Professional Documents
Culture Documents
Ajr Am J Roentgenol 2020 214 2 296-305
Uploaded by
Fernando SousaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajr Am J Roentgenol 2020 214 2 296-305
Uploaded by
Fernando SousaCopyright:
Available Formats
Wo m e n ’s I m a g i n g • R ev i ew
Destounis et al.
Breast Density, Risk Estimation, and Supplemental Screening
Women’s Imaging
Review
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
Update on Breast Density,
FOCUS ON:
Risk Estimation, and
Supplemental Screening
Stamatia V. Destounis1 OBJECTIVE. Dense breast tissue is an established risk factor for the development of
Amanda Santacroce breast cancer. Methods for reliable and reproducible identification of breast density have been
Andrea Arieno developed and are increasingly being adopted into clinical practice, allowing enhanced iden-
tification of patients who will benefit from supplemental screening. Breast density is being
Destounis SV, Santacroce A, Arieno A used for patient risk stratification through incorporation into risk models, leading to more pre-
cise management and improved decision making regarding personalized screening strategies.
CONCLUSION. This review provides an update on breast density assessment, evalua-
tion of patient’s risk status, and the use of supplemental screening.
reast density notification legisla- ogy (ACR) BI-RADS [6]. Other qualitative
B tion has been adopted in more
than half of the states of the
United States. Increased breast
measures of breast density include the orig-
inal Wolfe classification [7] and the Tabar
patterns [8]. The Wolfe classification, as de-
density is an independent risk factor for the scribed first in 1976, classified women into
development of breast cancer; women in the four categories of parenchymal patterns
highest density category, classified as ex- based on the relative amounts of fat, epitheli-
tremely dense (d), are four to six times more al and connective tissue densities, and prom-
likely than women with fatty tissue to devel- inent ducts seen on mammography [7]. The
op breast cancer [1, 2]. Further, the presence Tabár patterns, from 1997, went beyond clas-
of dense breast tissue limits the sensitivity of sifying on the basis of simple tissue patterns
mammography because of the masking ef- and instead is based on anatomic-mammo-
fect [3]. Legislation varies from state to state, graphic correlation using a 3D subgross tech-
ranging from only requiring reporting of nique [8]. Table 1 compares these two meth-
breast density to the patient to reporting den- ods of categorizing breast density. Use of the
sity as well as describing the associated risks visual BI-RADS method has been criticized
of having increased breast density and the because of high rates of both intra- and in-
potential benefit of integrating additional terreader variability [9–13]. Further incon-
screening into the breast care plan. The risk sistency came to light with changes from the
stratification based on breast density that is 4th edition to the 5th edition of BI-RADS [4,
Keywords: breast density; breast imaging; occurring is guiding referral to supplemental 14] (Table 2). Assessment of breast density
risk assessment; supplemental screening screening [4, 5]. Simultaneously, the need for changed from a percentage value of the fi-
accurate and reproducible measures of breast broglandular tissue in relation to the whole
doi.org/10.2214/AJR.19.21994
density has increased because no recommen- breast area to a general visual impression by
Received July 10, 2019; accepted after revision dations for standardized breast density as- the image interpreter, putting more weight
September 5, 2019. sessment are currently available. on the masking effect of dense tissue and al-
1
This review provides an update on breast lowing the reader to categorize the breast as
All authors: Elizabeth Wende Breast Care, LLC,
density assessment, evaluation of patient’s risk dense when only a focal area of dense tis-
170 Sawgrass Dr, Rochester, NY 14620. Address
correspondence to S. V. Destounis status, and the use of supplemental screening. sue is present [6]. The impact of this change
(sdestounis@ewbc.com). in practice is not fully defined, though a few
Breast Density Assessment small-scale studies have found that the new
AJR 2020; 214:296–305 Visual Density Assessment guidelines lead to an increase in dense as-
0361–803X/20/2142–296
The most widely used method to assess sessments [15, 16]. One such investigation
breast density has been visual assessment found an overall decrease in fatty assess-
© American Roentgen Ray Society guided by the American College of Radiol- ments of 5.0%, 2.8% increase in scattered,
296 AJR:214, February 2020
Breast Density, Risk Estimation, and Supplemental Screening
TABLE 1: Comparison of Wolfe Classifications and Tabár Patterns
Categorization Description Risk Level
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
Wolfe classification
N1 Normal Lower
P1 Composed mostly of fat, displaying prominent ducts behind the areola or in the upper axillary quadrant occupying no Lower
more than 25% of the breast
P2 A more prominent duct pattern than P1, a quarter or more of the breast occupied Higher
DY General increase in breast density with possible minor involvement of prominent ducts Higher
Tabár pattern
I Predominantly dense tissue with nodular densities, regions of fatty tissue Lower
II Completely fatty breasts Lower
III Mostly fatty breast with visible ducts behind areola Lower
IV Predominantly dense breasts with linear and nodular densities Higher
V High levels of homogeneous density Higher
2.6% increase in heterogeneously dense, riods, using three different mammographic [22] posited that adopting automated meth-
and 0.4% decrease in extremely dense as- screening modalities: FFDM alone, FFDM ods will greatly reduce the variability of den-
sessments [17]. When categorizing the four with DBT, and synthetic mammography with sity assessments, help standardize density
densities into two categories (dense and non- DBT. Readers visually assessed breast den- thresholds for supplemental screening, and
dense), there was an increase in dense assess- sity in a dichotomized fashion (nondense or better refine risk assessment and personal-
ments. Adaptation to the new guidelines has dense). A transition to more nondense assess- ized screening. Semiautomated and fully au-
varied from radiologist to radiologist. ments is a significant finding that would ben- tomated methods take a variety of approach-
Further discrepancies in density assess- efit from large-scale investigation, because es to density measurement; some are 2D
ment have been noticed with the widespread the impact of fewer women being classified area-based, others use 3D volumetric-based
adoption of digital breast tomosynthesis as having dense breasts would lead to fewer methods [23].
(DBT), with or without the synthetic view, recommendations for supplemental screen- Cumulus (University of Toronto) and
leading to the recent incorporation of a new ing based solely on breast density. However, Madena (Eye Physics) are two examples of
section to the BI-RADS atlas [18]. This shift Gastounioti et al. performed density assess- semiautomated interactive methods [24, 25].
has had implications for density assessment, ment visually, and this method comes with These methods use segmentation and thresh-
particularly when a facility is using the syn- known limitations. olding performed by the image interpreter to
thetic view in place of full-field digital mam- Increased awareness of breast density separate the breast edge and the areas of den-
mography (FFDM), because the synthetic has been accompanied by growing criticism sity on the mammogram; each pixel within
view can look very different from traditional about making screening recommendations the breast area is segmented into either fat
FFDM. Just how this impacts density assess- based on the subjective visual BI-RADS as- or fibroglandular tissue. Automated tech-
ment is not completely understood, though sessment. This controversy has been a driv- niques utilizing an area-based approach in-
Zuckerman et al. [19] and Aujero et al. [20] ing force behind the growth of automated clude ImageJ (National Institutes of Health),
reported that more breasts are categorized methods of density assessment. MedDensity (Giulio Tagliafico), the STRA-
as nondense than dense when using the syn- TUS algorithm, Libra (Computational Breast
thetic image. Gastounioti et al. [21] report- Semiautomated and Fully Automated Imaging Group), and PowerLook (iCAD),
ed density differed with imaging modali- Density Assessment which was formerly known as iReveal [26–
ty, with more breasts classified as nondense Automated density software has been in- 30]. Studies have found comparable perfor-
with DBT and synthetic mammography. troduced to address the subjective nature of mance between some of these methods, as
That study evaluated three different time pe- visual assessment. Conant and colleagues well as in comparison with visual BI-RADS
TABLE 2: Comparison of the BI-RADS 4th Edition and 5th Edition Density Assessments
4th Edition 5th Edition
Assessment Breast Tissue Characteristics Assessment Breast Tissue Characteristics
1 Almost entirely fatty (< 25% glandular) a Almost entirely fatty
2 Scattered densities (approximately 25–50% glandular) b Scattered areas of fibroglandular density
3 Heterogeneously dense, which could obscure detection of c Heterogeneously dense, which may obscure detection of small
small masses (approximately 51–75% glandular) masses
4 Extremely dense, which may lower the sensitivity of d Extremely dense, which lowers the sensitivity of mammography
mammography (> 75% glandular)
AJR:214, February 2020 297
Destounis et al.
assessment [27, 31–33]. Despite some posi- es the reliability of the software [34]. Posi- the door open for further work. Research is
tive results, limitations have been reported, tive performance of some of these methods is ongoing to improve the accuracy and consis-
including being time-consuming, difficult, important, because it gives radiologists con- tency of density assessment.
and prone to inter- and intraobserver subjec- fidence in taking an automated approach to
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
tivity [34–36]. These limitations are largely assessing breast density. However, the pur- Density Assessment and Risk Prediction
the reasons that such methods have not been chase, use, and maintenance of these prod- Automated density measures have also
routinely incorporated in clinical practice. ucts can be associated with significant cost, been applied as a predictor of risk for the de-
Two of the most well-known fully auto- which may be a limiting factor to widespread velopment of breast cancer. The risk of ad-
mated volumetric-based methods are Volpa- clinical adoption. vanced cancer has been reported to be four
ra and Quantra [37, 38]. Both methods take a times higher for women with extremely
volumetric quantitative density measurement Role of Augmented Intelligence in dense breasts than for all other women when
and have been shown to be reliable and re- Density Assessment using a fully automated breast density mea-
producible [39–41]. These methods has been Application of deep learning (DL) meth- surement for predicting the risk of advanced-
largely used with FFDM, but positive re- ods for density assessment is an expanding stage diagnosis and the first negative screen-
sults have also been seen when using DBT, area of research. Lehman et al. [46] devel- ing round [50]. This finding is comparable
which is necessary because DBT continues oped a DL method to assess BI-RADS breast with that of a similar publication, which
to be adopted in clinical practices at a high density using the original interpretation by found that the highest risk for developing
rate. Agreement between visual BI-RADS an experienced radiologist. The algorithm breast cancer was for women with breasts
and automated density grades by Volpara was developed and tested on randomly se- in the highest density category [42]. In that
have shown moderate agreement (weighted lected digital mammograms, with BI-RADS retrospective study, Destounis et al. [42]
κ = 0.512) [42]. Youk et al. [15] compared vi- breast density recorded by one of 12 radi- found breast density was the only risk factor
sual assessments by radiologists using both ologists specializing in breast imaging. The significantly associated with the diagnosis of
the BI-RADS 4th and 5th editions; the re- model was trained to map images in a single interval cancer versus screen-detected can-
sults were then correlated with automated view to assess breast density. To combine the cer, for both visual BI-RADS assessment and
assessment by Quantra. Interobserver agree- density assessments from each view into an automated volumetric breast density (VBD).
ment on breast density category was moder- assessment for the examination, researchers Results from this study showed a strong lin-
ate to substantial (κ = 0.58–0.63) with the 4th used the consensus density across views. A ear relationship between sensitivity of mam-
edition and substantial (κ = 0.63–0.66) with reader study compared agreement between mography and automated volumetric breast
the 5th edition, but there was not a significant the DL model and the majority consensus of density, with substantial decreases in sensi-
difference between the two. The proportion five breast imagers, between the DL model tivity for women in the two higher automated
of dense breast assignments increased, and and the original interpreting radiologist, and density groups (the equivalent of BI-RADS c
the proportion of fatty breast assignments between the majority consensus and the orig- and d). Visual BI-RADS assessment showed
decreased with use of the 5th edition com- inal interpreting radiologist. After that, the women whose breasts were in the highest
pared with the 4th edition (p < 0.0001) when algorithm was implemented clinically. Table density category were 3.6 times more like-
assessing intraobserver agreement. Auto- 3 provides a summary of the study findings. ly than women in the two lower categories
mated assessment had a significant correla- The DL model showed very good agreement to have an interval cancer diagnosis. Ac-
tion with both editions of BI-RADS visual with radiologists in the clinical setting, with cording to quantitative VBD results, wom-
assessment. Eom and colleagues [43] report- 94% of the binary dense versus nondense en in the highest quartile were four times as
ed similarly high agreement levels between DL assessments accepted by the interpreting likely as those in the lower quartile to have
visual assessment and volumetric assess- physician; 90% were accepted in the four- a diagnosis of interval versus screen-detect-
ment; in particular, the agreement between category BI-RADS assessment. This is a ed cancer, leading the authors to conclude
nondense and dense categories was almost promising investigation with a new tool that that VBD more precisely captures the poten-
perfect between readers and Volpara (κ = may be able to address concerns regarding tial masking risk of dense breasts. As part
0.83). Tromans and colleagues (presented accurate density assessment to properly allo- of the ongoing Predicting Risk of Cancer
at the European College of Radiology 2014 cate supplemental screening resources. Oth- at Screening, or PROCAS, study, research-
annual meeting) evaluated density assess- er DL methods have been investigated for ers compared density assessment by visu-
ment between FFDM and DBT and report- density assessment [47–49]; however, none al analog scale (VAS), Cumulus, Densitas
ed Volpara had a strong positive agreement were included in clinical practice, leaving (Densitas), Quantra (Hologic), and Volpara
with BI-RADS (κ = 0.953) and a volumet-
ric breast density correlation between DBT TABLE 3: Summary of Findings From Lehman et al. [46]
and FFDM (r = 0.903). Phantom work with Comparison κ
Quantra has found that breast density is 10%
Deep learning model vs original interpretation (test set) 0.67
higher with DBT than with FFDM [44]. Cu-
mulus has shown strong intra- and interuser Deep learning model vs original interpretation (reader consensus setting) 0.62
correlations and agreement with DBT [45]. Reader consensus vs original interpretation 0.63
MedDensity has shown moderately positive Deep learning model vs reader consensus 0.78
correlation of BI-RADS with DBT, though
Deep learning model vs final radiologist assessment (clinical implementation) 0.85
image noise limits its capabilities and reduc-
298 AJR:214, February 2020
Breast Density, Risk Estimation, and Supplemental Screening
(Volpara Solutions) [51]. VAS was found to ies has been a recent genetic advancement, DL) using mammograms alone, and a hybrid
be the strongest predictor of screen-detect- with this information allowing improved risk DL model using both traditional risk factors
ed cancer at study entry, after adjustment for assessment at the individual level [55]. A re- and mammography images [67]. Comparisons
classic risk factors, in the highest versus low- cent study, OncoArray [60], reported that were made with the TC version 8 model (TC
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
est percent density. Volpara and VAS showed 18% of familial risk of breast cancer can be 8). When the image-only DL model was used,
a significant trend with increasing density. explained by SNPs [61]. At least one com- 31% of women were identified as having high
Densitas and Cumulus percent density mea- monly used risk assessment model, TC, now risk, compared with 18% when the TC 8 mod-
sures were also statistically significant when gives the option to include SNP information, el was used. The hybrid DL model was found
comparing the highest quintile to the lowest; if available. Polygenic risk scores (PRSs) have to be significantly more accurate than TC 8
for Quantra there was no significant associ- been developed, which when combined with (AUC of 0.70 vs 0.62, respectively). Interest-
ation. Although VAS was found to predict other classic factors can be used to estimate ingly, the image-only DL model outperformed
breast cancer risk significantly better than an individual’s risk. Research is continuing in TC 8; in particular, when traditional risk factor
all other density assessment methods, the au- this area, evaluating the potential to ultimate- information was unavailable, the image-only
thors cautioned that use of this method is un- ly stratify women according to PRS. PRS pro- DL model was able to provide more accurate
likely for wide-scale stratified screening and vides powerful risk discrimination; even bet- risk assessment. This difference can have im-
thus conclude that Volpara or Densitas pro- ter risk discrimination will be obtained by portance in clinical practice because of limi-
vide the most practical solution. As breast combining the PRS with family history and tations of patient-reported family history. The
imaging moves closer to personalized risk- other risk factors [62]. Continued studies to incorporation of images is a common trend
based assessments, determining which den- validate risk models including genetic, hor- in the new research occurring for risk assess-
sity methods are the most appropriate will be monal, and lifestyle factors, will be needed. ment. Harvard researchers collected screening
increasingly important. Automated assess- The incorporation of this level of individual- breast MR images and developed a DL mod-
ment tools will likely play a large role. ized genomic information will lead to a new el to predict 5-year breast cancer risk of a pa-
level of personalized risk assessment, stratifi- tient on the basis of a single breast MR image
Risk Estimation cation, and management. from the patient’s screening MRI examina-
Individual risk for developing breast can- The addition of mammographic density tion [68]. The single image used for this study
cer varies between 11.6% for women of aver- to breast cancer risk models has shown im- was a manipulated image, created by subtract-
age risk and 85% for women with pathogenic proved predictive power [63–66]. A study by ing the unenhanced 3D dataset from the con-
germline mutations in highly penetrant genes Brentnall et al. [63] incorporated mammo- trast-enhanced 3D dataset, leaving a single 3D
(i.e., BRCA1, BRCA2, TP53, and PTEN) [52– graphic breast density into the Gail and TC volumetric image. Then, the axial view of the
56]. Assessment of individual risk is critical models, resulting in improvement in AUCs maximum intensity projection was used to
for tailoring screening and prevention strat- from 0.55 and 0.57 to 0.59 and 0.61, respec- convert this 3D volumetric image to a 2D im-
egies appropriate to the distinct risk lev- tively. A more recent study by Brentnall and age. The model was trained to map a patient’s
el. The determination of a patient’s risk in- colleagues [64] found that the addition of risk factors at the time of an MRI examina-
volves many factors, traditionally including volumetric and visual density assessment tion to determine whether the patient had can-
family history, hormonal factors, body mass to traditional risk factors can improve risk cer develop within 5 years using the previously
index (BMI), and hormone therapy use [53, stratification. When mammographic density described 2D projection image. The DL mod-
57–59]. Some of the most commonly used was added to the TC model, both volumet- el’s performance was compared with a logis-
risk assessment models in the clinical setting ric and visual assessment increased the ac- tic regression model based on traditional risk
are the Gail, Claus, and Tyrer-Cuzick (TC) curacy of risk prediction, with odds ratios of factors in addition to personal history of breast
models. Each considers a different combina- 1.55 and 1.40, respectively. The study also cancer and background parenchymal enhance-
tion of the classic risk factors. The Gail mod- found that adding mammographic density ment on MRI and the TC 8 model. Table 4
el uses reproductive and biopsy information, affected the number of women assessed as provides a summary of the performance of the
with limited family history [53]. The Claus having high risk. When the TC model was three models. The image DL model showed
model includes greater family history (first- used without density, 4.8% of the population improved individual risk discrimination com-
and second-degree relatives) but does not in- was found to be at high risk; this increased to pared with the TC model.
clude other factors such as hormonal factors 7.1% with incorporation of BI-RADS densi-
or biopsy history [57]. TC is the more com- ty and 6.8% when combined with volumetric Impact of Risk Assessment on Clinical Practice
prehensive of these models, using reproduc- density. Combining breast density with clas- Finding a comprehensive model to deter-
tive history, biopsy history, extended family sic risk factors almost doubled the number of mine the most accurate and individualized
history, and BMI [58]. Recent advancements patients identified as being at high risk.
have led to the incorporation of polygenic Because of efforts to provide more inclu- TABLE 4: Summary of Findings From
risk information and breast density with the sive breast cancer risk assessment models for Portnoi et al. [68]
goal of increasing risk assessment accuracy. clinical use, DL methods are taking develop-
ment further. Three models use risk factor in- Model Mean AUC ± SD
Advancements in Risk Assessment Models formation from the patient’s medical record Image-based deep learning 0.638 ± 0.094
Identification of over 100 single nucleotide and provide risk within 5 years: a risk fac- Risk factor logistic regression 0.558 ± 0.108
polymorphisms (SNPs) associated with breast tor–based logistic regression model using tra-
Tyrer-Cuzick 0.493 ± 0.092
cancer through genomewide association stud- ditional risk factors, a DL model (image-only
AJR:214, February 2020 299
Destounis et al.
lifetime risk score for patients is a large fo- Patient and Physician Knowledge and five states with notification of the presence
cus to allow accurate stratification of wom- Understanding of Breast Density and of dense tissue but no mention of potential
en into groups at different levels of risk, Supplemental Screening benefits and another group of four states with
ultimately allowing more informed deci- Recently, the U. S. Food and Drug Admin- notification of dense tissue and a brief expla-
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
sion-making regarding supplemental screen- istration acknowledged the importance of nation of potential benefits of supplemen-
ing and prevention. Individualized risk as- women being informed of their own breast tal screening. Utilization was 1.3 per 1000
sessment is an important service to offer, yet anatomy to make informed health decisions women higher in the group notified of po-
it is important to ensure that there is patient and proposed a rule to amend the reporting tential benefits, suggesting women may ben-
access and understanding. A large, popula- requirements of mammography results to in- efit from a more detailed explanation along
tion-based study found that most patients re- clude a woman’s personal breast density [70]. with tissue type notification. This is impor-
ported wanting genetic testing, but only 29% This rule would impact the information giv- tant information for providers, because sim-
reported having it [69]. Only 52.9% of pa- en to women in 15 states because although ply informing women of their tissue type is
tients at high risk reported having genetic 38 states have mandated Dense Breast No- not enough to influence participation in addi-
testing. Patients described lack of a physi- tification laws, three of those do not include tional screening.
cian’s recommendation, not expense, as their informing women of their breast density. A Research has shown that once women are
primary reason for not testing. The study au- mandate at the federal level would have pow- informed of their breast density, the option
thors suggested improving physicians’ com- erful implications for women’s autonomy for supplemental screening, or both, many
munication skills with patients, along with over their own breast health. Although the reach out to their physicians to discuss [77].
assessment of patients’ risk and desire for movement for notification has been in place However, recent studies have found that pri-
testing, to better guide appropriate patients for several years, studies are continuing to mary care physicians do not feel fully educat-
toward risk assessment and testing. These find general confusion and lack of under- ed or prepared to answer all questions on this
changes will ultimately lead the way to en- standing concerning the meaning of dense topic [78, 79]. A recent survey of breast im-
suring that patients at higher risk are not tissue and the implications for screening [71– aging radiologists questioned the perceived
only identified but also understand the im- 74]. Santiago-Rivas et al. [75], through use adequacy of patient-provider conversations
portance of their risk level and can be pro- of a survey, reported that most participants regarding screening guidelines and found
vided the information they need to pursue had heard about breast density but less than that radiologists largely feel patient-provider
supplemental screening. one-third knew their personal breast density. discussions are inadequate, specifically cit-
Knowledge of the impact of breast density on ing that discussions regarding supplemental
Breast Density Implications for the accuracy of mammography was found to screening for increased breast density should
Supplemental Screening Practices be associated with the likelihood of complet- be standardized [80]. Most respondents re-
As risk assessments become more com- ing supplemental ultrasound, highlighting ported breast density information is includ-
prehensive, a large population of women the importance of having an informed con- ed in patient letters and radiology reports
are being notified of their lifetime risk for versation with patients. Busch et al. [76] in- yet feel further patient education regarding
breast cancer for the first time [64]. Wom- vestigated the association of dense breast no- breast density and supplemental screening
en who have significant factors that increase tification on the utilization of supplemental should be performed by radiologists.
their risk score above designated thresh- ultrasound and whether the type of informa-
olds (frequently > 20% lifetime risk) are in tion in the notification had an influence. The Breast Density Is Shifting Screening
the higher-risk category, which has well-de- study included 1.2 million women who un- Recommendations
fined screening guidelines. A larger num- derwent 1.4 million screening mammograms With more women being told they have
ber of women, however, are finding them- from 34 states, nine of which had adopted dense breasts, identification of best screening
selves in the vaguely defined moderate-risk dense breast notification and 25 of which practices for this population is needed [15, 81,
group, which is lacking consensus and clar- with no dense breast notification. The nine 82]. Mammography is the reference standard
ity on appropriate management. The incor- states selected had supplemental ultrasound screening modality regardless of density,
poration of breast density into updated risk as a covered benefit and were included to de- with the proven ability to reduce breast can-
assessment models has changed this land- crease the likelihood that cost was a decid- cer mortality [83]. Nevertheless, reduced per-
scape further by identifying a new subset of ing factor in pursuing supplemental screen- formance in certain populations of women,
women who are at increased risk because of ing. The results showed that in the population primarily those with increased breast densi-
their breast density. Simultaneously, there of women who received notification that they ty, has led to the use of other imaging mo-
has been a nationwide movement to inform had dense breasts, an additional 10.5 individ- dalities for supplemental screening, primar-
women of their breast density, with the goal uals per 1000 followed the screening mam- ily DBT, breast ultrasound, and breast MRI.
of making those in the highest density cat- mogram with screening ultrasound, result- Organizations have issued position state-
egories aware and providing information on ing in a statistically significant increase: ments on supplemental screening; however,
the risks of dense tissue and potential bene- 0.37 more breast cancers detected per 1000 the messages are often ambiguous and non-
fit of additional screening. The combination mammograms. The study further differenti- committal. The latest position statement by
of these factors have catapulted discussion of ated the population who received the dense the American Cancer Society acknowledg-
best screening practices for this population, breasts notification, distinguishing utiliza- es that both ultrasound and MRI have higher
but so far, there are no formal screening or tion rates between two groups of states based cancer detection rates in women with dense
management recommendations. on the notification received: one group of breast tissue but also describes the low speci-
300 AJR:214, February 2020
Breast Density, Risk Estimation, and Supplemental Screening
ficity, resulting in increased rates of unneces- “somewhat likely” to recommend supple- Studies have found that some cancers
sary tests and biopsies. The advice given is mental ultrasound. Patients highly value the missed by DBT can be detected on supple-
to “talk with your healthcare provider about recommendation of radiologists; higher rates mental ultrasound or MRI. The ability of ul-
whether you should have other tests” [84]. In of referrals and utilization could occur if ra- trasound and MRI to find additional mam-
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
a similar vein, recent ACR Appropriateness diologists were more likely to recommend mographically occult cancers is broadly
Criteria for breast cancer screening give sup- ultrasound screening, as a recent study in acknowledged, but there are known draw-
plemental ultrasound for women with dense the AJR found [88]. Of 751 women with nor- backs to these technologies that prevent
breasts (of all risk levels) a “may be appropri- mal mammograms and breast density of het- widespread endorsement of their routine
ate” rating [85]. The ACR acknowledges that erogeneously or extremely dense breasts, the use. Although a complete enumeration of the
dense breast tissue lowers mammograph- study examined the return rate for a screen- benefits and drawbacks are outside the scope
ic sensitivity and that adding ultrasound in- ing ultrasound on the basis of the type of fol- of this article, we briefly highlight the most
creases the cancer detection rate but at the low-up communication the patient received. common advantages and disadvantages of
cost of a substantial increase in false-positive One-third of the women received a letter these supplemental screening modalities and
rates. Ultimately, the criteria state that add- stating mammography was normal, with no indicate areas of current research seeking to
ing ultrasound may be useful, but the balance mention of density or supplemental screen- improve on the limitations.
of benefits and harms should be considered ing benefits. Another one-third received a
when making the decision to use supplemen- letter indicating a normal mammogram and Screening Ultrasound
tal ultrasound. The suggestion for patients to included the density category. When appli- Screening breast handheld ultrasound
balance the benefits and harms and have in- cable, an explanation of how supplemental (HHUS) has been shown in several single-
formed conversations with healthcare pro- screening may be beneficial was included. and multiple-institution studies to detect
viders follows an increasing trend toward The remaining one-third received the same breast cancers otherwise missed by mam-
personalized screening with the intent of al- letter as the second group and received a fol- mography, including DBT [96–98]. Addi-
lowing women to make decisions regarding low-up telephone call from the radiology of- tional benefits aside from increased cancer
their healthcare on the basis of informed con- fice reiterating the mammography results, detection include no ionizing radiation and
versations and individual risk level. presence of dense tissue, and possible ben- no need for contrast agents. The increased
efit of supplemental screening. The group cancer detection rate with HHUS combined
Current and Future Use of Supplemental of women receiving the letter with densi- with mammography is reportedly up to 4.3
Screening Modalities ty information and benefits of supplemental cancers per 1000 women screened, and most
A recent study by Liao and colleagues screening had a return rate for supplemental of these cancers are stage 0 or 1 [99–102].
[86] investigated physician ordering levels ultrasound of 48.8%, and the group who re- However, HHUS has drawbacks that prove to
of screening ultrasound examinations. The ceived the letter and a follow-up telephone be limiting factors for its widespread use in
study used the National Ambulatory Medi- call had a return rate of 86.9%. In compari- a screening setting, including that it is oper-
cal Care Survey data to analyze screening son, women who received no information re- ator-dependent, lacks reproducibility, is time
ultrasound ordering rates before and after garding density, supplemental screening, or intensive, and requires specially trained staff
mandated dense breast notification. The phy- a follow-up call had a 9.9% return rate. Such [103]. Automated systems (i.e., automated
sicians included were primarily from prima- results illustrate the important influence a ra- breast ultrasound [ABUS]) have been devel-
ry care, family practice, internal medicine, diologist’s advice can have on patients. oped to improve on the limitations of HHUS.
and gynecology and encountered patients ABUS removes the dependence on a skilled
at preventive services wellness visits. Of Digital Breast Tomosynthesis operator to perform the examination, utiliz-
the 12,787 visits that met inclusion criteria, DBT use in the United States has increased ing an automated scanner. ABUS has been
22.1% received mammography referrals and exponentially since 2011 when it received ap- shown to provide reproducible, high-resolu-
3.3% received screening ultrasound referrals. proval from the Food and Drug Administra- tion images. Results from several prospec-
Referral rates did not change significantly af- tion. Value has been shown in utilizing DBT tive studies have shown that ABUS increases
ter legislation took effect (3.9% before and as a supplement to FFDM, with large retro- cancer detection rates and has specificity and
4.2% after legislation). These low rates show spective and prospective studies consistent- sensitivity comparable with those of HHUS
that physicians are not ordering supplemen- ly showing increased cancer detection rates, [101, 104, 105], showing that ABUS is a fea-
tal tests but could also indicate that women reduced recall rates, and increased sensi- sible alternative to HHUS for screening pur-
are not asking for them. A recent survey by tivity [89–92]. Since 2011, DBT has proven poses. A commonly cited criticism of both
the Society of Breast Imaging sought to dis- more effective not only as a supplemental of these methods is the false-positive rate,
cover what supplemental screening practic- tool but also as a primary screening device which has been shown to be substantially
es and recommendations are occurring in for all breast types [93]. DBT has also been more than what is seen with mammography
clinical practice [87]. The survey results re- shown to perform well in imaging women screening. Recent investigations have exam-
vealed DBT is recommended at the highest with dense breast tissue [94]. However, many ined the utility of additional automated ultra-
rate, with radiologists stating they are “like- practices have not been able to make a com- sound applications with the goal of decreas-
ly” and “very likely” to recommend DBT, plete transition, working with a limited num- ing the number of false-positives, including
regardless of patient risk level. The level of ber of units or no units at all. In these hybrid optoacoustic breast imaging, contrast-en-
endorsement for ultrasound was not as high, scenarios, practices frequently use DBT as a hanced ultrasound, and elastography. Opto-
with the respondents stating they were only supplement to FFDM [95]. acoustic imaging is a novel ultrasound ap-
AJR:214, February 2020 301
Destounis et al.
plication that fuses anatomic and functional cluded in any screening guidelines for this ty assessment will help to streamline the pro-
diagnostic imaging through use of laser op- group. The DENSE trial evaluated the effect cess of dense tissue identification in a way
tics and sound. The fusion of laser optic im- of supplemental MRI for women with ex- that is reproducible and reliable and allow
aging and gray-scale ultrasound gives this tremely dense breasts within a population- incorporation into risk assessment models,
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
technology the ability to depict structure and based screening program (Bakker MFLS, to permit the most accurate identification of
hemoglobin as well as relative oxygenation et al., presented at the European Congress women at higher than average risk. The hope
within and around breast masses. Results of of Radiology 2019 annual meeting). The re- is that this will lead to refinement in supple-
a prospective multicenter trial found that op- sults showed excellent performance in this mental screening guidelines as well as tai-
toacoustic ultrasound had better specificity population, with a cancer detection rate lored, personalized screening.
than the internal gray-scale ultrasound of the of 16.5/1000 and positive predictive val-
device in breast mass assessment [106]. ue for biopsy of 26.3%. This high detection References
Contrast-enhanced ultrasound (CEUS) has rate and positive predictive value for biopsy 1. McCormack VA, dos Santos Silva I. Breast den-
shown potential value in predicting benig- show MRI can be a useful tool for decreas- sity and parenchymal patterns as markers of
nity when evaluating breast masses. A pilot ing false-positives. Despite the evidence of breast cancer risk: a meta-analysis. Cancer
study evaluating CEUS to reduce the num- greatly increased benefit to women in this Epidemiol Biomarkers Prev 2006; 15:1159–1169
ber of benign breast masses recommended population, the deterrents of traditional MRI 2. Boyd NF, Martin LJ, Bronskill M, Yaffe MJ, Du-
for biopsy used prediction models and found still pose a problem for mainstream utiliza- ric N, Minkin S. Breast tissue composition and
that CEUS may reduce 31% of benign biop- tion, which has led the way for abbreviated susceptibility to breast cancer. J Natl Cancer Inst
sies for masses that are nonenhancing with breast MRI protocols to be developed. Re- 2010; 102:1224–1237
circumscribed margins or enhancing with an duced magnet time, shown to be as little as 3. Boyd NF, Guo H, Martin LJ, et al. Mammo-
oval shape and homogeneous enhancement 3 minutes, combined with reduced image in- graphic density and the risk and detection of
[107]. A meta-analysis similarly concluded terpretation time, can significantly reduce the breast cancer. N Engl J Med 2007; 356:227–236
that CEUS has good sensitivity and specific- cost of MRI and thus significantly increase 4. Kerlikowske K, Sprague BL, Tosteson ANA, et
ity for the characterization of breast lesions, the availability of screening MRI. Studies al. Strategies to identify women at high risk of
potentially being able to help reduce unnec- have shown that abbreviated MRI maintains advanced breast cancer during routine screening
essary benign biopsies [108]. the high level of cancer detection, sensitivity, for discussion of supplemental imaging. JAMA
Ultrasound elastography has been avail- and diagnostic accuracy of traditional MRI Intern Med 2019 Jul 1 [Epub ahead of print]
able for over 15 years, though use in clini- protocols [112–115]. By addressing the short- 5. Vourtsis A, Berg WA. Breast density implica-
cal practice remains relatively infrequent be- comings of MRI while maintaining levels of tions and supplemental screening. Eur Radiol
cause it has not been incorporated as standard diagnostic integrity, access can be increased 2019; 29:1762–1777
care. Recent advancements in elastography to groups of women outside of the higher- 6. D’Orsi CJ, Sickles EA, Mendelson EB, et al. ACR
technology include shear wave techniques. risk classification, such as women with dense BI-RADS Atlas, Breast Imaging Reporting and
Shear wave elastography was investigated in breast tissue. In the ongoing EA1141 trial, Data System. Reston, VA: American College of
a large multinational trial and was found to women without symptoms who are not de- Radiology, 2013
improve specificity of breast ultrasound mass fined as high risk (lifetime risk < 20%) with 7. Wolfe JN. Breast patterns as an index of risk for de-
assessment without a loss of sensitivity [109]. dense breasts undergo DBT and abbreviated veloping breast cancer. AJR 1976; 126:1130–1137
Acoustic radiation force impulse has been breast MRI in randomized order for 2 con- 8. Gram IT, Funkhouser E, Tabár L. The Tabar
introduced, which has two different modes: secutive years [116]. Participants then return classification of mammographic parenchymal
virtual touch tissue quantification and vir- to regular screening and are followed for an- patterns. Eur J Radiol 1997; 24:131–136
tual touch tissue imaging. Researchers have other 3 years. Cancer detection rates of DBT 9. Sprague BL, Conant EF, Onega T, et al. Variation
found potential with these techniques [110, compared with abbreviated MRI in the first in mammographic breast density assessments
111]. Many of these advancements seek to (prevalence) and second (incidence) screen- among radiologists in clinical practice: a multi-
improve on limitations of traditional ultra- ing rounds, along with positive predictive center observational study. Ann Intern Med 2016;
sound, but further work is needed for them to values and types of cancers found are the ob- 165:457–464
gain widespread acceptance. jectives for comparison and will provide in- 10. Kerlikowske K, Grady D, Barclay J, et al. Vari-
sight into the potential for abbreviated MRI ability and accuracy in mammographic interpre-
MRI and Abbreviated MRI in clinical practice for screening. tation using the American College of Radiology
Traditionally, screening MRI has not been Breast Imaging Reporting and Data System.
recommended to any group of patients out- Conclusion J Natl Cancer Inst 1998; 90:1801–1809
side of those with higher (> 20%) lifetime Dense breast tissue remains a significant 11. Ciatto S, Houssami N, Apruzzese A, et al. Cate-
risk, primarily because of the time the pro- topic in breast imaging. The acknowledg- gorizing breast mammographic density: intra-
cedure takes for the patient, the reading time ment of breast density as a risk factor has and interobserver reproducibility of BI-RADS
for the radiologist, the unknown effects of led to improvements in screening technolo- density categories. Breast 2005; 14:269–275
long-term gadolinium exposure, the rate of gies as well as a grassroots movement to in- 12. Ekpo EU, Ujong UP, Mello-Thoms C, McEntee
false-positives, and the high cost of the pro- form women of their breast density. Efforts MF. Assessment of interradiologist agreement
cedure. Because women with dense tissue do to standardize density assessment are neces- regarding mammographic breast density classifi-
not fall into the higher-risk category on the sary, with widespread adoption of automated cation using the fifth edition of the BI-RADS
basis of density alone, MRI has not been in- measures likely. The use of automated densi- Atlas. AJR 2016; 206:1119–1123
302 AJR:214, February 2020
Breast Density, Risk Estimation, and Supplemental Screening
13. Spayne MC, Gard CC, Skelly J, Miglioretti DL, 26. Li J, Szekely L, Eriksson L, et al. High-through- user manual. Bedford, MA: Hologic, 2012
Vacek PM, Geller BM. Reproducibility of put mammographic-density measurement: a tool 39. Wang J, Azziz A, Fan B, et al. Agreement of
BI-RADS breast density measures among com- for risk prediction of breast cancer. Breast mammographic measures of volumetric breast
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
munity radiologists: a prospective cohort study. Cancer Res 2012; 14:R114 density to MRI. PLoS One 2013; 8:e81653
Breast J 2012; 18:326–333 27. Tagliafico A, Tagliafico G, Tosto S, et al. Mam- 40. Alonzo-Proulx O, Mawdsley GE, Patrie JT,
14. D’Orsi CJ, Mendelson EB, Ikeda DM, et al. mographic density estimation: comparison Yaffe MJ, Harvey JA. Reliability of automated
Breast Imaging Reporting and Data System: among BI-RADS categories, a semi-automated breast density measurements. Radiology 2015;
ACR BI-RADS—breast imaging atlas. Reston, software and a fully automated one. Breast 2009; 275:366–376
VA: American College of Radiology, 2003 18:35–40 41. Engelken F, Singh JM, Fallenberg EM, Bick U,
15. Youk JH, Kim SJ, Son EJ, Gweon HM, Kim JA. 28. Eriksson M, Czene K, Pawitan Y, Leifland K, Bottcher J, Renz DM. Volumetric breast compo-
Comparison of visual assessment of breast density Darabi H, Hall P. A clinical model for identifying sition analysis: reproducibility of breast percent
in BI-RADS 4th and 5th editions with automated the short-term risk of breast cancer. Breast density and fibroglandular tissue volume mea-
volumetric measurement. AJR 2017; 209:703–708 Cancer Res 2017; 19:29 surements in serial mammograms. Acta Radiol
16. Alikhassi A, Gourabi HE, Baikpour M. Com- 29. Keller BM, Chen J, Daye D, Conant EF, Kontos 2014; 55:32–38
parison of inter- and intra-observer variability of D. Preliminary evaluation of the publicly avail- 42. Destounis S, Johnston L, Highnam R, Arieno A,
breast density assessments using the fourth and able Laboratory for Breast Radiodensity Assess- Morgan R, Chan A. Using volumetric breast den-
fifth editions of Breast Imaging Reporting and ment (LIBRA) software tool: comparison of ful- sity to quantify the potential masking risk of
Data System. Eur J Radiol Open 2018; 5:67–72 ly automated area and volumetric density mammographic density. AJR 2017; 208:222–227
17. Irshad A, Leddy R, Lewis M, et al. Changes in measures in a case-control study with digital 43. Eom HJ, Cha JH, Kang JW, Choi WJ, Kim HJ,
breast density reporting patterns of radiologists mammography. Breast Cancer Res 2015; 17:117 Go E. Comparison of variability in breast density
after publication of the 5th edition BI-RADS 30. iCad website. Powerlook Density Assessment. assessment by BI-RADS category according to
guidelines: a single institution experience. AJR www.icadmed.com/assets/dmm211_powerlook_ the level of experience. Acta Radiol 2018;
2017; 209:943–948 density_assessment_revg.pdf. Accessed October 59:527–532
18. Lee CH, Destounis SV, Friedewald SM, Newell 22, 2019 44. Ren BR, Smith A, Jing ZX. Measurement of
MS. Digital breast tomosynthesis (DBT) guid- 31. Tagliafico A, Tagliafico G, Astengo D, Airaldi S, breast density with digital breast tomosynthesis.
ance (a supplement to ACR BI-RADS Mammog- Calabrese M, Houssami N. Comparative estima- In: Pelc NJ, Nishikawa RM, Whiting BR, eds.
raphy 2013). Reston, VA: American College of tion of percentage breast tissue density for digital Medical imaging: physics of medical imaging—
Radiology, 2013 mammography, digital breast tomosynthesis, and proceedings of SPIE, vol. 8313. Bellingham, WA:
19. Zuckerman SP, Conant EF, Keller BM, et al. Imple- magnetic resonance imaging. Breast Cancer Res SPIE, 2012:83134Q
mentation of synthesized two-dimensional mam- Treat 2013; 138:311–317 45. Ekpo EU, McEntee MF. Measurement of breast
mography in a population-based digital breast to- 32. Tagliafico A, Tagliafico G, Astengo D, et al. density with digital breast tomosynthesis: a sys-
mosynthesis screening program. R adiology 2016; Mammographic density estimation: one-to-one tematic review. Br J Radiol 2014; 87:20140460
281:730–736 comparison of digital mammography and digital 46. Lehman CD, Yala A, Schuster T, et al. Mammo-
20. Aujero MP, Gavenonis SC, Benjamin R, Zhang breast tomosynthesis using fully automated soft- graphic breast density assessment using deep
Z, Holt JS. Clinical performance of synthesized ware. Eur Radiol 2012; 22:1265–1270 learning: clinical implementation. Radiology
two-dimensional mammography combined with 33. Couwenberg AM, Verkooijen HM, Li J, et al. As- 2019; 290:52–58
tomosynthesis in a large screening population. sessment of a fully automated, high-throughput 47. Wu N, Geras KJ, Shen Y, et al. Breast density
Radiology 2017; 283:70–76 mammographic density measurement tool for classification with deep convolutional neural net-
21. Gastounioti A, McCarthy AM, Pantalone L, use with processed digital mammograms. Can- works. arXiv website. arxiv.org/pdf/1711.03674.
Synnestvedt M, Kontos D, Conant EF. Effect of cer Causes Control 2014; 25:1037–1043 Published November 10, 2017. Accessed October
mammographic screening modality on breast 34. Bakic PR, Carton AK, Kontos D, Zhang C, 23, 2019
density assessment: digital mammography ver- Troxel AB, Maidment AD. Breast percent densi- 48. Kallenberg M, Petersen K, Nielsen M, et al. Unsu-
sus digital breast tomosynthesis. Radiology ty: estimation on digital mammograms and cen- pervised deep learning applied to breast density
2019; 291:320–327 tral tomosynthesis projections. Radiology 2009; segmentation and mammographic risk scoring.
22. Conant EF, Sprague BL, Kontos D. Beyond 252:40–49 IEEE Trans Med Imaging 2016; 35:1322–1331
BI-RADS density: a call for quantification in the 35. Yaffe MJ. Mammographic density: measurement 49. Mohamed AA, Berg WA, Peng H, Luo Y,
breast imaging clinic. Radiology 2018; 286:401– of mammographic density. Breast Cancer Res Jankowitz RC, Wu S. A deep learning method for
404 2008; 10:209 classifying mammographic breast density cate-
23. Destounis S, Arieno A, Morgan R, Roberts C, Chan 36. Oliver A, Tortajada M, Lladó X, et al. Breast den- gories. Med Phys 2018; 45:314–321
A. Qualitative versus quantitative mammographic sity analysis using an automatic density segmenta- 50. Puliti D, Zappa M, Giorgi Rossi P, et al.;
breast density assessment: applications for the US tion algorithm. J Digit Imaging 2015; 28:604–612 DENSITY Working Group. Volumetric breast
and abroad. Diagnostics (Basel) 2017; 7:E30 37. Highnam R, Brady M, Yaffe MJ, Karssemeijer N, density and risk of advanced cancers after a neg-
24. Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe Harvey J. Robust breast composition measurement: ative screening episode: a cohort study. Breast
MJ. The quantitative analysis of mammographic Volpara. In: Martí J, Oliver A, Freixenet J, Martí R, Cancer Res 2018; 20:95
densities. Phys Med Biol 1994; 39:1629–1638 eds. Proceedings of the Digital Mammography: 51. Astley SM, Harkness EF, Sergeant JC, et al. A
25. Ursin G, Astrahan MA, Salane M, et al. The detec- 10th International Workshop—IWDM 2010. Ber- comparison of five methods of measuring mam-
tion of changes in mammographic densities. lin/Heidelberg, Germany: Springer, 2010:342–349 mographic density: a case-control study. Breast
Cancer Epidemiol Biomarkers Prev 1998; 7:43–47 38. [No authors listed]. Understanding Quantra 2.0: Cancer Res 2018; 20:10
AJR:214, February 2020 303
Destounis et al.
52. Kuchenbaecker KB, Hopper JL, Barnes DR, et sity. J Natl Cancer Inst 2006; 98:1215–1226 antiago-Rivas M, Jandorf L. Physician knowledge,
S
al.; BRCA1 and BRCA2 Cohort Consortium. 66. Tice JA, Cummings SR, Ziv E, Kerlikowske K. attitudes, and practices regarding breast density.
Risks of breast, ovarian, and contralateral breast Mammographic breast density and the Gail mod- J Womens Health (Larchmt) 2019; 28:1193–1199
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
cancer for BRCA1 and BRCA2 mutation carriers. el for breast cancer risk prediction in a screening 80. Aminololama-Shakeri S, Soo MS, Grimm LJ,
JAMA 2017; 317:2402–2416 population. Breast Cancer Res Treat 2005; Destounis S. Screening guidelines and supple-
53. Costantino JP, Gail MH, Pee D, et al. Validation 94:115–122 mental screening tools: assessment of the ade-
studies for models projecting the risk of invasive 67. Yala A, Lehman C, Schuster T, Portnoi T, quacy of patient-provider discussions. J Breast
and total breast cancer incidence. J Natl Cancer Barzilay R. A deep learning mammography-
Imaging 2019; 1:109–114
Inst 1999; 91:1541–1548 based model for improved breast cancer risk pre- 81. Irshad A, Leddy R, Ackerman S, et al. Effects of
54. Tan MH, Mester JL, Ngeow J, Rybicki LA, diction. Radiology 2019; 292:60–66 changes in BI-RADS density assessment guide-
Orloff MS, Eng C. Lifetime cancer risks in indi- 68. Portnoi T, Yala A, Schuster T, et al. Deep learn- lines (fourth versus fifth edition) on breast den-
viduals with germline PTEN mutations. Clin ing model to assess cancer risk on the basis of a sity assessment: intra- and interreader agree-
Cancer Res 2012; 18:400–407 breast MR image alone. AJR 2019; 213:227–233 ments and density distribution. AJR 2016;
55. Wood ME, Farina NH, Ahern TP, et al. Towards 69. Kurian AW, Griffith KA, Hamilton AS, et al. Ge- 207:1366–1371
a more precise and individualized assessment of netic testing and counseling among patients with 82. Youk JH, Gweon HM, Son EJ, Kim JA. Auto-
breast cancer risk. Aging (Albany NY) 2019; newly diagnosed breast cancer. JAMA 2017; mated volumetric breast density measurements
11:1305–1316 317:531–534 in the era of the BI-RADS fifth edition: a com-
56. Bray F, Ferlay J, Soerjomataram I, Siegel RL, 70. Mammography Quality Standards Act: proposed parison with visual assessment. AJR 2016;
Torre LA, Jemal A. Global cancer statistics 2018: rule. Fed Regist 2019; 84:11669–11686 206:1056–1062
GLOBOCAN estimates of incidence and mortal- 71. Pacsi-Sepulveda AL, Shelton RC, Rodriguez CB, 83. Tabár L, Vitak B, Chen TH, et al. Swedish two-
ity worldwide for 36 cancers in 185 countries. CA Coq AT, Tehranifar P. “You probably can’t feel as county trial: impact of mammographic screening
Cancer J Clin 2018; 68:394–424 safe as normal women”: Hispanic women’s reac- on breast cancer mortality during 3 decades.
57. Claus EB, Risch N, Thompson WD. Autosomal tions to breast density notification. Cancer 2019; Radiology 2011; 260:658–663
dominant inheritance of early-onset breast can- 125:2049–2056 84. Oeffinger KC, Fontham ETH, Etzioni R, et al.
cer: implications for risk prediction. Cancer 72. Miles RC, Lehman C, Warner E, Tuttle A, Saksena Breast cancer screening for women at average
1994; 73:643–651 M. Patient-reported breast density awareness and risk: 2015 guideline update from the American
58. Tyrer J, Duffy SW, Cuzick J. A breast cancer pre- knowledge after breast density legislation passage. Cancer Society. JAMA 2015; 314:1599–1614
diction model incorporating familial and per- Acad Radiol 2019; 26:726–731 85. Mainiero MB, Moy L, Baron P, et al. American
sonal risk factors. Stat Med 2004; 23:1111–1130 73. Gunn CM, Battaglia TA, Paasche-Orlow MK, College of Radiology appropriateness criteria
59. Parmigiani G, Berry DA, Aquilar O. Determin- West AK, Kressin NR. Women’s perceptions of breast cancer screening. American College of
ing carrier probabilities for breast cancer suscep- dense breast notifications in a Massachusetts Radiology website. acsearch.acr.org/docs/70910/
tibility genes BRCA1 and BRCA2. Am J Hum safety net hospital: “So what is that supposed to Narrative/. Revised 2017. Accessed June 28, 2019
Genet 1998; 62:145–148 mean?” Patient Educ Couns 2018; 101:1123–1129 86. Liao GJ, Hippe DS, Chen LE, et al. Physician or-
60. Michailidou K, Lindstrom S, Dennis J, et al. As- 74. Haas JS, Giess CS, Harris KA, et al. Randomized dering of screening ultrasound: national rates
sociation analysis identifies 65 new breast cancer trial of personalized breast density and breast and association with state-level breast density
risk loci. Nature 2017; 551:92–94 cancer risk notification. J Gen Intern Med 2019; reporting laws. J Am Coll Radiol 2019 Jul 18
61. Lilyquist J, Ruddy KJ, Vachon CM, Couch FJ. 34:591–597 [Epub ahead of print]
Common genetic variation and breast cancer 75. Santiago-Rivas M, Benjamin S, Andrews JZ, 87. Singer T, Lourenco AP, Baird GL, Mainiero MB.
risk: past, present, future. Cancer Epidemiol Jandorf L. Breast density awareness and knowl- Supplemental screening for women with dense
Biomarkers Prev 2018; 27:380–394 edge, and intentions for breast cancer screening breasts: what do practicing radiologists recom-
62. Rudolph A, Song M, Brook MN, et al. Joint as- in a diverse sample of women age eligible for mend? J Breast Imaging 2019; 1:32–36
sociations of a polygenic risk score and environ- mammography. J Cancer Educ 2019; 34:90–97 88. Aripoli A, Fountain K, Winblad O, et al. Supple-
mental risk factors for breast cancer in the Breast 76. Busch SH, Hoag JR, Aminawung JA, et al. As- mental screening with automated breast ultra-
Cancer Association Consortium. Int J Epidemiol sociation of state dense breast notification laws sound in women with dense breasts: comparing
2018; 47:526–536 with supplemental testing and cancer detection notification methods and screening behaviors.
63. Brentnall AR, Harkness EF, Astley SM, et al. after screening mammography. Am J Public AJR 2018; 210:[web]W22–W28
Mammographic density adds accuracy to both Health 2019; 109:762–767 89. Tagliafico AS, Mariscotti G, Valdora F, et al. A
the Tyrer-Cuzick and Gail breast cancer risk 77. Cappello NM, Richetelli D, Lee CI. The impact prospective comparative trial of adjunct screen-
models in a prospective UK screening cohort. of breast density reporting laws on women’s ing with tomosynthesis or ultrasound in women
Breast Cancer Res 2015; 17:147 awareness of density-associated risks and conver- with mammography-negative dense breasts
64. Brentnall AR, Cohn WF, Knaus WA, et al. A sations regarding supplemental screening with (ASTOUND-2). Eur J Cancer 2018; 104:39–46
case-control study to add volumetric or clinical providers. J Am Coll Radiol 2019; 16:139–146 90. Skaane P, Sebuødegård S, Bandos AI, et al. Per-
mammographic density into the Tyrer-Cuzick 78. Gunn CM, Kressin NR, Cooper K, Marturano C, formance of breast cancer screening using digital
breast cancer risk model. J Breast Imaging 2019; Freund KM, Battaglia TA. Primary care provider breast tomosynthesis: results from the prospec-
1:99–106 experience with breast density legislation in tive population-based Oslo Tomosynthesis
65. Chen J, Pee D, Ayyagari R, et al. Projecting abso- Massachusetts. J Womens Health (Larchmt) Screening Trial. Breast Cancer Res Treat 2018;
lute invasive breast cancer risk in white women 2018; 27:615–622 169:489–496
with a model that includes mammographic den- 79. Brown J, Soukas C, Lin JJ, Margolies L, 91. Conant EF, Beaber EF, Sprague BL, et al. Breast
304 AJR:214, February 2020
Breast Density, Risk Estimation, and Supplemental Screening
cancer screening using tomosynthesis in combi- vated risk of breast cancer. JAMA 2008; 108. Li Q, Hu M, Chen Z, et al. Meta-analysis: con-
nation with digital mammography compared to 299:2151–2163 trast-enhanced ultrasound versus conventional
digital mammography alone: a cohort study 100. Weigert J, Steenergen S. The Connecticut experi- ultrasound for differentiation of benign and ma-
Downloaded from www.ajronline.org by Hospital Italiano de Buenos Aires on 05/13/20 from IP address 132.174.251.183. Copyright ARRS. For personal use only; all rights reserved
within the PROSPR consortium. Breast Cancer ment: the role of ultrasound in the screening of lignant breast lesions. Ultrasound Med Biol
Res Treat 2016; 156:109–116 women with dense breasts. Breast J 2012; 2018; 44:919–929
92. Ciatto S, Houssami N, Bernardi D, et al. Integra- 18:517–522 109. Berg WA, Cosgrove DO, Dore CJ, et al. Shear-
tion of 3D digital mammography with tomosyn- 101. Hooley RJ, Greenberg KL, Stackhouse RM, et al. wave elastography improves the specificity of
thesis for population breast-cancer screening Screening US in patients with mammographi- breast US: the BE1 multinational study of 939
(STORM): a prospective comparison study. cally dense breasts: initial experience with Con- masses. Radiology 2012; 262:435–449
L ancet Oncol 2016; 14:583–589 necticut Public Act 09-41. Radiology 2012; 110. Kapetas P, Pinker-Domenig K, Woitek R, et al.
93. Caumo F, Zorzi M, Brunelli S, et al. Digital 265:59–69 Clinical application of acoustic radiation force
breast tomosynthesis with synthesized two- 102. Destounis S, Arieno A, Morgan R. Initial experi- impulse imaging with Virtual Touch IQ in breast
dimensional images versus full-field digital ence with the New York State breast density in- ultrasound: diagnostic performance and repro-
mammography for population screening: out- form law at a community-based breast cen- ducibility of a new technique. Acta Radiol 2017;
comes from the Verona screening program. Ra- ter. J Ultrasound Med 2015; 34:993–1000 58:140–147
diology 2017; 287:37–46 103. Maimone S, McDonough M. Dense breast notifi- 111. Jayaraman J, Indiran V, Kannan K, Maduraimuthu
94. Destounis SV, Morgan R, Arieno A. Screening cation and supplemental screening: a survey of P. Acoustic radiation force impulse imaging in
for dense breasts: digital breast tomosynthesis. current strategies and sentiments. Breast J 2017; benign and malignant breast lesions. C ureus
AJR 2015; 204:261–264 23:193–199 2017; 9:e1301
95. Gao Y, Babb JS, Toth HK, Moy L, Heller SK. Dig- 104. Wilczek B, Wilczek HE, Rasouliyan L, Leifland 112. Panigrahi B, Mullen L, Falomo E, et al. An ab-
ital breast tomosynthesis practice patterns follow- K. Adding 3D automated breast ultrasound to breviated protocol for high-risk screening breast
ing 2011 FDA approval: a survey of breast imaging mammography screening in women with hetero- magnetic resonance imaging: impact on perfor-
radiologists. Acad Radiol 2017; 24:947–953 geneously and extremely dense breasts: report mance metrics and BI-RADS assessment. Acad
96. Ohuchi N, Suzuki A, Sobue T, et al.; J-START In- from a hospital-based, high-volume, single-cen- Radiol 2017; 24:1132–1138
vestigator Groups. Sensitivity and specificity of ter breast cancer screening program. Eur J 113. Strahle DA, Pathak DR, Sierra A, et al. System-
mammography and adjunctive ultrasonography to Radiol 2016; 85:1554–1563 atic development of an abbreviated protocol for
screen for breast cancer in the Japan strategic anti- 105. Giger ML, Inciardi MF, Edwards A, et al. Auto- screening breast magnetic resonance imaging.
cancer randomized trial (J-START): a randomised mated breast ultrasound in breast cancer screen- Breast Cancer Res Treat 2017; 162:283–295
controlled trial. Lancet 2016; 387:341–348 ing of women with dense breasts: reader study of 114. Kuhl CK, Schrading S, Strobel K, et al. Abbrevi-
97. Destounis S, Arieno A, Morgan R. New York mammography-negative and mammography- ated breast magnetic resonance imaging (MRI):
State breast density mandate: follow-up data with positive cancers. AJR 2016; 206:1341–1350 first post-contrast subtracted images and maxi-
screening sonography. J Ultrasound Med 2017; 106. Neuschler EI, Butler R, Young CA, et al. A piv- mum-intensity projection—a novel approach to
36:2511–2517 otal study of optoacoustic imaging to diagnose breast cancer screening with MRI. J Clin Oncol
98. Vourtsis A, Kachulis A. The performance of 3D benign and malignant breast masses: a new eval- 2014; 32:2304–2310
ABUS versus HHUS in the visualisation and uation tool for radiologists. Radiology 2018; 115. Mango VL, Morris EA, David Dershaw D, et al.
BI-RADS characterisation of breast lesions in a 287:398–412 Abbreviated protocol for breast MRI: are multi-
large cohort of 1,886 women. Eur Radiol 2018; 107. Lee SC, Tchelepi H, Grant E, et al. Contrast- ple sequences needed for cancer detection? Eur J
28:592–601 enhanced ultrasound imaging of breast masses: Radiol 2015; 84:65–70
99. Berg WA, Blume JD, Cormack JB, et al. Com- adjunct tool to decrease the number of false-pos- 116. Kuhl CK. Abbreviated breast MRI for screening
bined screening with ultrasound and mammog- itive biopsy results. J Ultrasound Med 2019; women with dense breast: the EA1141 trial. Br J
raphy vs mammography alone in women at ele- 38:2259–2273 Radiol 2018; 91:20170441
AJR:214, February 2020 305
You might also like
- Atypical Breast Proliferative Lesions and Benign Breast DiseaseFrom EverandAtypical Breast Proliferative Lesions and Benign Breast DiseaseFarin AmersiNo ratings yet
- Malignant and Benign Breast Cancer Classification Using Machine Learning AlgorithmsDocument5 pagesMalignant and Benign Breast Cancer Classification Using Machine Learning AlgorithmsRohit SinghNo ratings yet
- Screening Breast Ultrasound: Past, Present, and FutureDocument7 pagesScreening Breast Ultrasound: Past, Present, and FutureAnonymous wdmpgxNo ratings yet
- Risk Factor Analysis For Capsular Contracture A.5Document9 pagesRisk Factor Analysis For Capsular Contracture A.5fregianiNo ratings yet
- TEMPLATE FOR THE REVIEW OF RELATED LITERATURE - SeveraDocument7 pagesTEMPLATE FOR THE REVIEW OF RELATED LITERATURE - SeveraSevered AppleheadNo ratings yet
- Analisis Jurnal Tentang Faktor-Faktor Yang Mempengaruhi Deteksi Dini Kanker Serviks Dengan Analia PicotDocument9 pagesAnalisis Jurnal Tentang Faktor-Faktor Yang Mempengaruhi Deteksi Dini Kanker Serviks Dengan Analia PicotVelinia WijayantiNo ratings yet
- Recommendation of Pre-Operative Screening Intervention Evaluation Nursing Intervention Manpower Resources RequiredDocument7 pagesRecommendation of Pre-Operative Screening Intervention Evaluation Nursing Intervention Manpower Resources RequiredBernice EbbiNo ratings yet
- E047687 FullDocument7 pagesE047687 FullCesar GuevaraNo ratings yet
- Triyana2017efek of CCT On Coverage and Quality of Atenalatal Care IndonesiaDocument10 pagesTriyana2017efek of CCT On Coverage and Quality of Atenalatal Care IndonesiaMuhammad dzaky AdzhanyNo ratings yet
- Understanding Breast Imaging - Breast360.org - The American Society of Breast Surgeons Foundation PDFDocument5 pagesUnderstanding Breast Imaging - Breast360.org - The American Society of Breast Surgeons Foundation PDFdivyanshu kumarNo ratings yet
- Ovarian CancerDocument10 pagesOvarian CancerdianaveebaeNo ratings yet
- Assessment of Fetal Well-Being Diagnostic Tests Sheet1Document2 pagesAssessment of Fetal Well-Being Diagnostic Tests Sheet1msbunnileeNo ratings yet
- Motherhood After Breast Cancer: Searching For La Dolce Vita - Azim Et Al., 2011Document12 pagesMotherhood After Breast Cancer: Searching For La Dolce Vita - Azim Et Al., 2011CSNo ratings yet
- The Histofy of ObstetrictDocument19 pagesThe Histofy of ObstetrictKathyNogalesNo ratings yet
- Volumetric Breast Density Measurement For Personalized Screening: Accuracy, Reproducibility, Consistency, and Agreement With Visual AssessmentDocument12 pagesVolumetric Breast Density Measurement For Personalized Screening: Accuracy, Reproducibility, Consistency, and Agreement With Visual AssessmentMax Ramires SantosNo ratings yet
- NU726 Scientific Inquiry For Evidence-Based Practice Evidence Summary ToolDocument6 pagesNU726 Scientific Inquiry For Evidence-Based Practice Evidence Summary Toolgloria olekanmaNo ratings yet
- Placenta AcretaDocument118 pagesPlacenta AcretaPaco Vega WooNo ratings yet
- Retained Placenta and Associated Risk FactorsDocument3 pagesRetained Placenta and Associated Risk Factorskenny stefanusNo ratings yet
- Hospital Variation in Mortality After Emergent.3Document9 pagesHospital Variation in Mortality After Emergent.3Roberto KlappenbachNo ratings yet
- Ovarian Masses and O-RADS - A Systematic Approach To Evaluating and Characterizing Adnexal Masses With MRIDocument12 pagesOvarian Masses and O-RADS - A Systematic Approach To Evaluating and Characterizing Adnexal Masses With MRIDanteAugustoVazquezGonzalezNo ratings yet
- Breast Cancer AwarenessDocument8 pagesBreast Cancer AwarenessThe Livingston County NewsNo ratings yet
- Nursing Care Plan For Breast Cancer NCP PDFDocument2 pagesNursing Care Plan For Breast Cancer NCP PDFMaina BarmanNo ratings yet
- Nursing Care Plan For Breast Cancer NCP PDFDocument2 pagesNursing Care Plan For Breast Cancer NCP PDFMaina Barman100% (1)
- Nursing Care Plan For Breast Cancer NCPDocument2 pagesNursing Care Plan For Breast Cancer NCPMaina BarmanNo ratings yet
- Nursing Care Plan For Breast Cancer NCPDocument2 pagesNursing Care Plan For Breast Cancer NCPEsha MeharNo ratings yet
- Diagnosing and Treating Insomnia in Adults and Older Adults: Academic HighlightsDocument8 pagesDiagnosing and Treating Insomnia in Adults and Older Adults: Academic Highlightsgiselle155204No ratings yet
- Presentation1 Poster Up NewDocument1 pagePresentation1 Poster Up Newlely puspita andriNo ratings yet
- Research ClassifiedDocument6 pagesResearch ClassifiedPatricia OrtegaNo ratings yet
- Ultrasound Assessment of Diaphragmatic DysfunctionDocument10 pagesUltrasound Assessment of Diaphragmatic DysfunctionNoon NaanNo ratings yet
- Enfermedad de PagetDocument4 pagesEnfermedad de PagetNicolás BertachiniNo ratings yet
- Ultrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Document9 pagesUltrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Сергей СадовниковNo ratings yet
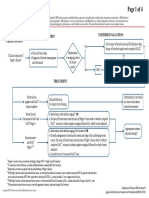
- Screening Endometrial Web AlgorithmDocument3 pagesScreening Endometrial Web AlgorithmKadir GümüşNo ratings yet
- Elastography of Breast Lesions. Initial Clinical Results.Document8 pagesElastography of Breast Lesions. Initial Clinical Results.Mercy PeñaNo ratings yet
- Materi 4 - Kanker Pada Perempuan - DR - Tofan, SP - Og (K)Document41 pagesMateri 4 - Kanker Pada Perempuan - DR - Tofan, SP - Og (K)Tuti KristantiNo ratings yet
- Tabel Analisa Jurnal KeperawatanDocument9 pagesTabel Analisa Jurnal KeperawatanbianmanNo ratings yet
- Dela Cruz, J. M3 NCPDocument2 pagesDela Cruz, J. M3 NCPNelly CruzNo ratings yet
- The Placenta Accreta Spectrum Epidemiology and Risk FactorsDocument10 pagesThe Placenta Accreta Spectrum Epidemiology and Risk FactorsYoga ParipurnaNo ratings yet
- Breast Abscess ManagementDocument10 pagesBreast Abscess Managementطلال العمريNo ratings yet
- Publication - Module - Measuring Harm in Healthcare SettingsDocument4 pagesPublication - Module - Measuring Harm in Healthcare SettingsnovizainNo ratings yet
- Beneficios y Riesgos de Esterilizacion InglésDocument14 pagesBeneficios y Riesgos de Esterilizacion InglésCecilia EstradaNo ratings yet
- Designing A Breast Abscess Pathway: A Guide For General SurgeonsDocument5 pagesDesigning A Breast Abscess Pathway: A Guide For General SurgeonsRobert ChristevenNo ratings yet
- How To Perform C-Section in Dogs - Clinician's BriefDocument13 pagesHow To Perform C-Section in Dogs - Clinician's BriefnaruenathvetmNo ratings yet
- Sahani 2013Document12 pagesSahani 2013Patricia BezneaNo ratings yet
- This Study Resource Was Shared ViaDocument5 pagesThis Study Resource Was Shared ViaMarco VillanuevaNo ratings yet
- Pub 2Document6 pagesPub 2Rudolph SunnydaysNo ratings yet
- Exercise After Breast Augmentation A Randomized.13Document7 pagesExercise After Breast Augmentation A Randomized.13CPR tyoNo ratings yet
- Episiotomía Desgarro PerinealDocument9 pagesEpisiotomía Desgarro PerinealjigagomezNo ratings yet
- 30 Gibbs - Barrow Quarterly 25-1-2013Document7 pages30 Gibbs - Barrow Quarterly 25-1-2013xcskijoeNo ratings yet
- Committee Opinion No 624 Cervical CancerDocument3 pagesCommittee Opinion No 624 Cervical CancerEliana PariNo ratings yet
- Practice Management Guidelines For The Evaluation.38Document14 pagesPractice Management Guidelines For The Evaluation.38Jaime GonzalezNo ratings yet
- Articulo BaseDocument4 pagesArticulo BaseEdison HernandezNo ratings yet
- The 2011 Infusion Nursing Standards of PracticeDocument12 pagesThe 2011 Infusion Nursing Standards of PracticeSugeng PrakosoNo ratings yet
- Fineberg 2012 Evaluation of Computed Tomography Achievement and ChallengeDocument4 pagesFineberg 2012 Evaluation of Computed Tomography Achievement and ChallengeDaniel GrigorasNo ratings yet
- Effective Feature Selection Using Multi-Objective Improved Ant Colony Optimization For Breast Cancer ClassificationDocument10 pagesEffective Feature Selection Using Multi-Objective Improved Ant Colony Optimization For Breast Cancer ClassificationAli Asghar Pourhaji KazemNo ratings yet
- Prediction of Breast Cancer Using Supervised Machine Learning TechniquesDocument5 pagesPrediction of Breast Cancer Using Supervised Machine Learning TechniquesOnoja Mary oluwafunkeNo ratings yet
- Archdischild 2019 318779Document7 pagesArchdischild 2019 318779SaifuddinNo ratings yet
- JLH and Rambo Final PosterDocument1 pageJLH and Rambo Final Posterapi-271971026No ratings yet
- Optimal Management of Sarcomas of The Breast - An UpdateDocument6 pagesOptimal Management of Sarcomas of The Breast - An UpdateZaniru Raúl Marín MartínezNo ratings yet
- Breast Cancer Risk Assessment and Screening in Average Risk WomenDocument16 pagesBreast Cancer Risk Assessment and Screening in Average Risk WomenAlejandro Abarca VargasNo ratings yet
- Damage-Control Surgery For Maternal Near-Miss Cases of Placenta Previa and Placenta Accreta SpectrumDocument6 pagesDamage-Control Surgery For Maternal Near-Miss Cases of Placenta Previa and Placenta Accreta SpectrumMuh AqwilNo ratings yet
- J Infect Public Health 2014 7 4 323-32Document10 pagesJ Infect Public Health 2014 7 4 323-32Fernando SousaNo ratings yet
- Acta Cardiol 2021 Jul 26 Masson WDocument8 pagesActa Cardiol 2021 Jul 26 Masson WFernando SousaNo ratings yet
- J Infect Chemother 2014 20 12 762-7Document6 pagesJ Infect Chemother 2014 20 12 762-7Fernando SousaNo ratings yet
- J Hepatol 2022 Jan 20 Pape S Mat Compl 1Document17 pagesJ Hepatol 2022 Jan 20 Pape S Mat Compl 1Fernando SousaNo ratings yet
- J Hepatol 2022 76 3 588-99 Mat Compl 2Document2 pagesJ Hepatol 2022 76 3 588-99 Mat Compl 2Fernando SousaNo ratings yet
- Calcif Tissue Int 2021 Jul 31 Warner SeDocument11 pagesCalcif Tissue Int 2021 Jul 31 Warner SeFernando SousaNo ratings yet
- Indian J Nephrol 2021 31 3 266-70Document5 pagesIndian J Nephrol 2021 31 3 266-70Fernando SousaNo ratings yet
- J Rheumatol 2021 Jun 15 Fernandez-Avila DGDocument7 pagesJ Rheumatol 2021 Jun 15 Fernandez-Avila DGFernando SousaNo ratings yet
- J Clin Rheumatol 2021 Aug 2 Fernandez-Avila DGDocument4 pagesJ Clin Rheumatol 2021 Aug 2 Fernandez-Avila DGFernando SousaNo ratings yet
- Acta Radiol 2021 Aug 3 Urrutia JDocument6 pagesActa Radiol 2021 Aug 3 Urrutia JFernando SousaNo ratings yet
- Pediatr Transplant 2021 E14105Document4 pagesPediatr Transplant 2021 E14105Fernando SousaNo ratings yet
- Arch Argent Pediatr 2021 119 4 273-8Document10 pagesArch Argent Pediatr 2021 119 4 273-8Fernando SousaNo ratings yet
- Disaster Med Public Health Prep 2021 Aug 2 Cereghini JDocument11 pagesDisaster Med Public Health Prep 2021 Aug 2 Cereghini JFernando SousaNo ratings yet
- J Shoulder Elbow Surg 2021 Aug 3 Rossi LaDocument24 pagesJ Shoulder Elbow Surg 2021 Aug 3 Rossi LaFernando SousaNo ratings yet
- Int J Biol Macromol 2021 Aug 5 Salinas DRCDocument39 pagesInt J Biol Macromol 2021 Aug 5 Salinas DRCFernando SousaNo ratings yet
- Eur J Ophthalmol 2020 May 13 Diamint DVDocument5 pagesEur J Ophthalmol 2020 May 13 Diamint DVFernando SousaNo ratings yet
- Ann Surg 2021 Aug 4 Machairas NDocument22 pagesAnn Surg 2021 Aug 4 Machairas NFernando SousaNo ratings yet
- World Neurosurg 2020 142 532Document1 pageWorld Neurosurg 2020 142 532Fernando SousaNo ratings yet
- Orthop J Sports Med 2021 9 7 23259671211013394Document6 pagesOrthop J Sports Med 2021 9 7 23259671211013394Fernando SousaNo ratings yet
- Aging Clin Exp Res 2020 May 9 Schapira MDocument8 pagesAging Clin Exp Res 2020 May 9 Schapira MFernando SousaNo ratings yet
- Hypertension 2020 76 2 333-41Document9 pagesHypertension 2020 76 2 333-41Fernando SousaNo ratings yet
- Obtaining Accurate and Calibrated Coil Models For Transcranial Magnetic Stimulation Using Magnetic Field MeasurementsDocument16 pagesObtaining Accurate and Calibrated Coil Models For Transcranial Magnetic Stimulation Using Magnetic Field MeasurementsGao MiNo ratings yet
- Effect of PEEP On Dead Space in An Experimental Model of ARDSDocument10 pagesEffect of PEEP On Dead Space in An Experimental Model of ARDSFernando SousaNo ratings yet
- Cereb Cortex 2020 30 6 3856Document1 pageCereb Cortex 2020 30 6 3856Fernando SousaNo ratings yet
- An Bras Dermatol 2020 95 4 540-2Document3 pagesAn Bras Dermatol 2020 95 4 540-2Fernando SousaNo ratings yet
- An Bras Dermatol 2020 95 4 540-2Document3 pagesAn Bras Dermatol 2020 95 4 540-2Fernando SousaNo ratings yet
- Jbjs Rev 2020 8 1 E0039Document8 pagesJbjs Rev 2020 8 1 E0039Fernando SousaNo ratings yet
- RMD Open 2020 6 1 E001097Document6 pagesRMD Open 2020 6 1 E001097Fernando SousaNo ratings yet
- J Low Genit Tract Dis 2020 24 1 62-8Document7 pagesJ Low Genit Tract Dis 2020 24 1 62-8Fernando SousaNo ratings yet
- J Low Genit Tract Dis 2020 24 1 62-8Document7 pagesJ Low Genit Tract Dis 2020 24 1 62-8Fernando SousaNo ratings yet
- Warm Mix Asphalt: "National Perspective"Document46 pagesWarm Mix Asphalt: "National Perspective"Royhan RizkyNo ratings yet
- Progress Test 3Document7 pagesProgress Test 3Mỹ Dung PntNo ratings yet
- Unit 2 Travel EnquiryDocument10 pagesUnit 2 Travel EnquiryQuân Soon Lê ChuNo ratings yet
- TechRef SoftstarterDocument11 pagesTechRef SoftstarterCesarNo ratings yet
- Fuzzy Based Techniques For Handling Missing ValuesDocument6 pagesFuzzy Based Techniques For Handling Missing ValuesFarid Ali MousaNo ratings yet
- Transmission Line4 PDFDocument46 pagesTransmission Line4 PDFRevathi PrasadNo ratings yet
- 1Document6 pages1Vignesh VickyNo ratings yet
- Human Behavior in OrganizationDocument85 pagesHuman Behavior in OrganizationNeric Ico Magleo100% (1)
- ZF SI 6hp Family Tree enDocument2 pagesZF SI 6hp Family Tree enfercho573No ratings yet
- Manipulatives/Interactive Media (Lecture B) : By: John T Franco 11 Humss-3Document25 pagesManipulatives/Interactive Media (Lecture B) : By: John T Franco 11 Humss-3tyron plandesNo ratings yet
- FAC1502 Bank Reconcilliation NotesDocument22 pagesFAC1502 Bank Reconcilliation NotesMichelle Foord0% (1)
- Business Plan: Malaysian NGV SDN BHDDocument81 pagesBusiness Plan: Malaysian NGV SDN BHDMurtaza ShaikhNo ratings yet
- 7 - 8 CSS - WK 3 Ergonomic Guidelines For Computer Workstations - Jesucrtina NimenzoDocument6 pages7 - 8 CSS - WK 3 Ergonomic Guidelines For Computer Workstations - Jesucrtina NimenzoEdelmar BenosaNo ratings yet
- Oman Vision 2040 Vision Document 8Document27 pagesOman Vision 2040 Vision Document 8Abdul Aziz AlbalushiNo ratings yet
- RESEARCH TEMPLATE 2023 1 AutoRecoveredDocument14 pagesRESEARCH TEMPLATE 2023 1 AutoRecoveredMark Lexter A. PinzonNo ratings yet
- Class 10th IMO 5 Years EbookDocument71 pagesClass 10th IMO 5 Years EbookAdarsh Agrawal100% (1)
- Tutorial EllothDocument15 pagesTutorial EllothLepota SvetaNo ratings yet
- Marathi Typing 30 WPM Passage PDF For Practice Arathi Typing 30 WPM Passage PDF For PracticeDocument1 pageMarathi Typing 30 WPM Passage PDF For Practice Arathi Typing 30 WPM Passage PDF For Practiceshankar jonwalNo ratings yet
- ACI-20 S2 Indonesia - en PDFDocument3 pagesACI-20 S2 Indonesia - en PDFOktaNo ratings yet
- List of Circulating Currencies by CountryDocument8 pagesList of Circulating Currencies by CountryVivek SinghNo ratings yet
- 6 - Designing Manufacturing Processes - Hill - Product ProfilingDocument20 pages6 - Designing Manufacturing Processes - Hill - Product ProfilingLalit S KathpaliaNo ratings yet
- AIFI Association of Indian Forgin IndustryDocument7 pagesAIFI Association of Indian Forgin IndustryDnyanesh ThorathNo ratings yet
- Metric Tables 2012Document2 pagesMetric Tables 2012ParthJainNo ratings yet
- LFT - Development Status and Perspectives: Prof. DR Michael SchemmeDocument7 pagesLFT - Development Status and Perspectives: Prof. DR Michael SchemmeabiliovieiraNo ratings yet
- Project - PPT 5 ImplementationDocument39 pagesProject - PPT 5 ImplementationBirhanu AbrhaNo ratings yet
- Casio fx-82MSDocument49 pagesCasio fx-82MSPéter GedeNo ratings yet
- Understanding Oil & Gas BusinessDocument349 pagesUnderstanding Oil & Gas Businessbala11ap459897% (31)
- Service Manual: Super Audio CD/DVD ReceiverDocument88 pagesService Manual: Super Audio CD/DVD Receiveralvhann_1No ratings yet
- A Guide To The Automation Body of Knowledge, 2nd EditionDocument8 pagesA Guide To The Automation Body of Knowledge, 2nd EditionTito Livio0% (9)
- 01 04 2018Document55 pages01 04 2018sagarNo ratings yet