSESSMENTRose Ann Salanap80% (5)
- Health Assessment Form CSPCDocument2 pagesHealth Assessment Form CSPCJoyce Ann B. Apin100% (2)
- Obstructive Sleep Apnea PDFDocument11 pagesObstructive Sleep Apnea PDFLaura MoiseNo ratings yet
- Dental Clinic's ServicesDocument4 pagesDental Clinic's ServicesDani ANo ratings yet
- MCQ exam on pharmacology, medicine and treatmentsDocument10 pagesMCQ exam on pharmacology, medicine and treatmentsعزالدين الطيارNo ratings yet
- Initial Visit FormsDocument4 pagesInitial Visit FormsBertie SynowiecNo ratings yet
- Choose Your Favorite WebsiteDocument177 pagesChoose Your Favorite WebsiteSheila Judd78% (9)
- Faculty of Dentistry Academic Calendar 2018-2019Document179 pagesFaculty of Dentistry Academic Calendar 2018-2019Sheila JuddNo ratings yet
- SDCEP Drug Prescribing For Dentistry 3rd EditionDocument96 pagesSDCEP Drug Prescribing For Dentistry 3rd EditionsrideviNo ratings yet
- Pediatric Initial Patient HistoryDocument11 pagesPediatric Initial Patient HistoryLinh TrịnhNo ratings yet
- Defibrillators (C)Document41 pagesDefibrillators (C)Percy Caceres OlivaresNo ratings yet
- Physician Verified Medical HistoryDocument2 pagesPhysician Verified Medical HistoryHoracio RubioNo ratings yet
- 130 Physicians-Report 7-21-2023Document2 pages130 Physicians-Report 7-21-2023medisnadaNo ratings yet
- Medical History Form and Physicians Report For SHS and College StudentsDocument2 pagesMedical History Form and Physicians Report For SHS and College StudentsKimNo ratings yet
- Dental ChartDocument1 pageDental Chartkhalil carloas mendozaNo ratings yet
- Health DeclarationDocument8 pagesHealth DeclarationmkwinijoanNo ratings yet
- Patient Information Record: For MinorsDocument2 pagesPatient Information Record: For MinorsSheere Ann Putoy - ValenzuelaNo ratings yet
- Health History QuestionnaireDocument3 pagesHealth History QuestionnairejlaferriereNo ratings yet
- Newpatient FormsDocument2 pagesNewpatient Formsapi-239262305No ratings yet
- AHG Health & Medical FormsDocument12 pagesAHG Health & Medical FormsAnonymous 2buCBbFNo ratings yet
- Medical Form 2014Document6 pagesMedical Form 2014api-27703975No ratings yet
- Dental Registration and Health History: Insurance InformationDocument4 pagesDental Registration and Health History: Insurance InformationOmar PerezNo ratings yet
- Carolina Plastic SurgeryDocument5 pagesCarolina Plastic SurgeryBob LoblawNo ratings yet
- Chronicle Diabetes Assessment FormDocument8 pagesChronicle Diabetes Assessment FormpriyaNo ratings yet
- Chart OdgDocument2 pagesChart Odgkhistine castilloNo ratings yet
- Webb Doc PaperworkDocument8 pagesWebb Doc Paperworkapi-723577399No ratings yet
- General Questions NO YESDocument5 pagesGeneral Questions NO YESChristian James PACILANNo ratings yet
- Natoza Medical Form For Grade 7 12Document3 pagesNatoza Medical Form For Grade 7 12Deonna AngelineNo ratings yet
- Health Declaration FormDocument1 pageHealth Declaration FormPhilip WanNo ratings yet
- Hypertension HistoryDocument2 pagesHypertension HistorybassamNo ratings yet
- New Patient Paperwork 1Document5 pagesNew Patient Paperwork 1sham AlmasNo ratings yet
- Massage Intake Form TemplateDocument4 pagesMassage Intake Form TemplateronaNo ratings yet
- Vulvar Vaginal Clinic QuestionnaireDocument5 pagesVulvar Vaginal Clinic QuestionnairenovywardanaNo ratings yet
- AXE Medical Questionnaire and Informed ConsentDocument1 pageAXE Medical Questionnaire and Informed ConsentJefferson Kevin MorcoNo ratings yet
- Holistic Approach to Health CareDocument13 pagesHolistic Approach to Health CareRebecca KnightNo ratings yet
- Needs AssessmentDocument16 pagesNeeds Assessmentlilian monariNo ratings yet
- Patient Health ProfileDocument9 pagesPatient Health ProfilerogeliocszNo ratings yet
- Parent/Baby Information SheetDocument7 pagesParent/Baby Information SheetJONABELL B YLAGANNo ratings yet
- Medical+Form InglesDocument1 pageMedical+Form Inglescidaparecida141977No ratings yet
- 2.physical E, HISTORY NCPDocument13 pages2.physical E, HISTORY NCPمريم حجيNo ratings yet
- Adult Communication Case HistoryDocument2 pagesAdult Communication Case HistoryHarshit AmbeshNo ratings yet
- PhyexamfmDocument2 pagesPhyexamfmapi-261727970No ratings yet
- Medical Self-Declaration Form: HCG/HR/MED/09/17/001Document2 pagesMedical Self-Declaration Form: HCG/HR/MED/09/17/001laison issacNo ratings yet
- Nutrition Assessment FormDocument2 pagesNutrition Assessment FormJaerine SyNo ratings yet
- Welcome To Davis Family Hearing: Audiology Case History FormDocument2 pagesWelcome To Davis Family Hearing: Audiology Case History FormweirdoflayloNo ratings yet
- Section ADocument25 pagesSection ABobbiNo ratings yet
- HH FormDocument2 pagesHH FormStefanie Kiss-PlucasNo ratings yet
- Health History QuestionnaireDocument2 pagesHealth History QuestionnaireKumar KNo ratings yet
- Background Demographic FormDocument4 pagesBackground Demographic Formupper010No ratings yet
- Adult Medical History FormDocument3 pagesAdult Medical History Formquanghuy147No ratings yet
- Atient AME GE Ender Irth ATE Ddress Hone ITY Tate IP Hysician S AME ITY HoneDocument2 pagesAtient AME GE Ender Irth ATE Ddress Hone ITY Tate IP Hysician S AME ITY Hone14-120 RahmaNo ratings yet
- Medical History 2022Document2 pagesMedical History 2022auraester.sionillo-18No ratings yet
- Case History Child & Adolescent Intake FormDocument5 pagesCase History Child & Adolescent Intake FormAmol GoreNo ratings yet
- Self Report MedicationDocument3 pagesSelf Report MedicationMarjhun Flores GuingayanNo ratings yet
- Patient Assessment Form: Current ProblemDocument8 pagesPatient Assessment Form: Current ProblemJonard Ariefsieter HelperNo ratings yet
- Student Health Inventory: School YearDocument2 pagesStudent Health Inventory: School YearDave JohnsonNo ratings yet
- Pediatric Medical History FormDocument2 pagesPediatric Medical History FormRoshandiep Gill100% (1)
- General Health Profiling Questionnaire For Punjab University StudentsDocument4 pagesGeneral Health Profiling Questionnaire For Punjab University StudentsMuhammad YousafNo ratings yet
- General Health Profiling QuestionnaireDocument4 pagesGeneral Health Profiling QuestionnaireMuhammad YousafNo ratings yet
- PT. Asuransi Allianz Life Indonesia: Medical CertificateDocument3 pagesPT. Asuransi Allianz Life Indonesia: Medical CertificateEvan RandikaNo ratings yet
- Medical HistoryDocument1 pageMedical HistoryrehbergNo ratings yet
- Dermatology Associates of Central NJ & Freehold Skin Clinic & Cancer CenterDocument2 pagesDermatology Associates of Central NJ & Freehold Skin Clinic & Cancer Centercara harrisNo ratings yet
- Staying Healthy Tips, Techniques and Diet Suggestions for Heart PatientsFrom EverandStaying Healthy Tips, Techniques and Diet Suggestions for Heart PatientsNo ratings yet
- Prescribing and Dispensing Drugs StandardsDocument15 pagesPrescribing and Dispensing Drugs StandardsSheila JuddNo ratings yet
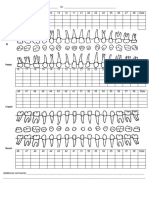
- Sample Odontogram Existing and Planned Treatment PDFDocument2 pagesSample Odontogram Existing and Planned Treatment PDFSheila Judd100% (1)
- Sample Medical History Form77576Document1 pageSample Medical History Form77576Sheila JuddNo ratings yet
- Minimal Moderate Sedation StandardsDocument59 pagesMinimal Moderate Sedation StandardsSheila JuddNo ratings yet
- Patient-Centred Dentistry StandardsDocument6 pagesPatient-Centred Dentistry StandardsSheila JuddNo ratings yet
- Sample Periodontal Chart PDFDocument1 pageSample Periodontal Chart PDFSheila JuddNo ratings yet
- Oral Cancer Clinical Practice GuidelineDocument8 pagesOral Cancer Clinical Practice GuidelineSheila JuddNo ratings yet
- Infection Prevention and Control Wall PosterDocument1 pageInfection Prevention and Control Wall PosterSheila JuddNo ratings yet
- Sample Initial Periodontal Occlusal Examination Form PDFDocument1 pageSample Initial Periodontal Occlusal Examination Form PDFSheila JuddNo ratings yet
- A Guide To CDA Services: Prosthodontic Module Services Orthodontic ModuleDocument2 pagesA Guide To CDA Services: Prosthodontic Module Services Orthodontic ModuleSheila JuddNo ratings yet
- Infection control guidelines for BC dental professionalsDocument48 pagesInfection control guidelines for BC dental professionalsSheila JuddNo ratings yet
- Dispensing of Non-Prescription Medication by Certified Dental AssistantsDocument3 pagesDispensing of Non-Prescription Medication by Certified Dental AssistantsSheila JuddNo ratings yet
- Dismissing A PatientDocument1 pageDismissing A PatientSheila JuddNo ratings yet
- Infection Prevention and Control (IPAC) Guidelines Frequently Asked QuestionsDocument2 pagesInfection Prevention and Control (IPAC) Guidelines Frequently Asked QuestionsSheila JuddNo ratings yet
- General Anaesthesia Standards PDFDocument63 pagesGeneral Anaesthesia Standards PDFSheila JuddNo ratings yet
- Dental Recordkeeping Guidelines PDFDocument16 pagesDental Recordkeeping Guidelines PDFSheila JuddNo ratings yet
- Guide To CDA Services To ViewDocument4 pagesGuide To CDA Services To ViewSheila JuddNo ratings yet
- Your Obligations in Dental Emergencies: For DentistsDocument4 pagesYour Obligations in Dental Emergencies: For DentistsSheila JuddNo ratings yet
- Dental Radiography Standards and GuidelinesDocument22 pagesDental Radiography Standards and GuidelinesKhaidir AlimNo ratings yet
- Crdha Drug GuidelinesDocument40 pagesCrdha Drug GuidelinesSheila JuddNo ratings yet
- Sample Dental History PDFDocument1 pageSample Dental History PDFSheila JuddNo ratings yet
- About Dental Emergencies: For PatientsDocument4 pagesAbout Dental Emergencies: For PatientsSheila JuddNo ratings yet
- Deep Sedation StandardsDocument61 pagesDeep Sedation StandardsSheila JuddNo ratings yet
- Confidentiality Clauses in Settlement Agreements Information SheetDocument2 pagesConfidentiality Clauses in Settlement Agreements Information SheetSheila JuddNo ratings yet
- Blood Borne Pathogen PolicyDocument3 pagesBlood Borne Pathogen PolicySheila JuddNo ratings yet
- Standards of PracticeDocument1 pageStandards of PracticeSheila JuddNo ratings yet
- Syllabus Cancer of ColonDocument7 pagesSyllabus Cancer of ColonMoonyeen NatanawanNo ratings yet
- Lyme Disease InterventionsDocument3 pagesLyme Disease InterventionsahiNo ratings yet
- Circulatory System Reading QuestionsDocument3 pagesCirculatory System Reading QuestionsJanith VimukthiNo ratings yet
- Health 9 Q3 M2Document14 pagesHealth 9 Q3 M2Jorely Barbero MundaNo ratings yet
- Meda QantasDocument12 pagesMeda QantasAviasiNo ratings yet
- Approach To Hemolytic AnemiasDocument41 pagesApproach To Hemolytic AnemiasAmit KinareNo ratings yet
- HDFC Life Group Credit Protect Plus Insurance Plan20161128 093336 PDFDocument8 pagesHDFC Life Group Credit Protect Plus Insurance Plan20161128 093336 PDFSara LopezNo ratings yet
- Education: Recreational TherapistDocument3 pagesEducation: Recreational Therapistapi-570783384No ratings yet
- Unit 4 Endoscopy Bronchoscopy LaporosDocument115 pagesUnit 4 Endoscopy Bronchoscopy LaporosAC19UBM035 SOWMIYA.PNo ratings yet
- Pleno Skenario A TB Dewasa-1Document58 pagesPleno Skenario A TB Dewasa-1ninja sanjeninNo ratings yet
- New global hospital and critical care centre in AkolaDocument2 pagesNew global hospital and critical care centre in AkolaPrashant WankhadeNo ratings yet
- Risks & Benefits of Blood TransfusionDocument34 pagesRisks & Benefits of Blood TransfusionBryand KostaNo ratings yet
- CV Abdul HafeezDocument7 pagesCV Abdul HafeezAbdul Hafeez KandhroNo ratings yet
- Block M2 EYE Distribution by MMCDocument3 pagesBlock M2 EYE Distribution by MMCF ParikhNo ratings yet
- SFP-Vol403 Unit2Document10 pagesSFP-Vol403 Unit2TnchNo ratings yet
- A Cochrane Review of Superficial Heat or ColdDocument9 pagesA Cochrane Review of Superficial Heat or ColdIvanFierroNo ratings yet
- General Stress Level of SHS ABM Students in Their Specialized SubjectDocument4 pagesGeneral Stress Level of SHS ABM Students in Their Specialized SubjectThons Nacu LisingNo ratings yet
- The Twelve Salts and Some of Their Keynote SymptomsDocument2 pagesThe Twelve Salts and Some of Their Keynote Symptomstaichi7No ratings yet
- Stop The Bleed Booklet FinalDocument16 pagesStop The Bleed Booklet FinalUrsula MalauNo ratings yet
- Pathfit 1Document23 pagesPathfit 1Sep TemNo ratings yet
- PATH Fit module on safety protocols and exercise health appraisalDocument1 pagePATH Fit module on safety protocols and exercise health appraisaljinNo ratings yet
- The Psychiatric Comorbidity of Epilepsy PDFDocument14 pagesThe Psychiatric Comorbidity of Epilepsy PDFTanjung E SumekarNo ratings yet
- Music TherapyDocument2 pagesMusic TherapytinaNo ratings yet
- Prevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateDocument7 pagesPrevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateIJAERS JOURNALNo ratings yet
- AlopeciaDocument2 pagesAlopeciaAldrich ArquizaNo ratings yet
- Aids HandoutDocument2 pagesAids Handoutapi-272957818No ratings yet
- Agacayak 2014Document5 pagesAgacayak 2014ERVINA TYAWARMANNo ratings yet