Professional Documents
Culture Documents
22 Iajps22102020
Uploaded by
iajpsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
22 Iajps22102020
Uploaded by
iajpsCopyright:
Available Formats
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN : 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
SJIF Impact Factor: 7.187
http://doi.org/10.5281/zenodo.4065092
Available online at: http://www.iajps.com Research Article
ASSOCIATION BETWEEN NON-ALCOHOLIC FATTY LIVER
DISEASE (NAFLD) AND RAISED CAROTID INTIMA-MEDIA
THICKNESS (CIMT)
1Dr.
Fatima Safdar, 2Dr. Muhammad Haris Sarwar, 3Dr. Ghulam Mustafa
1
Ex-house Officer, Bahawal Victoria Hospital, Bahawalpur
2
Ex-house Officer, Bahawal Victoria Hospital, Bahawalpur
3
Ex-house Officer, Bahawal Victoria Hospital, Bahawalpur
Article Received: August 2020 Accepted: September 2020 Published: October 2020
Abstract:
Objective: To determine the association between nonalcoholic fatty liver disease (NAFLD) and raised
carotid intima-media thickness
Materials & Methods: This cross-sectional study was conducted at Department of Medicine, Bahawal
Victoria Hospital, Bahawalpur from July 2019 to December 2019 over the period of 6 months. Total 109
patients either male or female having age from 30-45 years having nonalcoholic fatty liver disease were
selected for this study.
Results: The mean age in cases group was 37.51 ± 4.07 years and in control group was 37.45 ± 4.03 years. Out of
218 patients, 136 (62.39%) were males and 82 (37.61%) were females with male to female ratio of 1.7:1. Frequency
of raised CIMT in cases group was seen in 62 (56.88%) while in control group was seen in 41 (37.61%) cases with a
p-value of 0.004 and odds ratio of 2.1879 which is statistically significant and shows a positive association between
NAFLD and raised CIMT.
Conclusion: This study concluded that the frequency of raised carotid intima-media thickness is higher in patients
with non-alcoholic fatty liver disease and shows the positive association between nonalcoholic fatty liver disease
(NAFLD) and raised carotid intima-media thickness.
Keywords: Liver, alcohol, fatty, carotid.
Corresponding author:
Dr. Fatima Safdar, QR code
Ex-house Officer, Bahawal Victoria Hospital, Bahawalpur
.
Please cite this article in press Fatima Safdar et al, Association Between Non-Alcoholic Fatty Liver Disease (NAFLD)
And Raised Carotid Intima-Media Thickness (CIMT)., Indo Am. J. P. Sci, 2020; 07(10).
www.iajps.com Page 100
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
INTRODUCTION: hundred and nine controls, preferably from relatives of
Nonalcoholic fatty liver disease (NAFLD) is a highly these patients, having normal liver echogenicity on
prevalent condition characterized by excessive abdominal ultrasound, were matched for age, gender
accumulation of fat in liver cells.1Nonalcoholic fatty and body mass index were selected.
liver disease (NAFLD) encompass a spectrum of
pathological conditions, ranging from simple steatosis Patients with diabetes mellitus (having fasting serum
to nonalcoholic steatohepatitis (NASH) and cirrhosis2, glucose ≥ 126mg/dl or on treatment for diabetes),
resembling that of alcoholic liver disease but occurs in patients with hypertension (having BP ≥ 140/90
persons who do not abuse alcohol.3 Thus, NAFLD mmHg or on treatment for hypertension), having
shares many features of metabolic syndrome, a highly history of ischemic heart disease, history of chronic
atherogenic condition, and its presence could signify a liver disease, patients with alcohol consumption (
substantial cardiovascular risk above and beyond that more than 140g weekly in men and 70g weekly in
conferred by individual risk factors.4 NAFLD itself is women), Cigarette smoking (smoking ≥ 20
a risk factor for increased morbidity and mortality, cigarettes/day for last 6 months) and having history of
cardiovascular disease and malignancy.5 Despite these pregnancy in previous year or history of delivery
facts, most patients have a good prognosis if the within past six months and positive viral markers were
condition is caught in its early stages. excluded from the study. Approval of the ethical
committee of the institution was sought. Written
In published data, the mortality rate for coronary heart informed consent of the patients was taken.
disease in patients with NAFLD is equal to mortality
related to cirrhosis.6 It is important to determine OPERATIONAL DEFINITIONS:
whether NAFLD is an independent predictor of 1. NAFLD: was defined by the presence of at
cardiovascular morbidity and mortality and several least 2 of 3 abnormal findings on abdominal
studies have suggested that there is an association ultrasound: diffusely increased echogenicity
between NAFLD and cardiovascular disease.7 (bright) liver with liver echogenicity greater
NAFLD is the most common cause of abnormal liver than kidney or spleen, vascular blurring and
function tests in adults. There is no data available deep attenuation of ultrasound signal, after
locally regarding the role of carotid atherosclerosis in exclusion of significant alcohol intake (more
NAFLD patients. Furthermore, study of this kind was than 140g weekly in men and 70g weekly in
required for establishing if atherosclerosis affects women).
vascular anatomy and physiology in NAFLD patients, 2. Carotid intima-media thickness: Maximal
independent of other risk factors. Through this study, IMT was measured bilaterally at posterior
we would be able to find the relation between wall of common carotid artery, 2cm before
nonalcoholic fatty liver disease and carotid intima- the bifurcation as the distance between first
media thickness as the main predictor of (lumen-intima interface) and second (media-
cardiovascular disease, by comparing CIMT of adventitia interface) echogenic lines of
sonographically diagnosed NAFLD patients with anterior and posterior arterial walls. Three
control group having normal liver echogenicity on measurements were taken at each site and
ultrasound. Our study would provide baseline and average measurement used. The cut-off value
current local statistics of association between NAFLD for CIMT was set at 0.8 mm (CIMT ≥ 0.8mm
and raised CIMT. It would also help in deciding was considered raised).
whether further recommendations, with regards to
CIMT screening, should be implemented in all All the subjects were undergone abdominal and
NAFLD patients. Therefore, this study would be of carotid ultrasound in order to assess nonalcoholic fatty
clinical importance in planning prevention and liver disease and carotid IMT measurement. All
therapeutic strategies. investigations were performed by two consultant
sonologists (one performing abdominal ultrasound
MATERIAL AND METHODS: and the other doing carotid ultrasound) at radiology
This cross-sectional study was conducted at department, using standardized ultrasound equipment
Department of Medicine, Bahawal Victoria Hospital, and blinded to each other regarding respective
Bahawalpur from July 2019 to December 2019 over ultrasound measurements and unaware of patients’
the period of 6 months. Total 109 patients either male clinical data. Nonalcoholic fatty liver disease was
or female having age from 30-45 years having defined according to operational definition.
nonalcoholic fatty liver disease on ultrasound and with
HbsAg –ve, AntiHCV –ve were selected. One
www.iajps.com Page 101
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
For carotid ultrasound, patients were examined in a Age range in this study was from 30 to 45 years with
supine position, neck extended and chin facing mean age of 37.48 ± 4.04 years. The mean age in cases
contralateral side. Maximum CIMT was measured group was 37.51 ± 4.07 years and in control group was
bilaterally at posterior wall of common carotid artery, 37.45 ± 4.03 years. Majority of patients were 96
2cm before the bifurcation. Thickness of intima media (44.04%) were between 36-40 years of age as shown
was measured vertical to arterial wall. Three readings in Table I. The mean BMI in cases group was 29.64 ±
were recorded at each site and average measurement 4.19 kg/m2 and in control group was 29.62 ± 4.53 as
was used. The cut-off value for CIMT was set at 0.8 shown in Table II. Out of 218 patients, 136 (62.39%)
mm (CIMT ≥ 0.8mm was considered raised). were males and 82 (37.61%) were females with male
to female ratio of 1.7:1 (Figure I). Frequency of raised
All the collected data was entered in pre-designed CIMT in cases group was seen in 62 (56.88%) while
proforma along with demographic profile of all the in control group was seen in 41 (37.61%) cases as
patients. shown in Figure II which has shown p-value of 0.004
and odds ratio of 2.1879 which is statistically
Data was entered and analyzed using SPSS-11. significant and shows a positive association between
Descriptive statistics were applied to calculate mean NAFLD and raised CIMT.
and standard deviation for quantitative variables like
age and BMI. Frequencies and percentages were Stratification of raised CIMT with respect to age
calculated for qualitative variables like gender and groups has shown in Table III which showed
raised CIMT. Chi-square test was used to determine statistically significant association between NAFLD
the association between NAFLD and raised CIMT. p- and raised CIMT in age group 41-45 years. Table IV
value less than or equal to 0.05 (p ≤ 0.05) was has shown the stratification of raised CIMT with
considered as significant and odds ratio was also respect to BMI and showed statistically significant
calculated. Effect modifiers like age, gender and BMI association between NAFLD and raised CIMT in BMI
were controlled by stratification. Post stratification >30 kg/m2. Stratification of raised CIMT with respect
chi-square test was also applied and odds ratio was to gender is shown in Table V which showed
also calculated. statistically significant association between NAFLD
and raised CIMT in male gender.
RESULTS:
Table-I: Age distribution for both groups (n=218).
Cases (n=109) Controls (n=109) Total (n=218)
Age (years)
No. of patients %age No. of patients %age No. of patients %age
30-35 33 30.27 33 30.27 66 30.27
36-40 48 44.04 48 44.04 96 44.04
41-45 28 25.69 28 25.69 56 25.69
Mean ± SD 37.51 ± 4.07 37.45 ± 4.03 37.48 ± 4.04
Table-II: Percentage of patients according to BMI in both groups.
Cases (n=109) Controls (n=109) Total (n=218)
BMI (kg/m2)
No % N % No %
≤ 30 61 55.96 61 55.96 122 55.96
>30 48 44.04 48 44.04 96 44.04
Mean ± SD 29.64 ± 4.19 29.62 ± 4.53 29.63 ± 4.35
www.iajps.com Page 102
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
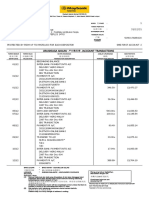
Figure-I: Percentage of patients according to Gender (n=218).
Figure II: Percentage of patients according to Raised CIMT between both Groups.
➢ P value is 0.004 which is statistically significant.
➢ Odds ratio is 2.1879 which is significant.
www.iajps.com Page 103
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
Table III: Stratification of Raised CIMT with respect to age groups.
Cases (n=109) Controls (n=109)
Age (years) Raised CIMT Raised CIMT P-value OR
Yes No Yes No
30-35 19 (57.58%) 14 (42.42%) 14 (42.42%) 19 (57.58%) 0.220 1.84
36-40 27 (56.25%) 21 (43.75%) 21 (43.75%) 27 (56.25%) 0.221 1.65
41-45 16 (57.14%) 12 (42.86%) 07 (25.0%) 21 (75.0%) 0.017 4.00
Table IV: Stratification of Raised CIMT with respect to BMI.
Cases (n=109) Controls (n=109)
BMI (kg/m2) Raised CIMT Raised CIMT P-value OR
Yes No Yes No
≤ 30 34 (55.74%) 27 (44.26%) 25 (40.98%) 36 (59.02%) 0.104 1.81
>30 28 (58.33%) 20 (41.67%) 16 (33.33%) 32 (66.67%) 0.015 2.80
Table V: Stratification of Raised CIMT with respect to Gender.
Cases (n=109) Controls (n=109)
Gender Raised CIMT Raised CIMT P-value OR
Yes No Yes No
Male 45 (55.74%) 23 (44.26%) 25 (40.98%) 43 (59.02%) 0.0007 3.36
Female 17 (58.33%) 24 (41.67%) 16 (33.33%) 25 (66.67%) 0.8219 1.12
DISCUSSION: to 35.8% of controls.12 Fracanzani et al13 concluded (in
We have conducted this case-control study to a series of normal and NAFLD subjects) that
determine the association between nonalcoholic fatty independent risk predictors of increased intima-media
liver disease (NAFLD) and raised carotid intima- thickness were the presence of hepatic steatosis (odds
media thickness. Age range in our study was from 30 ratio (OR) = 6.9), age (OR 6.0), and increased systolic
to 45 years with mean age of 37.48 ± 4.04 years. The blood pressure (OR 2.3).
mean age in cases group was 37.51 ± 4.07 years and in
control group was 37.45 ± 4.03 years. Majority of Zayed BE et al9 in his study has shown a significant
patients, 96 (44.04%) were between 36-40 years of increase in carotid IMT in patients of NAFLD (0.8
age. These results are very much comparable to the ±0.1) mm than normal control persons (0.6 ±0.03) mm
studies of Guleria A et al8 and Zayed BE et al9 who had which was highly significant (p=0.0001), which
reported mean age of 37 and 39 years respectively. On means that the patients with NAFLD may be at risk of
the other hand, many previous studies have shown early generalized atherosclerosis. Algarem NH et al10
much larger mean age i.e. greater than 50 years, as also found a significant increase in carotid IMT in
compared to our study.10-11 In initial studies of patients with NAFLD (0.73±0.1mm) than normal
NAFLD, the percentage of female patients was control persons (0.50±0.08mm) which was highly
reported to be as high as 75%; however, in subsequent significant (p value <0.001). Similarly, Guleria A et
studies, the percentage fell to roughly 50%. In our al8 had found the mean CIMT of both the right and left
study, 62.39% were males and 37.61% were females side significantly higher (0.70±0.11 mm vs. 0.61±0.08
with male to female ratio of 1.7:1. This male mm) (p=0.007) and FMD% significantly lower in
predominance is also found in many previous patients with NAFLD (9.79±3.81%) in comparison to
studies.10-11 controls (17.02±3.39%) (p<0.0001).
In our study, frequency of raised CIMT in cases group Despite the fact that several previous studies
was seen in 62 (56.88%) while in control group was demonstrated the association between NAFLD and
seen in 41 (37.61%) subjects which has shown p-value carotid IMT and/or carotid plaque, no general
of 0.004 and odds ratio of 2.1879 which is statistically consensus exists on the systematic screening of carotid
significant and shows a positive association between atherosclerosis in patients with fatty liver disease.
NAFLD and raised CIMT. In one study, CIMT was However, patients with NAFLD having increased
increased in 52.5% of patients with NAFLD compared carotid IMT could be candidates not only for
www.iajps.com Page 104
IAJPS 2020, 07 (10), 100-105 Fatima Safdar et al ISSN 2349-7750
aggressive treatment of the liver disease, but also for artherosclerosis in a large European
cholesterol lowering and aggressive treatment of population. Hepatology. 2009;49:1537–1544.
underlying CVD risk factors; this would help to 6. Mohammadi A, Habibpour H, Sedani HH,
modify and potentially decrease the global CVD risk Ghasemi-rad M. Evaluation of carotid intima-
of these patients. media thickness and flow-mediated dilatation
in middle-aged patients with nonalcoholic
CONCLUSION: fatty liver disease. Vasc Health Risk Manag.
This study concluded that that the frequency of raised 2011;7:661-65.
carotid intima-media thickness is higher in patients 7. Kang JH, Cho KI, Kim SM, Lee JY, Kim JJ,
with non-alcoholic fatty liver disease and shows the Goo JJ, et al. Relationship between
positive association between nonalcoholic fatty liver nonalcoholic fatty liver disease and carotid
disease (NAFLD) and raised carotid intima-media artery atherosclerosis beyond metabolic
thickness. So, we recommend that CIMT screening disorders in non-diabetic patients. J
should be implemented in all NAFLD patients and Cardiovasc Ultrasound. 2012;20(3):126-33.
patients with increased carotid IMT could be 8. Guleria A, Duseja A, Kalra N, Das A,
aggressively treated not only for liver disease but also Dhiman R, Chawla Y, et al. Patients with
for underlying CVD risk factors which will ultimately non-alcoholic fatty liver disease (NAFLD)
reduce the morbidity and mortality of these high-risk have an increased risk of atherosclerosis and
patients. cardiovascular disease. Tropical
Gastroenterol. 2013;34(2):74–82.
REFERENCES: 9. Zayed BE, El-Din SS, El-Mooatism E.
1. Mohammadi A, Bazazi A, Ghasemi-rad M. Association between Non Alcoholic Fatty
Evaluation of atherosclerotic findings in Liver Disease and Early Carotid
patients with nonalcoholic fatty liver disease. Atherosclerosis. Med J Cairo Univ.
Int J Gen Med. 2011;4:717-22. 2012;80(1):143-49.
2. Lankarani KB, Mahmoodi M, Lofti M, Zamiri 10. Algarem NH, Amin MA, Fawzi MM, Aiad AH.
N, Heydari ST, Ghaffarpasand F, et al. Carotid Intima Media Thickness (CIMT) in
Common carotid intima-media thickness in Nondiabetic Patients with non Alcoholic Fatty
patients with nonalcoholic fatty liver disease: Liver Disease (NAFLD). Med J Cairo Univ.
a population-based case-control study. 2011;79(1):491-96.
Korean J Gastroenterol. 2013;62:344-51. 11. Kim D, Choi SY, Park EH, Lee W, Kang JH,
3. Mishra S, Yadav D, Gupta M, Mishra H, Kim W, et al. Nonalcoholic Fatty Liver
Sharma P. A study of carotid atherosclerosis Disease Is Associated With Coronary Artery
in patients with nonalcoholic fatty liver Calcification. Hepatol. 2012;56(2):605-13.
disease. Ind J Clin Biochem. 2013;28(1):79- 12. Kang JH, Cho KI, Kim SM, Lee JY, Kim JJ,
83. Goo JJ, et al. Relationship between
4. Brea A, Mosquera D, Martin E, Arizti A, nonalcoholic fatty liver disease and carotid
Cordero JL, Ros E. Nonalcoholic fatty liver artery atherosclerosis beyond metabolic
disease is associated with carotid disorders in non-diabetic patients. J
atherosclerosis: a case-control study. Cardiovasc Ultrasound. 2012;20(3):126-33.
Arterioscler Thromb Vasc Biol. 13. Fracanzani AL, Burdick L, Raselli S. Carotid
2005;25:1045-50. artery intima-media thickness in
5. Gastaldelli A, Kozakova M, Hojlund K, et al. nonalcoholic fatty liver disease. Am J Med.
Fatty liver is associated with insulin resistance, 2008;121(1):72–8.
risk of coronary heart disease, and early
www.iajps.com Page 105
You might also like
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Semaglutide For The Treatment of Non Alcoholic Steatohepatitis Trial Design and Comparison of Non-Invasive BiomarkersDocument9 pagesSemaglutide For The Treatment of Non Alcoholic Steatohepatitis Trial Design and Comparison of Non-Invasive BiomarkersAntonio SalemeNo ratings yet
- Performance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseDocument8 pagesPerformance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseChausarPutraBenagilNo ratings yet
- Liver Fibrosis and Steatosis in Patients With Type 2 Diabetes Mellitus: A Transient Elastography StudyDocument5 pagesLiver Fibrosis and Steatosis in Patients With Type 2 Diabetes Mellitus: A Transient Elastography StudyIJAR JOURNALNo ratings yet
- IntJMedPublicHealth32111-7924347 220043Document0 pagesIntJMedPublicHealth32111-7924347 220043budi_26690No ratings yet
- Clinical Profile With Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome PatientsDocument7 pagesClinical Profile With Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome PatientsIJAR JOURNALNo ratings yet
- Elastografia Hepatica Transitoria Higado Graso No AlcoholicoDocument5 pagesElastografia Hepatica Transitoria Higado Graso No Alcoholicoalan obeth hipolito seguraNo ratings yet
- Ferraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundDocument12 pagesFerraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundThesisaurus IDNo ratings yet
- Crosstalk Between Nafld and CKD and Its Effect On EgfrDocument5 pagesCrosstalk Between Nafld and CKD and Its Effect On EgfrIJAR JOURNALNo ratings yet
- Differences in Nutritional Risk Assessment Between NRS2002, RFH-NPT and LDUST in Cirrhotic PatientsDocument8 pagesDifferences in Nutritional Risk Assessment Between NRS2002, RFH-NPT and LDUST in Cirrhotic PatientsMasna ArahmanNo ratings yet
- 11 134 v12n4 2013 PredictingPortalDocument11 pages11 134 v12n4 2013 PredictingPortalDevy Widiya GrafitasariNo ratings yet
- Hepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andDocument15 pagesHepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andjim.palmarbNo ratings yet
- Thesis Protocol: DNB General MedicineDocument30 pagesThesis Protocol: DNB General Medicinegattu santoshNo ratings yet
- Risk Factors Associated With Type 2 Diabetes Mellitus and The Frequency of Nafld Affected PatientsDocument5 pagesRisk Factors Associated With Type 2 Diabetes Mellitus and The Frequency of Nafld Affected PatientsIJAR JOURNALNo ratings yet
- Annals of HepatologyDocument10 pagesAnnals of HepatologyMedicina Preventiva Servicios Médicos UJATNo ratings yet
- Estimation of Lipid Profile and Glycemic Status and Liver Enzymes, Among Patients With Non-Alcoholic Fatty Liver DiseaseDocument13 pagesEstimation of Lipid Profile and Glycemic Status and Liver Enzymes, Among Patients With Non-Alcoholic Fatty Liver DiseaseIJAR JOURNALNo ratings yet
- Complete Resolution of Nonalcoholic Fatty LiverDocument32 pagesComplete Resolution of Nonalcoholic Fatty LiverRegir KurNo ratings yet
- Histopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisDocument18 pagesHistopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisLaia BertranNo ratings yet
- Chest: High Prevalence of Undiagnosed Airfl Ow Limitation in Patients With Cardiovascular DiseaseDocument8 pagesChest: High Prevalence of Undiagnosed Airfl Ow Limitation in Patients With Cardiovascular DiseaseRoberto Enrique Valdebenito RuizNo ratings yet
- The Perils of Fatty Liver Disease: Linical Aboratory EwsDocument20 pagesThe Perils of Fatty Liver Disease: Linical Aboratory EwsamirohkurniatiNo ratings yet
- Medical Ultrasonography July 2009 Vol 11 No 2 Page 15 18Document4 pagesMedical Ultrasonography July 2009 Vol 11 No 2 Page 15 18roxitanaNo ratings yet
- Clinical - Liver: Simple Noninvasive Systems Predict Long-Term Outcomes of Patients With Nonalcoholic Fatty Liver DiseaseDocument12 pagesClinical - Liver: Simple Noninvasive Systems Predict Long-Term Outcomes of Patients With Nonalcoholic Fatty Liver Disease走过一些路No ratings yet
- 2017 - Bansal - Corelation of HbA1c Levels and Duration of Diabetes With PADDocument4 pages2017 - Bansal - Corelation of HbA1c Levels and Duration of Diabetes With PADbuat nugas28No ratings yet
- Clinical Spectrum of Non-Alcoholic Fatty Liver Disease in Patients With Diabetes MellitusDocument13 pagesClinical Spectrum of Non-Alcoholic Fatty Liver Disease in Patients With Diabetes Mellitusblume diaNo ratings yet
- Pharmaceutical Sciences: Gastrointestinal Determinants Complications That in Cardiac ServicesDocument6 pagesPharmaceutical Sciences: Gastrointestinal Determinants Complications That in Cardiac ServicesiajpsNo ratings yet
- Bmri2019 3951574Document10 pagesBmri2019 3951574Anonymous 1EQutBNo ratings yet
- MSB 20188793 PDFDocument16 pagesMSB 20188793 PDFAndreea RoxanaNo ratings yet
- Adler 2015Document7 pagesAdler 2015nathaliepichardoNo ratings yet
- Diabetes & Metabolic Syndrome: Clinical Research & Reviews: Bladder Cancer With Pioglitazone: A Caseecontrol StudyDocument7 pagesDiabetes & Metabolic Syndrome: Clinical Research & Reviews: Bladder Cancer With Pioglitazone: A Caseecontrol StudyМалиша МанићNo ratings yet
- E000198 FullDocument6 pagesE000198 Fulljim.palmarbNo ratings yet
- Accepted Manuscript: Digestive and Liver DiseaseDocument28 pagesAccepted Manuscript: Digestive and Liver DiseaseMuhammad AdithiaNo ratings yet
- Non-Alcoholic Fatty Liver Disease in Patients With Type 2 - Tuong, Tran Thi Khanh Tran, Dang Khoa Phu, Pham Quang - Diagnostics, #3, 10, PagesDocument11 pagesNon-Alcoholic Fatty Liver Disease in Patients With Type 2 - Tuong, Tran Thi Khanh Tran, Dang Khoa Phu, Pham Quang - Diagnostics, #3, 10, PagesLigia AbdalaNo ratings yet
- Liver Transplant Candidates Have Impaired Quality of Life Ac 2020 Annals ofDocument7 pagesLiver Transplant Candidates Have Impaired Quality of Life Ac 2020 Annals oftatianacoronel1803No ratings yet
- Jamanetworkopen 2020 5143Document11 pagesJamanetworkopen 2020 5143Trần Quốc KhánhNo ratings yet
- Role of Carbohydrate Antigen (Ca19-9) and Carcinoembryonic Antigen (Cea) As A Prognostic Factors in Pancreatic CarcinomaDocument6 pagesRole of Carbohydrate Antigen (Ca19-9) and Carcinoembryonic Antigen (Cea) As A Prognostic Factors in Pancreatic CarcinomaIJAR JOURNALNo ratings yet
- 36-39 DevaDocument4 pages36-39 DevaEndhy KurniawanNo ratings yet
- Research: Non-Alcoholic Fatty Liver Disease and Mortality Among US Adults: Prospective Cohort StudyDocument9 pagesResearch: Non-Alcoholic Fatty Liver Disease and Mortality Among US Adults: Prospective Cohort StudyBuyungNo ratings yet
- Nafld Global PrevalenceDocument12 pagesNafld Global PrevalenceSvt Mscofficial2No ratings yet
- Sex-Related Relationships Between Uric Acid AnDocument8 pagesSex-Related Relationships Between Uric Acid Annguyenthanhluan2801No ratings yet
- Fibroscan 01Document8 pagesFibroscan 01AmiablePCNo ratings yet
- Prevalence and Pattern of Dyslipidemia in Hyperglycemic Patients and Its Associated Factors Among Pakistani PopulationDocument6 pagesPrevalence and Pattern of Dyslipidemia in Hyperglycemic Patients and Its Associated Factors Among Pakistani PopulationayazNo ratings yet
- Obs Jaundice AcceptedDocument8 pagesObs Jaundice AcceptedNovita ApramadhaNo ratings yet
- Clinical Outcomes and Mortality in Elderly Peritoneal Dialysis PatientsDocument6 pagesClinical Outcomes and Mortality in Elderly Peritoneal Dialysis PatientsbayuNo ratings yet
- Presentation 1Document15 pagesPresentation 1Sanjeevini KNo ratings yet
- NIH Public Access: Author ManuscriptDocument16 pagesNIH Public Access: Author Manuscriptgonzalo_acosta_6No ratings yet
- GHFBB 7 055Document8 pagesGHFBB 7 055RezaTiansahNo ratings yet
- Journal PresentationDocument7 pagesJournal PresentationShahin ShekhNo ratings yet
- Relationship Between Psoriasis and Non-Alcoholic Fatty Liver DiseaseDocument14 pagesRelationship Between Psoriasis and Non-Alcoholic Fatty Liver Diseaseimam mulyadiNo ratings yet
- 2018 - Article - 6627 SurvivalDocument10 pages2018 - Article - 6627 SurvivalMario OrtizNo ratings yet
- New Nomenclature For NAFLD - Understanding MASLD MetALD and Their Implications in Clinical PracticeDocument8 pagesNew Nomenclature For NAFLD - Understanding MASLD MetALD and Their Implications in Clinical Practiceguadalupe.cabrera.mdNo ratings yet
- Nejmoa 1912035Document11 pagesNejmoa 1912035Subhashini KNo ratings yet
- The Association Between Nonalcoholic Fatty Liver Disease and Stroke: Results From The Korean Genome and Epidemiology Study (Koges)Document11 pagesThe Association Between Nonalcoholic Fatty Liver Disease and Stroke: Results From The Korean Genome and Epidemiology Study (Koges)winnerfromparisNo ratings yet
- Assesmentof Fibro Q Test, AAR & APRI Indices As Markers of Fibrosis in Chronic Liver DiseaseDocument5 pagesAssesmentof Fibro Q Test, AAR & APRI Indices As Markers of Fibrosis in Chronic Liver Diseaseferdinan goutamaNo ratings yet
- NAFLD Current Concepts: Brief CommunicationDocument5 pagesNAFLD Current Concepts: Brief CommunicationdeepusebinNo ratings yet
- Prevalence of Hypertension Among Obese and Non-Obese Patients With Coronary Artery DiseaseDocument4 pagesPrevalence of Hypertension Among Obese and Non-Obese Patients With Coronary Artery DiseasePrinceTumbuktooNo ratings yet
- Non-Invasive Diagnosis of NASH and NAFLDDocument17 pagesNon-Invasive Diagnosis of NASH and NAFLDRaeni Dwi PutriNo ratings yet
- 2A17882Fd01 PDFDocument5 pages2A17882Fd01 PDFWahyuningsih HamidNo ratings yet
- Role of Diet in The Management of Carcinoid Syndrome Clinical Recommendations For Nutrition in Patients With Neuroendocrine TumorsDocument11 pagesRole of Diet in The Management of Carcinoid Syndrome Clinical Recommendations For Nutrition in Patients With Neuroendocrine TumorsDoc Nelson JuniorNo ratings yet
- JVS PublicationDocument8 pagesJVS PublicationMHS7No ratings yet
- Prognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaDocument8 pagesPrognostic Factors For Recurrence in Patients With Papillary Thyroid CarcinomaLeonardo LeónNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 195 Iajps195092020 PDFDocument5 pages195 Iajps195092020 PDFiajpsNo ratings yet
- 194 Iajps194092020 PDFDocument7 pages194 Iajps194092020 PDFiajpsNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 197 Iajps197092020 PDFDocument5 pages197 Iajps197092020 PDFiajpsNo ratings yet
- 196 Iajps196092020 PDFDocument4 pages196 Iajps196092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureDocument6 pagesPharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureiajpsNo ratings yet
- 192 Iajps192092020 PDFDocument5 pages192 Iajps192092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationDocument4 pagesPharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationiajpsNo ratings yet
- Pharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersDocument7 pagesPharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersiajpsNo ratings yet
- 191 Iajps191092020Document8 pages191 Iajps191092020iajpsNo ratings yet
- Pharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreDocument6 pagesPharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreiajpsNo ratings yet
- 50 Iajps50102020Document13 pages50 Iajps50102020iajpsNo ratings yet
- 44 Iajps44102020Document4 pages44 Iajps44102020iajpsNo ratings yet
- 40 Iajps40102020Document4 pages40 Iajps40102020iajpsNo ratings yet
- 46 Iajps46102020Document7 pages46 Iajps46102020iajpsNo ratings yet
- Pharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswlDocument6 pagesPharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswliajpsNo ratings yet
- 42 Iajps42102020Document8 pages42 Iajps42102020iajpsNo ratings yet
- Pharmaceutical SciencesDocument5 pagesPharmaceutical SciencesiajpsNo ratings yet
- Pharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationDocument4 pagesPharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationiajpsNo ratings yet
- Pharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistanDocument5 pagesPharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistaniajpsNo ratings yet
- Pharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleDocument6 pagesPharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleiajpsNo ratings yet
- Pharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationDocument12 pagesPharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationiajpsNo ratings yet
- 35 Iajps35102020Document4 pages35 Iajps35102020iajpsNo ratings yet
- 33 Iajps33102020Document6 pages33 Iajps33102020iajpsNo ratings yet
- Pharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaDocument3 pagesPharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaiajpsNo ratings yet
- 34 Iajps34102020Document7 pages34 Iajps34102020iajpsNo ratings yet
- 37 Iajps37102020Document9 pages37 Iajps37102020iajpsNo ratings yet
- Pharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsDocument8 pagesPharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsiajpsNo ratings yet
- Pharmaceutical Sciences: Massive Inguinal Hernia-A Rare Presentation of Common DiseaseDocument4 pagesPharmaceutical Sciences: Massive Inguinal Hernia-A Rare Presentation of Common DiseaseiajpsNo ratings yet
- MANILA HOTEL CORP. vs. NLRCDocument5 pagesMANILA HOTEL CORP. vs. NLRCHilary MostajoNo ratings yet
- Palma vs. Fortich PDFDocument3 pagesPalma vs. Fortich PDFKristine VillanuevaNo ratings yet
- Marimba ReferenceDocument320 pagesMarimba Referenceapi-3752991No ratings yet
- Kangar 1 31/12/21Document4 pagesKangar 1 31/12/21TENGKU IRSALINA SYAHIRAH BINTI TENGKU MUHAIRI KTNNo ratings yet
- Los Angeles County Sheriff's Department InvestigationDocument60 pagesLos Angeles County Sheriff's Department InvestigationBen Harper0% (1)
- Katyusha Rocket LauncherDocument7 pagesKatyusha Rocket LauncherTepeRudeboyNo ratings yet
- Thesis - Behaviour of Prefabricated Modular Buildings Subjected To Lateral Loads PDFDocument247 pagesThesis - Behaviour of Prefabricated Modular Buildings Subjected To Lateral Loads PDFFumaça FilosóficaNo ratings yet
- Fallacy of Subjectivity:: ExamplesDocument2 pagesFallacy of Subjectivity:: ExamplesKaustav MannaNo ratings yet
- MAraguinot V Viva Films DigestDocument2 pagesMAraguinot V Viva Films DigestcattaczNo ratings yet
- Lista Destinatari Tema IDocument4 pagesLista Destinatari Tema INicola IlieNo ratings yet
- Math Grade 7 Q2 PDFDocument158 pagesMath Grade 7 Q2 PDFIloise Lou Valdez Barbado100% (2)
- Econ 281 Chapter02Document86 pagesEcon 281 Chapter02Elon MuskNo ratings yet
- Multiple Effect EvaporatorDocument4 pagesMultiple Effect EvaporatorKusmakarNo ratings yet
- Argumentative EssayDocument5 pagesArgumentative EssayParimalar D/O RathinasamyNo ratings yet
- The Prediction of Travel Behaviour Using The Theory of Planned BehaviourDocument16 pagesThe Prediction of Travel Behaviour Using The Theory of Planned Behaviourhaneena kadeejaNo ratings yet
- Sperber Ed Metarepresentations A Multidisciplinary PerspectiveDocument460 pagesSperber Ed Metarepresentations A Multidisciplinary PerspectiveHernán Franco100% (3)
- Computer Education in Schools Plays Important Role in Students Career Development. ItDocument5 pagesComputer Education in Schools Plays Important Role in Students Career Development. ItEldho GeorgeNo ratings yet
- Assessment of Loan Repayment Performance: in Case of Awash Bank in Sikela BranchDocument9 pagesAssessment of Loan Repayment Performance: in Case of Awash Bank in Sikela Branchbundesa buzo100% (1)
- Delivery ReceiptDocument28 pagesDelivery Receiptggac16312916No ratings yet
- Molecular Docking Terhadap Senyawa Kurkumin Dan Arturmeron Pada Tumbuhan Kunyit (Curcuma Longa Linn.) Yang Berpotensi Menghambat Virus CoronaDocument7 pagesMolecular Docking Terhadap Senyawa Kurkumin Dan Arturmeron Pada Tumbuhan Kunyit (Curcuma Longa Linn.) Yang Berpotensi Menghambat Virus Coronalalu reza rezki muanggaraNo ratings yet
- LGBT in Malaysia: Social Welfare SystemDocument24 pagesLGBT in Malaysia: Social Welfare SystemMuhammad Syazwan Ahmad Fauzi100% (1)
- Measures of Variability For Ungrouped DataDocument16 pagesMeasures of Variability For Ungrouped DataSharonNo ratings yet
- A Brief History: The Four Waves of FeminismDocument2 pagesA Brief History: The Four Waves of FeminismMuHammAD ShArjeeLNo ratings yet
- The VerdictDocument15 pagesThe VerdictEbuka sixtusNo ratings yet
- Rajiv Gandhi Govt. Polytechnic Itanagar (A.P) : Web Page DesigningDocument13 pagesRajiv Gandhi Govt. Polytechnic Itanagar (A.P) : Web Page Designingkhoda takoNo ratings yet
- Labor Law Review Midterm Exercise 2ndsem 2017-2018Document17 pagesLabor Law Review Midterm Exercise 2ndsem 2017-2018MaeJoyLoyolaBorlagdatanNo ratings yet
- Chicago Citation and DocumentDocument8 pagesChicago Citation and DocumentkdemarchiaNo ratings yet
- Marcos v. CADocument2 pagesMarcos v. CANikki MalferrariNo ratings yet
- Dirac Equation Explained at A Very Elementary LevelDocument16 pagesDirac Equation Explained at A Very Elementary Levelsid_senadheera100% (2)
- Ingo Plag Et AlDocument7 pagesIngo Plag Et AlDinha GorgisNo ratings yet