Professional Documents
Culture Documents
Anesthetic Considerations For Ambulatory Anesthesia: Advantages of Ambulatory Surgery
Uploaded by
Isabel CastilloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anesthetic Considerations For Ambulatory Anesthesia: Advantages of Ambulatory Surgery
Uploaded by
Isabel CastilloCopyright:
Available Formats
ANESTHESIOLOGY
EXIMIUS
ANESTHETIC CONSIDERATIONS FOR AMBULATORY ANESTHESIA
DR. ERWIN A. TAGUINOD, DPBA JANUARY 2020 2021
ADVANTAGES OF AMBULATORY SURGERY: Exclusion from Day Surgery
1. Greater control over scheduling Age and medical exclusions:
2. Greater privacy and convenience o ex-preterm infant < 60 weeks of post-conceptual age
1
3. Increased efficiency and consistency in nursing staff and support o Inadequately controlled systemic disease (e.g. epilepsy, asthma)
personnel o Active viral or bacterial infection (esp. respiratory)
4. Decreased cost to the patient o Complex congenital heart disease
o Cardiac murmur that has not been investigated
Most surgical procedures are performed in: o Poorly controlled diabetes mellitus
a. In-hospital procedures as outpatient o Sickle cell disease
b. Hospital-based ambulatory surgery centers Surgical and anaesthetic exclusions:
c. Free-standing ambulatory centers o Inexperienced surgeon or anaesthetist
d. Office-based surgery facilities o Prolonged procedure (>1 hour)
o Significant risk of excessive preoperative haemorrhage
Examples of advanced procedures successfully carried out in ambulatory o Opening a body cavity
settings: o Difficult airway
• Laparoscopic major gastric surgery: cholecystectomy, o Sleep apnoea
fundoplication, gastric banding, gastric sleeve o Malignant hyperthermia susceptibility
• Laparoscopic major gynecologic surgery: hysterectomy o Unlikely relief of pain by oral analgesia after discharged home
• Minimally invasive low back surgery Social exclusions
• Breast surgery
o Parents incapable or reluctant to care for child at home
• Bladder/prostate cancer surgery
o Unsupported single parent with other children
• Cruciate ligament repair o Inadequate housing conditions
• Major plastic surgery: breast reduction, abdominal fat reduction
o No telephone
• Thyroidectomy o Inadequate post operative transport
• Tonsillectomy o Arrangements (public transport unacceptable)
o Long journey (> 1 hour)
The anesthesiologiost, before delivery of anesthesia care is responsible
for: Patient inappropriate for outpatient surgery:
1. Reviewing the available medical record
Pediatric:
2. Interviewing and performing a focused examination of the
a. Formerly premature infants of less than 50 weeks post-
patient to discuss and assess
conceptual age
3. Ordering and reviewing pertinent available tests and
b. Infants with respiratory disease
consultation necessary
c. Infants with cardiovascular diseases
4. Ordering appropriate preop meds
d. Children with fever, cough, sore throat, onset of worsening urti
5. Ensuring that consent has been obtained
Adult:
6. Documenting in the chart that the above has been performed
a. Patients expected to have major blood loss
Approaches to screening patients: b. ASA III or IV patients whose systemic disease is unstable or
1. Facility visit prior to the day of surgery requires monitoring
2. Office visit prior to the day of surgery c. Morbily obese patients
3. Telephone interview/no visit d. Patients with a need for complex pain management
4. Review of health survey/no visit e. Patients with fever, wheezing, nasal congestion, coughing, urti
5. Preoperative screening and visit on the morning of surgery
6. Computer-assisted information gathering Independent risk factors for cardiac complications:
7. The use of telemedicine technology • High-risk surgery
8. Nurse-assisted interview • History of ischemic heart disease
• History of congestive heart failure
The goal to determine who is fit for outpatient surgery, then optimize • History of cerebrovascular disease
these patients. • Preoperative treatment with insulin
• Preoperative serum creatinine >2.0 mg/dL
Depends on the type of facility, patient population, procedure to be
done. Practical Screening Tool
• Poor exercise tolerance (<4 metabolic equivalents or METS) is an
Selection criteria will differ for the type of ambulatory unit involved. independent predictor of serious perioperative complications.
*Laboratory examinations should be obtained for medical indications • The likelihood of serious complications is inversely related to the
only number of blocks walked or flight of stairs climbed
*“Routine” testing of no value Independent predictors of adverse cardiac events:
*Information gained from a thorough history and PE and clear • age above 68 years
communication with perioperative team is of considerable benefit • Active congestive heart failure
• BMI >/= 30 kg/m3
Contributory factors in preventable adverse events: • Emergency surgery
• Poor airway assessment • Previous cardiac intervention
• Communication problems • Cerebrovascular disease
• Inadequate preoperative evaluation • Operative duration >3.8 hours
• Administration of one or more units of PRBCs
TRANSCRIBERS Marky, Josh, Reima EDITOR
1 of 4
ANESTHETIC CONSIDERATIONS FOR AMBULATORY ANESTHESIA EXIMIUS
2021
0000
Key points: (AHA/ACC guidelines) Pulmonary disease
• Ambulatory procedures are considered low risk with reported Focus on:
cardiac mortality of <1% o Need for home oxygen
• In the absence of “active cardiac conditions” interventions o Use of inhalers (incl rescue meds)
based on cardiovascular testing in patients would rarely result in o Ability to walk up to 2 flights of stairs
a change in management and it would be appropriate to o Frequency of coughing and secretions
proceed with planned surgery Useful tests:
o Preoperative x-ray
Difficult airway o ABG
• Depends on available resources including advanced airway o Spirometry incl vital capacity & FEVI
equipment Vital capacity of less than 1.5-2 meters or an adult FEVI of less than 1-1.5
• Access to personnel with experience dealing with difficult liters indicates increased likelihood of the need for ventilator support and
airways inpatient conversion postop
• Ensure adequate NPO
• Ascertain potential difficult airway Smoking
• Increases risk of perioperative complications
Cardiovascular disease
o Pneumonia
• Routine cardiac testing is not recommended
o Unplanned intubation
• Exceptions: decompensated or new onset heart failure, unstable o Mechanical ventilation
or severe angina, a recent MI (within 60 days), symptomatic
o Cardiac arrest
arrhythmias and severe aortic or mitral stenosis
o MI
o Stroke
Ischemic heart disease
o Sepsis
• The function of ventricles and portion of the myocardium at risk o Infection
predict a further cardiac event, not the age of the infarction
o Septic shock
• Delay atleast 60 days
• Aspirin, statin, beta-blocker
Obstructive sleep apnea
Associated with:
Coronary Intervention
o Increased age, obesity, and presence of redundant pharyngeal
• Recommendation to delay surgery
tissues
• Angioplasty: two weeks
o Snoring, episodes of apnea, tiredness despite normal night’s
• BMS: 4-6 weeks
sleep
• DES: 12 months
• CABG: 4 weeks
Approaches to managing patients with OSA in an ambulatory setting
• Access to CPAP after discharge and optimized comorbidities à
Arrhythmias
proceed with ambulatory surgery with CPAP in the
• Rule out of MI, ischemia, drug toxicity, or metabolic causes
postoperative period
• Further evaluation needed for AV block, atrial fibrillation with
• Unable or unwilling to use CPAP after discharge à proceed with
rapid ventricular response, new onset symptomatic bradycardia,
ambulatory surgery if postoperative pain relief provided without
newly recognized ventricular tachycardia
opioids
• Risk of stopping or continuing anticoangulants considered
• If patient comorbidities not optimized à not suitable for
individually
ambulatory surgery
• Upper airway surgery à per surgeon’s and anaesthesiology's
ICDs/Pacemakers
discretions
• Discuss with patient’s cardiologist a perioperative plans
• Consider placing defibrillator pads
OSA (ASA guidelines)
• Minimize surgical electrocoagulation
• Not discharged from the recovery area to an unmonitored
setting until no longer at risk for postop respiratory depression
Hypertension
• Observed no longer breathing room air in an unstimulated
• Stable hypertension acceptable (resting values 180 systolic, 110
environment
diastolic)
• Newly diagnosed, high values or unstable high values need
further evaluation
• Medications should be continued (ACEi, ARBs)
Valvular abnormalities
• A preoperative echocardiogram (done within a year) needed to
evaluate the value in symptomatic or physically inactive patients
when symptoms cannot be assessed.
TRANSCRIBERSx Marky, Josh, Reima EDITOR 2 of 4
ANESTHETIC CONSIDERATIONS FOR AMBULATORY ANESTHESIA EXIMIUS
2021
0000
Postop pain analgesia
• Topical drops
• Wound infiltration
• PNBs
• Caudal blocks
• Nsaids, paracetamol
• Oral opioids
Discharge criteria
• Awake, alert, oriented, responsive
• Minimal pain
• No active bleeding
• Vital signs stable
• Minimal nausea
• No vomiting
• Can perform sustained five second head lift
• 02 saturation of 94% on room air
Obese patients
• BMI >30 and <50 without comorbidities
• Comorbidities and ASA status
Diabetes mellitus
• FBS should tested preoperatively
• Accepted value: <180 mg/dL or 10mmol/l (Association
of clinical endocrinologists, 2015)
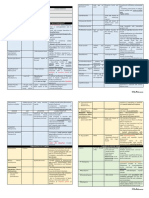
Insulin recommendations for day of surgery
INSULIN MEDICATION INSTRUCTIONS
Insulin pump Set to basal rate
Long acting, peakless insulins 75-100% morning dose
Intermediate acting insulins
(NPH) 50-75% of morning dose
Fixed combination insulins 50-75% of morning dose Home instructions:
• For the next 24 hours:
Short or rapid acting insulins Hold the dose o may feel a little sleepy
o rest at home, no strenuous activity
Pregnancy o Have a responsible adult
• Elective surgery during 1st and 3rd trimester is discouraged o May not:
• Malignancy or a condition that will deteriorate unless treated, o Drive
acceptable o Operate heavy machinery
• Ambulatory setting, if fetal monitoring is available o Make any important decisions
Breastfeeding patients Postoperative pain management:
• Breastmilk contains low levels of anesthetic agents within 24 Multimodal therapy, which combines two or more analgesics to treat
hours of GA, breastfeeding can continue unchanged postoperative pain, is often used.
• Repeated and high doses of benzodiazepines and opioids may
accumulate to dangerous levels in breastmilk, suggesting Complications and challenges of ambulatory anesthesia recovery
mothers pump and discard milk before breastfeeding • Inadequate analgesia
• Postoperative nausea and vomiting (PONV)
ESRD • Postdischarge nausea and vomiting (PDNV)
• Allowed if dialysis is done prior • Rebleeding from surgical site
• No acidosis, volume overload, electrolyte abnormalities
• Some advocate checking Potassium levels Strategies to reduce risk of PONV
• Use regional anesthesia (avoid gen. anesthesia)
• Propofol for induction and maintenance
• Avoid nitrous oxide
• Avoid volatile anesthetics
TRANSCRIBERSx Marky, Josh, Reima EDITOR 3 of 4
ANESTHETIC CONSIDERATIONS FOR AMBULATORY ANESTHESIA EXIMIUS
2021
0000
• Minimization of intraoperative and postoperative opioids
• Minimization of neostigmine
• Adequate hydration
Home instructions:
• Medications – include specific instructions and schedule of
intake
• Diet – progress slowly to regular diet; start with clear fluids
(water, gatorade)
• When to call doctor
• Names and numbers of persons to call, in case
• Additional instructions
Future Doctors, always remember:
“How much you earn does not define your worth.”
TRANSCRIBERSx Marky, Josh, Reima EDITOR 4 of 4
You might also like
- Hysterectomy, (Removal of Uterus) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHysterectomy, (Removal of Uterus) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- NCM116-LESSON3-RLE Pre-OperativeDocument6 pagesNCM116-LESSON3-RLE Pre-OperativeMilcah NuylesNo ratings yet
- Midterms ReviewDocument13 pagesMidterms ReviewGiel Margareth Lindo100% (1)
- Perioperative Nursing NotesDocument13 pagesPerioperative Nursing NotesJuliana Lourdes V. CañadaNo ratings yet
- Or NursingDocument6 pagesOr NursingMark Elben TeodoroNo ratings yet
- Day Case Anaesthesia: Andrew Green MBBS, Fracgp GP Anaesthetist ANZCA RegistrarDocument50 pagesDay Case Anaesthesia: Andrew Green MBBS, Fracgp GP Anaesthetist ANZCA RegistrarSolape Akin-WilliamsNo ratings yet
- Perioperative Care of A Pediatric Surgical PatientDocument60 pagesPerioperative Care of A Pediatric Surgical Patienthabtsh habshaNo ratings yet
- Anesthesia services for GI proceduresDocument6 pagesAnesthesia services for GI proceduresHidayati IdaNo ratings yet
- Patient Care Delivery and Safety StandardsDocument4 pagesPatient Care Delivery and Safety StandardsANDREW DEL ROSARIONo ratings yet
- Pre and Postoperative CareDocument17 pagesPre and Postoperative CaremeghanaNo ratings yet
- Day Case SurgeryDocument11 pagesDay Case SurgeryArslan Ahmed179No ratings yet
- Perioperative IIDocument10 pagesPerioperative IIshaghafalaghparyNo ratings yet
- PeriopDocument48 pagesPeriopCherry Ann Garcia Durante100% (1)
- L01 - Preoperative Anaesthetic Assessment and Premedication RevisedDocument27 pagesL01 - Preoperative Anaesthetic Assessment and Premedication RevisedReddyNo ratings yet
- Perioperative NursingDocument24 pagesPerioperative Nursingann aquino100% (1)
- 2.04 Surgical Illness in PregnancyDocument6 pages2.04 Surgical Illness in PregnancyRaquel ReyesNo ratings yet
- Pre-Op Nursing Care GuideDocument31 pagesPre-Op Nursing Care GuideZarlyn MirafloresNo ratings yet
- Care of ClientsDocument37 pagesCare of Clientsirene joy deplaNo ratings yet
- Nursing Care of Surgical ClientsDocument8 pagesNursing Care of Surgical ClientsMelchor Felipe SalvosaNo ratings yet
- 107 Rle Virtual Duty - Opd: Internal MedicineDocument6 pages107 Rle Virtual Duty - Opd: Internal MedicineGiel Margareth LindoNo ratings yet
- Medical Surgical ReviewerDocument9 pagesMedical Surgical ReviewerMary Ann Sambo OgoyNo ratings yet
- Medical Surgical 1Document16 pagesMedical Surgical 1stephaniecaronan15No ratings yet
- Valoración PreanestesicaDocument5 pagesValoración PreanestesicaSebastian Hdez BolañosNo ratings yet
- 235 Fall2020 U8 Surgery Obstetrics VOCDocument37 pages235 Fall2020 U8 Surgery Obstetrics VOCHuỳnh Tiến KhoaNo ratings yet
- Perioperative NursingDocument13 pagesPerioperative NursingLeah MalateNo ratings yet
- Pre and Post Operative ManagementDocument3 pagesPre and Post Operative Managementdrsb54No ratings yet
- Surgery RobaDocument26 pagesSurgery Robaroba shukreNo ratings yet
- Perioperative Concepts and Nursing Management: NCM 112-LecturerDocument98 pagesPerioperative Concepts and Nursing Management: NCM 112-LecturerJaylord Verazon100% (1)
- Hip Fracture Pathway First Ed 2022Document18 pagesHip Fracture Pathway First Ed 2022SabaruddinAbdullahNo ratings yet
- Peri Operative NursingDocument22 pagesPeri Operative NursingIvyBanez100% (1)
- Med Surg 1Document26 pagesMed Surg 1RogerQuxNo ratings yet
- Care of Preoperative Patients 1 3 .Docx-1Document4 pagesCare of Preoperative Patients 1 3 .Docx-1mark OrpillaNo ratings yet
- Perioperative NursingDocument41 pagesPerioperative Nursingbajaoc100% (8)
- Case 2 (Pgma-Rocklet-Wena-Manay-Chuchi-Pocha-Jb)Document5 pagesCase 2 (Pgma-Rocklet-Wena-Manay-Chuchi-Pocha-Jb)api-3743483No ratings yet
- Standard Treatment Guidelines General Surgery: Ministry of Health & Family Welfare Govt. of IndiaDocument73 pagesStandard Treatment Guidelines General Surgery: Ministry of Health & Family Welfare Govt. of IndiaiuytrerNo ratings yet
- Perioperative Nursing PhasesDocument9 pagesPerioperative Nursing Phases11 - JEMELYN LOTERTE100% (1)
- 11-SurgeriesDocument11 pages11-SurgeriesJanely EstreraNo ratings yet
- PERILIGHT EXPOSUREperinealcare Enema PDFDocument7 pagesPERILIGHT EXPOSUREperinealcare Enema PDFDanna Uy100% (1)
- Guidelines For Pneumatic Dilatation For AchalasiaDocument1 pageGuidelines For Pneumatic Dilatation For AchalasiaBenni Andica SuryaNo ratings yet
- Perioperative Nursing PhaseDocument80 pagesPerioperative Nursing PhaseMary Ann Sambo OgoyNo ratings yet
- Perioperative Pre-Class Mini-Lecture - CH 17-19Document22 pagesPerioperative Pre-Class Mini-Lecture - CH 17-19Marcel YoungNo ratings yet
- Peri Pre Intra Post ReviewerDocument12 pagesPeri Pre Intra Post ReviewerZen Kenneth DaudNo ratings yet
- Secondary PPH diagnosis and managementDocument3 pagesSecondary PPH diagnosis and managementYwagar YwagarNo ratings yet
- Pre - OperativeDocument11 pagesPre - OperativeVelpulakavyasree SonuNo ratings yet
- Perio-Op CfuDocument3 pagesPerio-Op CfuHoney Lyn AlebioNo ratings yet
- Week 1 2 Perioperative Nursing PDFDocument171 pagesWeek 1 2 Perioperative Nursing PDFGiselle EstoquiaNo ratings yet
- Perioperative Nursing Concept PDFDocument21 pagesPerioperative Nursing Concept PDFMari Fe100% (1)
- Day Care Dental Anesthesia for Minor ProceduresDocument20 pagesDay Care Dental Anesthesia for Minor Proceduresramanrajesh83No ratings yet
- Msn-Pain - SurgeryDocument45 pagesMsn-Pain - SurgeryweissNo ratings yet
- Medical Surgical Nursing Module 12Document45 pagesMedical Surgical Nursing Module 12weissNo ratings yet
- Perioperative Nursing Phases and ResponsibilitiesDocument12 pagesPerioperative Nursing Phases and ResponsibilitiesIrish Jane Gallo100% (11)
- Perioperative Nursing ManagementDocument14 pagesPerioperative Nursing ManagementMelody B. MiguelNo ratings yet
- Emilio Aguinaldo CollegeDocument8 pagesEmilio Aguinaldo CollegeKatrina Mae MedinaNo ratings yet
- ANTI-REMOVAL-1Document6 pagesANTI-REMOVAL-1Jade CentinoNo ratings yet
- Perioperative Nursing: Prepared By: Annabeth K. Salonga RN, MANDocument67 pagesPerioperative Nursing: Prepared By: Annabeth K. Salonga RN, MANAnnabeth Kwong Salonga100% (2)
- CPC Interventional RadiologyDocument138 pagesCPC Interventional RadiologyEbrahim Adel Ali AhmedNo ratings yet
- Perioperative NursingDocument27 pagesPerioperative NursingJohn Anthony de GùzmanNo ratings yet
- Preoperative Nursing Care ExplainedDocument3 pagesPreoperative Nursing Care ExplainedJmarie Brillantes PopiocoNo ratings yet
- Female Repro PhysiologyDocument18 pagesFemale Repro PhysiologyEmi LestariNo ratings yet
- SURGICAL PATHOLOGY SOFT TISSUES TableDocument4 pagesSURGICAL PATHOLOGY SOFT TISSUES TableIsabel CastilloNo ratings yet
- Surgical Pathology - Peripheral NervesDocument1 pageSurgical Pathology - Peripheral NervesIsabel CastilloNo ratings yet
- Ok Ok Notes PediaDocument10 pagesOk Ok Notes PediaIsabel CastilloNo ratings yet
- Doctor's Guide to PrescriptionsDocument54 pagesDoctor's Guide to PrescriptionsNo Longer HumanNo ratings yet
- CNS Tumors - Types, Grades and Key Imaging FeaturesDocument2 pagesCNS Tumors - Types, Grades and Key Imaging FeaturesIsabel CastilloNo ratings yet
- Surgical Pathology - Bones and JointsDocument2 pagesSurgical Pathology - Bones and JointsIsabel CastilloNo ratings yet
- DERMATOLOGY - Cuteneous Candidiasis, PityrosporumDocument4 pagesDERMATOLOGY - Cuteneous Candidiasis, PityrosporumIsabel CastilloNo ratings yet
- Dermatology - Exanthematous Viral DiseasesDocument6 pagesDermatology - Exanthematous Viral DiseasesIsabel CastilloNo ratings yet
- Surgical Pathology - Major and Minor Salivary GlandsDocument2 pagesSurgical Pathology - Major and Minor Salivary GlandsIsabel CastilloNo ratings yet
- DERMATOLOGY - Sexually Transmitted DiseaseDocument6 pagesDERMATOLOGY - Sexually Transmitted DiseaseIsabel CastilloNo ratings yet
- TemperamentsDocument2 pagesTemperamentsIsabel CastilloNo ratings yet
- Dermatology - Skin NeoplasmsDocument12 pagesDermatology - Skin NeoplasmsIsabel CastilloNo ratings yet
- Implantation and Placental DevelopmentDocument62 pagesImplantation and Placental DevelopmentIsabel CastilloNo ratings yet
- Child Growth and DevelopmentDocument60 pagesChild Growth and DevelopmentIsabel CastilloNo ratings yet
- Embryo and Fetal DevelopmentDocument50 pagesEmbryo and Fetal DevelopmentIsabel CastilloNo ratings yet
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- Pneumonia Diagnosis and TreatmentDocument6 pagesPneumonia Diagnosis and TreatmentIsabel CastilloNo ratings yet
- Genetic Basis of Congenital DisordersDocument87 pagesGenetic Basis of Congenital DisordersIsabel CastilloNo ratings yet
- Newborn Diseases Pediatrics IIDocument17 pagesNewborn Diseases Pediatrics IIIsabel CastilloNo ratings yet
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- PEDIATRIC CHAIN OF SURVIVALDocument10 pagesPEDIATRIC CHAIN OF SURVIVALIsabel CastilloNo ratings yet
- Inflammatory Bowel Disease: Microorganisms That Drive DiseaseDocument4 pagesInflammatory Bowel Disease: Microorganisms That Drive DiseaseIsabel CastilloNo ratings yet
- Pedia Pre School NewsDocument3 pagesPedia Pre School NewsIsabel CastilloNo ratings yet
- Irritable Bowel SyndromeDocument3 pagesIrritable Bowel SyndromeIsabel CastilloNo ratings yet
- Interatitial Lung DiseaseDocument2 pagesInteratitial Lung DiseaseIsabel CastilloNo ratings yet
- Adolescent Medicine: Early AdolescenceDocument2 pagesAdolescent Medicine: Early AdolescenceIsabel CastilloNo ratings yet
- Pediatric Therapeutics: Eximius 2021Document13 pagesPediatric Therapeutics: Eximius 2021Isabel CastilloNo ratings yet
- Acute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankDocument4 pagesAcute Appendicitis and Peritonitis: RLQ, To The Pelvis, Right FlankIsabel CastilloNo ratings yet
- Acute and Chronic PancreatitisDocument8 pagesAcute and Chronic PancreatitisIsabel CastilloNo ratings yet
- Pack-Years of Cigarette Smoking Is The Most HighlyDocument5 pagesPack-Years of Cigarette Smoking Is The Most HighlyIsabel CastilloNo ratings yet
- PC and NPC Creation Tables PDFDocument7 pagesPC and NPC Creation Tables PDFAut80% (5)
- High quality blood agar production with MEDIAJET and DOSE ITDocument2 pagesHigh quality blood agar production with MEDIAJET and DOSE ITBenjamin TantiansuNo ratings yet
- Medical Terminology A Short Course 7th Edition Chabner Test BankDocument25 pagesMedical Terminology A Short Course 7th Edition Chabner Test BankKatherineMooretfqm100% (52)
- Heart Disease in Pregnancy FinalDocument24 pagesHeart Disease in Pregnancy FinalBhawna JoshiNo ratings yet
- The Transgender Community Living in District Kamber Shahdadkot SindhDocument7 pagesThe Transgender Community Living in District Kamber Shahdadkot SindhnhussainmagsiNo ratings yet
- Tuberculosis QsenDocument22 pagesTuberculosis Qsenapi-534410130No ratings yet
- 19 Amazing Benefits of Fennel SeedsDocument9 pages19 Amazing Benefits of Fennel SeedsnasimNo ratings yet
- Seery, Marilyn R.: Patient ReportDocument2 pagesSeery, Marilyn R.: Patient ReportMarilyn SeeryNo ratings yet
- Arogya Sanjeevani Policy, Star Health and Allied Insurance Co LTDDocument9 pagesArogya Sanjeevani Policy, Star Health and Allied Insurance Co LTDMANTUNo ratings yet
- Gestational Diabetes Mellitus - : One Disease Two Lives at StakeDocument31 pagesGestational Diabetes Mellitus - : One Disease Two Lives at StakeSadia YousafNo ratings yet
- Literature ReviewDocument8 pagesLiterature Reviewapi-584358270No ratings yet
- Disease Prediction Using Machine Learning Algorithms2020 PDFDocument7 pagesDisease Prediction Using Machine Learning Algorithms2020 PDFSumati BaralNo ratings yet
- FSRH Ukmec Summary September 2019Document11 pagesFSRH Ukmec Summary September 2019Kiran JayaprakashNo ratings yet
- 10) One Word That Can Save Your LifeDocument4 pages10) One Word That Can Save Your LifeParesh PathakNo ratings yet
- Case Presentation On: TB Meningitis and Hepatitis B, HTNDocument26 pagesCase Presentation On: TB Meningitis and Hepatitis B, HTNAntoNo ratings yet
- Anthropometric Measurement - Prepare The Materials NeededDocument2 pagesAnthropometric Measurement - Prepare The Materials NeededMemer-alasadNo ratings yet
- Using tokens to reduce tantrums in autistic studentsDocument6 pagesUsing tokens to reduce tantrums in autistic studentsWanHanifNo ratings yet
- Journal Polyphenols SugarcaneDocument11 pagesJournal Polyphenols SugarcaneMarkNo ratings yet
- Textual EvidenceDocument28 pagesTextual EvidenceGRECEL JOYCE M. ONGCONo ratings yet
- UntitledDocument990 pagesUntitledRodica GrecuNo ratings yet
- The Obesity FixDocument82 pagesThe Obesity Fixjbennet065No ratings yet
- Dessler15e - HRM - Ch16Document46 pagesDessler15e - HRM - Ch16mohamed gbreelNo ratings yet
- Biometry: Dr. Sanjay Kumar SarkerDocument67 pagesBiometry: Dr. Sanjay Kumar SarkerNiloy Basak100% (3)
- ESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDocument5 pagesESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDini SuhardiniNo ratings yet
- Karolinska Sleepiness Scale (KSS) ChapterDocument2 pagesKarolinska Sleepiness Scale (KSS) ChapterSrija GottiparthiNo ratings yet
- Case Presewntation - C - SectionDocument12 pagesCase Presewntation - C - Sectionpriyanka50% (2)
- Respiratory Viruses: Organisms Causing PneumoniaDocument17 pagesRespiratory Viruses: Organisms Causing PneumoniaSherree HayesNo ratings yet
- CEDA-2023-Programme Final Pentru SiteDocument24 pagesCEDA-2023-Programme Final Pentru SiteMaricela IvașcuNo ratings yet
- Diagnosis and Management of Dyslipidemia in Family PracticeDocument41 pagesDiagnosis and Management of Dyslipidemia in Family PracticeKai ChuaNo ratings yet
- A Pilot Study On Safety and Clinical Utility of A Single-Use 72-Hour Indwelling Transesophageal Echocardiography ProbeDocument7 pagesA Pilot Study On Safety and Clinical Utility of A Single-Use 72-Hour Indwelling Transesophageal Echocardiography ProbeminiypuntoNo ratings yet