Professional Documents
Culture Documents
A02v27n4 PDF
A02v27n4 PDF
Uploaded by
José CarlosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A02v27n4 PDF
A02v27n4 PDF
Uploaded by
José CarlosCopyright:
Available Formats
Artículo Original / Original Article
Rev Estomatol Herediana. 2017 Oct-Dic;27(4):210-18
Musculoskeletal disorders associated to dentists
work activities in Brazilian primary health care
Trastornos musculosqueléticos asociados a actividades de trabajo de dentistas en el cuidado primario de
salud brasileño
Fábio Barbosa De Souza1,a, Isabelle Ribeiro Braga Costa 2,b, Larissa Lívia Silva Pinto 2,b, Márcia Maria
Dantas Cabral De Melo 3,a
RESUMEN
Objetivos: Verificar la prevalencia de los trastornos musculoesqueléticos asociados con el trabajo (TMEAT) de
los dentistas de la red de atención primaria de salud en Recife, Brasil. Material y Métodos: Se utilizó el Cuestio-
nario nórdico de síntomas musculoesqueléticos con el objetivo de identificar la presencia de dolor, incomodidad
o latencia en diferentes áreas del cuerpo. Resultados: El 97,3% de los entrevistados mencionaron los síntomas
musculoesqueléticos asociados con la práctica de la Odontología. El Cuello (56,75%); el puño / manos / dedos
(54.06%); los hombros (51.35%) y la región lumbar (48,65%) fueron los lugares más afectados. Al medir la aso-
ciación entre TMEAT y las “5” variables extraprofesionales estudiadas, solo la actividad física se asoció con sín-
tomas en la región de puño / manos / dedos (p <0,05). Conclusiones: se observó un alta prevalencia de TMEAT
en dentistas de Recife. La práctica de actividad física regular demostró ser un posible factor de protección para
las lesiones puño / manos / dedos.
PALABRAS CLAVE: Epidemiología, prestación de atención de salud, enfermedades profesionales (DeCS,
BIREME).
1
Department of Prosthesis and Maxillofacial Surgery, Federal University of Pernambuco. Pernambuco, Brazil.
2
Federal University of Pernambuco. Pernambuco, Brazil.
3
Department of Clinics and Preventive Dentistry, Federal University of Pernambuco. Pernambuco, Brazil.
a
M.Sc, PhD
b
Doctor of Dental Surgery.
210 Rev Estomatol Herediana. 2017 Oct-Dic;27(4).
De-Souza FB, Costa IRB, Pinto LLS, Melo MMDC.
SUMMARY
Objectives: It was aimed to verify the prevalence of work-related musculoskeletal disorders (WRMSD) of den-
tists from the primary health care network in Recife, Brazil. Material and Methods: The Nordic Musculoskel-
etal Symptom Questionnaire was used having as goal to identify the presence of pain, discomfort or dormancy
in different body areas. Results: The musculoskeletal symptoms associated with the practice of Dentistry were
mentioned by 97.3% of the interviewees. Neck (56.75%); fist/hands/fingers (54.06%); shoulders (51.35%) and
lumbar region (48.65%) were the most affected locations. When measuring the association between WRMSD
and the “5” extra-professional variables studied, only physical activity was associated with symptoms in the fist
/ hands / fingers area (p <0.05). Conclusions: A high prevalence of WRMSD was observed in dentists of Reci-
fe. The practice of regular physical activity showed to be a possible protective factor for the fist/hands/fingers
lesions.
KEYWORDS: Epidemiology, health care, occupational diseases (DeCS, BIREME).
INTRODUCTION on the same day (3).
The word ‘‘ergonomics’’ is derived from the Greek In Brazil, occupational syndromes have been recog-
language in which ‘‘ergo’’ means ‘‘work’’ and ‘‘no- nized by the Social Insurance Ministry as Work-Rela-
mos’’ means ‘‘law’’. From this point of view, ergo- ted Musculoskeletal Disturbances (WRMSDs). The-
nomics deals with the planning of devices, technical se syndromes can occurs through the permanence of
systems and tasks in order to increase staff security, body segments in determined positions for an exten-
health, comfort and performance. In Dentistry, the ded period of time. The signs and symptoms are mus-
application of ergonomic principles shows to be fun- cles, tendons, fascias, nerves, ligaments, vessels and
damental to the well-being of the working team and articulations inflammation (4). The most common
has as main goal to obtain resources and systems to forms of clinical presentation of these pathologies on
decrease physical/cognitive stress and to prevent di- dentists are tendinitis, tenosynovitis, carpal tunnel sy-
seases related to dental practice, seeking a more ex- ndrome, myositis and bursitis. “The diagnosis of the-
pressive productivity with better quality and greater se conditions should be performed through analysis
comfort for both professional and patient (1). of: professional life; movements’ frequency; equip-
ments; posture during working hours; environmental
Dental practice causes dental surgeons to work for conditions; the time in duty; existence of breaks du-
long hours seated and to assume at times incorrect ring work and of the interpersonal relationships with
postures, thus provoking a mechanic compression on co-workers and superiors”(3).
the structures located in the lumbar region and ad-
jacent areas. The use of instruments and apparatus Prevalence studies in scientific literature have de-
along with task repeatability and excessive applied monstrated that the MSDs have presented expressive
force in certain procedures, expose these professio- numbers among dental surgeons from all around the
nals to develop musculoskeletal lesions from occupa- world with incidence percentage ranging from 63%
tional order (2). Besides dentist’s posture and move- to 95% (5-7) Therefore, with the vertiginous increase
ments-related issues, lesions can derive from modern of the importance of ergonomics in the current con-
technology insertion such as mechanization and text and the crescent Dentistry professionals’ number
automation of work processes, ignoring the lack of involved with musculoskeletal disturbances, a syste-
adaptation and training of workers in this new reality. mic ergonomic approach is necessary to the enhance-
Thus, the tasks are now developed with less effort, ment of working conditions, optimizing productivity
while the movements, however, can be repeated and and reducing lesions occurrence (8,9).
at many times static, always overburdening the same
muscular group through the maintenance of a posture In the last decades, health workforce, management,
that is at times inappropriate and during long periods worker healthcare protection and quality of work en-
Rev Estomatol Herediana. 2017 Oct-Dic;27(4). 211
Musculoskeletal disorders associated to dentists work activities in Brazilian primary health care
vironment issues have been in the center of health po- PHC network of Recife in 2016 (164 professionals).
litical discussions in Brazil (10,11). In Primary Health A pilot or convenience sample composed of 50% of
Care (PHC), dentists’ determined attributions aim in- the group (82 dentists) was randomly selected from a
dividual and collective integral attention to oral heal- population composed of 164 dentists from the city of
th, with familiar and communitarian approach (12). Recife. In each of the eight districts, the selection of
However, it can be observed that assistance activities the sample was made randomly and corresponded to
concentrate this professional major daily workload. 50% of the total number of professionals.
Additionally, there is a scarcity of studies that aim to
clarify the impact of musculoskeletal diseases related Data collection
to the activities carried out by dentists that work in
the PHC (14,15), with the goal of supporting the plan- Data collection used validated Brazilian version of the
ning of actions that intent to prevent the development self-application form named Nordic Musculoskeletal
of these disorders, to improve working conditions and Questionnaire (17), in which the interviewee would
increase quality in services rendered. Therefore, the register the presence or absence of pain, discomfort
intention of this study was to ascertain the prevalence or dormancy in nine body areas: neck/cervical area;
of musculoskeletal disorders related to the work of shoulders; arms; elbows; forearm; fists/hands/fingers;
dental surgeons that perform in health unities in the dorsal area; lumbar region; hips/lower limbs, men-
PHC network of Recife, Pernambuco, Brazil. tioning the frequency of symptoms presence accord-
ing to the following categories: no, rarely, often and
MATERIALS AND METHODS always. Two researchers were responsible for data
collection. The training of the researchers had the ob-
Design and area study jective of standardizing the steps regarding to the data
collection with the respondents: appointment with
The study is defined as observational of the dentist for the delivery of the form; reading of
transversal and quantitative character. The study informed consent for compliance with ethical requi-
development area corresponded to the eight Health rements; receipt of questionnaires after 24 hours. For
Districts (HD) in the PHC network of Recife’s that reason, a reserved location in the BHS was selec-
Secretariat of Health, of which Recife is the capital ted for delivery of the informed consent form and the
of the state of Pernambuco, located in the northeast research form. It was suggested that the interviewee
region of Brazil. should use this space to respond to the form, during
In the city of Recife, in the Northeast Region of the period of work of the dentist.
Brazil, the PHC network expanded in 9 times
the number of Family Health Teams (FHT) in All questions were answered by relating the affect-
the last decade, meaning a coverage increase of ed body area. Besides that, each research participant
would answer if the symptoms presented kept any re-
54%. Data from 2014, informs the existence of
lationship with the dental work performed. Through
153 oral health teams (ESB), which corresponds
this instrument, information regarding the practice of
to 32% of assistance coverage in oral health, physical activity and extraprofessional activities were
considered insufficient (Recife, 2014) (16). Ei- also collected as well as sociodemographic data for
ghty-two dentists are distributed as follows: HD1 the characterization of sample profile.
/ 10, HD2 / 28, HD 3 / 6, HD 4 / 24, HD 5 / 20,
HD 6 / 14, HD 7 / 34 and HD 8 / 28.The modality The data collection was only realized after each par-
of work is 40 hours per week, with 70% reserved ticipant was enlightened about each research step
for ambulatory care. and agreed to participate through the signature of an
informed consent form. This research was approved
Participants by the Research Ethics Committee of the Centro de
Ciências da Saúde of the Universidade Federal de
The study population corresponded to dental surgeons Pernambuco, CAAE: 53378216.4.0000.5208. Ap-
that were performing clinic activities in the BHS and proval Number: 1.473.034/2016.
212 Rev Estomatol Herediana. 2017 Oct-Dic;27(4).
De-Souza FB, Costa IRB, Pinto LLS, Melo MMDC.
Data analysis the ranges 26-30 (6%), 16-20 (9,1%), 36-40 (9,1%).
The range of 6 to 10 years obtained the percentage of
It was structured the distribution of absolute and 15.2%.
relative frequencies of the studied sample, according
to different variables. Inferential statistical analysis Figure 1 shows the prevalence of musculoskeletal
was carried out to verify the association between disorders according to the anatomical region and its
pain/discomfort and some external variables to frequency. Considering the last 12 months, the most
the professional practice. For the association tests affected body areas regarding pain, discomfort or dor-
between these variable, it was used the Fisher’s mancy were neck area (56.75%); fist/hands/fingers
exact test and to measure the association force, the (54.06%); shoulders (51.35%) and lumbar region
odds ratio bruta (OR) was calculated as well as its (48.65%), taking into accountthe total sum of the an-
respective confidence interval at a level of 95% (CI swers ‘‘Often’’ and ‘‘Always’’. None of these condi-
of 95%). The margin of error used in the decisions tions possessed significant statistical association re-
of statistical tests was of 5%. The statistical program lated to the sex of the interviewees.
used was EPI info, version 7.
RESULTS
Regarding working hours, 91.89% of the dentists
From the total of 82 selected dentists from the eight work in a regimen of 8 or more hours per day. The
sanitary districts that form the health socio-geograph- fact of not practicing physical activity was informed
ic organization of the city of Recife, thirty-seven of by 54.05% of the interviewees. For this reason, when
them were interviewed for this study, which corre- carrying out the association test between the expo-
sponded to a percentage of 45.12% of the total in- sure to physical activities and the presence of pain/
tended. The high percentage of losses was caused, discomfort in different body areas, it was observed
for the most part, by the professional’s refusal to stop a significant statistically relationship in wrists/hands/
his clinical activities to answer the questionnaires. A fingers area (OR=0.195/ CI 95%; p=0.038), consider-
minority of the losses occurred due to the absence of ing that 85% of dentists which do not physical activi-
the professional in the work place at the time of the ty presented problems related to this area.
research due to vacations.
Among the daily activities external to professional
According to obtained data regarding sample charac- activity, computer use (56.76%) and the execution of
terization, from the 37 professionals interviewed, 29 household activities were the most related in the re-
(78.38%) were of the female sex and 8 (21.62%) of search (figure 2).
the male sex, with age raging from 29 to 65 years,
presenting a mean of 45.67 years old (standard devia-
tion – SD = 10.89) The majority of the interviewees Concerning the influence of these daily activities on
reported having the right hand as dominant (89.19%). the appearance of pain and/or muscular discomfort,
It was verified a mean of clinical activity time of tables 1 and 2 display association measures, regar-
25.51 years (SD=10.48%). ding neck, fists/hands/fingers, shoulders and lumbar
regions, considering that these were the most men-
The greater part of the interviewees (97.3%) affirmed tioned areas in the interview, as presented in figure 1.
having some type of musculoskeletal disorder related However, none of the tested associations demonstra-
to his/her professional activity, regardless of profes- ted to be statistically significant (p>0.05).
sional practice time. Only one interviewee with the
time of 12 years of work stated that they did not have
WRMSD. However, participants in the range of 11 to
15 years of work had the highest percentage of WR-
MSD (27.3%), followed respectively by the intervals
of 31-35 (24.2%) and 21-25 (18.2%). Lower percent-
ages of participants with WRMSD were observed for
Rev Estomatol Herediana. 2017 Oct-Dic;27(4). 213
Musculoskeletal disorders associated to dentists work activities in Brazilian primary health care
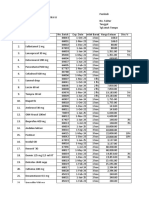
Table 1. Association between musculoskeletal disorders (pain/discomfort) in neck and fists/hands/ fingers regions and ex-
traprofessional activities in dentists. Recife, 2016.
Neck Fists / Hands / Fingers
Activity Presence of pain/Discomfort Presence of pain/Discomfort
n % p* OR n % p* OR
(IC=95%) (IC=95%)
Computer
Yes 17 80.95 0.317 1.931 16 76.19 0.293 1.92
Use No 11 68.75 (0.423- 10 62.5 (0.461-
8,813) 7.989)
Household Yes 16 84.21 0.195 2.666 14 73,68 0.457 1.4
Activities No 12 66.67 (0.551- 12 66.67 (0.34-5.764)
12.883)
* Fisher’s Exact Test
Table 2.– Association between musculoskeletal disorders (pain/discomfort) in Lumbar and Shoulders Regions and extra-
professional activities in dentists. Recife, 2016.
Lumbar Region Shoulders
Presence of Pain/Discomfort Presence of Pain/Discomfort
Activity p* OR
N % p* OR n %
(IC=95%) (IC=95%)
Computer Yes 13 61.9 0.348 1.625 12 57.14 0.108 2.933
Use No 8 50.0 (0.435- 5 31.25 (0.748-
6.068) 11.491)
Household Yes 11 57.89 0.574 1.1 10 52.63 0.306 1.746
Activities No 10 52.38 (0.299 – 7 38.89 (0.472-
4.042) 6.453)
* Fisher’s Exact Test
214 Rev Estomatol Herediana. 2017 Oct-Dic;27(4).
De-Souza FB, Costa IRB, Pinto LLS, Melo MMDC.
Figure 1. Prevalence and frequency of musculoskeletal disorders’ involvement in a sample of
dentists from the PHC network of the city of Recife-PE, Brazil, 2016.
Figure 2. Prevalence and activities external to the professional practice from a dentist’s
sample from the PHC network of the city of Recife-PE, Brazil, 2016.
Rev Estomatol Herediana. 2017 Oct-Dic;27(4). 215
Musculoskeletal disorders associated to dentists work activities in Brazilian primary health care
DISCUSSION can result in accumulation of work that is performed
in a non-ergonomic manner and whose consequences
The discoveries of this research settled a diagnosis on reflect in the professionals’ health. It was verified in
the occupational health of dentists belonging to the a similar research an average clinical activity of 12.2
PHC network of a metropolis from the northeast re- years, but still, recorded a WRMSD frequency in ap-
gion of Brazil and are according to countless studies proximately 60% of the participants (22).
when describing the WRMSD as the main problem
related to occupational health in workers involved In addition to professional practice time, working
with oral health (5-7). hours can also be an aggravating factor to the occu-
rrence of lesions. In a research realized in the city of
It was observed that women are responsible for great Fortaleza, Ceará, Brazil, 55% of the interviewees had
part of the dental workforce in city studied. The Per- a workload of more than 8 daily hours in the private
nambuco state has a population formed in its major- sector, also being possible to observe the detachment
ity by women (18). However, regardless the popula- of 60% of the professionals due to pain occurrences.
tion matter, women participation as workforce has In turn, in the city of Recife, 91.89% of the inter-
increased considerably in the different human tasks viewees reported to work 8 or more hours per day (6).
(19). In the dental area, specifically, this fact has been This result shows the great workload of the professio-
observed and confirmed by many researches (20-22). nals who work in the HPC ambit.
The average age found among the interviewees in
the city of Recife-PE was 45.67 years old, including The nature of the dental surgeon activity can expo-
both young and older professionals, with 29 years old se this professional to many nuisances and harmful
and 65 years old being minimum and maximum ages, factors during his/her working hours (24). The usual
respectively. From this group, the majority (97.3%) posture adopted by the dental surgeon is characteri-
related the presence of musculoskeletal symptoms. zed by maintaining the upper limbs in suspension,
In a study carried out with dental surgeons from the torso rotation and head flexion, forcing the cervical,
military police of Pernambuco, also with the applica- scapular and thoracic-lumbar musculature. This pos-
tion of questionnaires, similar data was found, with ture, in a repetitive manner, causes discomfort and
an average age of 45.81 years old and 84.1% of the disorders to the musculoskeletal and the peripheral
interviewees relating the presence of pain or discom- nervous systems and tends to provoke fatigue in the
fort.21 This great prevalence has been observed in oth- structures involved in its maintenance, with the possi-
er researches: 73% (5); 95% (6);70% (7); 60% (22); bility of causing acute or chronic lesions (25).
95.9% (23).
But how to explain the high prevalence of WRMSD
It is important to emphasize that the presence of in dentists that work with family health strategy,
WRMSD occurred independently of the time of pro- whose professional activities are not exclusively cli-
fessional practice, which ranged from 6 to 40 years. nical-ambulatory nature? According to the Brazilian
However, it is not possible to affirm that there is a policy regarding the HPC, the attributions of a den-
relationship between professional practice time and tal surgeon are intended not only to the performance
presence of WRMSD, since most of the respondents of dental clinical procedures but also the promotion
stated that they present symptoms. In addition, the of health collectively, locally and of mapping of the
type of study adopted did not allow evidence of such operational area. In spite of that, clinical attendance
relation, which requires other analytical approaches takes 70% of primary care dentists’ working hours,
and longitudinal study design. a considerable percentage represented almost always
by patient continuous and successive care (12). Con-
On the other hand, the experience of accumulat- sidering the great demand of patients directed to pu-
ed years can represent a path to be explored. In this blic health service, specifically in Recife, the stress
case, the average time of practice as a clinic dentist is and the intense work caused by a great number of
around 25 years, data which was found in this inves- clinical attendances, associated to intervals reduc-
tigation, and can indicate that the pains, dormancies tion between them, may have contributed to the high
or discomforts related to the most diverse body areas number of professionals affected by WRMSD in this
216 Rev Estomatol Herediana. 2017 Oct-Dic;27(4).
De-Souza FB, Costa IRB, Pinto LLS, Melo MMDC.
study. Dental practice causes dentists to work seated ciency found in his/her workplace.
for long hours, assuming at times incorrect postures
which in turn causes a mechanic compression on ana- For this reason, it can be observed that the occupations
tomic structures involved (2). Besides, the use of ins- can produce specific pathologies related to the type of
truments and devices together with task repeatability work performed, which demonstrates the importance
and excessive administrated force in certain procedu- of investigating the frequency of dental practice-rela-
res, expose these professionals to the development of ted musculoskeletal complaints. Prevention still is the
musculoskeletal lesions of occupational order. best way of fighting the onset of WRMSD; routine
habits alterations and work organization are attitudes
In the present research, the most affected body areas that need to be encouraged in order to obtain a better
regarding pain, discomfort or dormancy were neck, life quality (29,30).
fist/hands/fingers, shoulders and lumbar region. The-
se findings were similar to the ones obtained from Regarding this study limitation, methodological care
other investigations (5,7,22,26,27). These locations was taken so that the analyses produced would in-
represent body areas frequently activated during den- deed express the opinion reported by the research’s
tal practice. Dentists spend half their work time with subjects. However, possible information biases must
their neck flexed at an angle starting in 60 degrees, be considered. The high loss percentage interfered in
with their torso assuming angles superior to 30 de- the identification of associations of the considered
grees of inclination, with abductees shoulders (28). level. Nevertheless, it was possible to know the pre-
Thus, due to mechanic disadvantage imposed to ar- valence and describe the socioprofessional profile of
ticulations, it is necessary a greater effort to main- dental surgeons that work in PHC in Recife. Thus, it
tain these static postures. Consequently, the overuse is expected that this study findings contribute to ex-
of the anatomic structures and the lack of recovery pand the discussion about the problematic in question
time for this musculature, unleash musculoskeletal which is related to the improvement of health and
disorders, which can be avoided through the adoption work conditions of the worker in the PHC and that
of healthier lifestyle, such as: nutritional care, sports consequently impacts the service quality given to the
practice, daily stretching performance and ergonomic communities, which are targets of Recife’s PHC heal-
principles application (3). th interventions.
As a result, it was ascertained that great part (85%) of It was observed a high prevalence of WRMSD among
sedentary dentists presented musculoskeletal symp- dental surgeons of the city of Recife with neck; fist/
toms in the fist/hands/fingers area. This result points hands/fingers; shoulders and lumbar being the most
the need of adopting regular physical activities as affected body areas. There was no association be-
protective and strengthening measures of dentists’ tween the disorders and the external activities to
main work instrument anatomic structures: the hands. dental practice. Additionally, it was verified that the
Similar data was found in an investigation, that veri- adoption of regular physical activity can be a pro-
fied the absence of physical activity can have a ne- tection factor against the WRMSD related to the fist/
gative influence upon the professional’s health (20). hands/fingers area.
In the present study, extraprofessional activities did
not present a relationship with the painful symptoms
chart reported by dentists, leading to believe that such Corresponding author
relation of symptoms was caused strictly by non-er-
gonomic maneuvers associated with professional ac- Fábio Barbosa de Souza
tivity, corroborating with other studies (7,22). These E-mail: fabiobsdsouza@gmail.com
maneuvers are realized in ordinary manner when the
work environment does not cooperate with the pro- REFERENCES
fessional’s health integrity maintenance, hazarding
his/her physical and mental well-being and leading 1. Castro SL, Figlioli MD. Ergonomia aplicada à den-
the professional to conserve inappropriate postures tística: avaliação da postura e posições de trabalho do
and movements to compensate the ergonomic defi- cirurgião-dentista destro e da auxiliar odontológica em
Rev Estomatol Herediana. 2017 Oct-Dic;27(4). 217
Musculoskeletal disorders associated to dentists work activities in Brazilian primary health care
procedimentos restauradores. JBC J Bras Clin Estet 2002; 36: 307-312.
Odontol. 1999; 3(4): 56-62. 18. Instituto Brasileiro de Geografia e Estatística. Censo
2. Feron LO, Boniatti CM, Arruda FZ, et al. Lesões por demográfico 2012: resultados preliminares. Rio de Ja-
esforço repetitivo em cirurgiões-dentistas: uma re- neiro, RJ: IBGE; 2012.
visão da literatura. Rev Cienc Saude. 2014; 16: 79-86. 19. Moimaz, SAS, Saliba NA, Blaci MRB. A força
3. Medeiros UV, Segatto GG. Lesões por esforços repeti- do trabalho feminino na odontologia, em Araça-
tivos (LER) e distúrbios osteomusculares (DORT) em tuba – SP. Appl Oral Sci. 2003; 11: 301-5.
dentistas. Rev Bras Odontol. 2012; 69: 49-54. 20. Amaral RMS, Pires RCCP. Ergonomia e saúde:
4. Fish DR, Morris-Allen DM. Musculoskeletal disor- percepção de sintomas osteomusculares entre os ci-
ders in dentists. N Y State Dent J.1998; 64(4): 44-48. rurgiões-dentistas de Betim-MG, 2008. Nov@ Rev
5. Rabiei M, Shakiba M, Shahreza HD, Talebzadeh M. Cient, 2013; 2: 1-13.
Musculoskeletal disorders in dentists. Int J Occup 21. Santos RLX, Silva Junior EZ, Andrade RAR, Andrade
Hyg. 2012; 4(1): 36-40. ESS. Lesão por esforços repetitivos (LER/DORT) em
6. Souza IMA,Vasconcelos TB, Bastos VPD, Farias cirurgiões-dentistas da clínica odontológica da polícia
MSQ. Avaliação da dor e lesões ocasionadas pelo tra- militar de Pernambuco. Odontol. Clín. Cient. 2013;
balho em cirurgiões-dentistas na cidade de Fortaleza/ 12: 177-187.
Ce. Rev Fisioter S Fun Fortaleza. 2012; 1(2): 35-41. 22. Dantas FFO, Lima KC. The relationship between
7. Rehman B, Aslam A, Ali A, Tari A. Ergonomic ha- physical load and musculoskeletal complaints among
zards to dental surgeons: a cross-sectional study. Pa- brazilians dentists. Appl Ergon. 2015; 47:93-98.
kistan Oral & Dent J. 2016; 36: 168-171. 23. Bitencourt RS, Work MIR. Prevalence of discomfort/
8. Conrado CA, Tumang AJ, Gasparetto A, et al. Ava- pain complaints and related factors in dental pro-
liação da aplicação de conceitos de higiene e ergono- fessionals of the public health service in Araucária,
mia em consultórios odontológicos. Rev. ABO Nac. Paraná, Brazil. Work. 2012;41 Suppl 1:5715-7. doi:
1996; 4(1): 40-43. 10.3233/WOR-2012-0928-5715.
9. Rio LMSP. Ergonomia odontológica. Rev do CROMG. 24. Szymanska J. Disorders of musculoskeletal system
2000; 6: 28-33. among dentists from the aspect of ergonomics and
10. Brasil. Ministério da Saúde, Secretaria de Atenção à prophylaxis. Ann Agric Environ Med. 2002;9(2):169-
Saúde, Clínica ampliada e Compartilhada. O Huma- 73.
niza SUS na atenção básica. Brasília: Ministério da 25. Brandão TMC. Avaliação dos aspectos ergonômi-
Saúde; 2009. cos em odontologia: Lesão por esforços repetitivos
11. Buchan J, Fronteira I, Dussault G. Continuity and e distúrbios osteomusculares em cirurgiões dentistas.
change in human resources policies for health: lessons Goiânia, GO: Faculdade Sul Americana; 2015.
from Brazil. Hum Resouc Health. 2011; 9: 1-13. 26. Tzu-Hsien L, Yen-Chun L, Tien-Yu H, et al. Preva-
12. Brasil, Ministério da Saúde. Secretaria de Atenção à lence of and risk factors for musculoskeletal com-
Saúde, Departamento de Atenção Básica. Política na- plaints among taiwanese dentists. J Dent Sci. 2012;7:
cional de atenção básica. Brasília: Ministério da Saú- 65-71. Doi: https://doi.org/10.1016/j.jds.2012.01.009
de; 2006. 27. Abbas SB, Qazi SR, Iftikhar S, Iqbal MU. Musculo-
13. Instituto Brasileiro de Geografia e Estatística. Censo skeletal disorders among dentists and dental students.
demográfico 2010: resultados preliminares. Rio de Ja- Pakistan Oral Dent J. 2015; 35, 461-465.
neiro, RJ: IBGE; 2010. 28. Marklin RW, Cherney K. Working postures of dentists
14. Araújo MA, Paula MVQ. LER/DORT: um grave and dental hygienists. J Calif Dent Assoc. 2005; 33:
problema de saúde pública que acomete os cirur- 133-136.
giões-dentistas. Rev APS. 2003; 6: 87-93. 29. Bachiega JC. Sintomas de distúrbios osteomusculares
15. Almeida LGN, Torres, SC, Dos Santos CMF. Riscos relacionados à atividade de cirurgiões-dentistas bra-
ocupacionais na atividade dos profissionais de saúde sileiros. São Paulo, SP: Universidade Nove de Julho;
da atenção básica. Rev Enferm Contemp. 2012; 1: 2009.
142-154. 30. Silva HPL, Jesus CS. Sistemas osteomusculares em
16. RECIFE, Governo Municipal, Secretaria de Saúde do cirurgiões-dentistas da rede pública. Rev AMRIGS.
Recife, Secretaria Executiva de Coordenação Geral, 2013; 57: 44-48.
Gerência Geral de Planejamento. Plano Municipal de
Saúde 2014 – 2017. Recife, PE: Secretaria de Saúde
do Recife; 2014.
17. Pinheiro FA, Troccoli, BT, Carvalho CV, Validação
do Questionário Nórdico de Sinto-mas Osteomuscu- Recibido: 13-06-2016
lares como medida de morbidade. Rev Saude Publica. Aceptado: 15-10-2017
218 Rev Estomatol Herediana. 2017 Oct-Dic;27(4).
You might also like
- 8.A Manual para Asistentes DentalesDocument202 pages8.A Manual para Asistentes DentalesJuliiz Jiimenez88% (8)
- SHEM 10 Incident Reporting Rev 00 Jan 07 1Document54 pagesSHEM 10 Incident Reporting Rev 00 Jan 07 1Anonymous iI88LtNo ratings yet
- Psych Drug StudyDocument5 pagesPsych Drug StudyLorina Lynne Apelacio100% (4)
- 3 Construction Rating Audit Protocol PDFDocument30 pages3 Construction Rating Audit Protocol PDFAshimolowo BabatundeNo ratings yet
- Kuroinca Rules BhpoDocument15 pagesKuroinca Rules BhpoIzunahui Tomas Yami TakeshiNo ratings yet
- 01 EsDocument10 pages01 Eshf22-0277No ratings yet
- Modificación de La Dimension VerticalDocument7 pagesModificación de La Dimension VerticalElizabeth Mamani RamosNo ratings yet
- 03 EsDocument15 pages03 Eshf22-0277No ratings yet
- A131345 Montenegro A Satisfaccion Laboral de Los Odontologo 2020 TesisDocument21 pagesA131345 Montenegro A Satisfaccion Laboral de Los Odontologo 2020 TesisAbraham CorzoNo ratings yet
- Atencion en Podologia MedicaDocument12 pagesAtencion en Podologia MedicaKevin GodoyNo ratings yet
- Factores BalarezoRazzeto JoseDocument65 pagesFactores BalarezoRazzeto JoseSANTIAGO GONZALESNo ratings yet
- EUA Tellez Temple UniversityDocument15 pagesEUA Tellez Temple UniversitySebas barreiraNo ratings yet
- Estrategia de Intervención para Disminuir El Riesgo PosturalDocument15 pagesEstrategia de Intervención para Disminuir El Riesgo Posturalmarianahdez2182No ratings yet
- MetodologiaDocument36 pagesMetodologiaPilar Caceres VelasquezNo ratings yet
- Prevención en Salud Periodontal: Recomendaciones Actualizadas y Estatus Del Conocimiento Directamente Aplicable Al Entorno MexicanoDocument9 pagesPrevención en Salud Periodontal: Recomendaciones Actualizadas y Estatus Del Conocimiento Directamente Aplicable Al Entorno MexicanoDrismatoperNo ratings yet
- Universidad de Carabobo Facultad de Odontología Dpto. de Formación Integral Del Hombre Investigación en OdontologíaDocument7 pagesUniversidad de Carabobo Facultad de Odontología Dpto. de Formación Integral Del Hombre Investigación en OdontologíaCesar LopezNo ratings yet
- Disartria Evidencias y Guías Clínicas, MelleDocument14 pagesDisartria Evidencias y Guías Clínicas, Mellebz4dzwpzw8No ratings yet
- 02 EsDocument10 pages02 Eshf22-0277No ratings yet
- 1348 9585 58 389.en - EsDocument15 pages1348 9585 58 389.en - EsDayuma VillavicencioNo ratings yet
- Disartria. Práctica Basada en La EvidenciaDocument14 pagesDisartria. Práctica Basada en La EvidenciaTécnicos CredineNo ratings yet
- 218-Texto Del Artículo-279-1-10-20180523Document8 pages218-Texto Del Artículo-279-1-10-20180523Dra. Pamela MontillaNo ratings yet
- Instrumentos de Medida Más Frecuentemente Empleados en El TCEDocument7 pagesInstrumentos de Medida Más Frecuentemente Empleados en El TCEMario Alberto Tellez RamosNo ratings yet
- Prevalencia de Sintomas Asociados A Trastornos Musculoesqueléticos en Estudiantes de Odontologia PDFDocument6 pagesPrevalencia de Sintomas Asociados A Trastornos Musculoesqueléticos en Estudiantes de Odontologia PDFLidia Muñoz CastroNo ratings yet
- Romerorfo 1112017Document5 pagesRomerorfo 1112017paulasure97No ratings yet
- Artículo 2 de OsteoporosisDocument10 pagesArtículo 2 de OsteoporosisDany ValienteNo ratings yet
- DescriptivaDocument8 pagesDescriptivaYeraldim LopezNo ratings yet
- Aplicación Clínica de Los Parámetros Estéticos en Odontología RestauradoraDocument8 pagesAplicación Clínica de Los Parámetros Estéticos en Odontología RestauradoraJorge MelgarNo ratings yet
- 125-Texto Del Artículo-979-1-10-20211222Document6 pages125-Texto Del Artículo-979-1-10-20211222Brando mallma castroNo ratings yet
- Factores Biomecánicos en La Rehabilitación Por Prótesis Parcial Fija Sobre Implantes MicrodentDocument7 pagesFactores Biomecánicos en La Rehabilitación Por Prótesis Parcial Fija Sobre Implantes MicrodentEduardo Ubillus DavilaNo ratings yet
- Ergonomía, Una Ciencia Que Aporta Al Bienestar Odontológico PDFDocument5 pagesErgonomía, Una Ciencia Que Aporta Al Bienestar Odontológico PDFLiliana Miranda ANo ratings yet
- CAP I y II Corregido.Document19 pagesCAP I y II Corregido.Cesar LopezNo ratings yet
- Enfermería PrevenciónDocument11 pagesEnfermería Prevenciónmaria alejandra libreros gilonNo ratings yet
- Medisur 1727-897X: E-Issn: Mikhail@Infomed - Sld.CuDocument7 pagesMedisur 1727-897X: E-Issn: Mikhail@Infomed - Sld.CuJorge Saturno OrtizNo ratings yet
- Prevalencia de Sintomas Musculos Esqueleticos y Su Relacion Con Los Factores Ocupacionales en El Personal de La Salud de Una ClinicaDocument19 pagesPrevalencia de Sintomas Musculos Esqueleticos y Su Relacion Con Los Factores Ocupacionales en El Personal de La Salud de Una Clinicabryan trianaNo ratings yet
- La Discapacidad en Pacientes Cervicalgia MecánicasDocument7 pagesLa Discapacidad en Pacientes Cervicalgia MecánicasAntony YqNo ratings yet
- 198 621 2 PBDocument6 pages198 621 2 PBMoises FF CardenasNo ratings yet
- Artroplastia de CaderaDocument3 pagesArtroplastia de CaderaEvelyn Carhuachin GalarzaNo ratings yet
- Odontologia PreventivaDocument11 pagesOdontologia Preventivatania_ramosgarciaNo ratings yet
- Trabajo FinalDocument26 pagesTrabajo FinalanybustamantefernandezNo ratings yet
- FisioterapiaDocument14 pagesFisioterapiaUtushamash GrupoNo ratings yet
- Ortopedia y Traumatología: Epidemiología de Lesiones Ortopédicas de Origen Laboral en Un Hospital de ManizalesDocument9 pagesOrtopedia y Traumatología: Epidemiología de Lesiones Ortopédicas de Origen Laboral en Un Hospital de ManizalesMaEsther CMNo ratings yet
- 04 OssaDocument10 pages04 OssaLucyFloresNo ratings yet
- Línea Del TiempoDocument3 pagesLínea Del TiempoDiana JuarezNo ratings yet
- Caries DentalDocument46 pagesCaries DentalMELANYNo ratings yet
- Introducción y JustificaciónDocument9 pagesIntroducción y JustificaciónYuliana Marcela Sarria MontañoNo ratings yet
- Prevención de La Caries: Recomendaciones Actualizadas y Estatus Del Conocimiento Directamente Aplicable Al Entorno MexicanoDocument12 pagesPrevención de La Caries: Recomendaciones Actualizadas y Estatus Del Conocimiento Directamente Aplicable Al Entorno MexicanoDrismatoperNo ratings yet
- Odontologia Basada en La EvidenciaDocument6 pagesOdontologia Basada en La EvidenciaSantyLara001No ratings yet
- Tesis Dra. Marlen Lázara Vázquez González (Mayo2019)Document67 pagesTesis Dra. Marlen Lázara Vázquez González (Mayo2019)Juan De La Cruz OrtizNo ratings yet
- V de Gowin PDFDocument1 pageV de Gowin PDFsofiasequera1980No ratings yet
- Original 2Document7 pagesOriginal 2Saray MAHINo ratings yet
- IndicesDocument12 pagesIndicesJohanna PinedaNo ratings yet
- Efecto de La Aplicación de Un Programa de Gimnasia Laboral para Reducir La Prevalencia de Cervicalgia en Estudiantes de OdontologíaDocument10 pagesEfecto de La Aplicación de Un Programa de Gimnasia Laboral para Reducir La Prevalencia de Cervicalgia en Estudiantes de OdontologíaCaroSanReyNo ratings yet
- Artículo Unidad 1.5 Nivel de Conocimiento y Práctica de Medida de Bioseguridad en El HospitalDocument8 pagesArtículo Unidad 1.5 Nivel de Conocimiento y Práctica de Medida de Bioseguridad en El HospitalLuis Vara GarcíaNo ratings yet
- DescriptivaP1 PublicadoDocument8 pagesDescriptivaP1 PublicadogarciadeluisaNo ratings yet
- Rev Clase II. BAccetti - Cozza2006.en - EsDocument12 pagesRev Clase II. BAccetti - Cozza2006.en - EsLIZETH NATHALIA TOLOZA OCHOANo ratings yet
- Prevención de Trastornos Musculoesqueléticos en OdontólogosDocument10 pagesPrevención de Trastornos Musculoesqueléticos en OdontólogosAnonymous rFgfvTTNo ratings yet
- Epidemiologia de Los Principales Problemas de SaludDocument44 pagesEpidemiologia de Los Principales Problemas de Saludelizabeth garciaNo ratings yet
- Dialnet ConocimientosYPracticasSobreBioseguridadEnOdontolo 6194276 PDFDocument5 pagesDialnet ConocimientosYPracticasSobreBioseguridadEnOdontolo 6194276 PDFJhon Lopez SNo ratings yet
- Medicamentos AdminDocument2 pagesMedicamentos Adminjesus alejandro guerra dazaNo ratings yet
- Diapositivas Esguince de Tobillo, Eliumar GarridoDocument18 pagesDiapositivas Esguince de Tobillo, Eliumar Garridoyeymar1311No ratings yet
- Impacto Del Programa de IntervencionDocument14 pagesImpacto Del Programa de IntervencionYuri EpNo ratings yet
- Epidemiologia de Los Principales Problemas de SaludDocument46 pagesEpidemiologia de Los Principales Problemas de Saludelizabeth garciaNo ratings yet
- Allison Malm Hs Pe ResumeDocument2 pagesAllison Malm Hs Pe Resumeapi-334423293No ratings yet
- Pinxel-2 Microneedle RF MachineDocument18 pagesPinxel-2 Microneedle RF MachineAlex SongNo ratings yet
- St. Teresa's Hospital 聖德肋撒醫院: Common Chargeable Items 常用項目收費Document27 pagesSt. Teresa's Hospital 聖德肋撒醫院: Common Chargeable Items 常用項目收費Hemkerovner Keresztszegh von Kolowrat-KrakowskyNo ratings yet
- Types of ScaffoldingDocument21 pagesTypes of ScaffoldingKashmir Ka Bata Abdul GHAFFAR LAL DIN CHNo ratings yet
- Traumatic InjuriesDocument2 pagesTraumatic InjuriesMarionne MarianoNo ratings yet
- BGH Case SlipsDocument7 pagesBGH Case SlipsLoungayvan BatuyogNo ratings yet
- Health Economics Dissertation TopicsDocument8 pagesHealth Economics Dissertation TopicsBuyingPapersOnlineCollegeRochester100% (1)
- Wahyuningrum Indah Saraswati-01206321A - Tugas P.farprak - Penyimpanan ObatDocument50 pagesWahyuningrum Indah Saraswati-01206321A - Tugas P.farprak - Penyimpanan ObatSaraswati Indah ArumNo ratings yet
- An Organization For Women: Beijing Conference On WomenDocument2 pagesAn Organization For Women: Beijing Conference On WomenJohn ClarenceNo ratings yet
- Safety Data Sheet: Section 1. IdentificationDocument12 pagesSafety Data Sheet: Section 1. Identificationdavid montoyaNo ratings yet
- Online Exam Math50 ANOVA PDFDocument1 pageOnline Exam Math50 ANOVA PDFMaCristina Acidera AroganteNo ratings yet
- Consenso Rehabilitacion IOIDocument6 pagesConsenso Rehabilitacion IOIMatias Soto ParraNo ratings yet
- Looking Within: Self-Perceived Professional Strengths and Limitations of Psychotherapists in IndiaDocument17 pagesLooking Within: Self-Perceived Professional Strengths and Limitations of Psychotherapists in IndiaPrerna singhNo ratings yet
- Preprosthetic SurgeryDocument21 pagesPreprosthetic SurgeryAda MilanovićNo ratings yet
- Carter Cleaning Company - The New Training Program: Case SummaryDocument4 pagesCarter Cleaning Company - The New Training Program: Case SummaryCharvi GosaiNo ratings yet
- Chronic Pelvic Pain Without Obvious Pathology in Women Personal Observations and A Review of The ProblemDocument49 pagesChronic Pelvic Pain Without Obvious Pathology in Women Personal Observations and A Review of The ProblemRedfalconNo ratings yet
- LOCTITE EA 9309 MsdsDocument12 pagesLOCTITE EA 9309 MsdsMohammad shahriar jinnahNo ratings yet
- Askep PankreatitisDocument76 pagesAskep PankreatitisTomo PratamaNo ratings yet
- Efektifitas Terapi Musik Klasik Terhadap Penurunan Tingkat HalusinasiDocument9 pagesEfektifitas Terapi Musik Klasik Terhadap Penurunan Tingkat HalusinasiAnis RahmaNo ratings yet
- Fnac of Thyroid - 102717Document13 pagesFnac of Thyroid - 102717Lal RuattlingaNo ratings yet
- 13-17 Week Theories-WPS OfficeDocument14 pages13-17 Week Theories-WPS OfficeMauri B. DayagNo ratings yet
- ZEESHAN ALI RESUME 2021 Safety AdvisorDocument4 pagesZEESHAN ALI RESUME 2021 Safety AdvisorShahid BhattiNo ratings yet
- Soal PAS B.Ing Kelas 9 30 SoalDocument5 pagesSoal PAS B.Ing Kelas 9 30 SoalHusna istianaNo ratings yet
- BDP For ChildrenDocument7 pagesBDP For ChildrenjomarNo ratings yet
- Caregiving Grade 9Document20 pagesCaregiving Grade 9Markus Amevill100% (1)
- ReportDocument6 pagesReportShobhitNo ratings yet
- Slosson Intelligence Test (Sit) Interpretation Examiner: M.A.B Identifying InformationDocument1 pageSlosson Intelligence Test (Sit) Interpretation Examiner: M.A.B Identifying InformationFarrukh Ali KhanNo ratings yet