Professional Documents
Culture Documents
Acute or Chronic Penetrate: Pylori
Uploaded by
Sid0 ratings0% found this document useful (0 votes)
12 views5 pagesThis document discusses peptic ulcer disease, including its causes, symptoms, diagnosis and management. The main causes are infection with Helicobacter pylori bacteria and use of non-steroidal anti-inflammatory drugs. Common symptoms include recurrent epigastric pain related to meals. Diagnosis involves endoscopy to identify ulcers. Treatment focuses on eradicating H. pylori infections using proton pump inhibitors and antibiotics, managing NSAID use, and surgery for complications like perforation or bleeding. Successful treatment of H. pylori prevents most recurrences of peptic ulcers.
Original Description:
Derail description of peptic ulcer
Original Title
peptic ulcer
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses peptic ulcer disease, including its causes, symptoms, diagnosis and management. The main causes are infection with Helicobacter pylori bacteria and use of non-steroidal anti-inflammatory drugs. Common symptoms include recurrent epigastric pain related to meals. Diagnosis involves endoscopy to identify ulcers. Treatment focuses on eradicating H. pylori infections using proton pump inhibitors and antibiotics, managing NSAID use, and surgery for complications like perforation or bleeding. Successful treatment of H. pylori prevents most recurrences of peptic ulcers.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views5 pagesAcute or Chronic Penetrate: Pylori
Uploaded by
SidThis document discusses peptic ulcer disease, including its causes, symptoms, diagnosis and management. The main causes are infection with Helicobacter pylori bacteria and use of non-steroidal anti-inflammatory drugs. Common symptoms include recurrent epigastric pain related to meals. Diagnosis involves endoscopy to identify ulcers. Treatment focuses on eradicating H. pylori infections using proton pump inhibitors and antibiotics, managing NSAID use, and surgery for complications like perforation or bleeding. Successful treatment of H. pylori prevents most recurrences of peptic ulcers.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
conditions, particularly thyroid disease, may be present.
There is a
fourfold increase in gastric cancer.
Peptic ulcer disease
' Peptic ulcer' means an ulcer in the lower oesophagus, stomach or
duodenum, in the jejunum after gastrojejunostomy or, rarely, in the
ileum adjacent to a Meckel's diverticulum. Ulcers in the stomach or
duodenum may be acute or chronic; both penetrate the museularis
mucosae but acute ulcers show no evidence of fibrosis. Erosions do
not penetrate the muscularis mucosae.
Gastric and duodenal ulcer
The prevalence of peptic ulcer is decreasing in many Western
communities as a result of H. pylori eradication therapy but it
remains high in d eveloping countries. The male to female ratio for
duodenal ulcer varies from 5: 1 to 2: 1, whilst that for gastric ulcer
is ~ 2 :1.
Chronic gastric ulcer is usually single; most are situated on the
lesser curve within the antrum. Duodenal ulcer usually occurs in the
first part of the duodenum just distal to the junction of pyloric and
duodenal mucosa. Gastric and duodenal ulcers coexist in 10% of
patients and mul.tiple ulcers occur in 10-15%.
H. pylori: In the UK, the prevalence of H. pylori infection rises with
age (reaching 50% in those aged >50); in the developing world, it
affects up to 90%. Infections are probably acquired in childhood by
person-to-person contact. Most colonised people remain healthy and
asymptomatic. Around 90% of duodenal ulcer patients and 70% of
gastric ulcer patients are infected with H. pylori; the re maining 30%
of gastric ulcers are due to NSAIDs.
H. pylori is a motile Gram-negative organism that uses multiple
flagellae to burrow beneath the epithelial mucus layer. Here the pH
is nearly neutral and any acidity is buffered by the organism's pro-
duction of ammonia from urea. H. pylori exclusively colonises
gastric-type epithelium and is only found in the duodenum at
patches of gastric metaplasia. It stimulates chronic gastritis by pro-
voking an inflammatory response in the epithelium.
In most people, H. pylori causes antral gastritis with depletion of
somatostatin. The subsequent hypergastrinaemia stimulates parietal
cell acid production, but usually without clinical consequences. In a
few patients, particularly smokers, this process is exaggerated,
leading to duodenal ulceration. The pathogenesis of gastric ulcer is
less clear but H. pylori probably acts by reducing gastric mucosa!
resistance to acid and pepsin. Occasionally, H. pylori causes a pan-
gastritis, leading to gastric atrophy and hypochlorhydria, with bac-
terial proliferation in the stomach, predisposing to gastric cancer.
NSAIDs: See page 789.
Smoking: This increases the risk of gastric and, to a lesser extent,
duodenal ulcer. Once the ulcer has formed, it is more likely to cause
complications and less likely to heal if the patient smokes.
Clinical features and investigations
Peptic ulcer disease is a chronic condition with spontaneous relapse
and remission extending over decades. Duodenal and gastric ulcers
share common symptoms:
• Recurrent episodes of epigastric pain in relation to meals.
• Occasionally, vomiting; persistent daily vomiting suggests gastric
outlet obstruction.
In one-third of patients, especially elderly subjects taking NSAIDs,
the history is less characteristic. Pain may be absent or experienced
only as vague epigastric unease. Occasionally, the only symptoms
are anorexia and nausea, or a sense of undue repletion after meals.
The ulcer may even be 'silent', presenting with anaemia from chronic
undetected blood loss, haematemesis or acute perforation. The diag-
nostic value of individual symptoms of ulcer disease is poor.
Endoscopy is the preferred investigation. Gastric ulcers may occa-
sionally be malignant and therefore must always be biopsied and
followed up to ensu.r e healing.
Patients should be screened for H. pylori infection (Box 12.7). Some
tests requi.r e endoscopy; others are non-invasive. Overall, breath or
faecal antigen tests are best because of their accuracy, simplicity and
non-invasiveness.
Management
The aims of management are to relieve symptoms, induce healing
and prevent recurrence.
H. pylori eradication: All patients with acute or chronic duodenal
ulcer disease and those with gastric ulcers who are H. pylori-positive
should receive eradication therapy. This hea ls ulcers, prevents
12.7 ll111G111 tar . . dllli,lD 111 of ff. _ , II.....
Test Adwa11tages Dlllclnntages
Non-Invasive
Serology Rapid office kits Lacks sensitivity and
available; good for specificity; cannot differentiate
population studies current from past infection
1
3c urea breath High sensitivity and Requires expensive mass
tests specificity spectrometer
Faecal antigen test Cheap, > 95% specificity Acceptability
Invasive (antral biopsy)
Histology Sensitivity and specificity False negatives occur; takes
several days to process
Rapid urease tests Cheap, quick; > 95% 85% sensitivity
specificity
Microbiological 'Gold standard'·• defines Slow Md laborious; lacks
culture antibiotic sensitivity sensitivity
relapse and elimina tes the need for long-term treatment in >90% of
patients. A PPI is taken with two antibiotics (from amoxicillin, clari-
thromycin and metronidazole) for 7 days. First-line therapy is a PPI
(twice daily), clarithromycin 500 mg twice daily, and amoxicillin
1 g twice daily or metronidazole 400 mg twice daily, for 7 days.
Compliance, side-effects (usually diarrhoea, nausea, vomiting) and
metroni-d azole resistance iinfluence success rates.
Patients who remain infected after initial therapy should be
offered :second-line therapy. For those who are still colonised after
two treatments, the choice lies between a third attempt (guided by
antibiotic sensitivity testing) and long-term acid suppression.
H. pylori and NSAIDs are independent risk factors for ulcers, and
patients requiring Jong-term NSAID therapy should fi rst undergo
eradication therapy to reduce ulcer risk. Subsequent co-prescription
of a PPI with the NSAlD is ad vised but is not always necessary for
patients being given low-dose aspirin.
General measures: Cigarette smoking, aspirin and NSAIDs should
be avoided. Alcohol in moderation is no t harmful and no special
dietary advice is required.
Maintena nce treatt11e11t: This should not be necessary after suc-
cessful H. pylori eradication.
Surgica l treah 11e11 t: Surgery is now rarely required for peptic
ulcer, unless there is perforation, persis ting haemorrhage, gastric
outflow obstruction or persisting or recurrent ulcer after medical
treatment. Non-healing gastric ulcer is treated by partial gas-
trectomy, in which the uJcer and the ulcer-bearing area of the stom-
ach are :resected to exclude an underlying cancer. In the emergency
situation, biopsies are taken, and then 'unde r-running' the ulcer for
bleeding or 'oversewing' (patch repair) for perforation is sufficient.
Complications of peptic ulcer
Perforation: This allows stomach contents to escape into the peri-
toneum, causing peritonitis. It is more common in duodena] than in
gastric ulcers. About one-quarter of cases •occur in acute ulcers, often
with NSAIDs. It causes:
• Sudden, severe pain, often the first sign of ulcer, starting in the
upper abdomen and becoming generalised. Shoulder tip pain due
to diaphragmatic irritation, shallow respiration due to pain, and
shock are common. • Generalised rigidity. • Absent bowel sounds.
• Los:s of liver dullness due to gas under the diaphragm.
Rigidity persists, and although pain may temporarily improve,
the patient's condition later deteriorates with general peritonitis.
In at least 50% of cases, an erect CXR shows free air beneath the
diaphragm. If not, a water-soluble contrast swallow will confirm
perforation.
After resuscitation, the acute perforation is closed surgically.
Following surgery, H. pylori should be treated (if present) and
NSAIDs avoided. The mortality from perforation is 25%, reflecting
the age and comorbidity of the popuJation affected.
Gastric 011tlet obstn,ction: The most common cause is an ulcer
near the pylorus, but occas ional cases are due to antral cancer or
adult hypertrophic pyloric stenosis. Clinical features include:
• Nausea. • Vomiting of large quantities of gastric content.
• Abdominal distension.
Examination reveals wasting, dehydration and a succussion
splash persisting 4 hrs or more after the last meal. Visible gastric
peristalsis is diagnostic.
Investigations show:
• Low serum chloride and potassium. • Raised bicarbonate and urea:
dehydration results in enhanced renal absorption of Na• in exchange
for H· and paradoxical aciduria. • Nasogastric aspiration of at least
200 mL after an overnight fast: suggests the diagnosis. • Endoscopy:
performed after the stomach has been emptied by wide.bore
nasogastric tube.
Management includes:
• Nasogastric suction and the administration of large volumes of IV
isotonic saline with potassium. • PPis: may heal ulcers, relieve
pyloric oedema and overcome the need for surgery. • Balloon dilata-
tion of ben ign stenosis: may be possible. • Partial gastrectomy after
a 7-day period of nasogastric aspiration: necessary in other patients.
Bleeding: See pages -116-418.
You might also like
- Neutrophils: GastritisDocument16 pagesNeutrophils: GastritisUuhhNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Peptic UlcerDocument31 pagesPeptic UlcerHarpal Bajwa0% (1)
- Disease of StomchDocument43 pagesDisease of StomchHero StoreNo ratings yet
- Peptis Ulcer-Bs TâmDocument27 pagesPeptis Ulcer-Bs TâmÁnh PhạmNo ratings yet
- Peptic Ulcer Disease: Causes, Symptoms, and TreatmentDocument3 pagesPeptic Ulcer Disease: Causes, Symptoms, and TreatmentleahraizaNo ratings yet
- MD Guide to the Stomach and DuodenumDocument27 pagesMD Guide to the Stomach and Duodenumraed faisalNo ratings yet
- Peptic Ulcer Disease: Palangka Raya University Faculty of MedicineDocument70 pagesPeptic Ulcer Disease: Palangka Raya University Faculty of MedicineMITHA100% (1)
- H. Pylori CSSDocument26 pagesH. Pylori CSStiurNo ratings yet
- Gastric Ulcers: Presented By: Dr. Jawaria Memon & Dr. Deep KumarDocument31 pagesGastric Ulcers: Presented By: Dr. Jawaria Memon & Dr. Deep KumarDeep KhemaniNo ratings yet
- Peptic Ulcer Disease: Kalyanakrishnan Ramakrishnan, MD, Frcse, and Robert C. Salinas, MDDocument8 pagesPeptic Ulcer Disease: Kalyanakrishnan Ramakrishnan, MD, Frcse, and Robert C. Salinas, MDMonika WerdiningsihNo ratings yet
- 2 Gastric and Duodenal Peptic Ulcer Disease 2Document35 pages2 Gastric and Duodenal Peptic Ulcer Disease 2rayNo ratings yet
- Peptic Ulcer DiseaseDocument98 pagesPeptic Ulcer DiseaseOmar MohammedNo ratings yet
- Helicobacter Pylori Infection and Peptic UlcersDocument30 pagesHelicobacter Pylori Infection and Peptic UlcerstiurNo ratings yet
- Peptic UlserDocument8 pagesPeptic UlserSubhanshu DadwalNo ratings yet
- Disorders of The Stomach and DuodenumDocument42 pagesDisorders of The Stomach and DuodenumMillicent KajaraNo ratings yet
- Peptic Ulcer DiseaseDocument22 pagesPeptic Ulcer DiseasebhibhiNo ratings yet
- Stomach Ulcers (Peptic Ulcers)Document25 pagesStomach Ulcers (Peptic Ulcers)Irtza MajeedNo ratings yet
- Peptic Ulcer: by Dr.A.Vijay Anand Dept. of SurgeryDocument79 pagesPeptic Ulcer: by Dr.A.Vijay Anand Dept. of Surgeryvjanand07No ratings yet
- Evidence-Based Treatment of Peptic Ulcer DiseaseDocument9 pagesEvidence-Based Treatment of Peptic Ulcer DiseaseRandi AnugerahNo ratings yet
- Gastrointestinal Diseases - Part 1: Symptoms, Causes and Treatments of Common GI DisordersDocument27 pagesGastrointestinal Diseases - Part 1: Symptoms, Causes and Treatments of Common GI Disordersglenn johnstonNo ratings yet
- Exmd 509 Mcgill Stomach 2016Document36 pagesExmd 509 Mcgill Stomach 2016Sora OhNo ratings yet
- DYSPHAGIADocument76 pagesDYSPHAGIASaurabh AgarwalNo ratings yet
- Complication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaDocument76 pagesComplication of Peptic Ulcer: Department of Surgery S. S. Medical College Rewa and Associate GMH and SGMH RewaBrajesh MouryaNo ratings yet
- Esophageal StrictureDocument6 pagesEsophageal StrictureŽäíñäb ÄljaÑabìNo ratings yet
- Peptic UlcerDocument59 pagesPeptic UlcerfloramaeyecyecNo ratings yet
- Peptic Ulcer Disease: by Parthevan RajasingamDocument33 pagesPeptic Ulcer Disease: by Parthevan RajasingamNinaNo ratings yet
- Peptic Ulcer Disease Causes, Symptoms, Diagnosis (40Document5 pagesPeptic Ulcer Disease Causes, Symptoms, Diagnosis (40George Mikhail Labuguen100% (1)
- Hematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewDocument6 pagesHematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewWahyu Agung PribadiNo ratings yet
- Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer DiseaseDocument9 pagesPeptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer Disease Peptic Ulcer DiseaseRhesky Noer FhadillahNo ratings yet
- Nursing Management OF Git Problems Gastric and Duodenal DisordersDocument109 pagesNursing Management OF Git Problems Gastric and Duodenal DisorderstantanbaragoNo ratings yet
- Liver D PDFDocument71 pagesLiver D PDFermichoNo ratings yet
- Cholecystitis FinalDocument57 pagesCholecystitis FinalRajendra DesaiNo ratings yet
- Tropical Infections and InfestationsDocument53 pagesTropical Infections and Infestationssamiksha meshramNo ratings yet
- Perforated Gastric UlcerDocument15 pagesPerforated Gastric UlcerNorshahidah IedaNo ratings yet
- Complications: Pylori Were Updated in 2017. Although Strong Evidence Is LackDocument4 pagesComplications: Pylori Were Updated in 2017. Although Strong Evidence Is LackAinun Jariah FahayNo ratings yet
- Peptic Ulcer Disease - EMEDICINE.2020Document47 pagesPeptic Ulcer Disease - EMEDICINE.2020qayyum consultantfpsc100% (1)
- Lecture 1part 2Document50 pagesLecture 1part 2mashe1No ratings yet
- Pathogens: Hepatic AbscessDocument8 pagesPathogens: Hepatic Abscessalberto cabelloNo ratings yet
- Peptic Ulcer DiseaseDocument36 pagesPeptic Ulcer DiseaseRamanujam SekarNo ratings yet
- Peptic Ulcer DiseaseDocument29 pagesPeptic Ulcer DiseasesoumayacallenderNo ratings yet
- Peptic Ulcer Disease (PUD)Document6 pagesPeptic Ulcer Disease (PUD)Jacqueline TricaricoNo ratings yet
- Lecture 1 & 2 Peptic Ulcer DiseaseDocument26 pagesLecture 1 & 2 Peptic Ulcer DiseaseNovi ArthaNo ratings yet
- 01 Gastritis & PUDxxDocument51 pages01 Gastritis & PUDxxTor Koang ThorNo ratings yet
- Gastric UlcerDocument2 pagesGastric Ulcersaby abbyNo ratings yet
- Gastro-Oesophageal Reflux Disease: EpidemiologyDocument6 pagesGastro-Oesophageal Reflux Disease: EpidemiologyRehan RiyazNo ratings yet
- KGB - Stomach - 02 - DR KishoreDocument29 pagesKGB - Stomach - 02 - DR KishoreMituran IshwarNo ratings yet
- Perforated Peptic Ulcer Dr. Anbiar Manjas, SP.B-KBDDocument68 pagesPerforated Peptic Ulcer Dr. Anbiar Manjas, SP.B-KBDAndy YusufNo ratings yet
- Dyspepsia Management Guidelines: PrefaceDocument9 pagesDyspepsia Management Guidelines: PrefaceRiefka Ananda ZulfaNo ratings yet
- Part 3 PUDDocument227 pagesPart 3 PUDAnonymous MmiBnqnDyNo ratings yet
- Peptic Ulcer Disease: "Something Is Eating at Me"Document37 pagesPeptic Ulcer Disease: "Something Is Eating at Me"bobtaguba100% (1)
- Gastric Ulcer Causes, Symptoms and TreatmentDocument11 pagesGastric Ulcer Causes, Symptoms and TreatmentAsish GeiorgeNo ratings yet
- Chapter 6: Gastroduodenal DiseaseDocument12 pagesChapter 6: Gastroduodenal Diseasevizinho2000No ratings yet
- GI BLEEDING CAUSES AND DIAGNOSISDocument24 pagesGI BLEEDING CAUSES AND DIAGNOSISGunawan Cahyo SNo ratings yet
- Intestinal Obstruction: Methas Arunnart MDDocument42 pagesIntestinal Obstruction: Methas Arunnart MDJhe-sie AngelinaNo ratings yet
- Peptic and Other Benign UlcersDocument31 pagesPeptic and Other Benign Ulcersmomi311No ratings yet
- Clinical Clerk Seminar Series: Approach To Gi BleedsDocument11 pagesClinical Clerk Seminar Series: Approach To Gi BleedsAngel_Liboon_388No ratings yet
- Hematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewDocument6 pagesHematemesis Melena Due To Helicobacter Pylori Infection in Duodenal Ulcer: A Case Report and Literature ReviewodiNo ratings yet
- DBM PDFDocument10 pagesDBM PDFSidNo ratings yet
- Tooth Hypersensitivity GuideDocument11 pagesTooth Hypersensitivity GuideSidNo ratings yet
- Asthma PDFDocument2 pagesAsthma PDFSidNo ratings yet
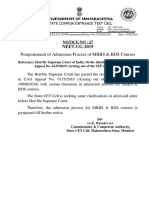
- NEET-UG 2019 Admission Process Postponed for MBBS & BDS CoursesDocument1 pageNEET-UG 2019 Admission Process Postponed for MBBS & BDS CoursesSidNo ratings yet
- Aadhaar Seeding Process PDFDocument3 pagesAadhaar Seeding Process PDFR KumarNo ratings yet
- Leader Test Schedule Neet AiimsDocument1 pageLeader Test Schedule Neet AiimsArpit SinghNo ratings yet
- Surah IkhlasDocument20 pagesSurah IkhlasShazwan FauzeeNo ratings yet
- Sayre Materia Medica-3Document87 pagesSayre Materia Medica-3ven_bams5840No ratings yet
- Nikola Tesla Was Murdered by Otto Skorzeny.Document12 pagesNikola Tesla Was Murdered by Otto Skorzeny.Jason Lamb50% (2)
- Lincoln Pulse On PulseDocument4 pagesLincoln Pulse On PulseEdison MalacaraNo ratings yet
- Monster of The Week Tome of Mysteries PlaybooksDocument10 pagesMonster of The Week Tome of Mysteries PlaybooksHyperLanceite XNo ratings yet
- KINETIC THEORY OF GASES TUTORIALDocument6 pagesKINETIC THEORY OF GASES TUTORIALMat SyafiqNo ratings yet
- BCP-8000 User's ManualDocument36 pagesBCP-8000 User's ManualAsad PatelNo ratings yet
- CANAL (T) Canal Soth FloridaDocument115 pagesCANAL (T) Canal Soth FloridaMIKHA2014No ratings yet
- Rotary Twin Scew Brochure UK HRDocument20 pagesRotary Twin Scew Brochure UK HRNguyễn Hữu DũngNo ratings yet
- Internal Audit ChecklistDocument18 pagesInternal Audit ChecklistAkhilesh Kumar75% (4)
- Plate-Load TestDocument20 pagesPlate-Load TestSalman LakhoNo ratings yet
- Drugs Pharmacy BooksList2011 UBPStDocument10 pagesDrugs Pharmacy BooksList2011 UBPStdepardieu1973No ratings yet
- Proceedings of The 16 TH WLCDocument640 pagesProceedings of The 16 TH WLCSabrinaNo ratings yet
- Design of Fixed Column Base JointsDocument23 pagesDesign of Fixed Column Base JointsLanfranco CorniaNo ratings yet
- Reflection 2: WHAT DOES It Mean To Be A Pacific Islander Today and in The Future To Me?Document5 pagesReflection 2: WHAT DOES It Mean To Be A Pacific Islander Today and in The Future To Me?Trishika NamrataNo ratings yet
- Taking Back SundayDocument9 pagesTaking Back SundayBlack CrowNo ratings yet
- HVCCI UPI Form No. 3 Summary ReportDocument2 pagesHVCCI UPI Form No. 3 Summary ReportAzumi AyuzawaNo ratings yet
- SOIL ASSESSMENT AND PLANT PROPAGATION OF BELL PEPPERS (Capsicum Annuum)Document35 pagesSOIL ASSESSMENT AND PLANT PROPAGATION OF BELL PEPPERS (Capsicum Annuum)Audrey Desiderio100% (1)
- Phenomenological of in Church and TV WorshipDocument18 pagesPhenomenological of in Church and TV WorshipCindy TirtaNo ratings yet
- Fundermax Exterior Technic 2011gb WebDocument88 pagesFundermax Exterior Technic 2011gb WebarchpavlovicNo ratings yet
- Cs8791 Cloud Computing Unit2 NotesDocument37 pagesCs8791 Cloud Computing Unit2 NotesTeju MelapattuNo ratings yet
- Placenta Previa Case Study: Adefuin, Jay Rovillos, Noemie MDocument40 pagesPlacenta Previa Case Study: Adefuin, Jay Rovillos, Noemie MMikes CastroNo ratings yet
- Ricoh 4055 PDFDocument1,280 pagesRicoh 4055 PDFPham Nguyen Hoang Minh100% (1)
- JK Paper Q4FY11 Earnings Call TranscriptDocument10 pagesJK Paper Q4FY11 Earnings Call TranscriptkallllllooooNo ratings yet
- Swatchh Bharat AbhiyanDocument13 pagesSwatchh Bharat AbhiyanHRISHI SHARMANo ratings yet
- A6 2018 D Validation Qualification Appendix6 QAS16 673rev1 22022018Document12 pagesA6 2018 D Validation Qualification Appendix6 QAS16 673rev1 22022018Oula HatahetNo ratings yet
- 2 - Elements of Interior DesignDocument4 pages2 - Elements of Interior DesignYathaarth RastogiNo ratings yet
- Mechanical Specifications For Fiberbond ProductDocument8 pagesMechanical Specifications For Fiberbond ProducthasnizaNo ratings yet
- ProtectionDocument160 pagesProtectionSuthep NgamlertleeNo ratings yet
- Liquid Out, Temperature 25.5 °C Tube: M/gs P / WDocument7 pagesLiquid Out, Temperature 25.5 °C Tube: M/gs P / WGianra RadityaNo ratings yet
- Private Schools Provide Better EducationDocument2 pagesPrivate Schools Provide Better EducationcitraNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Recovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyFrom EverandRecovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyRating: 4.5 out of 5 stars4.5/5 (201)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)