Professional Documents
Culture Documents
Thoracentesis PDF
Uploaded by
gireeshsachinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thoracentesis PDF
Uploaded by
gireeshsachinCopyright:
Available Formats
CHAPTER 36 / Nursing Care of Clients with Lower Respiratory Disorders 1145
A large pleural effusion compresses adjacent lung tissue.
This causes the characteristic manifestation of dyspnea. Pain
may develop, although with inflammatory processes pleuritic
pain often is relieved by formation of an effusion. Breath
sounds are diminished or absent, and a dull percussion tone is
Pleural
heard over the affected area. Chest wall movement may be effusion
limited.
COLLABORATIVE CARE
Chest X-ray often provides the first evidence of a pleural effu-
sion. Because fluid typically collects in dependent regions, it is
seen at the base of the affected lung on an upright chest X-ray,
and along the lateral wall when the client is positioned on the
affected side. CT scans and ultrasonography also are used to
localize and differentiate pleural effusions.
If the cause of pleural effusion is not apparent, a thoracen-
tesis is done. Thoracentesis is an invasive procedure in which
Figure 36–15 ■ Thoracentesis.With the client seated, a needle
fluid (or occasionally air) is removed from the pleural space is inserted between the ribs into the pleural space to withdraw
with a needle. Aspirated fluid is analyzed for appearance, cell accumulated fluid.
counts, protein and glucose content, the presence of enzymes
such as LDH and amylase, abnormal cells, and culture.
When pleural effusion is significant and interferes with res- sertion site. The amount of fluid removed is limited to 1200 to
pirations, thoracentesis is the treatment of choice to remove the 1500 mL at one time to reduce the risk of cardiovascular col-
fluid (Figure 36–15 ■). Thoracentesis may be performed at the lapse from rapid removal of too much fluid. Pneumothorax is
bedside, in a procedure room, or in an outpatient setting. Lo- a possible complication of thoracentesis if the visceral pleura
cal anesthesia is used, and the procedure requires less than 30 is punctured or a closed drainage system not maintained dur-
minutes to complete. Percussion, auscultation, radiography, or ing the procedure. Nursing care for the client undergoing a tho-
ultrasonography are used to locate the effusion and needle in- racentesis is outlined in the box below.
NURSING CARE OF THE CLIENT HAVING A THORACENTESIS
PREPROCEDURE CARE POSTPROCEDURE CARE
• Verify a signed informed consent for the procedure. This inva- • Monitor pulse, color, oxygen saturation, and other signs during
sive procedure requires informed consent. thoracentesis. These are indicators of physiologic tolerance of
• Assess knowledge and understanding of the procedure and its the procedure.
purpose; provide additional information as needed. An in- • Apply a dressing over the puncture site, and position on the
formed client will be less apprehensive and more able to cooper- unaffected side for 1 hour. This allows the pleural puncture to
ate during the thoracentesis. heal.
• Preprocedure fasting or sedation is not required. Only local • Label obtained specimen with name, date, source, and diag-
anesthesia is used in this procedure, and the gag and cough re- nosis; send specimen to the laboratory for analysis. Fluid ob-
flexes remain intact. tained during thoracentesis may be examined for abnormal cells,
• Administer a cough suppressant if indicated. Movement and bacteria, and other substances to determine the cause of the
coughing during the procedure may cause inadvertent damage to pleural effusion.
the lung or pleura. • During the first several hours after thoracentesis, frequently
• Obtain a thoracentesis tray, sterile gloves, injectable lidocaine, assess and document vital signs; oxygen saturation; respira-
povidone-iodine, dressing supplies, and an extra overbed table tory status, including, respiratory excursion, lung sounds,
or mayo stand. These supplies are used by the physician perform- cough, or hemoptysis; and puncture site for bleeding or crepi-
ing the procedure. tus. Frequent assessment is important to detect possible compli-
• Position the client upright,leaning forward with arms and head cations of thoracentesis, such as pneumothorax.
supported on an anchored overbed table. This position spreads • Obtain a chest X-ray. Chest X-ray is ordered to detect possible
the ribs, enlarging the intercostal space for needle insertion. pneumothorax.
• Inform the client that although local anesthesia prevents pain • Normal activities generally can be resumed after 1 hour if no
as the needle is inserted, a sensation of pressure may be felt. A evidence of pneumothorax or other complication is present.
pressure sensation occurs as the needle punctures the parietal The puncture wound of thoracentesis heals rapidly.
pleura to enter the pleural space.
You might also like
- THORACENTESISDocument14 pagesTHORACENTESISKatherine Jeanne RosalNo ratings yet
- Procedure of General AnaesthesiaDocument4 pagesProcedure of General AnaesthesiaNuridayu Sedek100% (1)
- The Romantic Connection FullDocument145 pagesThe Romantic Connection FullPhilipNo ratings yet
- Discharge Plan Patient Teaching Pleural Effusion CastleDocument6 pagesDischarge Plan Patient Teaching Pleural Effusion Castleapi-341263362100% (2)
- Respi DX Procedures Handouts For Asynch ActivityDocument8 pagesRespi DX Procedures Handouts For Asynch ActivityBamba FloresNo ratings yet
- Fragerstorm Test, Bronchoscopy, Abg, Thoracentesis, Pulmonary AngiographyDocument16 pagesFragerstorm Test, Bronchoscopy, Abg, Thoracentesis, Pulmonary AngiographyGrace AdornaNo ratings yet
- Tracheostomy B.MDocument25 pagesTracheostomy B.MEvancemwenya123No ratings yet
- ThoracentesisDocument25 pagesThoracentesisroger67% (3)
- Checklist Thoracentesis (Charisse) ADocument6 pagesChecklist Thoracentesis (Charisse) ARonel UsitaNo ratings yet
- Therapeutic and Diagnostic ProceduresDocument27 pagesTherapeutic and Diagnostic Proceduresamare mitkuNo ratings yet
- Surgical Management: Epidural AnesthesiaDocument4 pagesSurgical Management: Epidural AnesthesiabobtagubaNo ratings yet
- AsDocument48 pagesAsCyndi CastañerosNo ratings yet
- Concept On Surgery: Postoperative CareDocument44 pagesConcept On Surgery: Postoperative CareMelisa ClaireNo ratings yet
- Preoperative TeachingDocument11 pagesPreoperative TeachingDani ThomasNo ratings yet
- Diagnostic Tests: 1-Pulmonary Function Tests (PFTS)Document13 pagesDiagnostic Tests: 1-Pulmonary Function Tests (PFTS)yuddNo ratings yet
- Nursing Care of ThoracentesisDocument15 pagesNursing Care of ThoracentesisNora AlnaimNo ratings yet
- Assisting in Patients Undergoing A ThoracentesisDocument7 pagesAssisting in Patients Undergoing A Thoracentesiscoosa liquors0% (1)
- GI Diagnostic TestsDocument7 pagesGI Diagnostic TestspatzieNo ratings yet
- Thoracentesis ProDocument6 pagesThoracentesis ProRaidis PangilinanNo ratings yet
- Pre OpppDocument87 pagesPre Opppahmadardah416No ratings yet
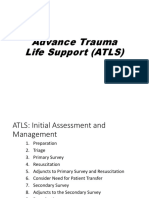
- Advance Trauma Life Support (ATLS)Document47 pagesAdvance Trauma Life Support (ATLS)Ben Man Jun100% (2)
- Perioperative ManagementDocument8 pagesPerioperative ManagementJaezee RamosNo ratings yet
- Mr. Abhijit Bhoyar Lecturer M. Sc. NursingDocument36 pagesMr. Abhijit Bhoyar Lecturer M. Sc. Nursingseeya rayamajhiNo ratings yet
- Pre & Post Operative Nursing CareDocument33 pagesPre & Post Operative Nursing CareJohnmark SimonNo ratings yet
- Take Home Quiz - Respi Quiz 2 1Document2 pagesTake Home Quiz - Respi Quiz 2 1Andrea Albester GarinoNo ratings yet
- Percutaneous Tracheostomy Guideline - 3.26.14 - June 2014Document5 pagesPercutaneous Tracheostomy Guideline - 3.26.14 - June 2014joseL1994No ratings yet
- Chest Tube Insertion: Prepare By: Amrita:Thapa Roll No. 7Document39 pagesChest Tube Insertion: Prepare By: Amrita:Thapa Roll No. 7sushma shresthaNo ratings yet
- 9 1 EndosDocument6 pages9 1 EndosmghNo ratings yet
- Tindakan TorakosentesisDocument15 pagesTindakan TorakosentesisAyu Ayu AyuNo ratings yet
- ThoracentesisDocument21 pagesThoracentesisAmna BatoolNo ratings yet
- Pre and OpDocument6 pagesPre and OpFatimah Alshareef100% (1)
- Reviewer RLEDocument30 pagesReviewer RLEEmman RamosNo ratings yet
- 4 - Post Operative Nursing ManagementDocument38 pages4 - Post Operative Nursing ManagementraghadNo ratings yet
- Nursing Care Plan An Unoccupied Bed Is PreparedDocument13 pagesNursing Care Plan An Unoccupied Bed Is PreparedDevhan RyuNo ratings yet
- Thoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnDocument7 pagesThoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnaparnaNo ratings yet
- ThoracentesisDocument36 pagesThoracentesisMarivic DianoNo ratings yet
- Appendicitis 191217094731Document37 pagesAppendicitis 191217094731OloanNo ratings yet
- THORACENTESISDocument11 pagesTHORACENTESISJeann sumbillaNo ratings yet
- Macro PneumohemoDocument28 pagesMacro PneumohemoSiti AishahNo ratings yet
- Chest Drainage Medical ManagementDocument3 pagesChest Drainage Medical ManagementPaul John RutaquioNo ratings yet
- SuctioningDocument17 pagesSuctioningKandi Issaya100% (1)
- Abdominal ParacentesisDocument5 pagesAbdominal ParacentesisVijith.V.kumar100% (1)
- AtlsDocument23 pagesAtlsRiri100% (1)
- ReportDocument60 pagesReportNikky Rossel Flores100% (1)
- Endoscopic Procedure (Nursing Responsibilities)Document4 pagesEndoscopic Procedure (Nursing Responsibilities)YessaminNo ratings yet
- Neck DissectionDocument24 pagesNeck Dissectionhayat al akoumNo ratings yet
- Bone Marrow AspirationDocument14 pagesBone Marrow AspirationhelloaNo ratings yet
- Tracheostomy SlidesDocument24 pagesTracheostomy SlidesMohammed AdamNo ratings yet
- Bachelor of Science in NursingDocument17 pagesBachelor of Science in NursingGeorgia De OcampoNo ratings yet
- Extubation After Difficult IntubationDocument3 pagesExtubation After Difficult Intubationramanrajesh83No ratings yet
- ColonosDocument20 pagesColonosCarl miguel LoretoNo ratings yet
- Chest Tube: Ministry of Higher Education and Scientific Research Al-Mustaqbal University College Department of NursingDocument10 pagesChest Tube: Ministry of Higher Education and Scientific Research Al-Mustaqbal University College Department of NursingMr. abbas fahim hamidNo ratings yet
- Intraoperative NotesDocument22 pagesIntraoperative NotesIsabel AranconNo ratings yet
- Trauma KepalaDocument31 pagesTrauma KepalaMuhammad ArifNo ratings yet
- Role of Anesthesia Nurse in Operation TheatreDocument37 pagesRole of Anesthesia Nurse in Operation TheatreZainul SaifiNo ratings yet
- July 27, 2009 Exploratory Laparotomy and Transverse Loop Colostomy 1.Document8 pagesJuly 27, 2009 Exploratory Laparotomy and Transverse Loop Colostomy 1.MaRVNo ratings yet
- NANDA DefinitionDocument5 pagesNANDA DefinitionAngel_Liboon_388No ratings yet
- Pleural Effusion: o o o oDocument5 pagesPleural Effusion: o o o oAisyahKautsarIlmiNo ratings yet
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANOFrom EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONo ratings yet
- Battle of UhadDocument14 pagesBattle of UhadMuiz “Daddy” AyubiNo ratings yet
- Econometrics PPT Final Review SlidesDocument41 pagesEconometrics PPT Final Review SlidesIsabelleDwightNo ratings yet
- Las Health 9 Quarter 4Document25 pagesLas Health 9 Quarter 49 - Sampaugita - Christian RazonNo ratings yet
- 23.09 Chapter 9 The Mughal EmpireDocument2 pages23.09 Chapter 9 The Mughal EmpireSima SinghNo ratings yet
- OptiX OSN 1800 Product OverviewDocument44 pagesOptiX OSN 1800 Product OverviewvladNo ratings yet
- Pobre Vs Mendieta GR 106677Document7 pagesPobre Vs Mendieta GR 106677Judel MatiasNo ratings yet
- JAR ATPL 032 PerformanceDocument20 pagesJAR ATPL 032 PerformanceMohamed Fariz100% (1)
- Creative Thinking of Low Academic Student Undergoing Search S PDFDocument18 pagesCreative Thinking of Low Academic Student Undergoing Search S PDFgiyonoNo ratings yet
- Literary Criticism of Graham GreeneDocument4 pagesLiterary Criticism of Graham GreeneAmylea SyazlinaNo ratings yet
- Genius Report - TempoDocument7 pagesGenius Report - TempoJerelyn Rose PalayNo ratings yet
- Psychological First Aid and Nursing: ReviewDocument7 pagesPsychological First Aid and Nursing: ReviewMarcelo Fernandez GomezNo ratings yet
- Preparing A Time of PrayerDocument3 pagesPreparing A Time of PrayerJeff Rey Casiño DalubatanNo ratings yet
- Using BIPublisher Memory Guard-1Document8 pagesUsing BIPublisher Memory Guard-1Ra12appsNo ratings yet
- Articulated Light: The Emergence of Abstract Film in AmericaDocument16 pagesArticulated Light: The Emergence of Abstract Film in AmericaitkusNo ratings yet
- Am IiiDocument1 pageAm IiibsbsbNo ratings yet
- General Morphological AnalysisDocument11 pagesGeneral Morphological AnalysisVictor LopezNo ratings yet
- EDSP 5320-D03 Spring 2020 Sunshine Valdilles - Project 2Document2 pagesEDSP 5320-D03 Spring 2020 Sunshine Valdilles - Project 2Sunshine Corliss ValdillesNo ratings yet
- Cant Tales UnitDocument14 pagesCant Tales Unitapi-295739816No ratings yet
- Pub Strategic Management Issues and CasesDocument264 pagesPub Strategic Management Issues and CasesCepi Juniar PrayogaNo ratings yet
- Textos de Las 116 PaginasDocument2 pagesTextos de Las 116 PaginaschaluloNo ratings yet
- The Constitution: I. Municipal Trial Courts and Municipal Circuit Trial CourtsDocument3 pagesThe Constitution: I. Municipal Trial Courts and Municipal Circuit Trial CourtsEduardo SurioNo ratings yet
- Anemia in PregnancyDocument5 pagesAnemia in PregnancySandra GabasNo ratings yet
- Arab Solfege PDFDocument167 pagesArab Solfege PDFRodrigo S BatalhaNo ratings yet
- Organizational Culture and Job Satisfaction in Bank: Perceptions and Reactions of EmployeesDocument14 pagesOrganizational Culture and Job Satisfaction in Bank: Perceptions and Reactions of EmployeesFun ki FlightNo ratings yet
- DelTech MUN 2024 BrochureDocument13 pagesDelTech MUN 2024 Brochureshwetas1807No ratings yet
- Ghana: InstructionsDocument2 pagesGhana: InstructionsBright KorantengNo ratings yet
- Chesterton - Outline of SanityDocument82 pagesChesterton - Outline of SanityKeith BuhlerNo ratings yet
- Perdev Week 1 - Lesson 4Document3 pagesPerdev Week 1 - Lesson 4Namja Ileum Ozara GaabucayanNo ratings yet
- All Tenses 1Document2 pagesAll Tenses 1Marina SanchezNo ratings yet