Professional Documents
Culture Documents
Amount payable under Star Care health insurance policy
Uploaded by
ShivaRamaKrishnaPatelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Amount payable under Star Care health insurance policy
Uploaded by
ShivaRamaKrishnaPatelCopyright:
Available Formats
Amount payable However in respect of disease / sickness / illness for which the claim/s has/have been made, the
/s has/have been made, the sum
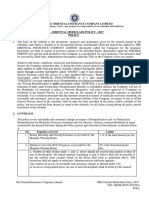
Description Hospital Bill (Rs.)
STAR CARE Insurance Policy Surgery for Cancer (Major Surgery) for self 55000
as per policy (Rs)
40000
insured will be restricted to sum insured under the policy when the signs or symptoms was/were first
diagnosed / received medical advice / treatment.
Unique Id : IRDA/NL-HLT/SHAI/P-H/V.I/10/14-15
In the event of this policy being withdrawn / modified with revised terms and/or premium with the prior
Accidental grievous injury for spouse 45000 40000 approval of the Competent Authority, the insured will be intimated three months in advance and
Star Care is a health insurance plan that gives protection for individuals as well as the entire
accommodated in any other equivalent health insurance policy offered by the Company, if requested
family, on the payment of a single premium under a single sum insured. The Single Annual Admission of son for Jaundice 8500 7500
for by the Insured Person, at the relevant point of time.
sum insured of Rs.1,00,000/- covers all your family members, if it is a floater policy.
Minor Surgery for draining of large 12500 ¬ EXCLUSIONS
19000 (Balance of sum
¬ Eligibility sub-cutaneous abcess for self 1. Pre Existing Diseases as defined in the policy until 48 consecutive months of continuous coverage
insured of
have elapsed; since inception of the first policy with any Indian Insurer. However the limit of the
Ÿ Any person aged between 18 years and 65 years, from Tier-1 & Tier-2 Places in India, Rs. 1,00,000/-)
Company's liability in respect of claim for pre-existing diseases shall be limited to the sum insured under
can take this insurance Maximum Liability Rs. 1,00,000/- the first policy with any Indian Insurance Company.
Ÿ Beyond 65 years, policy can be renewed for life time. 2. Any disease contracted by the insured person during the first 30 days from the commencement date of
¬ Pre & Post Hospitalization the policy. This exclusion shall not apply in case of the insured person having been covered under any
Ÿ Children from 2 years covered along with parents.
Pre-hospitalization medical expenses incurred up to 30 days prior to the date of admission are payable. health insurance policy (Individual or Group insurance policy) with any of the Indian Insurance
(Tier-1 places means those places where the population as per census 2011 is between 5,00,000 and
Post-hospitalization up to 60 days from the date of discharge from the hospital. A lump sum calculated companies for a continuous period of preceding 12 months without a break.
10,00,000. Tier-2 places means those places where the population as per census 2011 is less than 3. During the first two years of continuous operation of insurance cover any expenses on
@7% of the hospitalization expenses (excluding room charges) subject to a maximum of Rs.3,000/- is
5,00,000). payable. a) Cataract, Retinal detachment, Glaucoma, diseases of ENT, Mastoidectomy, Tympanoplasty,
¬ Policy Benefits Minimum period of hospitalisation is 24 hours. This time limit is waived where the treatment is taken for Stapedectomy diseases related to Thyroid, Prolapse of intervertebral disc (other than caused by
specified day care treatments listed in the policy. accident), varicose veins and varicose ulcers, all diseases of prostate, Stricture Urethra, all obstructive-
Ÿ Hospitalisation Benefits:
uropathies,all types of hernia, varicocele, hydrocele, fistula/fissure in ano, Hemorrhoids, Pilonidal sinus
¬ Pre Acceptance Medical Screening: There is no pre acceptance medical screening.
A) Room, Boarding, Nursing Expenses at 0.75% of sum insured either private room and fistula, Rectal Prolapse, stress incontinence and Congenital Internal disease / defect.
¬ Pre Existing Disease: Pre existing diseases are covered after 48 months of continuous insurance with
or shared accommodation. b) Gall bladder diseases and all treatments (conservative, interventional, laparoscopic and open) related
any Indian Insurance Company.
to Hepato pancreato-biliary including gall bladder and pancreatic calculi. All types of management for
B) ICU charges upto Rs.2,000/- subject to maximum of Rs.10,000/- per ¬ Day Care Treatment: 405 day care treatments are allowed. kidney and genitourinary tract calculi.
hospitalization. ¬ Portability: This policy is portable. If the insured is desirous of porting this policy to another Insurer c) All treatments (conservative, interventional, laparoscopic and open) related to all diseases of uterus,
C) Surgeon, Anesthetist, Medical Practitioner, Consultants & Specialist Fees. towards renewal, application in the appropriate form should be made to the Company at least before fallopian tubes, cervix and ovaries, dysfunctional uterine bleeding, pelvic inflammatory diseases,
45 days from the date when the renewal is due. benign breast diseases.
D) Anesthesia, Blood, Oxygen, Operation Theatre charges, cost of Pacemaker etc. Where the outcome of acceptance of portability is still waiting from the new insurer on the date of d) Conservative, operative treatment and all types of intervention for diseases related to tendon, ligament,
E) Cost of Medicine and drugs. renewal, the existing policy will be extended on the request of the Insured person, for a period not less fascia, bones and joint [other than caused by accident]
than one month on pro rata premium. Such extended cover will be cancelled only on the written request e) Degenerative disc and vertebral diseases including replacement of bones and joints and degenerative
F) Emergency ambulance charges for transporting the covered patient to the hospital by the Insured Person, subject to a minimum pro rata premium for one month. If the Insured Person diseases of the musculo-skeletal system
up to a sum of Rs.500/- per hospitalisation and overall limit of Rs.1000/- per policy requests in writing to continue the policy with the Company without porting, it will be allowed by
charging the regular premium with the same terms as per the expiring policy. In case of a claim made by f) Subcutaneous benign lumps, sebaceous cyst, dermoid cyst, lipoma, neurofibroma, fibroadenoma,
period. ganglion and similar pathology
the Insured person and admitted by the Company during such extension, the policy will be extended for
G) Hospital Cash will be paid at the rate of One Thousand Rupees per day of the remaining period by charging the regular premium. Portability is not possible during the policy g) Any transplant and related surgery
hospitalization subject to a maximum of 14 days, where the treatment is taken in This waiting period shall not however apply in the case of the Insured person/s having been covered
Government Hospital. This will be paid only for covered surgeries done as in- Age (Amount in Rs.) under any Individual health insurance scheme with any of the Indian Insurer for a continuous period of
(in years) Plan preceding 24 months without any break.
patient, whether any claim is made on indemnity basis or not. Payment of claim
1A 1A+1C 1A+2C 2A 2A+1C 2A+2C The claim for such illnesses/diseases/disabilities contracted/suffered if admitted will be processed as
under hospital cash benefit will not reduce the Sum Insured.
2-25 905 1,290 1,620 1,400 1,705 1,995 per the sum insured of the immediately preceding 24 months policy only. Where there is a change in the
Ÿ Treatment for specific diseases/illness as detailed below:- 26-40 1,100 1,665 2,090 1,805 2,200 2,500 sum insured in the second continuous policy year the lower of the sum insured will apply.
41-50 1,600 2,395 2,945 2,600 3,100 3,500
If these are pre-existing at the time of proposal they will be covered subject to Exclusion No 1 above.
Limit of indemnity per policy period 51-60 2,200 3,320 4,180 3,605 4,400 5,000
Ailment 4. Circumcision, Inoculation or Vaccination (except for post–bite treatment and for medical treatment
61-65 3,080 4,540 5,700 4,930 6,000 6,780
66-70 3,665 5,400 6,795 5,865 7,150 8,065 other than for prevention of diseases.)
Medical Management (Major diseases) ` 15, 000
Above 70 4,290 6,320 7,955 6,865 8,370 9,440 5. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Medical Management (Other diseases) ` 7, 500 Service Tax Extra (Dental implants are not payable)
Renewal premium subject to change with prior approval from IRDA. 6. Convalescence, general debility, run-down condition or rest cure, nutritional deficiency states,
Cataract ` 8, 500 psychiatric, mental and behavioral disorders, congenital external disease or defects or anomalies,
period. For details contact “portability@starhealth.in” or call Telephone No +91-044-28288869.
Accidental grevious injuries venereal disease and sexually transmitted diseases, intentional self injury and use of intoxicating drugs
(either surgery or medical management) ` 40, 000 ¬ Premium Chart / alcohol, smoking and tobacco chewing.
¬ Tax Benefits: Payment of premium by any mode other than cash for this insurance is eligible for relief 7. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of
Major Surgeries ` 40, 000 under Section 80D of the Income Tax Act 1961. foreign enemy, warlike operations (whether war be declared or not).
Other Surgeries ` 20, 000 ¬ Family: Proposer, spouse, dependent children up to 25 years (those who are economically dependent 8. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons / materials .
on their parents) 9. All expenses arising out of any condition directly or indirectly caused due to or associated with Human
Ÿ Benefit Illustration: ¬ Renewal Condition: Lifelong renewal of the policy is offered, except on grounds such as moral hazard, T-cell Lympho Trophic Virus type III (HTLV-III) or Lymphadenopathy Associated Virus (LAV) or the
misrepresentation / Non Disclosure or fraud committed. Mutants Derivative or Variations Deficiency Syndrome or any Syndrome or condition of a similar kind
Let us take the example of a family floater cover with following medical expenses during commonly referred to as AIDS.
A grace period of 30 days from the date of expiry of the policy is available for renewal. Any change in
the policy period: sum insured is possible only at the time of renewal. If the policy is to be renewed or ported from other It is however made clear that such of those who are positive for HIV (Human Immuno Deficiency Virus)
Indian Insurance Company for enhanced sum insured then the waiting period as applicable to a fresh would be entitled for expenses incurred for treatment, other than for opportunistic infections and for
policy will apply to additional sum insured as if a separate policy has been issued for the difference. In treatment of HIV/AIDS, provided at the time of first commencement of insurance under this policy, their
other words the enhanced sum insured will not be available for an illness, disease, injury already CD4 count is not less than 350.
contracted under the preceding policy period.
10. Treatment arising from or traceable to pregnancy, childbirth, miscarriage, abortion or ¬ Claims Procedure
complications of any of these (other than ruptured ectopic gestation), family planning Ÿ Call the 24 hour help-line for assistance-1800-425-2255 / 1800-102-4477. Inform the ID/Policy
STAR CARE INSURANCE POLICY
treatment and all types of treatment for infertility and its complications thereof. number for easy reference
11 Expenses incurred on weight control services including surgical procedures for Ÿ In case of planned hospitalization, inform 24 hours prior to admission in the hospital
treatment of obesity, medical treatment for weight control, treatment for metabolic, Ÿ In case of emergency hospitalization, information to be given within 24 hours of hospitalization
genetic and endocrine disorders.
Ÿ Cashless facility can be availed in network hospitals in Tier-1 & Tier-2 location.
12. Expenses incurred on High Intensity Focused Ultra Sound, Uterine fibroid
Ÿ In non-network hospitals payment, must be made up-front and then reimbursement will be effected
embolisation, Balloon Sinoplasty, Enhanced External Counter Pulsation Therapy and
on submission of documents.
related therapies, Chelation therapy, Deep Brain Stimulation, Hyperbaric Oxygen
Therapy, Rotational Field Quantum Magnetic Resonance Therapy, Photodynamic Ÿ Hospital Cash benefits, if applicable, will be paid on reimbursement basis. Health
therapy and such other therapies similar to those mentioned herein under exclusion ¬ The Company: Personal & Caring Insurance
No12. Star Health and Allied Insurance Company Ltd commenced its operations in 2006 with the business The Health Insurance Specialist
13. Expenses incurred on Lasik Laser or Refractive Error Correction and its complications interests in Health Insurance, Travel and Personal Accident. As an exclusive Health Insurance
all treatment for disorders of eye requiring intra-vitreal injections and related Company and the first of its kind in India, the Company is committed insetting international benchmarks
procedures. in service and personal caring.
14. Charges incurred at Hospital or Nursing Home primarily for diagnostic, X-ray or ¬ Star Advantages
laboratory examinations not consistent with or incidental to the diagnosis and treatment Ÿ No Third Party Administrator, direct in-house claims settlement.
of the positive existence or presence of any ailment, sickness or injury, for which Ÿ Faster & hassle –free claim settlement.
confinement is required at hospital/nursing home.
Ÿ Cashless hospitalization, wherever possible.
15. Expenses on vitamins and tonics unless forming part of treatment for injury or disease
Ÿ Network of more than 6000 hospitals across India.
as certified by the attending Physician.
Ÿ 24X7 Toll Free Helpline.
16. Naturopathy Treatment, unconventional, untested, unproven, experimental therapies
Ÿ Information on health through free health magazine.
17. Stem cell Therapy and related transplantation, Chondrocyte Implantation,
Immunotherapy, Oral Chemo Therapy. Ÿ Facility maintaining personal health records in electronic format.
18. Hospital registration charges, admission charges, record charges, telephone charges ¬ Prohibition of Rebates
and such other charges. Section 41 of Insurance Act 1938 : No person shall allow or offer to allow, either directly or indirectly, as
19. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk
medicines other than Allopathy. relating to lives or property in India, any rebate of the whole or part of the commission payable or any
20. Change of sex or cosmetic or aesthetic treatment of any description, plastic surgery rebate of the premium shown on the policy, nor shall any person taking out or renewing orcontinuing a
(other than as necessitated due to an accident or as a part of any illness), all treatment policy accept any rebate, except such rebate as may be allowed in accordance with the published
for erectile dysfunctions. prospectuses or tables of the insurer.
21. Cost of spectacles and contact lens, hearing aids, Cochlear implants walkers and Any person making default in complying with the provisions of this section shall be liable for a penalty
crutches, wheel chairs, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis, which may extend to ten lakh rupees.
infusion pump and such other similar aids.
22. Any specific time-bound or life time exclusions applied, specified and accepted by the
insured. The information provided in this brochure is only indicative.
23. Other expenses as detailed elsewhere in the policy. For more details on the risk factors, terms and conditions,
¬ Cancellation: The Company may cancel this policy on grounds of misrepresentation, please read the policy wordings before concluding sale
fraud, moral hazard, non disclosure of material fact or non cooperation by the insured Or
person, by sending the Insured 30 days notice by registered letter at the Insured Visit our website www.starhealth.in
person's last known address and no refund of premium will be made.
The insured may at any time cancel this policy and in such event the Company shall
allow refund after retaining premium at Company's short Period rate only (table given
below) provided no claim has occurred up to the date of cancellation.
¬ Free Look Period : A free look period of 15 days from the date of receipt of the policy is
RATE OF PREMIUM TO BE RETAINED
PERIOD ON RISK
BY THE INSURER
Up to one-month 1/3rd of annual premium
BRO / CARE / V.4 / 2017 - 18
“IRDAI OR ITS OFFICIALS DO NOT INVOLVE IN ACTIVITIES LIKE SALE OF ANY KIND OF
Up to three Months ½ of annual premium
INSURANCE OR FINANCIAL PRODUCTS NOR INVEST PREMIUMS. IRDAI DOES NOT
Up to six months 3/4th of annual premium
ANNOUNCE ANY BONUS. THOSE RECEIVING SUCH PHONE CALLS ARE REQUESTED TO
Exceeding six months Full annual premium
LODGE A POLICE COMPLAINT ALONG WITH DETAILS OF PHONE CALL AND NUMBER”
available to the insured to review the terms and conditions of the policy. In case the
insured is not satisfied with the terms and conditions, the insured may seek cancellation Call Toll-free: 1800-425-2255 / 1800-102-4477, sms STAR to 56677 STAR CARE INSURANCE POLICY
of the policy and in such an event the Company shall allow refund of premium paid after Fax Toll Free No: 1800-425-5522 « Email : support@starhealth.in
adjusting the cost of pre-acceptance medical screening, stamp duty charges and CIN : U66010TN2005PLC056649 « IRDAI Regn. No: 129
SQPIL-06.11.2015-5K
proportionate risk premium for the period concerned provided no claim has been made
until such cancellation.
Free look cancellation is not applicable at the time of renewal of the policy STAR CARE INSURANCE POLICY
Unique ID: IRDA/NL-HLT/SHAI/P-H/V.I/10/14-15
You might also like
- Raise Your Vibration With Essential OilsDocument34 pagesRaise Your Vibration With Essential OilsYahya Saleem-BeyNo ratings yet
- THE AFFORDABLE ARTHRITIS & OSTEOPOROSIS CUREDocument18 pagesTHE AFFORDABLE ARTHRITIS & OSTEOPOROSIS CURENatalia NeliNo ratings yet
- Drug Classification Indication Action and Pharmacokinetics Contraindication Adverse Effect Monitoring ParameterDocument5 pagesDrug Classification Indication Action and Pharmacokinetics Contraindication Adverse Effect Monitoring ParameteryssatNo ratings yet
- Shatavari - Benefits, Precautions and DosageDocument13 pagesShatavari - Benefits, Precautions and Dosagenvenkatesh485No ratings yet
- The Family Doctor - Prof. Henry S Taylor, M.D., 1860Document324 pagesThe Family Doctor - Prof. Henry S Taylor, M.D., 1860IreneRainsNo ratings yet
- St. Luke's Accredited DoctorsDocument20 pagesSt. Luke's Accredited DoctorsCrest PedrosaNo ratings yet
- The Accidental Prime Minister Inside Look at Indian PoliticsDocument4 pagesThe Accidental Prime Minister Inside Look at Indian PoliticsWaseem Khan0% (1)
- Senior Citizen Red Carpet BrochureDocument2 pagesSenior Citizen Red Carpet Brochureramki020983No ratings yet
- Royal Sundaram General Insurance Co. Limited (Formerly Known As Royal Sundaram Alliance Insurance Company Limited)Document2 pagesRoyal Sundaram General Insurance Co. Limited (Formerly Known As Royal Sundaram Alliance Insurance Company Limited)Abhijit MohantyNo ratings yet
- Balsam Leaflet en PDFDocument8 pagesBalsam Leaflet en PDFEng. Waleed AhmedNo ratings yet
- Oriental Insurance Company's Happy Family Floater PolicyDocument31 pagesOriental Insurance Company's Happy Family Floater PolicyAmit RajNo ratings yet
- Policy Benefits 023173Document3 pagesPolicy Benefits 023173pradosh002No ratings yet
- All day care treatments covered by cancer care insuranceDocument2 pagesAll day care treatments covered by cancer care insuranceNitin BandgarNo ratings yet
- IT Exemption Guidelines 2023-24Document7 pagesIT Exemption Guidelines 2023-24rashiramesh31No ratings yet
- Family Health Optima Insurance Plan NewDocument8 pagesFamily Health Optima Insurance Plan NewNeeraj NemaNo ratings yet
- Happy Family Floater - Policy NewDocument45 pagesHappy Family Floater - Policy Newpooja singhalNo ratings yet
- Star Health policy wordingsDocument4 pagesStar Health policy wordingsKishore KNo ratings yet
- Niva PB ReAssure SS v5Document2 pagesNiva PB ReAssure SS v5samdsozaNo ratings yet
- Niva ReAssure SS v11Document2 pagesNiva ReAssure SS v11CHELLASWAMY RAMASWAMYNo ratings yet
- COMPLETE HEALTH INSURANCE WITH COVID COVERAGEDocument2 pagesCOMPLETE HEALTH INSURANCE WITH COVID COVERAGEPRADEEP GUPTANo ratings yet
- Reassurance at Every Step: Keeps Giving You More!Document2 pagesReassurance at Every Step: Keeps Giving You More!rajatshrimalNo ratings yet
- Niva ReAssure SS v3Document2 pagesNiva ReAssure SS v3Arun GoyalNo ratings yet
- Reassurance at Every Step: Keeps Giving You More!Document2 pagesReassurance at Every Step: Keeps Giving You More!ASHOK NAGESHWARANNo ratings yet
- Niva ReAssure SS v3Document2 pagesNiva ReAssure SS v3megha mazumdarNo ratings yet
- Niva ReAssure SS v3Document2 pagesNiva ReAssure SS v3arya aroraNo ratings yet
- Family Plus Brochure PDFDocument2 pagesFamily Plus Brochure PDFAnonymous B7N7Pj33mhNo ratings yet
- Leaflet PDFDocument9 pagesLeaflet PDFVyshak SamakNo ratings yet
- The Oriental Insurance Company LimitedDocument33 pagesThe Oriental Insurance Company LimitedSharma AmanNo ratings yet
- Star Comprehensive Prospectus New 1Document10 pagesStar Comprehensive Prospectus New 1Anil WadhaveNo ratings yet
- Product Liability Insurance Policy - AxaDocument4 pagesProduct Liability Insurance Policy - AxaAbhishekNo ratings yet
- Star Health and Allied Insurance Company Limited: Prospectus - Mediclassic Insurance Policy (Individual)Document8 pagesStar Health and Allied Insurance Company Limited: Prospectus - Mediclassic Insurance Policy (Individual)mfsrajNo ratings yet
- Health-Booster BrochureDocument10 pagesHealth-Booster BrochureParasaram SrinivasNo ratings yet
- ReAssure_SSDocument2 pagesReAssure_SSAmit Kumar KandiNo ratings yet
- Celebrating 60 Years of Excellence, Sri Lanka Insurance PresentsDocument2 pagesCelebrating 60 Years of Excellence, Sri Lanka Insurance PresentsSivaneswaran ChandrasekaranNo ratings yet
- Mediclaim Insurance Policy (Group) Policy WordingsDocument29 pagesMediclaim Insurance Policy (Group) Policy WordingsSaransh SharmaNo ratings yet
- Reliance Personal Loan Care Insurance Policy - 2013-2014Document24 pagesReliance Personal Loan Care Insurance Policy - 2013-2014pankhuri.singhNo ratings yet
- For Example,: Free Look PeriodDocument2 pagesFor Example,: Free Look PeriodPankaj_Ambesange_660No ratings yet
- Senior Citizens Red Carpet Health Insurance Policy PDFDocument8 pagesSenior Citizens Red Carpet Health Insurance Policy PDFrohit22221No ratings yet
- Health QuotationDocument4 pagesHealth QuotationKasturi SankarNo ratings yet
- The Oriental Insurance Company LimitedDocument9 pagesThe Oriental Insurance Company LimitedkmrezNo ratings yet
- Sahi ExportDocument8 pagesSahi ExportHeena ChoudharyNo ratings yet
- Virgilio Reyes 2024-03-12 03 - 01 - 57Document15 pagesVirgilio Reyes 2024-03-12 03 - 01 - 57Cyber ZoneNo ratings yet
- Induction Manual 1688120103Document24 pagesInduction Manual 1688120103Radhe shamNo ratings yet
- Comprehensive insurance policy featuresDocument1 pageComprehensive insurance policy featuresvamsiklNo ratings yet
- Senior Citizens Health Insurance ProspectusDocument7 pagesSenior Citizens Health Insurance ProspectusHdjhdhdNo ratings yet
- Key Information SheetDocument16 pagesKey Information SheetSwati ShuklaNo ratings yet
- Care Advantage-Policy WordingDocument61 pagesCare Advantage-Policy Wordingmilind.v.patilNo ratings yet
- PRUBiz Flyer Protect ENG FADocument5 pagesPRUBiz Flyer Protect ENG FAAmmar Ismail (Sparky90)No ratings yet
- Tata AIG MediCare Premier Policy SummaryDocument16 pagesTata AIG MediCare Premier Policy SummarySiddhartha PorwalNo ratings yet
- Income Tax: Chapter Vi-A Deductions From Gross Total IncomeDocument20 pagesIncome Tax: Chapter Vi-A Deductions From Gross Total Incomesoumya256No ratings yet
- Benefits Summary IndiaDocument9 pagesBenefits Summary IndiaABHISHEK BAGHNo ratings yet
- HFFP-2015 Revised ProspectusDocument25 pagesHFFP-2015 Revised Prospectuspooja singhalNo ratings yet
- POS Family Health Optima Insurance Plan PDFDocument5 pagesPOS Family Health Optima Insurance Plan PDFDeb Kumar BeraNo ratings yet
- Medgulf Nextcare Rn2 TobDocument4 pagesMedgulf Nextcare Rn2 Tobkcatolico00No ratings yet
- Rapyuta Robotics PVT LTD - GMC Renewal Quote - 28th Dec2022Document1 pageRapyuta Robotics PVT LTD - GMC Renewal Quote - 28th Dec2022nagarajgnairyNo ratings yet
- FHO Prospectus PDFDocument20 pagesFHO Prospectus PDFVidhyaRIyengarNo ratings yet
- Health 360 Rider Brochure 07Document6 pagesHealth 360 Rider Brochure 07Sreeraj P SNo ratings yet
- Bhavishya Arogya ProspectusDocument7 pagesBhavishya Arogya ProspectusHarsh RajNo ratings yet
- Tata AIG 360Document4 pagesTata AIG 360udemycourse1947No ratings yet
- ICICI GMC Quote - Baroda Decorators Revised 02.04.2024Document6 pagesICICI GMC Quote - Baroda Decorators Revised 02.04.2024silvershield.generalNo ratings yet
- KOCH Benefits Manual AgnityDocument50 pagesKOCH Benefits Manual AgnitymayankNo ratings yet
- Senior Citizen Red Carpet Brochure PDFDocument4 pagesSenior Citizen Red Carpet Brochure PDFCHRISTY JOSENo ratings yet
- Complete Health Insurance-Brochure PDFDocument16 pagesComplete Health Insurance-Brochure PDFRishi AroraNo ratings yet
- CompleteHealthInsuranceBrochure PDFDocument16 pagesCompleteHealthInsuranceBrochure PDFRishi AroraNo ratings yet
- 11-01-2023 Current AffairsDocument2 pages11-01-2023 Current AffairsShivaRamaKrishnaPatelNo ratings yet
- Highly Useful Current Affairs Quiz For Civils Groups S.I. Constables DSC Sachivalayam RRBDocument4 pagesHighly Useful Current Affairs Quiz For Civils Groups S.I. Constables DSC Sachivalayam RRBShivaRamaKrishnaPatelNo ratings yet
- IPS - Transfers - GODocument3 pagesIPS - Transfers - GOShivaRamaKrishnaPatelNo ratings yet
- 11-01-2023 Current AffairsDocument2 pages11-01-2023 Current AffairsShivaRamaKrishnaPatelNo ratings yet
- 11-01-2023 Current AffairsDocument2 pages11-01-2023 Current AffairsShivaRamaKrishnaPatelNo ratings yet
- ST BY G.MANJULA WPC IT&C 1803Document2 pagesST BY G.MANJULA WPC IT&C 1803ShivaRamaKrishnaPatelNo ratings yet
- Telangana State Level Police Recruitment Board: Press NoteDocument2 pagesTelangana State Level Police Recruitment Board: Press NoteShivaRamaKrishnaPatelNo ratings yet
- TS Police Annexure V Format PDF - Jobs AddaDocument1 pageTS Police Annexure V Format PDF - Jobs AddaShivaRamaKrishnaPatelNo ratings yet
- Pol. Sci. SyllabusDocument6 pagesPol. Sci. SyllabusNeerup DhamaNo ratings yet
- Dashboard shows invoice detailsDocument1 pageDashboard shows invoice detailsShivaRamaKrishnaPatelNo ratings yet
- Document From Sagargariganti986@gmailDocument2 pagesDocument From Sagargariganti986@gmailShivaRamaKrishnaPatelNo ratings yet
- Amount payable under Star Care health insurance policyDocument2 pagesAmount payable under Star Care health insurance policyShivaRamaKrishnaPatelNo ratings yet
- TSPSC Groupiv SyllabusDocument1 pageTSPSC Groupiv Syllabusapi-293926977No ratings yet
- Pacs Sulthanabad Date 17-06-2020 S.No Name Father Name Village AmountDocument2 pagesPacs Sulthanabad Date 17-06-2020 S.No Name Father Name Village AmountShivaRamaKrishnaPatelNo ratings yet
- TSPSC Group 1 SyllabusDocument14 pagesTSPSC Group 1 Syllabusapi-293926977No ratings yet
- GL11374558 Amort ScheduleDocument1 pageGL11374558 Amort ScheduleShivaRamaKrishnaPatelNo ratings yet
- 100 Sentences (19-06-12) PDFDocument7 pages100 Sentences (19-06-12) PDFSridhar Kumar JastiNo ratings yet
- Geography As A DisciplineDocument12 pagesGeography As A DisciplineAtul Saini100% (5)
- Claim FormDocument5 pagesClaim Formwawawa1No ratings yet
- Ources OF Nformation About THE NteriorDocument9 pagesOurces OF Nformation About THE NteriorShivaRamaKrishnaPatelNo ratings yet
- Mann PDFDocument33 pagesMann PDFShivaRamaKrishnaPatelNo ratings yet
- The Origin and Evolution of EarthDocument8 pagesThe Origin and Evolution of Earthhepzibah001No ratings yet
- 23 SCT Sar CPL PDFDocument1 page23 SCT Sar CPL PDFShivaRamaKrishnaPatelNo ratings yet
- X4 F SIZdsu MDLM H0 LDocument1 pageX4 F SIZdsu MDLM H0 LShivaRamaKrishnaPatelNo ratings yet
- RajuDocument2 pagesRajuShivaRamaKrishnaPatelNo ratings yet
- 23 SCT Sar CPLDocument1 page23 SCT Sar CPLShivaRamaKrishnaPatelNo ratings yet
- Management Trainee DetailsDocument10 pagesManagement Trainee DetailsAnirudh MølûgüNo ratings yet
- FIREMEN, 2018: Cut-Off Marks and Dob Adilabad District General HG 20%OPEN 137.00 CategoryDocument10 pagesFIREMEN, 2018: Cut-Off Marks and Dob Adilabad District General HG 20%OPEN 137.00 CategoryShivaRamaKrishnaPatelNo ratings yet
- General Tonic Monograph and Pharmacology Shi Quan Da Bu WanDocument8 pagesGeneral Tonic Monograph and Pharmacology Shi Quan Da Bu WanrikiNo ratings yet
- Cohort Study Meat Intake An Cancer RiskDocument8 pagesCohort Study Meat Intake An Cancer RiskHarunNo ratings yet
- Brunswick County 2022 Community Health Needs AssessmentDocument154 pagesBrunswick County 2022 Community Health Needs AssessmentJamie BouletNo ratings yet
- Stress Management Strategies: Individual Approaches Organizational ApproachesDocument13 pagesStress Management Strategies: Individual Approaches Organizational ApproachesYakshit GoelNo ratings yet
- Camille Suzaine Pradas - Labs and DrugsDocument7 pagesCamille Suzaine Pradas - Labs and DrugsCamille Suzaine PradasNo ratings yet
- Effect of Custom-Made Footwear On Foot Ulcer Recurrence in DiabetesDocument8 pagesEffect of Custom-Made Footwear On Foot Ulcer Recurrence in DiabetesJosé MorenoNo ratings yet
- CA 125II: Assay SummaryDocument14 pagesCA 125II: Assay SummaryThế TuyềnNo ratings yet
- English Task - Multiple Choices - 20200102Document8 pagesEnglish Task - Multiple Choices - 20200102bangtan's elite trashNo ratings yet
- Total Penectomy Urooncology 12thDocument10 pagesTotal Penectomy Urooncology 12thdr. Joko WibowoNo ratings yet
- 265 23686 1 10 20190515 PDFDocument10 pages265 23686 1 10 20190515 PDFanggiliaNo ratings yet
- Key Factors for Food Business SuccessDocument12 pagesKey Factors for Food Business SuccessOreoNo ratings yet
- Assign No. 1 Module 6Document3 pagesAssign No. 1 Module 6Cindy Mae de la TorreNo ratings yet
- IntroductionDocument5 pagesIntroductionDivyansh GolyanNo ratings yet
- Pediatric Malnutrition Causes and ManagementDocument38 pagesPediatric Malnutrition Causes and ManagementShafie ElmiNo ratings yet
- Pdoc - Vivicit LeafletDocument1 pagePdoc - Vivicit Leafletahmedrijone2014No ratings yet
- Prevention of Surgical Site Infections: Pola Brenner, Patricio NercellesDocument10 pagesPrevention of Surgical Site Infections: Pola Brenner, Patricio NercellesAmeng GosimNo ratings yet
- Practice Enteral and Parenteral CalculationsDocument2 pagesPractice Enteral and Parenteral CalculationsRavenNo ratings yet
- Nephrotic SyndromeDocument23 pagesNephrotic SyndromeDivina Francia JovenNo ratings yet
- Ectopic PregnancyDocument54 pagesEctopic Pregnancypatriciaatan1497No ratings yet
- Poor Diet, Lack of Sunshine Linked to Rising DepressionDocument7 pagesPoor Diet, Lack of Sunshine Linked to Rising DepressionAndri Ferdian100% (1)
- Ma. Sarah A. I. Concepcion, MD, Moh: Employees' Compensation CommissionDocument57 pagesMa. Sarah A. I. Concepcion, MD, Moh: Employees' Compensation CommissionemmalyneNo ratings yet
- Classifying Co-Morbid Chronic DiseasesDocument14 pagesClassifying Co-Morbid Chronic DiseasesAlvaro Paredes RiveraNo ratings yet
- No. Nama Penyakit Kode Dan Nama Diagnosa ICD 10Document16 pagesNo. Nama Penyakit Kode Dan Nama Diagnosa ICD 10Sari Eka RahayuNo ratings yet
- O and G Notes Notebank NumberedDocument173 pagesO and G Notes Notebank NumberedPerscitus Ali القحطانيNo ratings yet