Professional Documents
Culture Documents
Fiorella2005 PDF
Uploaded by
alecsaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fiorella2005 PDF
Uploaded by
alecsaCopyright:
Available Formats
The Laryngoscope
Lippincott Williams & Wilkins, Inc.
© 2005 The American Laryngological,
Rhinological and Otological Society, Inc.
Outcome of Septal Dermoplasty
in Patients With Hereditary
Hemorrhagic Telangiectasia
Maria Luisa Fiorella, MD; Douglas Ross, MD; Katharine J. Henderson, MS; Robert I. White, Jr., MD
Objectives/Hypothesis: Septal dermoplasty has 7 (10%) had symptomatic liver disease, and 5 (7%) had
been recommended as the treatment of choice for life- cerebral arteriovenous malformation. During the
threatening epistaxis in patients with hereditary follow-up, 14 patients died of other complications of he-
hemorrhagic telangiectasia. The purpose of the study reditary hemorrhagic telangiectasia (11 patients) and
was to evaluate the effectiveness and outcomes of unrelated causes (3 patients). Conclusion: Septal dermo-
septal dermoplasty for management of transfusion- plasty remains an effective way of reducing transfusion
dependent epistaxis. Study Design: Retrospective requirements in patients with hereditary hemorrhagic
study. Methods: Between 1994 and 2004, septal dermo- telangiectasia and subjectively improves their quality
plasty was performed on 67 consecutive patients with of life. The otolaryngologist caring for patients with he-
severe epistaxis attributable to hereditary hemor- reditary hemorrhagic telangiectasia should be familiar
rhagic telangiectasia. The numbers of units of blood with other organ involvement by hereditary hemor-
received 1 year before and 1 year after septal dermo- rhagic telangiectasia to prevent complications during
plasty were obtained. A subjective appraisal of the surgery. Key Words: Septal dermoplasty, epistaxis, he-
results of the surgery as well as second procedures reditary hemorrhagic telangiectasia.
after septal dermoplasty was determined. Patients Laryngoscope, 115:301–305, 2005
were screened for pulmonary and cerebral arterio-
venous malformations, gastrointestinal tract bleed-
INTRODUCTION
ing, and symptomatic liver disease. Results: Data
were obtained in 66 of 67 (98%) patients with a mean Hereditary hemorrhagic telangiectasia (HHT) is an
age of 61.5 years (mean follow-up, 3.9 y). Accurate uncommon systemic autosomal dominant disorder of an-
transfusion requirements 1 year before and 1 year giogenesis characterized by the presence of vascular tel-
after septal dermoplasty were available in 32 of 66 angiectases in mucocutaneous tissues, visceral organs,
(48%) patients. In these 32 patients, the mean units of and the central nervous system.1 Epistaxis, caused by
blood received decreased from 21 units (range, 2–100 spontaneous bleeding from telangiectases of the nasal mu-
units) 1 year before septal dermoplasty to 1 unit cosa, is the most common manifestation of HHT. It may be
(range, 0 –10 units) in the year after septal dermo- so severe as to require multiple transfusions and intrave-
plasty (P < .001). Improved quality of life was claimed nous iron supplementation. Bleeding becomes more severe
in 57 patients. Second therapies, ranging from cau-
in later decades in approximately two-thirds of affected
tery to repeat partial septal dermoplasty, were re-
quired in 15 patients during follow-up. Among the 67 persons.2 Although nasal manifestations of HHT are well
patients, 31 (46%) had pulmonary arteriovenous mal- known to otolaryngologists, many of the other organ man-
formation, 14 (21%) had gastrointestinal tract bleeding, ifestations of this disorder are less well known and may
pose issues for the physician treating the patient with
HHT.
From the Department of Otolaryngology (M.L.F.) Universita‘ degli
Studi di Bari, Bari, Italy; and the Sections of Otolaryngology (D.R.), De- Mild and moderate epistaxis is treated by hormonal
partment of Surgery, and Interventional Radiology (K.J.H., R.I.W.), Depart- therapy with estrogens,3 chemical cautery and electrocau-
ment of Diagnostic Radiology, Yale University School of Medicine, New tery, and laser coagulation.4 Life-threatening epistaxis,
Haven, Connecticut, U.S.A.
Supported in part by March of Dimes grant HHT-FY04 – 677 and
which is associated with HHT, has been treated with
Josephine Lawrence Hopkins Foundation and General Clinical Research varying success using embolization,5 surgical ligation,6
Center NIH M01-RR-00125 grant (R.I.W. and K.J.H.). Young’s surgical closure of the nostrils by a skin flap,7 and
Editor’s Note: This Manuscript was accepted for publication August microvascular free flaps.8
3, 2004.
Send Correspondence to Douglas Ross, MD, Section of Otolaryngol-
William Saunders pioneered a skin grafting tech-
ogy, Department of Surgery, Yale University School of Medicine, Yale nique for severe epistaxis in 1958; since then, this tech-
Physician’s Building, 4th Floor, 800 Howard Avenue, New Haven, Con- nique has undergone modification.9 The principle of this
necticut 06519, U.S.A. E-mail: douglas.ross@yale.edu
procedure is to replace the fragile respiratory mucosa of
DOI: 10.1097/01.mlg.0000154754.39797.43 the nose with strong keratinized split-thickness skin
Laryngoscope 115: February 2005 Fiorella et al.: Outcome of Septal Dermoplasty
301
grafts from the thigh that resist trauma and thereby pre-
vent bleeding.10
Since the early 1990s, the senior otolaryngologist
(D.R.) has used the Saunders method of septal dermoplasty
(SD), with his own modifications, to control transfusion-
dependent epistaxis.11 The purposes of the present study
were to describe indications and new variations of SD, to
characterize the phenotype of patients requiring this ther-
apy, and to report the long-term outcome of SD.
PATIENTS AND METHODS
The Yale Arteriovenous Malformation Center is an interdis-
ciplinary center of physicians caring for patients with HHT. From
a population of approximately 250 patients seen yearly, 67 con-
secutive patients with severe, debilitating epistaxis were referred
to the otolaryngologist and underwent SD. Human Investigations
Committee approval was obtained for a retrospective study that
included contacting all patients, as well as their primary care
physicians. Detailed information about total transfusions (units
of blood) 1 year before and 1 year after SD was requested. A
subjective appraisal of the results of the surgery was asked of the
patients and their families. Second therapies for control of nose-
bleeds after SD were also tabulated. Patients in the present study
were seen by the genetic counselor and senior physician in the
center and screened for pulmonary and cerebral arteriovenous
malformations12,13 and symptomatic liver disease.14
Surgical Technique
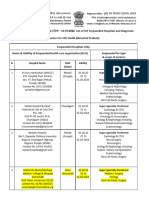
Surgical technique is shown in Figures 1 and 2. With the
patient under general endotracheal anesthesia, a 3 ⫻ 7-inch
split-thickness graft is taken from the lateral aspect of the right-
side thigh, using a Zimmer air dermatome on a setting of
141000of an inch. Xeroform and Telfa with Kerlex-wrapped
dressing are applied on completion of harvesting of the skin and
the graft, which is preserved in a saline-soaked sponge.
Bilateral inferior turbinectomies are performed in the fol-
lowing manner. Neo-Synephrine is placed into the nose for ade-
quate vasoconstriction; then the inferior turbinates are infil-
trated with 1% lidocaine and 1:100,000 epinephrine. The
turbinate is medialized and removed at its base using an anterior
straight scissor under endoscopic view, cutting anteroposteriorly,
as much as possible toward the lateral nasal wall. The free edge of
the remnant of the turbinate is then cut down using microderider. Fig. 1. (A and B) Sagittal views. (A) Nasal mucosa is removed with
a Faulkner curette (lateral wall). The nasal mucosa is resected, and
Meticulous hemostasis is achieved using Bovie electrocautery.
an inferior turbinectomy is performed. (B) The graft has been su-
The septal dermoplasty is performed. The nasal vestibule is tured anteriorly and applied to lateral wall.
injected with 1% lidocaine and 1:100,000 epinephrine. After 7
minutes a narrow circumferential strip of vestibular skin is ex-
cised from the septum and the floor and from the lateral wall of
both nostrils at the mucocutaneous junction. As much mucosa as 0.5 ⫻ 3-cm Neuropatties treated with mupirocin calcium oint-
possible is removed using a Faulkner curette, taking care to ment (Bactroban, Galaxo Smith Kline, Philadelphia, PA) are used
preserve the perichondrium of the septum that must nourish the for this task. The first pack is placed along the floor of the nose to
new grafts and the septal cartilage. anchor the graft inferiorly; then a second piece is placed superi-
Bleeding is controlled by the topical application of cotton orly, continuing in this alternate fashion until the nose is packed
soaked in epinephrine in one nostril and continuing the operation firmly. Packing is removed only after 5 days, when the grafts are
in the opposite side. Once the bleeding has slowed, the curetting well attached.
is continued until one is assured of adequate removal of mucosa. There is often “temporary” nasal obstruction after the packs
The skin graft is sutured in a U shape. A stitch is placed at are removed, because of excess skin at the posterior part of the
the inferior aspect of the rim incision with interrupted 3-0 chro- nose. This acts as an avascular small flap that eventually disin-
mic suture, and the skin graft is sutured circumferentially tegrates. When this occurs, the nasal airways improve.
around the rim incision of the nasal vestibule. The skin graft is
then inserted into the nose with a No. 2 bayonet forceps, and a Follow-Up Care
long nasal speculum is used to hold it in place for packing. Nothing more is performed for 10 to 14 days after surgery so
that the skin graft can become firmly attached to the nasal walls.
Packing and Removal During follow-up, cautious suctioning of crusts is performed to
An important aspect is careful nose packing, to avoid the facilitate breathing and success of graft take. Skin is not meant to
displacement of the skin graft while healing takes place. Multiple be in the nose, and crusting from desquamation frequently devel-
Laryngoscope 115: February 2005 Fiorella et al.: Outcome of Septal Dermoplasty
302
TABLE II.
Transfusion Requirements Before and After Septal Dermoplasty.
No. of patients requiring blood transfusion before SD 38
No. of patients requiring blood transfusion after SD 11
No. of units of blood received before SD*
Mean 21
Range 2–100
No. of units of blood received after SD*
Mean 1
Range 0–10
*Data from 32 patients with accurate determination of blood before and
after septal dermoplasty (SD).
Wilcoxon signed rank test, P ⬍ .001.
Fig. 2. (A and B) Coronal views. In 2002, we began performing
routine turbinectomies followed by mucosal resection. (A) The ex- Transfusion Requirements and
tent of mucosal resection before (right side) and after (left side) the Quality-of-Life Outcomes
introduction of turbinectomies is evident. (B) The extent of skin graft Thirty-eight of the 50 patients required blood trans-
and packing placement both before (right side) and after (left side)
the introduction of turbinectomies are evident.
fusions before SD, and 11 required them after SD (Table
II). In 32 patients we were able to determine the exact
number of units of blood received before and after SD. In
these 32 patients, the mean units of blood received de-
ops, requiring that the patient provide vigorous nasal hygiene. creased from 21 units in the year before SD (range, 2–100
Crusting may lead to nasal obstruction and odor; therefore, the units) to 1 unit (range, 0 –10 units) during the year after
nose must be cleaned once or twice daily. Cleaning is facilitated SD. The Wilcoxon signed rank test demonstrated a signif-
using cotton-tipped applicators and moisturizing substances such icant decrease in the number of transfusions in these
as mineral oil, Borofax ointment, half hydrogen peroxide and half
patients (P ⬍ .001).
water, or soap and water. Saline irrigations can also be used. This
We were able to question 57 patients or families of
cleaning cannot injure the skin, and it cannot be scraped off.
patients about quality of life: 53 reported that their qual-
ity of life had improved after SD, and 4 reported no im-
RESULTS
provement. Twenty-four of the 57 patients (42%) reported
Between 1994 and 2004, SD was performed in 67
no epistaxis (mean follow-up, 2 y [range, 2 mo– 8 y]); 29
patients (30 men and 37 women) (Table I). Data were
patients (51%) reported decreased frequency and duration
obtained in 66 of 67 patients (98%). The mean age at the
of epistaxis (mean follow-up, 2 y, 9 mo [range, 1 mo– 8 y]),
time of SD was 61.5 years (age range, 35– 80 y). Transfu-
and 4 patients (7%) had not improved since surgery (Table
sion requirements either before or after SD were available
II).
in 50 of 67 patients (75%). Complete data before and after
SD were available in 32 of 66 patients (48%) of this group.
Table II In 66 of 67 patients (98%), the mean follow-up
Clinical Phenotype
period was 3.9 years (range, 2 mo–9.8 y). Quality-of-life
Other organ involvement. Pulmonary arterio-
information was available for all living patients and from
venous malformations were present in 31 of 66 patients
their families for patients who had died.
(47%), and cerebral arteriovenous malformations were
found in 5 of 66 patients (7%). Symptomatic liver disease
was present in 7 of 66 patients (10%) (Table I). In addition,
14 patients (21%) had gastrointestinal tract bleeding be-
TABLE I.
Clinical Phenotypes in 67 Patients Undergoing
fore or after SD. Two patients had a prosthetic heart valve
Septal Dermoplasty. and tolerated coumadin well after SD.
Deaths during follow-up. Fourteen of 66 patients
Male n ⫽ 30
(21%) died during the follow-up after SD. Five of these
Female n ⫽ 37 patients had gastrointestinal tract bleeding but died of
Age (y) heart disease.
Mean 61 In 3 of 14 patients, death was attributed to pulmo-
Range 35–80 nary hypertension associated with HHT. Liver disease
Other organ: n (%) and intractable congestive heart failure were the causes of
Pulmonary arteriovenous malformation 31 (46%) death in 2 of 14 patients, respectively, and bleeding from
Cerebral arteriovenous malformation 5 (7%) esophageal varices (1 of 14 patients) accounted for the
Gastrointestinal tract bleeding 14 (21%) additional death in this group. Three of 14 patients died of
Symptomatic liver disease 7 (10%)
colon cancer, pancreatitis and pneumonia, and lung can-
cer, respectively.
Laryngoscope 115: February 2005 Fiorella et al.: Outcome of Septal Dermoplasty
303
Second therapies after septal dermoplasty. tial graft take and have received adjunctive therapy at 1
Multiple additional therapies have been performed in year, we currently recommend that all patients be seen 1
15 patients (laser therapy in 10 patients, a second SD in 6, year after surgery. Management of recurrent epistaxis by
embolization in 2, and maxillary artery ligation in 1 pa- laser or second partial SD is able to extend the time of
tient). Many of these therapies were performed at other improvement and emphasizes the importance of follow-up
institutions because some of the patients did not return to by the otolaryngologist performing the SD.
our center for follow-up.
DISCUSSION Importance of Phenotype
Many patients in the present series have had other
Technique History and Modifications serious organ involvement, which ultimately contributes
Since the early 1960s, surgical techniques for man- to their disability and mortality. Symptoms such as dys-
aging debilitating nosebleeds in HHT patients have pnea, fatigue, and congestive heart failure can be mani-
evolved, but epistaxis of this magnitude is still problem- festations of pulmonary arteriovenous malformations, he-
atic. Many authors have proposed alternative procedures patic arteriovenous malformations, gastrointestinal tract
including laser cauterization, embolization, maxillary ar- bleeding, and iron deficiency anemia or some combination
tery ligation, Young’s procedure, and microvascular free of all of theses.15 In addition, in patients with pulmonary
flaps. Although each method has advocates in these pa- arteriovenous malformations, the lung no longer has a
tients, no method has provided a complete cessation of capillary filter, and small blood clots, bacteria, and, occa-
epistaxis, and reporting of long-term outcomes in these sionally, air can pass directly through the pulmonary ar-
patients has been limited. teriovenous malformation into the systemic circulation,
Currently, the most credible technique is septal der- causing ischemic events in various organs.1 Intracerebral
moplasty, first described by Saunders9 in 1958. Replace- hemorrhages may also occur as a result of cerebral or
ment of the fragile nasal mucosa with a skin-thickness spinal arteriovenous malformations.1 In our study, three
graft from the thigh renders the nose more resistant to patients had primary pulmonary hypertension, which is a
trauma without altering the nasal respiratory function. syndrome newly recognized in HHT.16
However, good result of SD depends not only on quantity Patients with a history of pulmonary arteriovenous
of mucosa covered by the skin graft but also on the malformations are prone to air or clot emboli during in-
follow-up care. Skin graft desquamation produces odor travenous infusions. Antibiotics should be given prophy-
and crusting; therefore, daily cleaning is necessary to lactically for procedures. In most instances, the otolaryn-
avoid nasal obstruction and nose bleedings. gologist is the first physician to see a patient with HHT
Presence of telangiectases in nasal mucosa not cov- because epistaxis is the most common symptom.5 First-visit
ered by the graft, as well as graft contracture, can cause patients should be screened for other organ involvement.
postoperative epistaxis, which is treatable by laser tech- Although imperfect, the modified Saunders dermo-
nique. Septal dermoplasty may be repeated in patients plasty, coupled with follow-up care at 1 year and in sub-
with recurrent severe epistaxis. Modification of the tech- sequent years, is the best therapy for this subset of pa-
nique has been performed recently to facilitate the skin tients. In the near future, many new pharmacological
graft positioning, cleaning, and maintenance of airway by agents, with anti-angiogenesis properties will be devel-
inferior bilateral turbinectomies.11 Septectomy has been oped and, perhaps, may offer a possible nonsurgical solu-
useful for one patient with profuse nosebleeds and septal tion; However, until that time, SD that is specific for HHT
perforation. should be the mainstay for transfusion-dependent epistaxis.
Outcomes
Our study is a large retrospective review of patients CONCLUSION
with severe epistaxis attributable to HHT that was The modified SD for transfusion-dependent epistaxis
treated by SD. To date, the data on SD reported in the in patients with HHT provides excellent palliation and
literature have been based on a small number of patients improves quality of life. The need for transfusions was
and the duration of follow-up has been short. Our out- significantly reduced in the subset of 32 patients with
comes are longer than previously reported and are based accurate blood transfusion records 1 year before and 1
on transfusion requirements before and after SD, as well year after SD. All patients with HHT who are undergoing
as subjective questioning of the patient or family. Cessa- SD should be seen 1 year after SD because in as many as
tion or marked reduction of epistaxis occurs in 90% of 25% of patients, laser or other secondary procedures will
patients with HHT during the first 2 years after SD. Four be necessary. The otolaryngologist treating patients with
patients did not benefit from SD. Our clinical experience HHT should be aware of other organ manifestations,
has demonstrated that, beyond the obvious health dam- which may influence management of the patient during
age, epistaxis of this magnitude seriously affects the qual- and after SD.
ity of life of the patient with HHT.
Limitations of our study include the retrospective
design and the recall bias associated with the quality-of- Acknowledgment
life assessment. Because some of our patients developed The authors thank James Dziura for his assistance
repeat bleeding attributable to new telangiectases or par- with data analysis.
Laryngoscope 115: February 2005 Fiorella et al.: Outcome of Septal Dermoplasty
304
BIBLIOGRAPHY caused by hereditary hemorrhagic telangiectasia or septal
1. Guttmacher A, Marchuk D, White R. Hereditary hemorrhagic perforations. Trans Am Acad Ophthalmol Otolaryngol
telangiectasia. N Engl J Med 1995;333:918 –924. 1960;64:500 –506.
2. Ross D, Jassin B. Current trends in the diagnosis and man- 10. Saunders W. Hereditary hemorrhagic telangiectasia: effec-
agement of Osler-Weber-Rendu disease (hereditary hem- tive treatment of epistaxis by septal dermoplasty. Acta
orrhagic telangiectasia). Curr Opin Otolaryngol Head Neck Otolaryngol 1964;58:497–502.
Surg 1997;5:191–196. 11. Ross DA, Nguyen DB. Inferior turbinectomy in conjunction
3. Sadick H, Ramin N, Oulmi J, Karl H, Bergler W. Plasma with septodermoplasty for patients with hereditary hem-
surgery and topical estriol: effects on the nasal mucosa and orrhagic telangiectasia. Laryngoscope 2004;114:779 –781.
long-term results in patients with Osler’s disease. Otolar- 12. Nanthakumar K, Graham AT, Robinson TI, et al. Contrast
yngol Head Neck Surg 2003;129:233–238. echocardiography for detection of pulmonary arteriovenous
4. Shah RK, Dhingra JK, Shapshay SM. Hereditary hemor- malformation. Am Heart J 2001;141:243–246.
rhagic telangiectasia: a review of 76 cases. Laryngoscope 13. Moussouttas M, Fayad P, Rosenblatt M, et al. Pulmonary
2002;112:767–773. arteriovenous malformations: cerebral ischemia and neu-
5. Elden L, Montanera W, terBrugge K, Willinsky RA, Lasjau- rologic manifestations. Neurology 2000;55:959 –964.
nias P, Charles D. Angiographic embolization for the treat- 14. Garcia-Tsao G, Korzenik JR, Young L, et al. Liver disease in
ment of epistaxis: a review of 108 cases. Otolaryngol Head patients with hereditary hemorrhagic telangiectasia.
Neck Surg 1994;111:44 –50. N Engl J Med 2000;343:931–936.
6. Golding-Wood PH. The role of arterial ligation in intractable 15. Longacre AV, Gross CP, Gallitelli M, Henderson K, White R,
epistaxis. J Laryngol Otol Suppl 1983;8:120 –122. Proctor D. Diagnosis and management of gastrointestinal
7. Young A. Closure of the nostrils in atrophic rhinitis. J Lar- bleeding in patients with hereditary hemorrhagic telangi-
yngol Otol 1967;81:515–524. ectasia. Am J Gastroenterol 2003;98:59 – 65.
8. Bridger GP, Baldwin M. Microvascular free flap in hereditary 16. Trembath RC, Thomson JR, Machado RD, et al. Clinical and
hemorrhagic telangiectasia. Arch Otolaryngol Head Neck molecular genetic features of pulmonary hypertension in
Surg 1990;116:85– 87. patients with hereditary hemorrhagic telangiectasia.
9. Saunders WH. Septal dermoplasty for control of nosebleeds N Engl J Med 2001;345:325–334.
Laryngoscope 115: February 2005 Fiorella et al.: Outcome of Septal Dermoplasty
305
You might also like
- Facial Topography PDFDocument314 pagesFacial Topography PDFOdonto Plus100% (3)
- Libro Pie WagnerDocument1,390 pagesLibro Pie Wagnerarmando100% (1)
- Indications of The Caldwell-Luc Procedure in The eDocument7 pagesIndications of The Caldwell-Luc Procedure in The edayu100% (1)
- Health Care, Management & Entrepreneurship: A Report Submitted To Prof. Ratan JalanDocument4 pagesHealth Care, Management & Entrepreneurship: A Report Submitted To Prof. Ratan JalanDEEPANSHU SINGHNo ratings yet
- Prelims Pedia 102Document10 pagesPrelims Pedia 102quidditch07No ratings yet
- Jurnal VaskularDocument5 pagesJurnal VaskulardrelvNo ratings yet
- Submandibular Gland Excision Submandibular Gland Excision Submandibular Gland Excision Submandibular Gland Excision Submandibular Gland ExcisionDocument4 pagesSubmandibular Gland Excision Submandibular Gland Excision Submandibular Gland Excision Submandibular Gland Excision Submandibular Gland ExcisionmawarmelatiNo ratings yet
- A Study On Complications of Ventriculoperitoneal Shunt Surgery in Bir Hospital, Kathmandu, NepalDocument4 pagesA Study On Complications of Ventriculoperitoneal Shunt Surgery in Bir Hospital, Kathmandu, NepalHaziq AnuarNo ratings yet
- (2013) Surgical Treatment of Severe EpistaxisDocument6 pages(2013) Surgical Treatment of Severe EpistaxisBang mantoNo ratings yet
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552No ratings yet
- LnnkomplikacijeDocument8 pagesLnnkomplikacijeVinko GrubišićNo ratings yet
- Medip,+15 59 1 CEDocument7 pagesMedip,+15 59 1 CEKabir Ahmed LaskarNo ratings yet
- Complications of Temporomandibular Joint Arthroscopy: A Retrospective Analytic Study of 670 Arthroscopic ProceduresDocument5 pagesComplications of Temporomandibular Joint Arthroscopy: A Retrospective Analytic Study of 670 Arthroscopic ProceduresAbhishek SinghNo ratings yet
- 4 PDFDocument3 pages4 PDFSamiaNazNo ratings yet
- Epistaxis Etiology ArticleDocument7 pagesEpistaxis Etiology ArticleFaisal YousafNo ratings yet
- Laporan CS BM GINJALDocument31 pagesLaporan CS BM GINJALDellar Arciantika CahyaniNo ratings yet
- Long-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaDocument9 pagesLong-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaIdham Adyasa Manggala PutraNo ratings yet
- Knots and Knives - 3rd EditionsDocument4 pagesKnots and Knives - 3rd EditionsNasser AlbaddaiNo ratings yet
- Word 1663843244389Document11 pagesWord 1663843244389Atik PurwandariNo ratings yet
- The Perioperative Complication Rate of Orthopedic PDFDocument10 pagesThe Perioperative Complication Rate of Orthopedic PDFAnh Nguyen HuuNo ratings yet
- Shappdf25 PDFDocument6 pagesShappdf25 PDFOzzy YunandarNo ratings yet
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobNo ratings yet
- Short - and Long-Term Outcomes at A Single InstitutionDocument7 pagesShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNo ratings yet
- 1 s2.0 S1078588413007946 Main 2Document7 pages1 s2.0 S1078588413007946 Main 2Saffa AzharaaniNo ratings yet
- 2011 JET Van EekerenDocument7 pages2011 JET Van EekerenronnyNo ratings yet
- Lemus Rangel 2010Document2 pagesLemus Rangel 2010audiNo ratings yet
- Otolaryngology - Head and Neck Surgery: Hemorrhage Following Tonsillectomy and Adenoidectomy in 15,218 PatientsDocument7 pagesOtolaryngology - Head and Neck Surgery: Hemorrhage Following Tonsillectomy and Adenoidectomy in 15,218 PatientsreztrymaulidaNo ratings yet
- Iranjradiol 14 03 21742Document5 pagesIranjradiol 14 03 21742AisahNo ratings yet
- The Management of Chronic OsteomyelitisDocument7 pagesThe Management of Chronic OsteomyelitisLizzy WellaNo ratings yet
- Results of Heparin-Bonded ePTFE-covered Stents For Chronic Occlusive Superficial Femoral Artery DiseaseDocument8 pagesResults of Heparin-Bonded ePTFE-covered Stents For Chronic Occlusive Superficial Femoral Artery DiseaseNurul Azmi Rosmala PutriNo ratings yet
- Outpatient Tympanomastoidectomy: Factors Affecting Hospital AdmissionDocument4 pagesOutpatient Tympanomastoidectomy: Factors Affecting Hospital AdmissionGuillermo StipechNo ratings yet
- Puccinelli 2019Document8 pagesPuccinelli 2019RathavishwarajNo ratings yet
- Electrocautery Versus Curette Adenoidectomy: Comparison of Postoperative ResultsDocument8 pagesElectrocautery Versus Curette Adenoidectomy: Comparison of Postoperative Resultsthanhb1lqdNo ratings yet
- 1498 Reappraisal Lymph MAPPING Midgut NET Boudreaux 14Document6 pages1498 Reappraisal Lymph MAPPING Midgut NET Boudreaux 14vickyarmasrudNo ratings yet
- Epistaxis: Prevailing Factor and Treatment: Dr. H. Oscar Djauhari, SP - THTDocument19 pagesEpistaxis: Prevailing Factor and Treatment: Dr. H. Oscar Djauhari, SP - THTAbi NazhariNo ratings yet
- Evolving Approaches To The Iliacs, Femorals, Popliteals, and RenalsDocument12 pagesEvolving Approaches To The Iliacs, Femorals, Popliteals, and RenalsSohil ElfarNo ratings yet
- Streptokinase in The Treatment of Pleural Controlled Trial of IntrapleuralDocument7 pagesStreptokinase in The Treatment of Pleural Controlled Trial of IntrapleuraltomgasoneNo ratings yet
- Regarding Stroke After Varicose Vein Foam Injection Sclerotherapy Letters To Editor JVSDocument2 pagesRegarding Stroke After Varicose Vein Foam Injection Sclerotherapy Letters To Editor JVS89sbp4b7jqNo ratings yet
- Test PaperDocument4 pagesTest PaperJOSE MANUEL EspirituNo ratings yet
- Ecr2011 C-0318Document11 pagesEcr2011 C-0318zulvaasNo ratings yet
- JHLT 2020Document9 pagesJHLT 2020G WNo ratings yet
- Ultrasound-Guided Injection of Polidocanol Microfoam in The Management of Venous Leg UlcersDocument7 pagesUltrasound-Guided Injection of Polidocanol Microfoam in The Management of Venous Leg UlcersAlexandre Campos Moraes AmatoNo ratings yet
- Endovascular Embolization in The Treatment of EpistaxisDocument7 pagesEndovascular Embolization in The Treatment of Epistaxisjasa ebook18No ratings yet
- JournalDocument7 pagesJournalJirah KingadNo ratings yet
- Review Syefira SalshabilaDocument2 pagesReview Syefira Salshabilaqueen TinaNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- 2012 - Frympas G.Document8 pages2012 - Frympas G.alejandra gonzalezNo ratings yet
- Endoscopic Dacryocystorhinostomy Seems Promising For Lacrimal StenosisDocument4 pagesEndoscopic Dacryocystorhinostomy Seems Promising For Lacrimal StenosisAgitha Melita PutriNo ratings yet
- 2018 - Article Erdocan 8p.pdf - CopieDocument6 pages2018 - Article Erdocan 8p.pdf - CopieThomas HussonNo ratings yet
- IcuDocument56 pagesIcurulli_pranandaNo ratings yet
- Altered Speech Following Adenoidectomy A 20 Year ExperienceDocument5 pagesAltered Speech Following Adenoidectomy A 20 Year Experienceenfanat23No ratings yet
- Medip, IJOHNS-388 ODocument6 pagesMedip, IJOHNS-388 Onaveed gulNo ratings yet
- Embolization in The Management of Recurrent Secondary Post-Tonsillectomy Haemorrhage in ChildrenDocument7 pagesEmbolization in The Management of Recurrent Secondary Post-Tonsillectomy Haemorrhage in ChildrenNicolás HenaoNo ratings yet
- Legnani 2013Document6 pagesLegnani 2013wedawisnawaNo ratings yet
- Hydrocephalus 2Document8 pagesHydrocephalus 2caliptra36No ratings yet
- Chowdhry 2010Document4 pagesChowdhry 2010umer LoneNo ratings yet
- Study of Complications of Thyroidectomy: Pembimbing: Dr. Wahyu Adhiarto, SP.BDocument18 pagesStudy of Complications of Thyroidectomy: Pembimbing: Dr. Wahyu Adhiarto, SP.BandiamaliaNo ratings yet
- Subarachnoid Block in A Patient With Extensive Neurofibromatosis at The BackDocument4 pagesSubarachnoid Block in A Patient With Extensive Neurofibromatosis at The BackLedy Yorinda PutriNo ratings yet
- Delayed Epistaxis in External Dacryocystorhinostomy: Rate and Risk FactorsDocument4 pagesDelayed Epistaxis in External Dacryocystorhinostomy: Rate and Risk FactorsAhmed ShaalanNo ratings yet
- GJHS 6 221Document5 pagesGJHS 6 221Teuku FaisalNo ratings yet
- EnsDocument6 pagesEnsAlwi Qatsir AlyaNo ratings yet
- Distal Lakrimal Kanal T Kan KL Na e Lik Eden Lateral Nazal Duvar Patolojilerinin Incelenmesi (#180604) - 160005Document4 pagesDistal Lakrimal Kanal T Kan KL Na e Lik Eden Lateral Nazal Duvar Patolojilerinin Incelenmesi (#180604) - 160005Gusti Zidni FahmiNo ratings yet
- V 14 P 0159Document8 pagesV 14 P 0159Santi ParambangNo ratings yet
- Recurent EpistaxisDocument3 pagesRecurent EpistaxisFongmeicha Elizabeth MargarethaNo ratings yet
- Critical Care for Potential Liver Transplant CandidatesFrom EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNo ratings yet
- 10.1016@j.otc.2017.09.017 - ImprimatDocument31 pages10.1016@j.otc.2017.09.017 - ImprimatalecsaNo ratings yet
- Hereditaryhemorrhagic TelangiectasiaDocument18 pagesHereditaryhemorrhagic TelangiectasiaalecsaNo ratings yet
- Hereditary Hemorrhagic Telangiectasia: An Overview of Diagnosis, Management, and PathogenesisDocument10 pagesHereditary Hemorrhagic Telangiectasia: An Overview of Diagnosis, Management, and PathogenesisalecsaNo ratings yet
- Diagnosis and Treatment of Hereditary Hemorrhagic TelangiectasiaDocument5 pagesDiagnosis and Treatment of Hereditary Hemorrhagic TelangiectasiaalecsaNo ratings yet
- International Guidelines For The Diagnosis and Management of Hereditary Haemorrhagic TelangiectasiaDocument16 pagesInternational Guidelines For The Diagnosis and Management of Hereditary Haemorrhagic TelangiectasiaalecsaNo ratings yet
- Thalidomide Stimulates Vessel Maturation and Reduces Epistaxis in Individuals With Hereditary Hemorrhagic TelangiectasiaDocument10 pagesThalidomide Stimulates Vessel Maturation and Reduces Epistaxis in Individuals With Hereditary Hemorrhagic TelangiectasiaalecsaNo ratings yet
- Treatmentofhereditary Hemorrhagic Telangiectasia-RelatedepistaxisDocument16 pagesTreatmentofhereditary Hemorrhagic Telangiectasia-RelatedepistaxisalecsaNo ratings yet
- Safari - 1 Feb 2019 at 09:46Document7 pagesSafari - 1 Feb 2019 at 09:46alecsaNo ratings yet
- Isolated Abducens Nerve Palsy: Update On Evaluation and DiagnosisDocument1 pageIsolated Abducens Nerve Palsy: Update On Evaluation and DiagnosisalecsaNo ratings yet
- Lower Section Caeserian SectionDocument7 pagesLower Section Caeserian SectionSampat Kumawat100% (4)
- Treatment of Transverse DiscrepancyDocument75 pagesTreatment of Transverse DiscrepancyAomChanumpornNo ratings yet
- Summary:: Rodney B. SubaranDocument5 pagesSummary:: Rodney B. Subaranrodney subaranNo ratings yet
- DR - Nasmin.S, MBBS: ObjectiveDocument4 pagesDR - Nasmin.S, MBBS: ObjectiveNasmin AneeshNo ratings yet
- Ronald E Goldsteins Esthetics in DentistryDocument2 pagesRonald E Goldsteins Esthetics in Dentistrydianactb1397No ratings yet
- Anatomy of AgingDocument5 pagesAnatomy of AgingAndre3893No ratings yet
- OCULUS使用说明书 英文 - 73-144Document72 pagesOCULUS使用说明书 英文 - 73-144郭雨奇No ratings yet
- Caso Clinico Aortic Valve Replacement: Procedure: ProcedureDocument3 pagesCaso Clinico Aortic Valve Replacement: Procedure: Procedureapi-634258689No ratings yet
- Northern Trust - Whiteabbey Hospital Site PlanDocument1 pageNorthern Trust - Whiteabbey Hospital Site PlanFloyd PriceNo ratings yet
- Synthes MatrixMANDIBLeDocument30 pagesSynthes MatrixMANDIBLedoctorniravNo ratings yet
- MedOne MicroDose SF Injection KitDocument1 pageMedOne MicroDose SF Injection KitHaag-Streit UK (HS-UK)No ratings yet
- Position Indications Contraindications Supine Position - A Position Wherein TheDocument4 pagesPosition Indications Contraindications Supine Position - A Position Wherein TheGwyn Louise CarolinoNo ratings yet
- NURS 04 RLE - Bed To WheelchairDocument1 pageNURS 04 RLE - Bed To WheelchairayresNo ratings yet
- Cervical RibsDocument4 pagesCervical RibsshilusharmaNo ratings yet
- SonoTAP Flyer EnglishDocument1 pageSonoTAP Flyer English14-Sanika GarudNo ratings yet
- Aravind Eye Care SystemDocument3 pagesAravind Eye Care SystemShruti MohapatraNo ratings yet
- Pink Esthetics in Periodontics - Gingival Depigmentation: A Case SeriesDocument6 pagesPink Esthetics in Periodontics - Gingival Depigmentation: A Case SeriesdeviNo ratings yet
- Classification of Implant and AbutmentsDocument41 pagesClassification of Implant and AbutmentsKumarNo ratings yet
- Closed Treatment of Common Fractures by John Charnley: Read Online and Download EbookDocument7 pagesClosed Treatment of Common Fractures by John Charnley: Read Online and Download Ebookmuzammil kaziNo ratings yet
- Les Craniopharyngiomes Craniopharyngiomas: R. Van Effenterre, A.-L. BochDocument10 pagesLes Craniopharyngiomes Craniopharyngiomas: R. Van Effenterre, A.-L. BochyaalaNo ratings yet
- Centers For ESIC BaddiDocument5 pagesCenters For ESIC BaddiSangeeta VermaNo ratings yet
- Dental Update - May 2022Document88 pagesDental Update - May 2022Ahmed Abou FoulNo ratings yet
- Gastric LavageDocument11 pagesGastric LavageJay Villasoto100% (3)
- Aesculap Surgical Instruments: Cardiovascular and Thoracic Surgery Main CatalogDocument31 pagesAesculap Surgical Instruments: Cardiovascular and Thoracic Surgery Main Cataloginstrumed_globalNo ratings yet
- Dental ImplantsDocument30 pagesDental Implantsآلاء حسن يونسNo ratings yet