Professional Documents
Culture Documents
Antibody Mediated Rejection PDF
Uploaded by
علي حسين عودة العلياويOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibody Mediated Rejection PDF
Uploaded by
علي حسين عودة العلياويCopyright:
Available Formats
neinJdebJfnaanbJnaIirn JsbivanUilacJda naaJaHJnaIiribaJ
eainnleablJaHJrnl a aaaJnbIJtanabUirJnaIiriba
Jenea : ali hussein auda d nUU : 3 pnari: D Date:2020/03/25
Report title : Antibody‐mediated rejection
Antibody‐mediated rejection (AMR) is a significant complication following organ transplantation that
contributes toward both short‐ and long‐term injury. three types of AMR exists based on the timing and course
of the rejection event :
Hyperacute rejection : occurs within minutes to a few hours after transplantation in a presensitized host
and typically is recognized by the surgeon just after the vascular anastomosis is completed. In contrast with
a nonrejecting kidney graft, which regains a normal pink color and tissue turgor and promptly excretes
urine, a hyperacutely rejecting kidney rapidly becomes cyanotic, mottled, and flaccid and may excrete only
a few drops of bloody fluid. The histologic picture is characterized by widespread acute arteritis and
arteriolitis, vessel thrombosis, and ischemic necrosis, all resulting from the binding of preformed antibodies
to graft endothelium.
J Acute rejection : may occur within days to weeks of transplantation in a nonimmunosuppressed host or
may appear months or even years later, even in the presence of adequate immunosuppression. Acute
rejection is caused by both cellular and humoral immune mechanisms, and in any one patient, one or the
other may predominate, or both may be present. On histologic examination, cellular rejection is marked by
an interstitial mononuclear cell infiltrate with associated edema and parenchymal injury, whereas humoral
rejection is associated with vasculitis.
1. Acute cellular rejection most commonly is seen within the first months after transplantation and typically
is accompanied by clinical signs of renal failure.
2. Acute humoral rejection (rejection vasculitis) caused by antidonor antibodies also may participate in
acute graft rejection.
Chronic Rejection : Patients present with chronic rejection late after transplantation (months to years) with
a progressive rise in serum creatinine levels over a period of 4 to 6 months. Chronic rejection is dominated
by vascular changes, interstitial fibrosis, and loss of renal parenchyma; there are typically only mild or no
ongoing cellular parenchymal infiltrates.
Treatment:
The current strategy for treating AMR is use of a combination of modalities to address multiple
pathophysiologic pathways.regimens of plasmapheresis or immunoadsorption followed by low‐dose
intravenous immunoglobulin or high‐dose IVIg with or without steroids.
You might also like
- Paracetamol Overdose and Management IIIDocument10 pagesParacetamol Overdose and Management IIIعلي حسين عودة العلياويNo ratings yet
- Practical Histology:) Motor Neurone Disease (MNDDocument5 pagesPractical Histology:) Motor Neurone Disease (MNDعلي حسين عودة العلياويNo ratings yet
- Parasitology: Entamoeba HistolyticaDocument9 pagesParasitology: Entamoeba Histolyticaعلي حسين عودة العلياويNo ratings yet
- Colorectal Cancer IIDocument6 pagesColorectal Cancer IIعلي حسين عودة العلياويNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Controlled DemolitionDocument3 pagesControlled DemolitionJim FrancoNo ratings yet
- Bustax Midtem Quiz 1 Answer Key Problem SolvingDocument2 pagesBustax Midtem Quiz 1 Answer Key Problem Solvingralph anthony macahiligNo ratings yet
- Smart Plug Installation GuideDocument9 pagesSmart Plug Installation GuideFrancisco GuerreroNo ratings yet
- CH 15Document58 pagesCH 15Chala1989No ratings yet
- SAP HR - Legacy System Migration Workbench (LSMW)Document5 pagesSAP HR - Legacy System Migration Workbench (LSMW)Bharathk KldNo ratings yet
- Ransomware: Prevention and Response ChecklistDocument5 pagesRansomware: Prevention and Response Checklistcapodelcapo100% (1)
- Dance Terms Common To Philippine Folk DancesDocument7 pagesDance Terms Common To Philippine Folk DancesSaeym SegoviaNo ratings yet
- Introduction To FluidizationDocument9 pagesIntroduction To FluidizationEriCisacNo ratings yet
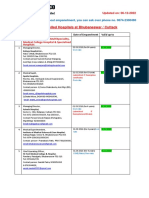
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Document19 pagesEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uNo ratings yet
- ATS2017 ProspectusDocument13 pagesATS2017 ProspectusGiri WakshanNo ratings yet
- Chestionar 2Document5 pagesChestionar 2Alex AndruNo ratings yet
- Yarn HairinessDocument9 pagesYarn HairinessGhandi AhmadNo ratings yet
- Pontevedra 1 Ok Action PlanDocument5 pagesPontevedra 1 Ok Action PlanGemma Carnecer Mongcal50% (2)
- Assembly InstructionsDocument4 pagesAssembly InstructionsAghzuiNo ratings yet
- A Process Reference Model For Claims Management in Construction Supply Chains The Contractors PerspectiveDocument20 pagesA Process Reference Model For Claims Management in Construction Supply Chains The Contractors Perspectivejadal khanNo ratings yet
- ProbDocument10 pagesProbKashif JawaidNo ratings yet
- Compact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightDocument2 pagesCompact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightStanley Ochieng' OumaNo ratings yet
- Paper II - Guidelines On The Use of DuctlessDocument51 pagesPaper II - Guidelines On The Use of DuctlessMohd Khairul Md DinNo ratings yet
- Sample Interview Questions For Planning EngineersDocument16 pagesSample Interview Questions For Planning EngineersPooja PawarNo ratings yet
- Auto Turn-Off For Water Pump With Four Different Time SlotsDocument3 pagesAuto Turn-Off For Water Pump With Four Different Time SlotsKethavath Sakrunaik K100% (1)
- SAED90DR Rev1 2 21.01.2011Document24 pagesSAED90DR Rev1 2 21.01.2011Cherry AbhiNo ratings yet
- IPS PressVest Premium PDFDocument62 pagesIPS PressVest Premium PDFLucian Catalin CalinNo ratings yet
- Individual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsDocument3 pagesIndividual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsMarian SalazarNo ratings yet
- SahanaDocument1 pageSahanamurthyarun1993No ratings yet
- Case Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Document15 pagesCase Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Jafer SayedNo ratings yet
- VLT 6000 HVAC Introduction To HVAC: MG.60.C7.02 - VLT Is A Registered Danfoss TrademarkDocument27 pagesVLT 6000 HVAC Introduction To HVAC: MG.60.C7.02 - VLT Is A Registered Danfoss TrademarkSamir SabicNo ratings yet
- Reference by John BatchelorDocument1 pageReference by John Batchelorapi-276994844No ratings yet
- What Is Product Management?Document37 pagesWhat Is Product Management?Jeffrey De VeraNo ratings yet
- MiddleWare Technology - Lab Manual JWFILESDocument171 pagesMiddleWare Technology - Lab Manual JWFILESSangeetha BajanthriNo ratings yet
- R15 Understanding Business CyclesDocument33 pagesR15 Understanding Business CyclesUmar FarooqNo ratings yet