100% found this document useful (1 vote)
420 views21 pagesVisual Disorders
This document provides an overview of the anatomy and physiology of the human eye and vision. It describes the external structures of the eye including the eyelids, eyelashes, conjunctiva, lacrimal apparatus and extraocular muscles. It also details the internal structures of the eyeball including the three layers, humors and refractive properties. Key elements of vision such as light refraction by the cornea and lens, accommodation, visual fields and pathways to the brain are summarized. In under 3 sentences.
Uploaded by
Jobelle AcenaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
420 views21 pagesVisual Disorders
This document provides an overview of the anatomy and physiology of the human eye and vision. It describes the external structures of the eye including the eyelids, eyelashes, conjunctiva, lacrimal apparatus and extraocular muscles. It also details the internal structures of the eyeball including the three layers, humors and refractive properties. Key elements of vision such as light refraction by the cornea and lens, accommodation, visual fields and pathways to the brain are summarized. In under 3 sentences.
Uploaded by
Jobelle AcenaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
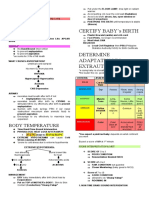
- The Eye and Vision: Introduction to the importance of vision and basic anatomy of the eye.
- Internal Structures: The Eyeball: Discussion on lacrimal glands and the internal anatomy of the eyeball.
- Pathway of Light through the Eye: Explains how light is refracted and travels through the eye to create vision.
- Application of the Nursing Process: Outlines the nursing process for eye care, including assessment and planning.
- Care of the Eyes: Information on the best practices for eye health maintenance and care.
- Planning for Health Maintenance and Restoration: Strategies for maintaining and restoring eye health, including use of medications and glasses.
- Common Related Disorders: Discusses common eye disorders such as conjunctivitis and cataracts, including their management.
- Glaucoma: Details the types of glaucoma, their symptoms, and treatment options.
- Refraction Errors of the Eyes: Covers errors in refraction such as myopia and hyperopia, detailing their impacts and corrections.
- Detachment of the Retina: Explanation on retinal detachment, its causes, and treatment approaches.
- References: References for the information contained in the document, detailing sources and contributors.