Professional Documents
Culture Documents
Gastric Ulcers: Presented By: Dr. Jawaria Memon & Dr. Deep Kumar
Uploaded by
Deep Khemani0 ratings0% found this document useful (0 votes)
41 views31 pagesGastric ulcers are lesions in the stomach lining caused by stomach acid and impaired defenses. Risk factors include H. pylori infection, NSAID use, and smoking. Clinical features include epigastric pain relieved by eating. Diagnosis is via endoscopy and biopsy. Complications include bleeding and perforation. Treatment involves eradication of H. pylori, PPIs, and surgery if complications occur. Surgical options aim to divert acid from the ulcer or reduce secretion. Post-op complications can include recurrent ulcers, dumping syndrome, and increased cancer risk.
Original Description:
Original Title
Gastric Ulcers
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGastric ulcers are lesions in the stomach lining caused by stomach acid and impaired defenses. Risk factors include H. pylori infection, NSAID use, and smoking. Clinical features include epigastric pain relieved by eating. Diagnosis is via endoscopy and biopsy. Complications include bleeding and perforation. Treatment involves eradication of H. pylori, PPIs, and surgery if complications occur. Surgical options aim to divert acid from the ulcer or reduce secretion. Post-op complications can include recurrent ulcers, dumping syndrome, and increased cancer risk.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
41 views31 pagesGastric Ulcers: Presented By: Dr. Jawaria Memon & Dr. Deep Kumar
Uploaded by
Deep KhemaniGastric ulcers are lesions in the stomach lining caused by stomach acid and impaired defenses. Risk factors include H. pylori infection, NSAID use, and smoking. Clinical features include epigastric pain relieved by eating. Diagnosis is via endoscopy and biopsy. Complications include bleeding and perforation. Treatment involves eradication of H. pylori, PPIs, and surgery if complications occur. Surgical options aim to divert acid from the ulcer or reduce secretion. Post-op complications can include recurrent ulcers, dumping syndrome, and increased cancer risk.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 31
GASTRIC ULCERS
PRESENTED BY: DR. JAWARIA
MEMON & DR. DEEP KUMAR
OUTLINE
• Introduction
• Pathophysiology
• Etiology/ Risk factors
• Types of PUD
• Clinical Presentation
• Investigation/ Diagnostic test
• Complications of PUD
• Management
• Post-operative complications
INTRODUCTION
• Peptic Ulcer is a lesion in the lining (mucosa) of the
digestive tract, typically in the stomach or duodenum,
caused by the digestive action of pepsin and stomach acid
and impaired mucosal defenses.
• Common sites are first part of duodenum, lesser curvature
of stomach, gastro-esophageal junction, Meckel's
diverticulum, stoma after gastric surgery, and less
commonly esophagus.
• Gastric ulcers have relatively normal levels of gastric acid
secretion as compared to duodenal ulcers.
PATHOPHYSIOLOGY
ETIOLOGY/ RISK FACTORS
• H.pylori infection – most important
• Chronic use of NSAIDS and aspirin
• Steriods
• Smoking
DUODENAL ULCERS GASTRIC ULCERS
1. Duodenal ulcers are more 1. Gastric ulcers occurs in low
common in older men. socioeconomic groups and are less
2. They're rarely malignant. common than duodenal ulcers.
2. Can be malignant
3. Most common complication is
3. Fibrosis cause hourglass contraction of
stenosis, perforation and bleeding. stomach
4. Both anterior and posterior 4. More common on lesser curvature at
ulcers together called kissing ulcers. the boundary between acid secreting
5. Anteriorly placed ulcers tend to and non acid secreting part.
perforate and posteriorly placed 5. Very difficult to distinguish benign
ulcers tend to bleed. ulcer and gastric cancer without biopsy.
Hence, every ulcer should be considered
malignant and biopsy should be sent.
CLINICAL FEATURES
1. Pain is epigastric, gnawing and radiates to back. Eating
may relieve discomfort. The pain is intermittent.
2. Periodicity is a classical feature. The symptoms may
disappear for months or weeks and then may reappear.
3. Vomiting not noticeable unless stenosis
4. Weight loss (gastric ulcer) or weight gain may occur
5. Bleeding may be chronic and endoscopy must be done.
6. Examination reveals epigastric tenderness.
DIAGNOSTIC TESTS
• Gastrodeuodenoscopy (GD) – Investigation of choice
– Endoscopic procedure
• Visualizes ulcer crater
• Ability to take tissue biopsy to R/O cancer and diagnose H. pylori
– Upper gastrointestinal series (UGI)
• Barium swallow
• X-ray that visualizes structures of the upper GI tract
– Urea Breath Testing
• Used to detect H.pylori
• Patient drinks a carbon-enriched urea solution
• Exhaled carbon dioxide is then measured
• All mucosal abnormalities at gastroesophageal junction must undergo multiple biopsies
because of increased incidence of cancer.
• In all patients with “Alarming symptoms”
endoscopy is required.
• Dysphagia.
• Weight loss.
• Vomiting.
• Anorexia.
• Hematemesis or Melena
Complications
• Bleeding (left gastric entry) – gastric ulcers
• Bleeding (gastroduodenal artery) – duodenal
ulcers
• Iron deficiency anemia
• Perforation
• Gastric outlet obstruction
Medical Treatment
1. Two week treatment with H2 antagonist or proton pump inhibitors causes
healing. Symptoms are relieved within few days. Relapse is almost
universal.
2. Eradication therapy is effective when H.pylori is the cause. OR when
patient doesn't take NSAIDS.
3. Patient taking NSAIDS or having Stomal ulcers or Zollinger Ellison
syndrome should have prolonged treatment with potent antisecretory
agents specially proton pump inhibitor (for ZES).
4. Antacids, Prostaglandin analogues and Mucosal barrier fortifiers also help.
5. Eradication therapy consists of a triple therapy: a proton pump inhibitor +
two antibiotics: Metronidazole + Clarithromycin fpr 14 days OR quadruple
therapy: triple therapy + Bismuth.
In case of failure
1. Endoscopic re-evaluation should be done if ulcers fail to heal
(differentiates between a refractory ulcer and persistent symptoms
despite ulcer healing)
2. Most common cause is persistent H.pylori infection
3. Biopsies should be done along with endoscopy as false negative
results with breath test are common and serum antibody levels take 6
months or more to fall.
4. Failure of eradication is because of poor compliance or bacterial
resistance so bacterial culture would help.
5.NSAID ingestion needs to be addressed
6. ZES must be suspected in H.pylori negative, non NSAID related
peptic ulcer and serum gastrin should be measured.
SURGICAL MANAGEMENT
• There is varying degree of morbidity, mortality
and post op side effects so it is important for
clinician to employ surgery if it's absolute
necessity.
DUODENAL ULCERS
• The aim is to the divert the
acid away from duodenum or
reducing the secretory portion
of stomach or both.
• Billroth 2 Gastrectomy: The
lower portion of the stomach
is removed and the remainder
is anastomosed to the
jejunum.
• Common cause of morbidity is
leakage from duodenal stump.
GASTROENTEROSTOMY:
• Creates a passage between
the body of stomach to small
intestines that allows
regurgitation of alkaline
duodenal contents into the
stomach and keeps acid away
from ulcerated area.
• Alkali reflux is protective
against duodenal ulcer but
stomal ulceration is common.
• PYLOROPLASTY:
Widens the
pylorus to
guarantee
stomach emptying
even without
vagus nerve
stimulation.
Truncal vagotomy and drainage:
Truncal vagotomy involves
denervation of the section of vagus
nerve that is involved in acid
production but this procedure alone
causes gastric stasis hence a
drainage procedure like heineke-
mikulicz pyloroplasty (most popular
drainage procedure) or
gastrojejunostomy (alternative)
should be employed along with it.
This combination is safer than
gastrectomy.
• Highly selective vagotomy: Involves
denervation of only parietal cell mass of the
stomach. This is most satisfactory operation for
duodenal ulcers and is gold standard. Lowest
mortality and morbidity as gastrointestinal
tract isn't opened during procedure. However,
it leads to Epigastric fullness and mild
dumping. Recurrence is common.
Truncal vagotomy and antrectomy: Has
exceedingly low recurrence rate but operative
morality is high.
GASTRIC ULCERS
Billroth I Gastrectomy:
Distal portion of the
stomach is removed and
the remainder is
anastomosed to the
duodenum.
Same recurrence,
morbidity and mortality
as with any gastric
resection.
Post-Operative Complications
1. Recurrent ulceration: treated the same as ulcers before
surgery.
• In case of gastrojejunal colic fistula, the anastomotic ulcer
penetrates into transverse colon.
• Patient has severe diarrhea following every meal. They have
foul breath and may vomit formed feaces. Severe weight loss
and vomiting occurs and condition mimics malignancy.
• Best imaging study is CT with IV contrast or barium enema.
• Treatment is to correct dehydration then perform revisional
surgery.
2. Small stomach syndrome: is characterized by early satiety due to
loss of receptive relaxation. This gets better with time on its own.
3. Bile vomiting: Charactetized by vomiting a mixture of food or
sometimes bile after a meal. Abdominal pain and reflux symptoms
are common after eating. Bile chelating agents are ineffective.
Revision surgery depending upon the original operation should be
done.
4. Dumping
Early dumping: the small bowel has food stuff that has high osmotic load
this leads to sequestration of fluid from circulation into GIT.
Treatment is Dietary manipulation. Small regular meals with protein and fat
and avoid fluids with high carbohydrate content. If itdoesn't improve,
somatostatin analogue octreotide before meals helps. This treatment can
lead to gallstones and also doesn't help with diarrhoea. Revisional surgery
can be performed if everything fails.
Late dumping: reactive hypoglycemia. The carbohydrate in small bowel
causes rise in plasma glucose which increases insulin levels causing
secondary hypoglycemia. The treatment is same as early dumping.
5. Post vagotomy diarrhoea: Is most devastating complication. Looseness
of bowel action is suffered by all patients after surgery but it's rarely
intractable. Precise Aetiology of problem is uncertain. It is related to rapid
gastric emptying. Diarrhea may take several forms from minor episodes
to severe and explosive. The condition is difficult to treat. Antidiarrheal
preparations may help. Octreotide and revisional surgery has no role.
6. Malignant transformation: Risk is increased to approximately 4 times
following gastric surgery. The lag phase between operation and
development of malignancy is at least 10 years.
7. Nutritional consequences: are common like weight loss,
iron deficiency anemia, vitaminb12 deficiency anemia and
bone disease in women.
8. Gallstones: Are strongly associated with truncal
vagotomy. Biliary tree along with stomach is denervated
leading to stasis and hence stone formation. Treatment is
cholecystectomy which may induce or worsen other post-
peptic surgery syndromes.
Perforated Peptic Ulcer
1. Patient presents with sudden onset severe generalised pain followed by bacterial peritonitis in
few hours accompanied by deterioration in patient's condition. Initially patient is in shock and
tachycardia, pyrexia occurs few hours after the event. Abdomen has board like rigidity and
doesn't move with respiration. Patient needs an operation without which the patient will
detoriate with septic peritonitis. This classic presentation is observed less commonly.
2. Most common site of perforation is anterior aspect of duodenum.
3. Investigation: Erect plain chest radiograph will show gas under diaphragm.
Ct scan is more accurate.
4. Serum amylase to differentiate between peptic ulcer, perforation and pancreatitis. Serum
amylase may be elevated following perforated peptic ulcer but the levels are not as high as in
acute pancreatitis.
5. Treatment involves resuscitation and analgesia.
Analgesia makes clinical signs more obvious.
Laparotomy is treatment of choice. Laparoscopy is alternative treatment.
6. All patients should be given eradication therapy along with anti-secretory agents and stomach
should be kept empty via nasogastric tube.
THANK YOU
You might also like
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Pathophysiology of DiarrheaDocument3 pagesPathophysiology of DiarrheaFathur RahmatNo ratings yet
- Peptic Ulcer DiseaseDocument12 pagesPeptic Ulcer Diseasehya2284No ratings yet
- Perforated Gastric UlcerDocument15 pagesPerforated Gastric UlcerNorshahidah IedaNo ratings yet
- Pepti C Ul Cer Dis Ea SeDocument36 pagesPepti C Ul Cer Dis Ea Segerald_ichigoNo ratings yet
- Cholelithiasis Treatment & ManagementDocument8 pagesCholelithiasis Treatment & ManagementRayhanun MardhatillahNo ratings yet
- Cholecystitis IntroductionDocument4 pagesCholecystitis IntroductionJechelle Ann Pabustan Martin-BoniquitNo ratings yet
- Addison's Disease: Adrenal Insufficiency and Adrenal CrisisDocument15 pagesAddison's Disease: Adrenal Insufficiency and Adrenal CrisisMaryONo ratings yet
- Liver AbscessDocument6 pagesLiver AbscessKenneth SunicoNo ratings yet
- Ascitic Fluid AnalysisDocument3 pagesAscitic Fluid AnalysisLohJNo ratings yet
- Complete Intestinal ObstructionDocument8 pagesComplete Intestinal ObstructionThuganamix100% (2)
- Gastritis Englis 2018Document115 pagesGastritis Englis 2018irinaNo ratings yet
- Mixed HemorrhoidsDocument4 pagesMixed HemorrhoidsHerne BalberdeNo ratings yet
- Case 2 and 3 Q1Document3 pagesCase 2 and 3 Q1Jeffrey Ramos0% (1)
- Schematic Diagram of Alcoholic Cirrhosis: Liver Steatosis/ Fatty LiverDocument2 pagesSchematic Diagram of Alcoholic Cirrhosis: Liver Steatosis/ Fatty LiverCarmelli Mariae CalugayNo ratings yet
- Colon Cancer: Risk FactorsDocument3 pagesColon Cancer: Risk FactorsAshley VillanuevaNo ratings yet
- Dave Jay S. Manriquez RN. Acute CholecystitisDocument11 pagesDave Jay S. Manriquez RN. Acute CholecystitisChilleMaeNo ratings yet
- Malnutrition in Older AdultsDocument44 pagesMalnutrition in Older Adultsjohnjoe subaynoNo ratings yet
- Gastritis: Medical AffairDocument11 pagesGastritis: Medical AffairKomal KhanNo ratings yet
- Intestinal Obstruction: EpidemiologyDocument11 pagesIntestinal Obstruction: EpidemiologyBereket temesgenNo ratings yet
- Edema: Dr. Bernardo Dámaso MataDocument55 pagesEdema: Dr. Bernardo Dámaso MataDeivis Dan ErickNo ratings yet
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- Pyloric StenosisDocument5 pagesPyloric StenosisMichael AlexanderNo ratings yet
- Pa Tho Physiology of PneumoniaDocument6 pagesPa Tho Physiology of PneumoniaPaula YoungNo ratings yet
- CYSTITIS!Document12 pagesCYSTITIS!crave24No ratings yet
- Cholecystitis (Surgery)Document100 pagesCholecystitis (Surgery)Hazel Aspera100% (1)
- Bowel ObstructionDocument6 pagesBowel ObstructionKryza Dale Bunado BaticanNo ratings yet
- Intestinal Obstruction: Methas Arunnart MDDocument42 pagesIntestinal Obstruction: Methas Arunnart MDJhe-sie AngelinaNo ratings yet
- Ulcerative ColitisDocument18 pagesUlcerative ColitisHoussein EL HajjNo ratings yet
- The Pathophysiology of Peptic UlcerDocument15 pagesThe Pathophysiology of Peptic UlcerKike Meneses100% (1)
- How Low Can You Endure The Pain, Mr. Bond?Document70 pagesHow Low Can You Endure The Pain, Mr. Bond?Venny VeronicaNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- PancreatitisDocument12 pagesPancreatitismardsz100% (5)
- Diagnosis of Gastrointestinal Bleeding in AdultsDocument8 pagesDiagnosis of Gastrointestinal Bleeding in AdultsSaeed Al-YafeiNo ratings yet
- Gastric Outlet Obstruction: Its Surgical ManagementDocument40 pagesGastric Outlet Obstruction: Its Surgical ManagementGudeta shegerNo ratings yet
- Pathophysiology of MalariaDocument20 pagesPathophysiology of Malariamelia100% (1)
- Ulcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryDocument71 pagesUlcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryFachry Al RafiqiNo ratings yet
- Summary Case Peptic Ulcer and PeritonitisDocument8 pagesSummary Case Peptic Ulcer and PeritonitissyududNo ratings yet
- Perforated Peptic UlcerDocument68 pagesPerforated Peptic UlcerSaibo BoldsaikhanNo ratings yet
- Bowel Obstruction SurgeryDocument12 pagesBowel Obstruction SurgeryDivya JoyNo ratings yet
- Intestinal ObstructionDocument58 pagesIntestinal ObstructionTUSHAR PARMARNo ratings yet
- Inflammatory Bowel Disease: DefinitionDocument4 pagesInflammatory Bowel Disease: Definitionkarl abiaadNo ratings yet
- Pneumonperitoneum A Review of Nonsurgical Causes PDFDocument7 pagesPneumonperitoneum A Review of Nonsurgical Causes PDFDellysa Eka Nugraha TNo ratings yet
- 7.peptic Ulcer DiseaseDocument20 pages7.peptic Ulcer DiseaseHayat AL AKOUMNo ratings yet
- Surgical Treatment of Hemorrhoidal Disease - UpToDateDocument27 pagesSurgical Treatment of Hemorrhoidal Disease - UpToDateJune DoNo ratings yet
- Buerger's DiseaseDocument4 pagesBuerger's DiseaseArchana ChaudharyNo ratings yet
- Intestinal ObstructionDocument12 pagesIntestinal ObstructionNurul Nurnita100% (1)
- Abdominal TraumaDocument24 pagesAbdominal TraumaSurgeryClassesNo ratings yet
- Hyperosmolar HyperglycemicDocument8 pagesHyperosmolar HyperglycemicCésar Augusto Sánchez SolisNo ratings yet
- Acute and Chronic Pancreatitis ShirleyDocument6 pagesAcute and Chronic Pancreatitis ShirleyVictor AladejanaNo ratings yet
- PericarditisDocument11 pagesPericarditisrbarcellonaNo ratings yet
- Crohn's DiseaseDocument38 pagesCrohn's Diseasetintukmathew100% (1)
- A Case Presentation On AppendecitisDocument30 pagesA Case Presentation On AppendecitisrodericpalanasNo ratings yet
- NephrolithiasisDocument2 pagesNephrolithiasisDeepthiNo ratings yet
- Adrenal InsufficiencyDocument10 pagesAdrenal InsufficiencyKhalil DiabNo ratings yet
- Peptic Ulcer Dse PathophysiologyDocument19 pagesPeptic Ulcer Dse PathophysiologySymone Jay Lapiz100% (1)
- Acute Cholecystitis - PCP CPG 2003Document37 pagesAcute Cholecystitis - PCP CPG 2003Teng IbanezNo ratings yet
- Anaphylactic ReactionDocument9 pagesAnaphylactic ReactionZahir Jayvee Gayak IINo ratings yet
- HemorrhoidectomyDocument5 pagesHemorrhoidectomydrnareshkumar3281100% (1)
- PA SystemDocument1 pagePA SystemSherif SalamaNo ratings yet
- FC52Document5 pagesFC52Bassel AlmouieNo ratings yet
- PTE Academic - Strategies For Summarize The Written TextDocument9 pagesPTE Academic - Strategies For Summarize The Written TextPradeep PaudelNo ratings yet
- Edna-Mode ScriptDocument2 pagesEdna-Mode ScriptNikkay Gepanaga CejarNo ratings yet
- ADL 12 Business Laws V4Document26 pagesADL 12 Business Laws V4Aditya BhatNo ratings yet
- Bài Kt 2 Biên Dịch 1-LiêmDocument10 pagesBài Kt 2 Biên Dịch 1-LiêmNguyen Loan100% (1)
- Theoretical Foundation For Large-Scale Computations For Nonlinear Material BehaviorDocument411 pagesTheoretical Foundation For Large-Scale Computations For Nonlinear Material BehaviorDalelAzaiezNo ratings yet
- 731 Mitendra Pratap SinghDocument2 pages731 Mitendra Pratap Singhmitendra pratap singhNo ratings yet
- Efficacy of DUMBCANE (Dieffenbachia Picta Schott.) Stem Extracts AGAINST GOLDEN APPLE SNAIL (Pomacea Canaliculata L.)Document3 pagesEfficacy of DUMBCANE (Dieffenbachia Picta Schott.) Stem Extracts AGAINST GOLDEN APPLE SNAIL (Pomacea Canaliculata L.)Mary rose YenyenNo ratings yet
- Catalogo Lowara DomoDocument6 pagesCatalogo Lowara DomoSergio ZegarraNo ratings yet
- Abs TechnologyDocument14 pagesAbs Technologyanime landNo ratings yet
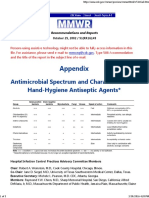
- Antimicrobial Spectrum and Characteristics of Hand-Hygiene Antiseptic AgentsDocument3 pagesAntimicrobial Spectrum and Characteristics of Hand-Hygiene Antiseptic AgentsdonsterthemonsterNo ratings yet
- Anushree - VivaDocument76 pagesAnushree - VivaCarolin R 16No ratings yet
- Wound Repair and RegenerationDocument8 pagesWound Repair and RegenerationdrsamnNo ratings yet
- Mathematical LanguageDocument9 pagesMathematical Languagejrqagua00332No ratings yet
- Anh 7 Cum 1 (2017-2018)Document6 pagesAnh 7 Cum 1 (2017-2018)anhthunoban2011No ratings yet
- DLL - Science 4 - Q4 - W1Document4 pagesDLL - Science 4 - Q4 - W1Jefferson BeraldeNo ratings yet
- List of Dealers Selected From Cuttack I Range For Tax Audit During 2011-12Document24 pagesList of Dealers Selected From Cuttack I Range For Tax Audit During 2011-12rchowdhury_10No ratings yet
- USB-Link™ 2 Bluetooth Edition Installation and Setup ManualDocument54 pagesUSB-Link™ 2 Bluetooth Edition Installation and Setup ManualMichael Bennett100% (2)
- Vamp 221 V221 en M C021 PDFDocument164 pagesVamp 221 V221 en M C021 PDFPaulo BraggioNo ratings yet
- Prestensioning & Post-TensioningDocument40 pagesPrestensioning & Post-TensioningKURUBA SARAN RAJ SamNo ratings yet
- A Level NdebeleDocument5 pagesA Level Ndebelenokwandadlamini2010No ratings yet
- Food Stuff From List CompaniesDocument3 pagesFood Stuff From List CompaniesListonNo ratings yet
- Union Feb. 10, 2016Document16 pagesUnion Feb. 10, 2016Your News. When You Want It.No ratings yet
- AGILE MCQsDocument51 pagesAGILE MCQsAmaan RazaNo ratings yet
- IV Fluid ChartDocument1 pageIV Fluid ChartQuality CapitalNo ratings yet
- Chapter 1 and Chapter 2 PowerpointDocument14 pagesChapter 1 and Chapter 2 Powerpointapi-252892423No ratings yet
- NewJaisa Corporate ProfileDocument14 pagesNewJaisa Corporate ProfileCRAZY ಕನ್ನಡಿಗNo ratings yet
- Delta Background-Group AssignmentDocument2 pagesDelta Background-Group AssignmentTinashe100% (2)
- Personal Information WorksheetDocument1 pagePersonal Information Worksheetdaniela cardonaNo ratings yet