Professional Documents
Culture Documents
Inpatient Asthma: Clinical Pathway
Uploaded by
dedeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inpatient Asthma: Clinical Pathway
Uploaded by
dedeCopyright:
Available Formats
THIS PATHWAY
CLINICAL PATHWAY: SERVES AS A GUIDE
Inpatient Asthma
AND DOES NOT
REPLACE CLINICAL
JUDGMENT.
The following tests and treatments
Inclusion Criteria: 1 yrs old, inadequate response to ED asthma treatment (see ED Asthma Pathway)
are NOT routinely indicated for the
Exclude Criteria: < 1yr old, primary diagnosis of bronchiolitis or pneumonia, active cardiac disease
treatment of asthma:
Ipratropium bromide should
Admit to Medical/ Surgical Unit not be administered after 24
Oxygen: Titrate per order hours of hospitalization
Oral Steroid: Chest x-rays (features typically
o Prednisone or Prednisolone 1mg/kg/dose q12hr; <12 yr old:
max 60 mg/day, 12 y/o: max 80 mg/day (Start 24 hr after associated with positive chest
dexamethasone. Total steroid course: 5 days) x-ray findings include fever,
o OR give additional dose of Dexamethasone 0.6 mg/kg (max no family history of asthma,
16mg) PO/IM prior to discharge and localized lung exam
Determine initial MPIS findings)
If poor PO, place PIV and administer IVF with potassium MPIS 7-10
MPIS 11 Use asthma-specific H&P to document asthma severity and control Antibiotics (unless diagnosed
(Appendix A, Appendix B, Appendix C) with a bacterial infection)
Consider ordering medications for bedside delivery on admission
Initiate Phase 2:
Initiate Phase 1:
Albuterol MDI w/ spacer 8 puffs q2hr
Albuterol via continuous neb:
(nebulizer can be used if patient sleeping or unable to
o <20kg: 10 mg/hr
perform proper MDI technique)
o 20kg: 20 mg/hr
Initiate Albuterol Wean Protocol*
Initiate Albuterol Wean Protocol*
Assess severity and treatment recommendations, start
o Option: If improving on 20 mg/hr, wean to
Inhaled Corticosteroids (Appendix A, Appendix B,
10 mg/hr prior to going to q2hr
Appendix C, Appendix D)
If not tolerating oral steroid:
Initiate Asthma Education and home treatment plan
o Methylprednisolone 1 mg/kg/dose IV q6hr
(<12 yr old: max 60 mg/day; 12 max 80 mg/day)
Discontinue CR monitor
Vital signs q4hr, MPIS q2hr
Place PIV, if not already done
Discontinue O2 when RA sat >92%
CR monitor w/continuous pulse oximetry
Intermittent pulse ox once off O2
Vital signs q4hr, MPIS q2hr
Initiate Asthma Education
Improvement?
(MPIS 6 x2)
Improvement? No Yes
(Two consecutive scores in
appropriate range) Continue on pathway Initiate Phase 3
as MPIS dictates Albuterol MDI w/ spacer 8 puffs q4hr
(nebulizer can be used if pt sleeping or
No Yes unable to perform proper MDI technique)
Continue Inhaled Corticosteroids (Appendix
Initiate Phase 2 and follow A, Appendix B, Appendix C, Appendix D),
pathway and consider ordering medications for
MPIS 13 x 1
bedside delivery if not done
Discontinue O2 when RA sat >92%
Intermittent pulse ox once off O2
Vital signs q4hr, MPIS q4hr
Increase Albuterol to Complete Asthma Education
20 mg/hr if on 10 mg/hr Supply nebulizer or spacer, if needed
Notify attending
Obtain PICU consult
Consider Mg sulfate Discharge Criteria:
Off supplemental oxygen, MPIS 5 on q4hr albuterol, hydrated without need for IVFs,
asthma home management plan of care complete, asthma education complete and family
given copy, appropriate follow up in place
Continue on pathway
Improvement? Yes Discharge Medications (to be outlined in Asthma Action Plan)
as MPIS dictates
Albuterol MDI with spacer: 4 puffs (or 2.5mg via neb) q4hr while awake
Total oral steroid x3-5 days (prednisone/prednisolone vs 2nd dose of dexamethasone)
No Controller therapy (Appendix C, Appendix D), based on chronic severity (Appendix A,
Appendix B)
Consider transfer Screen for Flu vaccine (Oct-March); administer if indicated
to PICU
MPIS SCORING TOOL
* ALBUTEROL WEAN PROTOCOL:
RT s wean Albuterol O2 Saturation Accessory
(RA) Muscle Use I:E Ratio Wheezing Heart Rate Respiratory Rate
according to this MPIS-driven
protocol
Wean when two consecutive
Score Score Score Score <3 yr old >3 yr old Score <6 yr old >6 yr old Score
scores are in appropriate
None: Good
range
>95% 0 None 0 2:1 0 aeration 0 <120 <100 0 <30 <20 0
RT s inform MD/APRN/PA of
End
ALL changes in Albuterol 93-95% 1 Mild 1 1:1 1 expiratory 1 121-140 101-120 1 31-45 21-35 1
dosing
Any escalation in care Insp/Exp:
requires an exam by MD/ 90-92% 2 Moderate 2 1:2 2 Good aeration 2 141-160 121-140 2 46-60 36-50 2
APRN/PA at bedside Insp/Exp:
MD/APRN/PA can authorize Decreased
variance from protocol <90% 3 Severe 3 1:3 3 aeration 3 >160 >140 3 >60 >50 3
NEXT PAGE
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
LAST UPDATED: 11.11.19
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
CLINICAL PATHWAY: THIS PATHWAY
SERVES AS A GUIDE
Inpatient Asthma AND DOES NOT
Appendix A: Simplified Controller Flowchart REPLACE CLINICAL
JUDGMENT.
Assessing Asthma Severity and Treatment Recommendations: Ages 5 and Up
> 2 days/week but
Symptom Frequency 2 days/week Daily Throughout the day
NOT daily
Assess and Night time
2x/month 3-4x/month >1x/week Every Night
DOCUMENT awakenings
Asthma Control Albuterol for
2 days/week >2 days/week Daily
Several times per
for 2 Weeks Prior symptom control day
1 to Exacerbation Interfere with
None Minor Limitation Some Limitation Extremely Limited
normal activity
Exacerbations
Determine requiring systemic 0-1/year 2/year with more frequent or intense events = greater severity
severity if new steroids
diagnosis of If currently on Increase Step by 1
asthma medication & well If on meds, taking
NO appropriately*?
YES UNLESS well controlled
controlled, continue (all green answers above)
current treatment
2 Classify Asthma Worst symptom
documented above Intermittent Mild Persistent Moderate Persistent Severe Persistent
Severity determines severity
(STEP 3)
If starting tx: 1 Puff (STEP 3 or 4)
Fluti casone 110 BID
(STEP 2) If stepping up tx: 1 Puff 2 Puff Fluticasone/
(STEP 1)
5-11 Years Old 2 Puffs Fluticasone Fluti casone 110 BID + Salmeterol 115/21 BID
Albuterol PRN Montelukast
44 BID OR 2 Puffs Fl uticasone/
OR
Treatment Salmeterol 45/21 BID +/- Consult Pulmonary
3
Recommendation Montelukast
(NHLBI STEP (STEP 3)
(STEP 3 or 4)
CORRELARY) Fluticasone/
2 Puffs Fluticasone
(STEP 2) Salmeterol 115
(STEP 1) 44 BID +
12+ Years Old 2 Puffs Fluticasone mcg/21 mcg 2 Puff
Albuterol PRN Montelukast OR 2
44 BID BID vs Fluticasone
Puff Fluticasone 110
110mcg 2 Puffs BID
BID
+ Montelukast
4 Consult (PRN) Consult Pulmonology If: Patient Requires Step 5 Treatment, Or High Dose Inhaled Steroids
(2+ Puffs 110 for 5-11yo, 2+ puffs 220 for >12 year old)
*Taking Controller Medications Appropriately:
Taking medications as prescribed >80% of the time (self report, pharmacy refills)
Using correct technique (using a spacer correctly)
If insurance does not cover the recommended medication, see below for equivalent doses of inhaled steroids
Fluticasone Beclomethasone
Fluticasone/ Budesonide/ Mometasone/
Salmeterol Formoterol Formoterol Montelukast
Dosing (Flovent) (Qvar)
(Advair) (Symbicort) (Dulera)
Conversion <6 years old 4mg daily;
Chart 44 mcg 40 mcg 45/21 mcg 80/4.5 mcg 100/5 mcg 6-14 years old: 5mg daily;
>14 years old: 10mg daily
110 mcg 80 mcg 115/21 mcg 160/4.5 mcg 200/5 mcg
RETURN TO
THE BEGINNING
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
LAST UPDATED: 11.11.19
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
LAST UPDATED: 11.11.19
INITIAL VISIT: CLASSIFYING ASTHMA SEVERITY AND INITIATING THERAPY
(in patients who are not currently taking long-term control medications)
Inpatient Asthma
Level of severity (Columns 2–5) is determined by events listed in Column 1 for both impairment (frequency and intensity of symptoms and functional limitations) and risk (of
exacerbations). Assess impairment by patient’s or caregiver’s recall of events during the previous 2–4 weeks; assess risk over the last year. Recommendations for initiating therapy
based on level of severity are presented in the last row.
CLINICAL PATHWAY:
Persistent
Intermittent
Components of Mild Moderate Severe
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
Severity
Ages Ages Ages Ages Ages Ages Ages Ages Ages Ages Ages Ages
0–4 years 5–11 years ≥12 years 0–4 years 5–11 years ≥12 years 0–4 years 5–11 years ≥12 years 0–4 years 5–11 years ≥12 years
Symptoms ≤2 days/week >2 days/week but not daily Daily Throughout the day
Nighttime awakenings 0 ≤2x/month 1–2x/month 3–4x/month 3–4x/month >1x/week but not nightly >1x/week Often 7x/week
SABA use for >2 days/week but
>2 days/week
symptom control ≤2 days/week not daily and not more Daily Several times per day
but not daily
(not to prevent EIB ) than once on any day
Interference with
None Minor limitation Some limitation Extremely limited
normal activity
Appendix B: NHLBI Asthma Classification
Normal FEV1 Normal FEV1
Impairment
Lung function between between
exacerbations exacerbations
Not Not Not Not
FEV1 (% predicted) >80% >80% >80% >80% 60–80% 60–80% <60% <60%
applicable applicable applicable applicable
FEV1 /FVC >85% Normal† >80% Normal† 75–80% Reduced 5%† <75% Reduced >5%†
RETURN TO
≥2 exacerb.
THE BEGINNING
in 6 months, Generally, more frequent and intense events indicate greater severity.
or wheezing
Asthma exacerbations ≥4x per
requiring oral systemic year lasting
0–1/year ≥2/year Generally, more frequent and intense events indicate greater severity.
corticosteroids‡ >1 day
AND risk
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
Risk
factors for
persistent
asthma
Consider severity and interval since last asthma exacerbation. Frequency and severity may fluctuate over time for patients in any severity category.
Relative annual risk of exacerbations may be related to FEV1 .
Recommended Step for Step 3
Initiating Therapy Step 3
medium-dose Step 4
Step 3 medium-dose Step 3 Step 3
(See “Stepwise Approach for Step 1 Step 2 ICS option or 5
ICS option
Managing Asthma Long Term,” or Step 4
page 7)
The stepwise approach is meant Consider short course of oral systemic corticosteroids.
to help, not replace, the clinical
decisionmaking needed to meet In 2–6 weeks, depending on severity, assess level of asthma control achieved and adjust therapy as needed.
individual patient needs. For children 0–4 years old, if no clear benefit is observed in 4–6 weeks, consider adjusting therapy or alternate diagnoses.
Abbreviations: EIB, exercise-induced bronchospam; FEV1 , forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroid; SABA, short-acting beta2-agonist.
† Normal FEV1 /FVC by age: 8–19 years, 85%; 20–39 years, 80%; 40–59 years, 75%; 60–80 years, 70%.
‡ Data are insufficient to link frequencies of exacerbations with different levels of asthma severity. Generally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)
Asthma Care Quick Reference
indicate greater underlying disease severity. For treatment purposes, patients with ≥2 exacerbations may be considered to have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
5
JUDGMENT.
THIS PATHWAY
AND DOES NOT
REPLACE CLINICAL
SERVES AS A GUIDE
LAST UPDATED: 11.11.19
6
FOLLOW-UP VISITS: ASSESSING ASTHMA CONTROL AND ADJUSTING THERAPY
Inpatient Asthma
Level of control (Columns 2–4) is based on the most severe component of impairment (symptoms and functional limitations) or risk (exacerbations). Assess impairment by patient’s or caregiver’s
recall of events listed in Column 1 during the previous 2–4 weeks and by spirometry and/or peak flow measures. Symptom assessment for longer periods should reflect a global assessment,
such as inquiring whether the patient’s asthma is better or worse since the last visit. Assess risk by recall of exacerbations during the previous year and since the last visit. Recommendations for
adjusting therapy based on level of control are presented in the last row.
CLINICAL PATHWAY:
Well Controlled Not Well Controlled Very Poorly Controlled
Components of Control Ages Ages Ages Ages Ages Ages Ages Ages Ages
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
0–4 years 5–11 years ≥12 years 0–4 years 5–11 years ≥12 years 0–4 years 5–11 years ≥12 years
≤2 days/week but >2 days/week or
Symptoms ≤2 days/week not more than ≤2 days/week >2 days/week multiple times on >2 days/week Throughout the day
once on each day ≤2 days/week
Nighttime awakenings ≤1x/month ≤2x/month >1x/month ≥2x/month 1–3x/week >1x/week ≥2x/week ≥4x/week
Asthma Care Quick Reference
Interference with
None Some limitation Extremely limited
normal activity
SABA use for
symptom control ≤2 days/week >2 days/week Several times per day
(not to prevent EIB )
Appendix B: NHLBI Asthma Classification
Lung function
FEV1 (% predicted)
or peak flow Not applicable Not applicable Not applicable
Impairment
>80% >80% 60–80% 60–80% <60% <60%
(% personal best)
FEV1 /FVC >80% Not applicable 75–80% Not applicable <75% Not applicable
Validated questionnaires†
RETURN TO
ATAQ Not applicable Not applicable 0 Not applicable Not applicable 1–2 Not applicable Not applicable 3–4
THE BEGINNING
ACQ ≤0.75‡ ≥1.5 Not applicable
ACT ≥20 16–19 ≤15
Asthma exacerbations 0–1/year 2–3/year ≥2/year >3/year ≥2/year
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
requiring oral systemic
corticosteroids§ Consider severity and interval since last asthma exacerbation.
Reduction in lung
Evaluation requires long-term Evaluation requires long-term Evaluation requires long-term
Risk
growth/Progressive loss Not applicable Not applicable Not applicable
follow-up care. follow-up care. follow-up care.
of lung function
Treatment-related Medication side effects can vary in intensity from none to very troublesome and worrisome.
adverse effects The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk.
Recommended Action Step up at least
Step up 1 step Step up 1 step
for Treatment 1 step Consider short course of oral systemic corticosteroids.
(See “Stepwise Approach for Maintain current step. Reevaluate in 2–6 weeks to achieve control. Step up 1–2 steps.
Managing Asthma Long Term,” Regular follow-up every 1–6 months.
page 7) For children 0–4 years, if no clear benefit observed in 4–6 Reevaluate in 2 weeks to achieve control.
Consider step down if well controlled for at least weeks, consider adjusting therapy or alternative diagnoses.
The stepwise approach is meant
to help, not replace, the clinical 3 months.
Before step up in treatment:
decisionmaking needed to meet Review adherence to medication, inhaler technique, and environmental control. If alternative treatment was used,
individual patient needs. discontinue and use preferred treatment for that step. For side effects, consider alternative treatment options.
Abbreviations: ACQ, Asthma Control Questionnaire©; ACT, Asthma Control TestTM; ATAQ, Asthma Therapy Assessment Questionnaire©; EIB, exercise-induced bronchospasm; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second;
SABA, short-acting beta2-agonist.
† Minimal important difference: 1.0 for the ATAQ; 0.5 for the ACQ; not determined for the ACT.
‡ ACQ values of 0.76–1.4 are indeterminate regarding well-controlled asthma.
§ Data are insufficient to link frequencies of exacerbations with different levels of asthma control. Generally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)
indicate poorer asthma control.
JUDGMENT.
THIS PATHWAY
AND DOES NOT
REPLACE CLINICAL
SERVES AS A GUIDE
CLINICAL PATHWAY: THIS PATHWAY
SERVES AS A GUIDE
Inpatient Asthma AND DOES NOT
Appendix C: NHLBI Step-Up Therapy REPLACE CLINICAL
JUDGMENT.
Asthma Care Quick Reference 7
STEPWISE APPROACH FOR MANAGING ASTHMA LONG TERM
The stepwise approach tailors the selection of medication to the level of asthma severity (see page 5) or asthma control (see page 6).
Generally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)
The stepwise approach is meant to help, not replace, the clinical decisionmaking needed to meet individual patient needs.
Abbreviations: ACQ, Asthma Control Questionnaire©; ACT, Asthma Control TestTM; ATAQ, Asthma Therapy Assessment Questionnaire©; EIB, exercise-induced bronchospasm; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second;
discontinue and use preferred treatment for that step. For side effects, consider alternative treatment options.
STEP UP IF NEEDED (first, check medication adherence, inhaler technique, environmental control, and comorbidities)
ASSESS
CONTROL:
STEP DOWN IF POSSIBLE (and asthma is well controlled for at least 3 months)
STEP 5 STEP 6
STEP 3 STEP 4
STEP 1 STEP 2
At each step: Patient education, environmental control, and management of comorbidities
Intermittent Persistent Asthma: Daily Medication
Asthma Consult with asthma specialist if step 3 care or higher is required. Consider consultation at step 2.
Preferred SABA as low-dose ICS medium-dose medium-dose high-dose ICS high-dose ICS
Treatment† needed ICS ICS + +
+ either LABA or either LABA or
0–4 years of age
either LABA or montelukast montelukast
montelukast +
oral corticosteroids
Alternative cromolyn or
Treatment†,‡ montelukast
If clear benefit is not observed in 4–6 weeks, and medication technique and adherence are satisfactory,
consider adjusting therapy or alternate diagnoses.
SABA as needed for symptoms; intensity of treatment depends on severity of symptoms.
Quick-Relief With viral respiratory symptoms: SABA every 4–6 hours up to 24 hours (longer with physician consult). Consider short
Medication course of oral systemic corticosteroids if asthma exacerbation is severe or patient has history of severe exacerbations.
Caution: Frequent use of SABA may indicate the need to step up treatment.
Intermittent Persistent Asthma: Daily Medication
Asthma Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3.
Preferred SABA as needed low-dose ICS low-dose ICS medium-dose high-dose ICS high-dose ICS
Treatment† + ICS + +
either LABA, + LABA LABA
LTRA, or LABA +
5–11 years of age
theophylline(b) oral corticosteroids
OR
Alternative cromolyn, LTRA, medium-dose ICS high-dose ICS high-dose ICS
medium-dose
Treatment†,‡ or theophylline§ + + +
ICS either LTRA or either LTRA or either LTRA or
theophylline§ theophylline§ theophylline§
Consider subcutaneous allergen immunotherapy for +
patients who have persistent, allergic asthma. oral corticosteroids
SABA as needed for symptoms. The intensity of treatment depends on severity of symptoms: up to 3 treatments
§ Data are insufficient to link frequencies of exacerbations with different levels of asthma control.
Quick-Relief every 20 minutes as needed. Short course of oral systemic corticosteroids may be needed.
Medication Caution: Increasing use of SABA or use >2 days/week for symptom relief (not to prevent EIB ) generally indicates
† Minimal important difference: 1.0 for the ATAQ; 0.5 for the ACQ; not determined for the ACT.
inadequate control and the need to step up treatment.
Intermittent Persistent Asthma: Daily Medication
Asthma Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3.
Preferred SABA as needed low-dose ICS low-dose ICS medium-dose high-dose ICS high-dose ICS
‡ ACQ values of 0.76–1.4 are indeterminate regarding well-controlled asthma.
Treatment† + ICS + +
LABA + LABA LABA
OR LABA AND +
oral
≥12 years of age
medium-dose ICS consider
corticosteroid§§
omalizumab for
Alternative cromolyn, LTRA, low-dose ICS medium-dose ICS patients who AND
Treatment†,‡ or theophylline§ + + have allergies†† consider
either LTRA, either LTRA, omalizumab for
theophylline,§ theophylline,§ patients who
or zileuton‡‡ or zileuton‡‡ have allergies††
Consider subcutaneous allergen immunotherapy
for patients who have persistent, allergic asthma.
SABA as needed for symptoms. The intensity of treatment depends on severity of symptoms: up to 3 treatments
SABA, short-acting beta2-agonist.
indicate poorer asthma control.
Quick-Relief every 20 minutes as needed. Short course of oral systemic corticosteroids may be needed.
Medication Caution: Use of SABA >2 days/week for symptom relief (not to prevent EIB ) generally indicates inadequate control
individual patient needs.
and the need to step up treatment.
Abbreviations: EIB, exercise-induced bronchospasm; ICS, inhaled corticosteroid; LABA, inhaled long-acting beta2-agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled
short-acting beta2-agonist.
† Treatment options are listed in alphabetical order, if more than one.
‡ If alternative treatment is used and response is inadequate, discontinue and use preferred treatment before stepping up.
§ Theophylline is a less desirable alternative because of the need to monitor serum concentration levels.
Based on evidence for dust mites, animal dander, and pollen; evidence is weak or lacking for molds and cockroaches. Evidence is strongest for immunotherapy with single allergens.
The role of allergy in asthma is greater in children than in adults.
†† Clinicians who administer immunotherapy or omalizumab should be prepared to treat anaphylaxis that may occur.
‡‡ Zileuton is less desirable because of limited studies as adjunctive therapy and the need to monitor liver function.
§§ Before oral corticosteroids are introduced, a trial of high-dose ICS + LABA + either LTRA, theophylline, or zileuton, may be considered, although this approach has not been studied
in clinical trials.
RETURN TO
THE BEGINNING
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
LAST UPDATED: 11.11.19
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
LAST UPDATED: 11.11.19
8
Inpatient Asthma
ESTIMATED COMPARATIVE DAILY DOSAGES: INHALED CORTICOSTEROIDS FOR LONG-TERM ASTHMA CONTROL
CLINICAL PATHWAY:
0–4 years of age 5–11 years of age ≥12 years of age
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
Daily Dose Low Medium High Low Medium High Low Medium High
MEDICATION
Beclomethasone MDI† N/A N/A N/A 80–160 mcg >160–320 mcg >320 mcg 80–240 mcg >240–480 mcg >480 mcg
40 mcg/puff 1–2 puffs 3–4 puffs 1–3 puffs 4–6 puffs
Asthma Care Quick Reference
2x/day 2x/day 2x/day 2x/day
1 puff 2x/day 2 puffs 2x/day 1 puff am, 2–3 puffs ≥4 puffs
80 mcg/puff ≥3 puffs 2x/day
2 puffs pm 2x/day 2x/day
Appendix D: Comparative Daily Dosages
Budesonide DPI† N/A N/A N/A 180–360 mcg >360–720 mcg >720 mcg 180–540 mcg >540–1,080 mcg >1,080 mcg
90 mcg/inhalation 1–2 inhs† 2x/day 3–4 inhs† 2x/day 1–3 inhs† 2x/day
180 mcg/ 2 inhs† 2x/day ≥3 inhs† 2x/day 1 inh† am, 2–3 inhs† 2x/day ≥4 inhs† 2x/day
inhalation 2 inhs† pm
Budesonide Nebules 0.25–0.5 mg >0.5–1.0 mg >1.0 mg 0.5 mg 1.0 mg 2.0 mg N/A N/A N/A
RETURN TO
THE BEGINNING
0.25 mg 1–2 nebs†/day 1 neb† 2x/day
0.5 mg 1 neb†/day 2 nebs†/day 3 nebs†/day 1 neb†/day 1 neb† 2x/day
1.0 mg 1 neb†/day 2 nebs†/day 1 neb†/day 1 neb† 2x/day
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
Ciclesonide MDI† N/A N/A N/A 80–160 mcg >160–320 mcg >320 mcg 160–320 mcg >320–640 mcg >640 mcg
1 puff am,
80 mcg/puff 1–2 puffs/day 2 puffs pm– ≥3 puffs 2x/day 1–2 puffs 2x/day 3–4 puffs 2x/day
2 puffs 2x/day
160 mcg/puff 1 puff/day 1 puff 2x/day ≥2 puffs 2x/day 2 puffs 2x/day ≥3 puffs 2x/day
Flunisolide MDI† N/A N/A N/A 160 mcg 320–480 mcg ≥480 mcg 320 mcg >320–640 mcg >640 mcg
80 mcg/puff 1 puff 2x/day 2–3 puffs 2x/day ≥4 puffs 2x/day 2 puffs 2x/day 3–4 puffs 2x/day ≥5 puffs 2x/day
It is preferable to use a higher mcg/puff or mcg/inhalation formulation to achieve as low a number of puffs or inhalations as possible.
† Abbreviations: DPI, dry powder inhaler (requires deep, fast inhalation); inh, inhalation; MDI, metered dose inhaler (releases a puff of medication); neb, nebule.
JUDGMENT.
THIS PATHWAY
AND DOES NOT
REPLACE CLINICAL
SERVES AS A GUIDE
LAST UPDATED: 11.11.19
ESTIMATED COMPARATIVE DAILY DOSAGES:
INHALED CORTICOSTEROIDS FOR LONG-TERM ASTHMA CONTROL (continued)
Inpatient Asthma
0–4 years of age 5–11 years of age ≥12 years of age
Daily Dose Low Low Low
CLINICAL PATHWAY:
Medium High Medium High Medium High
MEDICATION
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
Fluticasone MDI† 176 mcg >176–352 mcg >352 mcg 88–176 mcg >176–352 mcg >352 mcg 88–264 mcg >264–440 mcg >440 mcg
44 mcg/puff 2 puffs 2x/day 3–4 puffs 1–2 puffs 3–4 puffs 1–3 puffs
2x/day 2x/day 2x/day 2x/day
110 mcg/puff ≥2 puffs 2 puffs 2x/day 3 puffs 2x/day
1 puff 2x/day 1 puff 2x/day ≥2 puffs 2x/day
2x/day
220 mcg/puff 1 puffs 2x/day ≥2 puffs 2x/day
Appendix D: Comparative Daily Dosages
Fluticasone DPI† N/A N/A N/A 100–200 mcg >200–400 mcg >400 mcg 100–300 mcg >300–500 mcg >500 mcg
50 mcg/inhalation 1–2 inhs† 2x/day 3–4 inhs† 2x/day 1–3 inhs† 2x/day
100 mcg/inhalation 1 inh† 2x/day 2 inhs† 2x/day >2 inhs† 2x/day 2 inhs† 2x/day ≥3 inhs† 2x/day
250 mcg/inhalation 1 inh† 2x/day 1 inh† 2x/day ≥2 inhs† 2x/day
RETURN TO
Mometasone DPI† N/A N/A N/A 110 mcg 220–440 mcg >440 mcg 110–220 mcg >220–440 mcg >440 mcg
THE BEGINNING
110 mcg/inhalation 3–4 inhs† pm or
1 inh†/day 1–2 inhs† 2x/day ≥3 inhs† 2x/day 1–2 inhs† pm ≥3 inhs† 2x/day
2 inhs† 2x/day
220 mcg/inhalation 1–2 inhs†/day ≥3 inhs† divided 1 inh† pm 1 inh† 2x/day or ≥3 inhs† divided
in 2 doses 2 inhs† pm in 2 doses
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
It is preferable to use a higher mcg/puff or mcg/inhalation formulation to achieve as low a number of puffs or inhalations as possible.
† Abbreviations: DPI, dry powder inhaler (requires deep, fast inhalation); inh, inhalation; MDI, metered dose inhaler (releases a puff of medication); neb, nebule.
Therapeutic Issues Pertaining to Inhaled Corticosteroids (ICSs) for Long-Term Asthma Control
The most important determinant of appropriate dosing is the clinician’s judgment many European countries and in some scientific literature. Dry powder inhaler (DPI)
of the patient’s response to therapy. The clinician must monitor the patient’s doses are expressed as the amount of drug in the inhaler following activation.
response on several clinical parameters (e.g., symptoms; activity level; measures of
For children <4 years of age: The safety and efficacy of ICSs in children <1 year of
lung function) and adjust the dose accordingly. Once asthma control is achieved
age has not been established. Children <4 years of age generally require delivery of
and sustained at least 3 months, the dose should be carefully titrated down to the
ICS (budesonide and fluticasone MDI) through a face mask that fits snugly over nose
minimum dose necessary to maintain control.
and mouth to avoid nebulizing in the eyes. Face should be washed after treatment
Some doses may be outside package labeling, especially in the high-dose range. to prevent local corticosteroid side effects. For budesonide, the dose may be given
Budesonide nebulizer suspension is the only inhaled corticosteroid (ICS) with 1–3 times daily. Budesonide suspension is compatible with albuterol, ipratropium,
FDA-approved labeling for children <4 years of age. and levalbuterol nebulizer solutions in the same nebulizer. Use only jet nebulizers, as
ultrasonic nebulizers are ineffective for suspensions. For fluticasone MDI, the dose
Metered-dose inhaler (MDI) dosages are expressed as the actuator dose (amount
should be divided 2 times daily; the low dose for children <4 years of age is higher
leaving the actuator and delivered to the patient), which is the labeling required in the
Asthma Care Quick Reference
than for children 5–11 years of age because of lower dose delivered with face mask
United States. This is different from the dosage expressed as the valve dose (amount
and data on efficacy in young children.
of drug leaving the valve, not all of which is available to the patient), which is used in
9
JUDGMENT.
THIS PATHWAY
AND DOES NOT
REPLACE CLINICAL
SERVES AS A GUIDE
CLINICAL PATHWAY: THIS PATHWAY
SERVES AS A GUIDE
Inpatient Asthma AND DOES NOT
Appendix D: Comparative Daily Dosages REPLACE CLINICAL
JUDGMENT.
10 Asthma Care Quick Reference
USUAL DOSAGES FOR OTHER LONG-TERM CONTROL MEDICATIONS*
Medication 0–4 years of age 5–11 years of age ≥12 years of age
Combined Medication (inhaled corticosteroid + long-acting beta2-agonist)
Fluticasone/Salmeterol — N/A† 1 inhalation 2x/day; dose 1 inhalation 2x/day; dose
DPI† 100 mcg/50 mcg, 250 mcg/50 mcg, or depends on level of depends on level of severity
500 mcg/50 mcg severity or control or control
MDI† 45 mcg/21 mcg, 115 mcg/21 mcg, or
230 mcg/21 mcg
Budesonide/Formoterol — N/A† 2 puffs 2x/day; dose 2 puffs 2x/day; dose depends
MDI† 80 mcg/4.5 mcg or 160 mcg/4.5 mcg depends on level of on level of severity or control
severity or control
Mometasone/Formoterol — N/A† N/A† 2 inhalations 2x/day; dose
MDI† 100 mcg/5 mcg depends on severity of asthma
Leukotriene Modifiers
Leukotriene Receptor Antagonists (LTRAs)
Montelukast — 4 mg or 5 mg chewable tablet, 4 mg every night at 5 mg every night at 10 mg every night at
4 mg granule packets, 10 mg tablet bedtime (1–5 years of age) bedtime (6–14 years of age) bedtime
Zafirlukast — 10 mg or 20 mg tablet N/A† 10 mg 2x/day 40 mg daily
Take at least 1 hour before or 2 hours after a meal. (7–11 years of age) (20 mg tablet 2x/day)
Monitor liver function.
5-Lipoxygenase Inhibitor
Zileuton — 600 mg tablet N/A† N/A† 2,400 mg daily
Monitor liver function. (give 1 tablet 4x/day)
Immunomodulators
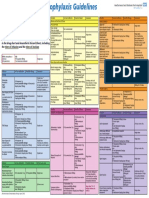
Omalizumab (Anti IgE†) — N/A† N/A† 150–375 mg subcutaneous
Subcutaneous injection, 150 mg/1.2 mL following every 2–4 weeks, depending
reconstitution with 1.4 mL sterile water for injection on body weight and
Monitor patients after injections; be prepared to treat pretreatment serum IgE level
anaphylaxis that may occur.
Cromolyn
Cromolyn — Nebulizer: 20 mg/ampule 1 ampule 4x/day, N/A† 1 ampule 4x/day 1 ampule 4x/day
<2 years of age
Methylxanthines
Theophylline — Starting dose 10 mg/kg/ Starting dose 10 mg/ Starting dose 10 mg/kg/day
Liquids, sustained-release tablets, and capsules day; usual maximum: kg/day; usual maximum: up to 300 mg maximum;
Monitor serum concentration levels. <1 year of age: 0.2 (age in 16 mg/kg/day usual maximum:
weeks) + 5 = mg/kg/day 800 mg/day
≥1 year of age:
16 mg/kg/day
Inhaled Long-Acting Beta2-Agonists (LABAs) – used in conjunction with ICS† for long-term control; LABA is NOT to be used as monotherapy
Salmeterol — DPI† 50 mcg/blister N/A† 1 blister every 12 hours 1 blister every 12 hours
Formoterol —DPI† 12 mcg/single-use capsule N/A† 1 capsule every 12 hours 1 capsule every 12 hours
Oral Systemic Corticosteroids
Methylprednisolone — 2, 4, 8, 16, 32 mg tablets 0.25–2 mg/kg daily 0.25–2 mg/kg daily 7.5–60 mg daily in single
in single dose in a.m. in single dose in a.m. dose in a.m. or every other
or every other day as or every other day as day as needed for control
Prednisolone — 5 mg tablets; 5 mg/5 cc, 15 mg/5 cc needed for control needed for control Short course “burst”: to
Short course “burst”: Short course “burst”: achieve control, 40–60 mg/
1–2 mg/kg/day, max 60 1–2 mg/kg/day, max 60 day as single or 2 divided
Prednisone — 1, 2.5, 5, 10, 20, 50 mg tablets; mg/d for 3–10 days mg/d for 3–10 days doses for 3–10 days
5 mg/cc, 5 mg/5 cc
* Dosages are provided for those products that have been approved by the U.S. Food and Drug Administration or have sufficient clinical trial safety and efficacy data in the
appropriate age ranges to support their use.
† Abbreviations: DPI, dry powder inhaler; IgE, immunoglobulin E; MDI, metered-dose inhaler; N/A, not available (not approved, no data available, or safety and efficacy not
established for this age group).
The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. The clinician
must monitor the patient’s response on several clinical parameters (e.g., symptoms; activity level; measures of lung function) and adjust
the dose accordingly. Once asthma control is achieved and sustained at least 3 months, the dose should be carefully titrated down to the
minimum dose necessary to maintain control.
RETURN TO
THE BEGINNING
CONTACTS: CHRISTINA GIUDICE, APRN | ALEX HOGAN, MD | ANAND SEKARAN, MD
LAST UPDATED: 11.11.19
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
THIS PATHWAY
CLINICAL PATHWAY: SERVES AS A GUIDE
Emergency Department Asthma
AND DOES NOT
REPLACE CLINICAL
JUDGMENT.
Inclusion Criteria: 1 yrs old, previous diagnosis of asthma or 2 previous episodes of wheezing, MPIS 5
Exclusion Criteria: <1 yrs old, bronchiolitis or pneumonia as primary diagnosis, chronic cardiac or lung disease other than asthma
Initial Assessment (MPIS 5):
Dexamethasone 0.6 mg/kg (max 16 mg) PO/IM
(Can substitute with prednisolone/prednisone/methylprednisolone 2 mg/kg at initial
provider s discretion. Can omit if already on oral steroids.)
MPIS 5-6 MPIS 7
Albuterol 4 puffs MDI/spacer
Albuterol 5 mg/
(with teach) OR
MPIS 6 MPIS 7 Ipratropium 500 mcg
Albuterol 2.5 mg neb
via nebulizer
Calculate MPIS
Reassess in 15-30 minutes
Calculate MPIS
Discharge Criteria/Instructions:
MDI/spacer teach
Albuterol 4 puffs
F/u with PCP in 2-3 days
MDI/spacer
Medications: Albuterol PRN MPIS 6 MPIS 7
(with teach)
*Consider Prednisolone/Prednisone for patients that
if not already done
might benefit from longer steroids. Start 24 hours
after Dexamethasone dose. Long Albuterol treatment:
• <20 kg: 10 mg over 1 hour
• >20 kg: 20 mg over 1 hour
• Reassess in 15-30 minutes
• Calculate MPIS
MPIS 6 MPIS 7-8 MPIS 9-10 MPIS 11-12 MPIS 13
Observe for 1 hour
Medications: Medications: Medications: Medications:
Albuterol 5 mg neb Resume continuous Resume continuous Resume continuous
Reassess q2hr Albuterol at Albuterol at Albuterol at 20 mg/hr
Calculate MPIS ED provider to place previous dose previous dose Consider additional
order Initiate ED provider to place ED provider to place therapies per PICU
Albuterol wean order Initiate order Initiate consultation (e.g,
RT will rescore MPIS Albuterol wean Albuterol wean methylprednisolone if
and speak with RT will rescore MPIS RT will rescore MPIS not done, MgSO4,
provider to place and speak with and speak with terbutaline)
MPIS 6 MPIS 7
appropriate provider to place provider to place
Albuterol order appropriate appropriate Nursing:
Albuterol order Albuterol order Place PIV (if not done)
Nursing:
Place PIV if Nursing: Nursing: Consults:
inadequate oral Place PIV if Place PIV Consult PICU attending
Discharge Criteria and intake, or unable to inadequate oral in ED: observe in ED for
Instructions: take oral steroids intake, or unable to further improvement
MDI/spacer teach take oral steroids vs admission to PICU
F/u with PCP in 2-3 days
Medications: Albuterol q4hr
*Consider Prednisolone/ Admission:
Prednisone for patients that might - Admit to MS floor or PICU
benefit from longer steroids. Start in discussion with IMT and
Admission:
24 hours after Dexamethasone PICU attending
Admit to MS (PHM or Pulmonary if patient is known to them)
dose. - If to be admitted to MS floor,
See Inpatient Asthma Pathway
ED provider to place order
At time of transfer: Initiate Albuterol wean . RT
will rescore MPIS and speak
Re-assess patient and calculate MPIS
with provider to place
Inform attending and admitting team if MPIS is increasing
appropriate
Hold transfer if MPIS 13 and consider PICU consult
Albuterol order.
CONTACTS: ERIC HOPPA, MD | KRISTIN WELCH, MD
LAST UPDATED: 10.21.19
©2019 Connecticut Children’s Medical Center. All rights reserved. 19-004
You might also like
- Pharmacology for Student and Pupil Nurses and Students in Associated ProfessionsFrom EverandPharmacology for Student and Pupil Nurses and Students in Associated ProfessionsNo ratings yet
- Brosur-VYGON Emergency APO-CPAP KitDocument2 pagesBrosur-VYGON Emergency APO-CPAP KitIrfan SulaimanNo ratings yet
- Croup Summary PDFDocument2 pagesCroup Summary PDFnurfitriaNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFNety Pandung SalembanNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFJim Christian EllaserNo ratings yet
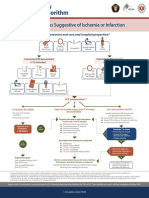
- Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionDocument1 pageSyndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionAnonymous CKAborxxwNo ratings yet
- Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionDocument8 pagesSyndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionNugroho TeguhNo ratings yet
- Acut Coronary SyndromesDocument1 pageAcut Coronary SyndromesMuhittin Selçuk ÖzkanNo ratings yet
- Should Patients With Mild Asthma Use Inhaled SteroidsDocument5 pagesShould Patients With Mild Asthma Use Inhaled Steroidstsiko111No ratings yet
- Formoterol Gonzaga.Document2 pagesFormoterol Gonzaga.Sheryl Anne GonzagaNo ratings yet
- 65 - Approach To Patients With CancerDocument1 page65 - Approach To Patients With CancerRica Alyssa PepitoNo ratings yet
- Asthma Clinical Pathway - Inpatient - Children's Hospital of PhiladelphiaDocument2 pagesAsthma Clinical Pathway - Inpatient - Children's Hospital of Philadelphiajoshua elnissiNo ratings yet
- Drug Study Acute BronchitisDocument6 pagesDrug Study Acute BronchitisCarl Simon CalingacionNo ratings yet
- MILV10NDocument5 pagesMILV10Ngarywall.ukNo ratings yet
- Adenosine 8-28-22Document1 pageAdenosine 8-28-22ladawskiNo ratings yet
- Acute Coronary Syndromes - HandoutDocument4 pagesAcute Coronary Syndromes - Handoutapi-641524095No ratings yet
- Pediatric Guidelines: Head and Neck Infections - MastoiditisDocument3 pagesPediatric Guidelines: Head and Neck Infections - MastoiditisJr SparkNo ratings yet
- Algorithm D: Pharmacological Treatment of Chronic Asthma in Children Under 5Document1 pageAlgorithm D: Pharmacological Treatment of Chronic Asthma in Children Under 5samNo ratings yet
- HQ - Tips For Dealing With Covid-19 at Home Version4 FINALDocument1 pageHQ - Tips For Dealing With Covid-19 at Home Version4 FINALYıldırım SütlüoğluNo ratings yet
- Stemi NSTEMI or Unstable Angina: Offer AspirinDocument1 pageStemi NSTEMI or Unstable Angina: Offer AspirinVemuri SrinivasNo ratings yet
- Posters For ClinicDocument80 pagesPosters For ClinicdenzkissaieNo ratings yet
- Megestrol AcetateDocument3 pagesMegestrol Acetateunkown userNo ratings yet
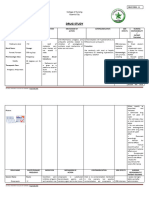
- Drug Study RosillosaDocument4 pagesDrug Study RosillosaJb RosillosaNo ratings yet
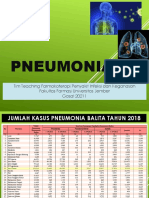
- Pneumonia: Tim Teaching Farmakoterapi Penyakit Infeksi Dan Keganasan Fakultas Farmasi Universitas Jember Gasal 20211Document67 pagesPneumonia: Tim Teaching Farmakoterapi Penyakit Infeksi Dan Keganasan Fakultas Farmasi Universitas Jember Gasal 20211Evie WulansariNo ratings yet
- Community Acquired Pneumonia CAP 1.28.21Document1 pageCommunity Acquired Pneumonia CAP 1.28.21Illaizah EdictoNo ratings yet
- DR - Dr. Fardah Akil, SP - PD (K) Geh Paracetamol 500mg/6jam/oral (Selama 3x24jam) Dr. Faisal Muchtar, SP - An-KICDocument2 pagesDR - Dr. Fardah Akil, SP - PD (K) Geh Paracetamol 500mg/6jam/oral (Selama 3x24jam) Dr. Faisal Muchtar, SP - An-KICfatimah syamNo ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital Preparationgusti angri angalanNo ratings yet
- Recommendation For The Use of Antibiotics For The Treatment of InfectionDocument5 pagesRecommendation For The Use of Antibiotics For The Treatment of InfectionGem BorjaNo ratings yet
- 3 RRP COPD GuidelinesDocument4 pages3 RRP COPD Guidelinesjyothi vallabhaneniNo ratings yet
- Drug StudyDocument11 pagesDrug StudyMichelle TamorNo ratings yet
- Cost-Effectiveness of New Antiplatelet Regimens Used As Secondary Prevention of Stroke or Transient Ischemic AttackDocument12 pagesCost-Effectiveness of New Antiplatelet Regimens Used As Secondary Prevention of Stroke or Transient Ischemic AttackTatiana Siska WardaniNo ratings yet
- Fundamentals of Oxygen Therapy.6Document3 pagesFundamentals of Oxygen Therapy.6Fitri Amelia RizkiNo ratings yet
- TestDocument1 pageTestnurul wahyuniNo ratings yet
- Family Medicine LectureDocument24 pagesFamily Medicine Lectureapi-549451092No ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationIGOR SHEYNINNo ratings yet
- Felinos, Dexmedetomina em Infusão e Reversão Com Atipamezole 2017Document7 pagesFelinos, Dexmedetomina em Infusão e Reversão Com Atipamezole 2017Joyce De PaulaNo ratings yet
- Efficacy and Safety of Remifentanil in A Rapid Sequence - 2020 - Anaesthesia CriDocument6 pagesEfficacy and Safety of Remifentanil in A Rapid Sequence - 2020 - Anaesthesia CriRicardoNo ratings yet
- Annals of Clinical Anesthesia Research: Ketamine in Current Clinical Practice: Anything New To Write Home About?Document5 pagesAnnals of Clinical Anesthesia Research: Ketamine in Current Clinical Practice: Anything New To Write Home About?regina pingkanNo ratings yet
- Generic Name:: Paracetamol, AcetaminophenDocument3 pagesGeneric Name:: Paracetamol, AcetaminophenShanel Aubrey Aglibut100% (1)
- ARDS Concept Map - BunayogDocument2 pagesARDS Concept Map - BunayogJacela Annsyle BunayogNo ratings yet
- ENGLISH MASTER Tips+for+dealing+with+Covid-19+at+home V5Document1 pageENGLISH MASTER Tips+for+dealing+with+Covid-19+at+home V5Pankaj KumarNo ratings yet
- Edmark 2014Document9 pagesEdmark 2014Juampi FerrariNo ratings yet
- Antibiotic Surgical Prophylaxis Protocol SMH October 2018 UpdateDocument7 pagesAntibiotic Surgical Prophylaxis Protocol SMH October 2018 Updatessrnew2023No ratings yet
- ICU One Pager ARDS v1.1Document1 pageICU One Pager ARDS v1.1Michael LevitNo ratings yet
- 2 Article JCDR FinalDocument4 pages2 Article JCDR FinalMythology KingdomNo ratings yet
- Tachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDocument1 pageTachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDendy Frannuzul RamadhanNo ratings yet
- AlgorithmACLStachycardiawithapulse PDFDocument1 pageAlgorithmACLStachycardiawithapulse PDFDendy Frannuzul RamadhanNo ratings yet
- Amlodipine Drug StudyDocument2 pagesAmlodipine Drug StudyAbigail Basco100% (3)
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Celecoxib Drug StudyDocument1 pageCelecoxib Drug StudyMan Gatuanko83% (12)
- COPD Guideline Ver 1.8Document9 pagesCOPD Guideline Ver 1.8Dina AyupnNo ratings yet
- Supplemental Online ContentDocument21 pagesSupplemental Online ContentKelompok BelajarNo ratings yet
- Anestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementDocument3 pagesAnestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementGilliNo ratings yet
- Cytopro Clinical Study ProtocolDocument19 pagesCytopro Clinical Study ProtocolbeequesadaNo ratings yet
- Manifest + Data Vaksin MbuDocument3 pagesManifest + Data Vaksin MbuIntan LestariNo ratings yet
- Daftar Obat High Alert Dan High RiskDocument2 pagesDaftar Obat High Alert Dan High RiskLidya rahmahNo ratings yet
- CAR-T Cell Therapy in India Requires A Paradigm ShiftDocument9 pagesCAR-T Cell Therapy in India Requires A Paradigm ShiftIndraneel GhoshNo ratings yet
- In F Circ ManualDocument4 pagesIn F Circ Manualalexa cuevasNo ratings yet
- New Microsoft Word DocumentDocument79 pagesNew Microsoft Word DocumentalexpharmNo ratings yet
- Pharmacology of Essential Medicine PDFDocument211 pagesPharmacology of Essential Medicine PDFKaka MamaNo ratings yet
- Pharmacoepidemiology: Pinar Yalcin Balcik, Gulcan KahramanDocument6 pagesPharmacoepidemiology: Pinar Yalcin Balcik, Gulcan KahramandebbyirmaNo ratings yet
- What Are Drugs!!Document6 pagesWhat Are Drugs!!CS AbdullahNo ratings yet
- Pharma AssignmentDocument2 pagesPharma AssignmentAbigail BascoNo ratings yet
- CPP BVM VentilationDocument5 pagesCPP BVM VentilationDhwwi YovanaNo ratings yet
- Albendazole 400 MG: NO Nama Obat Harga Sisa Tanggal ExpiredDocument6 pagesAlbendazole 400 MG: NO Nama Obat Harga Sisa Tanggal ExpiredKlinik PKBI AcehNo ratings yet
- ASHI ACLS - G2015 - Spec SheetDocument2 pagesASHI ACLS - G2015 - Spec SheetErwin RomeroNo ratings yet
- Pharmacology Final CoachingDocument4 pagesPharmacology Final CoachingCasey Jon VeaNo ratings yet
- Short Notes PHJDocument5 pagesShort Notes PHJVikash KushwahaNo ratings yet
- Kelompok Tugas Farmakoterapi LanjutanDocument2 pagesKelompok Tugas Farmakoterapi LanjutanWahyu Mafrudin .ANo ratings yet
- 8 10Document57 pages8 10rahmaNo ratings yet
- MDR - Oral Boomer PDFDocument15 pagesMDR - Oral Boomer PDFBandameedi RamuNo ratings yet
- Stratamed For PatientsDocument2 pagesStratamed For PatientsTechtureGNo ratings yet
- 06 Fagiolini 3Document10 pages06 Fagiolini 3gibbiNo ratings yet
- DivalproexDocument2 pagesDivalproexeefrheelNo ratings yet
- Drug-Food Interactions: DR - Kawooya Francis, Pharmd, MpsDocument28 pagesDrug-Food Interactions: DR - Kawooya Francis, Pharmd, MpsNina100% (2)
- RosperidonDocument7 pagesRosperidonEndang SusilowatiNo ratings yet
- CAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Document5 pagesCAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Sindu SankarNo ratings yet
- Daftar Obat: Untuk Perencanaan Tahun 2021Document17 pagesDaftar Obat: Untuk Perencanaan Tahun 2021jimmypatabang10No ratings yet
- Healthcare Cost Containment 1Document3 pagesHealthcare Cost Containment 1Cipta BangunNo ratings yet
- MCQs Pharmacology - Series III-ADocument13 pagesMCQs Pharmacology - Series III-Asidharta_chatterjee100% (1)
- National Essential Drug List Comments: Lowest Level of UseDocument6 pagesNational Essential Drug List Comments: Lowest Level of UseportosinNo ratings yet
- Chemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersDocument9 pagesChemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersRiri AmalinaNo ratings yet
- Vademecum OspsaDocument95 pagesVademecum OspsaGuadalupe FloresNo ratings yet