Professional Documents
Culture Documents
Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital Prepartion
Uploaded by
Nugroho TeguhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital Prepartion
Uploaded by
Nugroho TeguhCopyright:
Available Formats
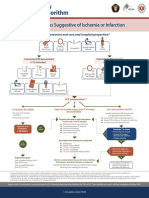
Acute Coronary
Syndromes Algorithm
Syndroms Suggestive of Ischemia or Infarction
EMS assessment and care and hospital prepartion*
Oxygen
Aspirin (If O sat< 94% Activate Cardiac Pain
2
12–Lead ECG Control
160–325 mg or O Sat>90%
2
Cath Lab
with COPD)
Concurrent ED assessment Immediate ED general
(<10 minutes) treatment
Aspirin Nitroglycerin
Check Vital Physical If O2 sat<94% Pain
IV Access 160–325 mg Sublingual or
Signs Exam Start Oxygen (If not already taken) Control spray
Activate Cardiac Cardiac Marker Chest X-ray
Cath Lab 12–Lead ECG
Levels (<30 mins)
ECG Interpretation**
ST-elevation MI (STEMI) High-risk unstable angina/non-ST-elevation Low-/Intermediate-risk ACS
Start adjunctive therapies
MI (UA/NSTEMI)
Consider admission to ED chest pain unit
as indicated or to appropriate bed and follow:
Do not delay reperfusion Serial cardiac markers (including troponin)
Troponin elevated or high-risk patient Repeat ECG/continuous ST-segment monitoring
Consider early invasive strategy if: Consider noninvasive diagnostic test
Refractory ischemic chest discomfort
Time from onset Recument/persistent ST deviation
of symptoms
>12 Ventricular tachycardia
hours Develops 1 or more:
≤ 12 hours? Hemodynamic instability
Signs of heart failure Clinical high-risk features
Dynamic ECG chages
consistent with ischemia
Troponin elevated
Start adjunctive treatments as indicated
≤12 Nitroglycerin
hours Heparin (UFH or LMWH)
Consider: PO β-blockers
Consider: Clopidogrel Abnormal diagnostic
Consider: Glycoprotein llb/llla inhibitor noninvasive imaging or
physiologic testing?
Reperfusion goals:
Door-to-balloon inflation (PCI)*** Admit to monitored bed Assess risk status Continue
goal of 90 minutes ASA heparin, and other therapies as indicated If no evidence of ischemia or
Door-to-needle (fibrinolysis) ACE inhibitor/ARB; HMG CoA reductase inhibitor (statin therapy) infarction by testing, can
goal of 30 minutes Not at high risk: cardiology to risk stratity discharge with follow-up
* O’Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, Menon V, O’Neil BJ, Travers AH, Yannopoulos D. “Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for
Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation. 2010;122(suppl 3):S787-S817. http://circ.ahajoumals.org/content/122/18_suppl_3/S787
**Afolabi BA, Novaro GM, Pinski SL, Fromkin KR, Bush HS. Use of the prehoapital ECG improves door to balloon times in ST segment elevation myocardial infarction irrespective of time of day or day of week. Emerg Med J. 2007;24:588-591
*** O’Connor, RE AL, Ali, brady , WJ, Ghaemmaghami CA, Menon V, Welsford M, shuster M. . Part 9: acute coronary syndromes: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation
and Emergency Cardiovascular Care. Circulation 2015;132(suppl2):S483-S500
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
Cardiac Arrest *
Circular Algorithm
Shout for Help/Activate Emergency Response
Start CPR
Give Oxygen Attach Monitor/Defibrillator
2 minutes Return of Spontaneous
Circulation (ROSC)
Check Post-Cardiac
Rhythm Arrest Care
If VF/VT
Shock
Drug Therapy
IV/IO access
Epinephrine every 3–5 minutes
uous CPR
Amiodarone for refractory VF / VT
Continuous CPR
Consider Advanced Airway
Quantitative waveform capnography
Contin
Treat Reversible Causes
Mo
nitor y
CPR Qualit
Doses/Details for the Cardiac Arrest Algorithms
CPR Quality Return of Spontaneous Circulation(ROSC)
Push hard (2” to 2.4” or 5–6cm) and fast (100–120/min) and allow Pulse and blood pressure
complete chest recoil. Abrupt sustained increase in PETCO2 (typically ≥ 40 mm Hg)
Minimize interrruptions in compressions.**
Spontaneous arterial pressure waves with intra-arterial
Avoid excessive ventilation monitoring
Rotate compressor every 2 minutes
If no advanced airway, 30:2 compression-ventilation ratio
Quantative waveform capnography
If PETCO2<10mm Hg, attempt to improve CPR quality
Shock Energy
If relaxation phase(diastolic) pressure<20mm Hg,
attempt to improve CPR quality. Biphasic: Manufacturer recommendation (eg. initial dose of
120–200 J): if unknown, use maximum available.
Second and subsequent doses should be equivalent, and
Drug Therapy higher doses may be considered
Monophasic: 360 J
Epinephrine IV/IO Dose: 1 mg every 3–5 minutes
Amiodarone IV/IO Dose***: First dose: 300 mg bolus
Second dose: 150 mg Reversible Causes
Hypovolemia Tension pneumothorax
Advanced Airway**** Hypoxia Tamponade, cardiac
Supraglottic advanced airway or endotracheal intubation Hydrogen ion (acidosis) Toxins
Waveform capnography to confirm and monitor ET tube placement Hypo-/Hyperkalemia Thrombosis, pulmonary
10 breaths per minute with continuous chest compressions Hypothermia Thrombosis, coronary
* Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O’Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW. Part 7: adult advanced cardiac life support. 2015 American
Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015 132 (suppl 2):S444-S464
** Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, Richman PB Minimally Interrupted cardiac resuscitation by emergency medical services for out of hospital cardiac arrest. JAMA 2008;299:1158-1165
***Dorian P, Cass D, Schwartz B, Cooper R. Gelaznikas R, Barr A. Amiodarone as compared with Lidocaine for shock resistant ventricular fibrillation N Engl J Med 2002;346:884-890.
**** Dorges V, Wenzel V, Knacke P, Gerlach K, Comparison of different airway management strategies to ventilate apneic, nonpreoxygenated patients. Crit Care Med. 2003;31:800-804
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
Cardiac Arrest
Algorithm
Shout for Help/Activate Emergency Response
Start CPR
1 Give Oxygen
Attach Monitor/Defibrillator
2 VF/VT Rhyhm Shockable? Asystole/PEA 9
3 Shock*
CPR 2 min
Epi 1 amp iv, IV/IO access
4
CPR 2 min flush NaCl 20
cc, angkat
10 Epinephrine every 3–5 min
IV/IO access Consider advanced airway,
tangan capnography
Rhyhm Shockable?
12
Rhyhm Shockable?
5 Shock
If no signs of return of
spontaneous circulation
(ROSC), go to 10 or 11.
CPR 2 min
Epinephrine every 3-5 min CPR 2 min
6 Consider advanced airway, Treat reversible causes 11
capnography
If ROSC, go to Post-
Cardiac Arrest Care.
Rhyhm Shockable? Rhyhm Shockable?
7 Shock Pada pVT polimorfik
pertimbangkan MgSO4
CPR 2 min Amiodarone 300 mg bolus
Amiodarone 8 Dosis kedua 150 mg
Go to 5 or 7
Treat reversible causes
* Link MS, Atkins DL, Plassman RS, Halperin HR, SAmson RA, White RD, Cudnik MT, Berg MD, Kudenchuk PJ, Kerber RE. “Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing:
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation. 2010;122(suppl 3): S706-S719.
http://circ. ahajournals.org/content/122/18_suppl_3/S706
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
Bradycardia With
a Pulse Algorithm
Parameter : Assess appropriateness for clinical condition.
Nadi spontan Heart rate typically < 50/min if bradyarrhythmia.
Peningkatan udara di
capnografi
??
Parameter belum lengkap
Identify and treat underlying cause
Maintain patent airway; assist breathing as necessary*
Oxygen (if hypoxemic)
Cardiac monitor to identify rhythm; monitor blood pressure and oximetry
IV access
12–Lead ECG if available; don’t delay therapy
Persistent bradyarrhythmia causing:
Monitor Hypotension?
and Acutely altered mental status?
Signs of shock?
observe
Ischemic chest discomfort?
Acute heart failure?
Atropine IV Dose:
First dose: 0.5 mg bolus
Repeat every 3–5 minutes
Maximum: 3 mg
If atropine ineffective:
Transcutaneous pacing**
OR
Dopamine IV infusion:
2–10 mcg/kg per minute
OR
Epinephrine IV infusion:
2–10 mcg per minute
Consider:
Expert consultation
Transvenous pacing
* Dorges V, Wenzel V, Knacke P, Gerlach K, Comparison of different airway management strategies to ventilate apneic, nonpreoxygenated patients. Crit Care Med. 2003;31:800-804
** Link MS, Atkins DL, Passman RS, Halperin HR, Samson RA, White RD, Cudnik MT, Berg MD, Kudenchuk PJ, Kerber RE. “Part 6: electrical therapies: automated external defibrillators, defillation, cardioversion, and pacing:
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation. 2010; 122(suppl 3):S706-S719. http://circ.ahajournals.org/content/122/18_suppl_3/S706
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
Immediate Post-Cardiac
Arrest Care Algorithm
Return of Spontaneous Circulation (ROSC)*
Optimize Ventilation and
Oxygenation Treat Hypotension (SBP < 90 mm Hg)
Maintain oxygen saturation 94% IV/IO bolus
Consider advanced airway Vasopressor infusion
waveform capnography Consider treatable causes
Do not hyperventilate 12-Lead ECG
Follow Commands ?
Induced Hypothermia**
Cardiac Catheterization Laboratory
Advanced Critical Care
Doses/Details Epinephrine IV Dopamine IV
Infusion Infusion
0.1–0.5 mcg/kg per minute 2–10 mcg/kg per minute
Ventilation/Oxygenation (in 70-kg adult: 7-35 mcg
per minute)
Avoid excessive ventilation Norepinephrine
Start at 10 94% breaths/min IV Infusion
and titrate to target PETCO2 Reversible Causes
of 35–40 mm Hg.
When feasible, titrate FIO2 0.1–0.5 mcg/kg per minute
to minimum necessary to Hypovolemia (in 70–kg adult: 7–35mcg
achieve SpO2 ≥ 94%. Hypoxia per minute)
Hydrogen ion (acidosis)
Hypo-/Hyperkalemia
IV Bolus Hypothermia
Tension pneumothorax
1–2 L normal saline or Tamponade, cardiac
lactated Ringer’s. Toxins
If inducing hypothermia, Thrombosis, pulmonary
may use 4°C fluid. Thrombosis, coronary
* Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out of hospital cardiac arrest: a systematic review and metanalysis Circ Cardiovasc Qual Outcomes. 2010;3:63-81.
** Bruel C, Parienti JJ, Marie W, Arrot X, Mild hypothermia during advanced life support, a preliminary study in out of hospital cardiac arrest. Crit Care. 2008;12: R31
*** Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, Meurer WJ, Peberdy MA, Thompson TM, Zimmerman JL. Part 8: post-cardiac arrest care: 2015 American Heart Association
Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132(suppl2):S465-S482
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
Stroke Assessment
The Cincinnati Prehospital Stroke Scale
Facial Droop
(have patient show teeth or smile)
NORMAL ABNORMAL
Both sides of face move equally. One side of face does not move
as well as the other side.
Arm Drift
(patient closes eyes and extends both arms straight out, with palms up for 10 seconds)
NORMAL ABNORMAL
Both arms move the same or both One arm does not move or one
arms do not move at all. arm drifts down compared
with the other.
Abnormal Speech
(have the patient say “you can’t teach an old dog new tricks”)
Normal - Patient uses correct Abnormal - Patient slurs
words with no slurring. words, uses the wrong words,
or is unable to speak.
If any 1 of these 3 signs is abnormal, the probability of a stroke is 72%
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
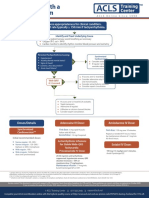
Suspected Stroke Algorithm:
Goals for Management of Stroke
Identify Signs and Symptoms of Possible Stroke
Active Emergency Response
Critical EMS assessments and actions
Support ABCs: Establish time of
Perform prehospital Triage to Activate stroke
Give Oxygen Check glucose symptom onset Alert hospital
stroke assessment stroke center team
if indicated (last normal)
NINDS TIME GOALS
If onset >3 hours consider triage to hospital
with interventional capabilities for stroke.
Immediate general assessment and stabilization* Immediate neurologic assessment by stroke team
or designee
Assess ABCs, vital signs
Provide oxygen if O sat <94%
2
Obtain IV access and perform laboratory Review patient history
assessments Establish time of symptom onset or last
Check glucose; treat if indicated known normal
Obtain 12–lead ECG Perform neurologic examination (NIH Stroke
Scale or Canadian Neurological Scale)
Perform neurologic screening assessment
Order emergent CT without contrast
Does CT Scan Show Hemorrhage?
No hemorrhage Hemorrhage
Probably acute ischemic stroke; Consult neurologist or neurosurgeon;
consider fibrinolytic therapy consider transfer if not available.
Check fibrinolytic exclusions
Repeat neurologic exam: are deficits Begin stroke or hemorrhage
rapidly improving to normal? pathway
Admit to stroke unit or
intensive care unit
Patient remains candidate Not a candidate
for fibrinolytic therapy? Administer aspirin
Candidate*
Begin post-rTPA stroke pathway
Review risks/benefits with patient & family. Aggressively monitor:
If acceptable: BP per protocol
Give rTPA** For neurologic deterioration
No anticoagulants or antiplatelet Emergent admission to stroke
treatment for 24 hours unit or intensive care unit
* Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan Y-F, Gentile N, Hazinski MF. “ Part 11: adult stroke: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitationand Emergency Cardiovascular
Care” . Circulation. 2010;122(suppl 3):S818-S828. http://circ.ahajournals.org/content/122/18_suppl_3/S818
** Tissue Plasminogen Activator for Acute Ischemic Stroke. N Engl J Med. 1995:333(24)1581-1587
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
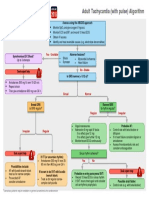
Tachycardia With a
Pulse Algorithm
Assess appropriateness for clinical condition.
Heart rate typically ≥ 150/min if tachyarrhythmia.
Identify and Treat Underlying Cause
Maintain patient airway; assist breathing as necessary
Oxygen (if O2 sat < 94%)
Cardiac monitor to identify rhythm; monitor blood pressure and oximetry
Persistent Tachyarrhythmia Causing:
Synchronized
Hypotension? Cardioversion*
Acutely altered mental status? Consider sedation
Signs of shock? If regular narrow complex,
Ischemic chest discomfort? consider adenosine
Acute heart failure?
IV access and 12–lead ECG if available.
Consider adenosine only if regular
Wide QRS? and monomorphic.
0.12 second Consider antiarrhythmic infusion.
Consider expert consultation.
B bloker di Indonesia
injeksi hanya
metoprolol Kalau adenosine
(vapressor)
CCB bisa dengan IV access and 12–lead ECG if available. tidak ada bisa
diltiazem inj 15-20 Vagal maneuvers. diganti ATP
mg, 15 mnt lagi 20-25, Adenosine (if regular) dengan dosis 2x
rumatan 5-15 mg/jam β-Blocker or calcium channel blocker. lipat
Consider expert consultation.
Doses/Details Adenosine IV Dose: Amiodarone IV Dose:
Synchronized First dose : 6 mg rapid IV push; First dose : 150 mg over 10 minutes.
Cardioversion** follow with NS flush.
Repeat as needed if VT recurs. Follow
Second dose : 12 mg if required by maintenance infusion of 1 mg/min
Initial recommended doses: for first 6 hours.
Narrow regular : 50–100 J Antiarrhythmic Infusions
Narrow irregular : 120–200 J for Stable Wide-QRS Sotalol IV Dose:
biphasic or 200 J monophasic Tachycardia
Wide regular : 100 J
Wide irregular : Defibrillation
Procainamide IV Dose: 100 mg (1.5 mg/kg) over 5 minutes.
Avoid if prolonged QT.
dose (not synchronized)
20-50 mg/min until arrhythmia
suppressed, hypotension ensues, QRS
TDP termasuk wide iregular duration increases > 50% or
maximum dose 17 mg/kg given.
Maintenance infusion: 1–4 mg/min.
Avoid if prolonged QT or CHF.
* Link MS, Atkins DL, Passman RS, Halperin HR, SAmson RA, White RD, Cudnik MT, Berg MD, Kudenchuk PJ, Kerbenchuk PJ, Kerber RE. “Part 6: electrical therapies: automated external defibrillators,
defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation. 2010;122(suppl 3):
S706-S719. http://circ.ahajournals.org/content/122/18_suppl_3/S706
** Scholten M, Szili-Torok T, Klootwijk P, Jordaens L, Comparison of monophasic and biphasic shocks for transthoracic cardioversion of atrial fibrillation. Heart 2003;89:1032-1034
Version control: This document is current with respect to 2015 American Heart Association Guidelines for CPR and ECC. These guidelines are current until they are replaced on October 2020.
If you are reading this page after October 2020, please contact ACLS Training Center at support@acls.net for an updated document. Version 2016.02.a
© ACLS Training Center 877-560-2940 support@acls.net
Complete your ACLS recertification online with the highest quality course at http://www.acls.net and use promo code PDF2016 during checkout for 15% off.
You might also like
- Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionDocument1 pageSyndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionAnonymous CKAborxxwNo ratings yet
- ACLS Advanced Cardiovascular Life Support Provider Manual 2023From EverandACLS Advanced Cardiovascular Life Support Provider Manual 2023No ratings yet
- Acut Coronary SyndromesDocument1 pageAcut Coronary SyndromesMuhittin Selçuk ÖzkanNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFJim Christian EllaserNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFNety Pandung SalembanNo ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationIGOR SHEYNINNo ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital Preparationgusti angri angalanNo ratings yet
- Posters For ClinicDocument80 pagesPosters For ClinicdenzkissaieNo ratings yet
- Acute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or InfarctionDocument1 pageAcute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or Infarctionjohndoe1995No ratings yet
- Acs PDFDocument1 pageAcs PDFPowool LalaNo ratings yet
- Reanimacion CardiopulmonarDocument15 pagesReanimacion CardiopulmonarVictoriano ValienteNo ratings yet
- Algorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSDocument6 pagesAlgorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSNenyNo ratings yet
- Emergency Department STEMI Algorithm GuideDocument1 pageEmergency Department STEMI Algorithm GuideOgizWaraNo ratings yet
- Tachycardia AlgorithmDocument1 pageTachycardia AlgorithmGideon BahuleNo ratings yet
- Tachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDocument1 pageTachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDendy Frannuzul RamadhanNo ratings yet
- AlgorithmACLStachycardiawithapulse PDFDocument1 pageAlgorithmACLStachycardiawithapulse PDFDendy Frannuzul RamadhanNo ratings yet
- Stemi NSTEMI or Unstable Angina: Offer AspirinDocument1 pageStemi NSTEMI or Unstable Angina: Offer AspirinVemuri SrinivasNo ratings yet
- Pediatric Bradycardia With A Pulse and Poor Perfusion AlgorithmDocument1 pagePediatric Bradycardia With A Pulse and Poor Perfusion AlgorithmRadhiatul MardhiahNo ratings yet
- ACLS Simplify AlgorithmDocument6 pagesACLS Simplify AlgorithmKristine Monforte Coma UritaNo ratings yet
- ACLS ReportDocument58 pagesACLS ReportCamille Honeyleith FernandoNo ratings yet
- EMS Chest Pain ACS GuidelinesDocument1 pageEMS Chest Pain ACS GuidelinesJuanaly BadiolaNo ratings yet
- Adult Tachycardia (With Pulse) AlgorithmDocument1 pageAdult Tachycardia (With Pulse) AlgorithmJames ChoiNo ratings yet
- Algoritma Ambulance - PHCDocument11 pagesAlgoritma Ambulance - PHCYassarNo ratings yet
- UNC ED Code Stroke Pathway 9 2016 FINALDocument2 pagesUNC ED Code Stroke Pathway 9 2016 FINALJackNo ratings yet
- Assess Appropriateness For Clinical Condition. Heart Rate Typically 150/min If TachyarrhythmiaDocument1 pageAssess Appropriateness For Clinical Condition. Heart Rate Typically 150/min If TachyarrhythmiaSiti Nur R Firda FauziyahNo ratings yet
- Peri-Arrest ArrythmiaDocument14 pagesPeri-Arrest Arrythmiamohamed mowafeyNo ratings yet
- Algorithm of Resuscitation CareDocument1 pageAlgorithm of Resuscitation CarejyothiNo ratings yet
- AiepiDocument12 pagesAiepiRenzo Iván Marín DávalosNo ratings yet
- ACLS 2015 Algorithm and Anesthesia ACLS PDFDocument14 pagesACLS 2015 Algorithm and Anesthesia ACLS PDFTaufiqurrahman RizkiNo ratings yet
- Algo ArrestDocument2 pagesAlgo ArrestLocomotorica FK UkiNo ratings yet
- ACS Algorithm 2016 PDFDocument1 pageACS Algorithm 2016 PDFrabin1994No ratings yet
- AlgorithmACLS Tachycardia 200612Document1 pageAlgorithmACLS Tachycardia 200612YassarNo ratings yet
- Acute Coronary SyndromeDocument7 pagesAcute Coronary SyndromePuskesmas Pinang JayaNo ratings yet
- Acute Coronary SyndromeDocument5 pagesAcute Coronary Syndromecotten joeNo ratings yet
- ACLS ACS Algorithm NewDocument3 pagesACLS ACS Algorithm Newsambo100% (1)
- Cardiac Arrest Circular AlgorithmDocument2 pagesCardiac Arrest Circular AlgorithmJunius SimarmataNo ratings yet
- Ecg ReadingsDocument11 pagesEcg ReadingsAnton Laurenciana100% (5)
- AdultTachycardiaWithPulse AlgorithmDocument1 pageAdultTachycardiaWithPulse AlgorithmIsmail SlimNo ratings yet
- Acute Coronary Syndromes - HandoutDocument4 pagesAcute Coronary Syndromes - Handoutapi-641524095No ratings yet
- Advanced Life Support Algorithm: Learning OutcomesDocument8 pagesAdvanced Life Support Algorithm: Learning OutcomesParvathy R NairNo ratings yet
- Inpatientpathway PDFDocument2 pagesInpatientpathway PDFLuis Fernando SaraviaNo ratings yet
- Start CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorDocument2 pagesStart CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorFelicia ErikaNo ratings yet
- G2015 Adult Tachycardia PDFDocument1 pageG2015 Adult Tachycardia PDFibbs91No ratings yet
- G2015 Adult Tachycardia PDFDocument1 pageG2015 Adult Tachycardia PDFPlabber JuneNo ratings yet
- Acs With New Stemi GuidelineDocument35 pagesAcs With New Stemi Guidelinematmin07No ratings yet
- Algorithm-ACLS ACS 200806 1Document1 pageAlgorithm-ACLS ACS 200806 1Kavya Shree100% (1)
- Algo Tachycardia PDFDocument1 pageAlgo Tachycardia PDFYudhistira AdiNo ratings yet
- Chest Pain System - DisorderDocument1 pageChest Pain System - DisorderAA DDNo ratings yet
- Onlinemeded Notes CardioDocument1 pageOnlinemeded Notes CardioCourtney HolbrookNo ratings yet
- Nursing CS Treatment-Of-Atrial-Dysrhythmias 02Document1 pageNursing CS Treatment-Of-Atrial-Dysrhythmias 02frankshro156No ratings yet
- Cardiac Arrest Circular AlgorhythmDocument4 pagesCardiac Arrest Circular AlgorhythmAisyah Nur KarimahNo ratings yet
- Diagnosis and Initial Treatment of Ischemic Stroke: Health Care GuidelineDocument62 pagesDiagnosis and Initial Treatment of Ischemic Stroke: Health Care GuidelineIrsyah Dwi RNo ratings yet
- Diagnosis and Initial Treatment of Ischemic Stroke: Health Care GuidelineDocument71 pagesDiagnosis and Initial Treatment of Ischemic Stroke: Health Care GuidelineRosyid PrasetyoNo ratings yet
- AngiographyDocument15 pagesAngiographyCrystal AdnalacNo ratings yet
- Jyane ReubenDocument35 pagesJyane ReubenAmr El-RefaeyNo ratings yet
- Nursing Lesson Plan on Pre-EclampsiaDocument13 pagesNursing Lesson Plan on Pre-EclampsiaSheena SharmaNo ratings yet
- Cardiovascular - Anatomy & PhysiologyDocument23 pagesCardiovascular - Anatomy & PhysiologySanthoshi Sadhanaa Sankar100% (1)
- Pedia Notes Print2Document5 pagesPedia Notes Print2John Christopher LucesNo ratings yet
- 2002 Sung-Gyu Lee - Adult-To-Adult LDLT at ASAN Medical CenterDocument8 pages2002 Sung-Gyu Lee - Adult-To-Adult LDLT at ASAN Medical CenterPhu PhamHongNo ratings yet
- GAS EXCHANGE AND THE RESPIRATORY SYSTEMDocument7 pagesGAS EXCHANGE AND THE RESPIRATORY SYSTEMChenul WickramasingheNo ratings yet
- The PancreasDocument31 pagesThe PancreasAryan DesaiNo ratings yet
- The Effect of Cilostazol On Right Heart FunctionDocument43 pagesThe Effect of Cilostazol On Right Heart FunctionGunawan YogaNo ratings yet
- Grand Rounds PresentationDocument40 pagesGrand Rounds Presentationapi-610941700No ratings yet
- Animaltissues 180604115637Document40 pagesAnimaltissues 180604115637proud.student2023No ratings yet
- Certified Ecg Tchnician Syllabus 2021Document5 pagesCertified Ecg Tchnician Syllabus 2021Whiteboard DiscoveryNo ratings yet
- NUR 146 MCN2 RLE P2 ExamDocument22 pagesNUR 146 MCN2 RLE P2 ExamMarga WreatheNo ratings yet
- Management of Splenic Injury in The Adult Trauma PatientDocument17 pagesManagement of Splenic Injury in The Adult Trauma PatientArnaldo Santizo SáenzNo ratings yet
- Hypertensive Heart DiseaseDocument13 pagesHypertensive Heart Diseasemariephynn100% (1)
- Lymphatic SystemDocument3 pagesLymphatic Systempierre TritzNo ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyChrischia Yvonne GualbertoNo ratings yet
- Serial Comparison Algorithm ReferenceDocument28 pagesSerial Comparison Algorithm ReferenceHoàng Anh NguyễnNo ratings yet
- The Cardiovascular System: Gerard Mark C. SantosDocument31 pagesThe Cardiovascular System: Gerard Mark C. SantosRamon T. De Vera100% (1)
- CONCEPT - QuestionsDocument2 pagesCONCEPT - Questionsgreen_archerNo ratings yet
- Contoh Soal FetomaternalDocument10 pagesContoh Soal FetomaternalBella AgustinNo ratings yet
- Unstable Angina PectorisDocument34 pagesUnstable Angina PectoriserinmowokaNo ratings yet
- Circulatory System PPT 1Document47 pagesCirculatory System PPT 1Czarae VillanuevaNo ratings yet
- Magdy El-Masry Prof. of Cardiology Tanta UniversityDocument55 pagesMagdy El-Masry Prof. of Cardiology Tanta UniversityPrabJot SinGhNo ratings yet
- Cardiotonics & Inotropic Drugs PDFDocument10 pagesCardiotonics & Inotropic Drugs PDFZehra AmirNo ratings yet
- Underwriting Cheat Sheet For WMDocument106 pagesUnderwriting Cheat Sheet For WMAleah DatukonNo ratings yet
- SIRSDocument8 pagesSIRSʕ•ᴥ•ʔNo ratings yet
- Obs JauDocument22 pagesObs JauRavi GuptaNo ratings yet
- Hemolytic Anemia IntrinsicDocument14 pagesHemolytic Anemia IntrinsicSophia Gail ChingNo ratings yet
- Centrimag Pre-Connected PackDocument17 pagesCentrimag Pre-Connected PackShuhengNo ratings yet