Professional Documents
Culture Documents
Endometrial Uterine Cancer
Uploaded by
Shena Mae Angela SILVA0 ratings0% found this document useful (0 votes)
8 views2 pagesOriginal Title
ENDOMETRIAL UTERINE CANCER
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views2 pagesEndometrial Uterine Cancer
Uploaded by
Shena Mae Angela SILVACopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
ENDOMETRIAL (Uterine) CANCER Assessment and Diagnostic Methods
Cancer of the uterine endometrium (fundus Annual checkups and gynecologic
or corpus) is the fourth most common examination.
cancer in women. Endometrial aspiration or biopsy is
Adenocarcinoma is the most common type, performed with perimenopausal or
accounting for 80% of all cases. menopausal bleeding.
Ultrasonography.
✔ It is slow growing with initial growth in the
uterine cavity, followed by extension into the
myometrium and cervix.
Type 1, which accounts for the majority of Assessment
cases, is estrogen related and occurs in
younger, obese, and perimenopausal Obtain patient information
women. It is usually low grade and Age and ethnicity
endometrioid. Risk factors of family history of cancer
Type 2, which occurs in about 10% of History of diabetes, obesity or
cases, is high grade and usually serous hypertension
cell or clear cell. It affects older women and Childbearing status, pregnancies, births,
African American women. infertility
Type 3, which also occurs in about 10% of Prolonged estrogen use
cases, is the hereditary or genetic types,
Obtain patient information
some of which are related to the Lynch II
syndrome. Age and ethnicity
Risk factors of family history of cancer
Discussions: Lynch II syndrome. This
History of diabetes, obesity or
syndrome is associated with the occurrence of
hypertension
breast, ovarian, colon, endometrial, and other
Childbearing status, pregnancies, births,
cancers throughout a family.
infertility
Risk Factors Prolonged estrogen use
Prolonged exposure to estrogen without the Surgical Management
protective effects of progesterone.
Surgical removal and cancer staging of the
Women in reproductive years.
tumor is first-line therapy. Typically, a total
Family history of endometrial cancer or abdominal hysterectomy is done.
hereditary nonpolyposis colorectal cancer
(HNPCC) Nonsurgical Management
Diabetes mellitus > Nulliparity
Radiation therapy and chemotherapy are
Hypertension > smoking used postoperatively and depend on the
Obesity > Late menopause surgical staging.
Tamoxifen (Nolvadex) give5 n for breast When Intracavitary radiation thehrapy (IRT)
cacner (brachytherapy) is performed, an applicator
Clinical Manifestations is positioned within the uterus through the
vagina. Implement these interventions for
Irregular bleeding and postmenopausal radiation safety and to prevent dislodgment
bleeding raise suspicion of endometrial of either the applicator or the radiation
cancer. source:
Sexual partners cannot “catch” cancer
1. Maintain radiation precautions. The patient is not radioactive (after the
2. Provide bedrest, laying the patient on her intracavitary radiation source is
back, with her head flat or elevated less removed).
than 20 degrees. Restrict active movement
to prevent dislodgment.
3. Assess for complications including cystitis,
diarrhea, and mucosal or skin irritation.
Instruct the patient undergoing external
beam radiation to:
1. Observe for signs of skin breakdown.
2. Avoid sunbathing.
3. Do not remove the markings that outline
the treatment site.
4. Recognize the complications of
treatment, including cystitis, diarrhea,
and nutritional alterations.
5. Recognize the reactions to RT vary
among patients and that some may feel
unclean or radioactive after treatments.
General management issues for the care of
patients undergoing intracavitary
(brachytherapy) or external (teletherapy)
RT
Chemotherapy is used as palliative
treatment in advanced or recurrent
endometrial cancer.
1. Chemotherapuetic agents frequently used
include doxorubicin (Adriamycin), cisplatin
(Platinol), paclitaxel (Taxol).
2. General management issues for the car of
patients receiving combination
chemotherapy
Community-based Care
Provide oral and written instructions on:
Effects or complications from surgery,
radiation, or chemotherapy that should
be reported to the provider, including
vaginal bleeding, rectal bleeding, foul-
smelling discharge, abdominal pain or
distention, and hematuria
Dosages, scheduling, and side effects of
prescribed drugs
Inform the patient that:
High-dose radiation causes sterility.
Vaginal shrinkage or dryness can occur
with radiation and chemotherapy
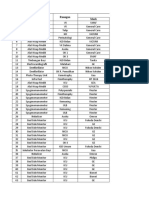
You might also like
- Family Centered CareDocument7 pagesFamily Centered CareSirisha ChelvaNo ratings yet
- PANCYTOPENIADocument51 pagesPANCYTOPENIAResmyNo ratings yet
- Micro Buzz Words - KEY WordsDocument8 pagesMicro Buzz Words - KEY WordsKris GulleyNo ratings yet
- Malignant Tumors of Uterus: DR Tahira RizwanDocument52 pagesMalignant Tumors of Uterus: DR Tahira RizwanSadia YousafNo ratings yet
- Johnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-121-140Document20 pagesJohnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-121-140toanbauNo ratings yet
- Burn Lecture NotesDocument5 pagesBurn Lecture NotesJerlyn Lopez100% (1)
- Breast CancerDocument33 pagesBreast Canceredenpearlcastillo67% (3)
- Carcinoma EndometriumDocument45 pagesCarcinoma EndometriumSapna SNo ratings yet
- Seminar On Tumour Complicating With PregnancyDocument22 pagesSeminar On Tumour Complicating With PregnancyMonika shankarNo ratings yet
- Cervical CancerDocument2 pagesCervical Cancergilpogs0% (1)
- Cervical CancerDocument36 pagesCervical CancerDebabrata SatapathyNo ratings yet
- Symptoms: Definition of Cervical Cancer: Cancer That Forms in Tissues of The Cervix (The Organ Connecting The UterusDocument5 pagesSymptoms: Definition of Cervical Cancer: Cancer That Forms in Tissues of The Cervix (The Organ Connecting The UterusHazel Joy Hokson-DiazNo ratings yet
- Endometrial Malignancies 1Document41 pagesEndometrial Malignancies 1jerrydanfordfxNo ratings yet
- Breast CancerDocument11 pagesBreast CancerRock'nRoll Buddies100% (2)
- Cervical CancerDocument28 pagesCervical CancerAmlan jyoti thanapatiNo ratings yet
- Gynaecological CancersDocument4 pagesGynaecological CancerssdfNo ratings yet
- Saso, S.Document8 pagesSaso, S.Azka Syifa AnnisaNo ratings yet
- Malignant Disease of The Body of The UterusDocument12 pagesMalignant Disease of The Body of The UterusAmmarNo ratings yet
- Endometrial CancerDocument23 pagesEndometrial CancerAlmina RehmanNo ratings yet
- Cancer of The Endometrium FinalDocument3 pagesCancer of The Endometrium FinalJoy KirumbaNo ratings yet
- CAembarazoDocument6 pagesCAembarazoMary VeraNo ratings yet
- Cancer Cervix: BY Ahmed Magdy ElmohandesDocument34 pagesCancer Cervix: BY Ahmed Magdy ElmohandesAhmed ElmohandesNo ratings yet
- Acta 90 405Document6 pagesActa 90 405Eftychia GkikaNo ratings yet
- Breast CancerDocument21 pagesBreast CancerfrankNo ratings yet
- Endometrium Cancer: DR - Supanji Raharja, Spog (K) Medical Faculty Muhammadyah University Surakarta 2018Document47 pagesEndometrium Cancer: DR - Supanji Raharja, Spog (K) Medical Faculty Muhammadyah University Surakarta 2018YoggaNo ratings yet
- Breast CancerDocument5 pagesBreast Cancerbobtaguba100% (1)
- An Are PortDocument18 pagesAn Are PortKirsten NVNo ratings yet
- Uterine Body Carcinoma - DRJDocument35 pagesUterine Body Carcinoma - DRJJyoti MishraNo ratings yet
- Ovarian and Prostate CancerDocument51 pagesOvarian and Prostate CancerMa. Angelica Alyssa RachoNo ratings yet
- Cervical Cancer: Predominately Squamous Cell CancerDocument1 pageCervical Cancer: Predominately Squamous Cell CancerAila CamachoNo ratings yet
- Endometrial Cancer: Clinical Expert SeriesDocument15 pagesEndometrial Cancer: Clinical Expert SeriesWilliam Vinicius WeberNo ratings yet
- Breast CancerDocument7 pagesBreast Cancermikhail juteNo ratings yet
- Endometrial CancerDocument16 pagesEndometrial CancerSusan Powell-ProctorNo ratings yet
- En Dome Trial Carcinoma Sobhi AboulouzDocument50 pagesEn Dome Trial Carcinoma Sobhi Aboulouzshygirl72No ratings yet
- Endometrial CarcinomaDocument6 pagesEndometrial CarcinomaĶHwola ƏľsHokryNo ratings yet
- en Dome Trial CarcinomaDocument31 pagesen Dome Trial Carcinomadr_asalehNo ratings yet
- Nursing Management of Breast Cancer: Learning OutcomesDocument12 pagesNursing Management of Breast Cancer: Learning OutcomesJanelle Cabida SupnadNo ratings yet
- Carcinoma Uterus - Amita MaheshwariDocument42 pagesCarcinoma Uterus - Amita MaheshwariMochammad Rizal AttamimiNo ratings yet
- Lynch Syndrome For The Gynaecologist, TOG-2021Document12 pagesLynch Syndrome For The Gynaecologist, TOG-2021saeed hasan saeedNo ratings yet
- Endometrial Cancer ESMO Clinical Practice GuidelinesDocument5 pagesEndometrial Cancer ESMO Clinical Practice Guidelinesjhon heriansyahNo ratings yet
- Breast Cancer ReportDocument34 pagesBreast Cancer ReportShehada Marcos BondadNo ratings yet
- Endometrial Cancer 2015Document21 pagesEndometrial Cancer 2015ErickNo ratings yet
- Reviewon Cervical CancerDocument7 pagesReviewon Cervical CancerAlmas TNo ratings yet
- Risk Factors: About Breast CancerDocument5 pagesRisk Factors: About Breast CancerShyamol Bose100% (1)
- Eng Kesper CBLDocument3 pagesEng Kesper CBLExo LNo ratings yet
- Imaging in Endometrial Carcinoma: I O: R ADocument11 pagesImaging in Endometrial Carcinoma: I O: R AЛарисаNo ratings yet
- 18-Endometrial Cancer UpdatedDocument50 pages18-Endometrial Cancer Updated03. Rajlaksmi BanikNo ratings yet
- ACOG On CA EndometriumDocument14 pagesACOG On CA EndometriumzoviNo ratings yet
- Moodule - Breast CancerDocument11 pagesMoodule - Breast CancerJanelle Cabida SupnadNo ratings yet
- 陳v Endometrial Cancer 2Document48 pages陳v Endometrial Cancer 201范芷紜No ratings yet
- Bregar 1Document7 pagesBregar 1atikha apriliaNo ratings yet
- Endometrial Cancer: Balberan, Saro D. Canabal, Kelvin Vincent Flores, MarloDocument30 pagesEndometrial Cancer: Balberan, Saro D. Canabal, Kelvin Vincent Flores, Marlomynoidanh19No ratings yet
- OBGYN Invasive Cervical Cancer ArticleDocument7 pagesOBGYN Invasive Cervical Cancer ArticleVanessa HermioneNo ratings yet
- Passarello, K.Document9 pagesPassarello, K.Azka Syifa AnnisaNo ratings yet
- Cervical CancerDocument38 pagesCervical Cancerreema.saleh123No ratings yet
- Endometrial HyperplasiaDocument12 pagesEndometrial HyperplasiaHenri KnafoNo ratings yet
- Endomaterial Cancer-1Document28 pagesEndomaterial Cancer-1A.H.ANo ratings yet
- Enometrial Hyperplasia & CADocument56 pagesEnometrial Hyperplasia & CAAddisu DawudNo ratings yet
- Guidelines For Management of Endometrial CarcinomaDocument41 pagesGuidelines For Management of Endometrial CarcinomaVeenaNo ratings yet
- Newest Breast CancerDocument27 pagesNewest Breast CancerSAMMYNo ratings yet
- Benign Proliferative Breast Disease: The Two Most Common Types AreDocument3 pagesBenign Proliferative Breast Disease: The Two Most Common Types AreYousef KhalifaNo ratings yet
- Breast Disease: Diagnosis and Pathology, Volume 1From EverandBreast Disease: Diagnosis and Pathology, Volume 1Adnan AydinerNo ratings yet
- Endometrial Cancer: A Comprehensive Resource for Patients and FamiliesFrom EverandEndometrial Cancer: A Comprehensive Resource for Patients and FamiliesNo ratings yet
- Drug Name Mechanism of Action Dosage/ Route Indication/ Contraindication Side Effects/ Adverse Reaction Nursing ResponsibilitiesDocument1 pageDrug Name Mechanism of Action Dosage/ Route Indication/ Contraindication Side Effects/ Adverse Reaction Nursing ResponsibilitiesLowell AgustinNo ratings yet
- Suture Size: SmallestDocument2 pagesSuture Size: SmallestGeraldine BirowaNo ratings yet
- Brad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Document36 pagesBrad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Cristian OrozcoNo ratings yet
- 3214Document8 pages3214hshobeyriNo ratings yet
- Concept of PreventionDocument48 pagesConcept of Preventionmahmoud100% (1)
- Protocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Document17 pagesProtocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Sara Daoudi FuentesNo ratings yet
- SHD Presentation For SIPAG Kumustahan v9 For SharingDocument75 pagesSHD Presentation For SIPAG Kumustahan v9 For Sharinganon_803348026No ratings yet
- For PrintDocument17 pagesFor Printexample mailNo ratings yet
- Drug Calculations For Nurses A Step-by-Step Approa... - (Chapter 8 Infusion Rate Calculations)Document22 pagesDrug Calculations For Nurses A Step-by-Step Approa... - (Chapter 8 Infusion Rate Calculations)HarjotBrarNo ratings yet
- Daftar Kalibrasi Alat 2020Document18 pagesDaftar Kalibrasi Alat 2020Budi SetyawanNo ratings yet
- F1000research 248187Document86 pagesF1000research 248187Ivan GeromeNo ratings yet
- Medical Prefixes and Suffixes and English Roots - 2003Document28 pagesMedical Prefixes and Suffixes and English Roots - 2003Nada SaviraNo ratings yet
- Federația Pro-Vita Ce Nu Se Spune În Discursul OficialDocument11 pagesFederația Pro-Vita Ce Nu Se Spune În Discursul OficialIoan CotarleaNo ratings yet
- Verrucous CarcinomaDocument12 pagesVerrucous Carcinomaanatomimanusia100% (1)
- 108 New Charm, CharmaidDocument3 pages108 New Charm, CharmaidAmit Kumar PandeyNo ratings yet
- Nursing Care PlansDocument4 pagesNursing Care Plansapi-19762967No ratings yet
- Pelvic Inflammatory Disease - Clinical Manifestations and DiagnosisDocument13 pagesPelvic Inflammatory Disease - Clinical Manifestations and DiagnosisJavier Manuel Escobedo CalderónNo ratings yet
- Perioprative 1Document2 pagesPerioprative 1Mar OrdanzaNo ratings yet
- Drug Study..Document4 pagesDrug Study..Micah SalesNo ratings yet
- 60 Revision MCQs For ProsDocument9 pages60 Revision MCQs For ProsUsman Ali AkbarNo ratings yet
- Ventilator Draeger Evita V300 - Spesifikasi Teknis PDFDocument4 pagesVentilator Draeger Evita V300 - Spesifikasi Teknis PDFArifyadin SudonoNo ratings yet
- Investigations For Diseases of The Tongue A Review PDFDocument6 pagesInvestigations For Diseases of The Tongue A Review PDFShantanu DixitNo ratings yet
- Pandu Anaemia An Ayurvedic Literature ReviewDocument7 pagesPandu Anaemia An Ayurvedic Literature ReviewAmith G R AnajiNo ratings yet
- ResearchDocument19 pagesResearchKeVongPugehNo ratings yet
- Antimicrobial Drug Interactionstable220716 PDFDocument4 pagesAntimicrobial Drug Interactionstable220716 PDFBhavin DesaiNo ratings yet