Professional Documents
Culture Documents
Jurnal Rindang 3 PDF
Uploaded by
Rindang Cahyani AbasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Rindang 3 PDF
Uploaded by
Rindang Cahyani AbasCopyright:
Available Formats
Hilton and Article
Original Hölmich 331
Full- or Split-Thickness Skin Grafting in Scalp
Surgery? Retrospective Case Series
Carolina Maria Helena Hilton1*, Lisbet Rosenkrantz Hölmich2
1. Department of Oncology, Rigshospitalet, ABSTRACT
København Ø, Denmark;
2. Lisbet Rosenkrantz Hölmich, Department BACKGROUND
of Plastic Surgery, Herlev Gentofte
University Hospital, Copenhagen
Closure of skin defects after scalp surgery may be accomplished by
University, Herlev, Denmark grafting; either split- or full-thickness. Both methods are used in
Denmark, and the optimal approach on scalp defects without exposed
bone is not known. This study aimed to investigate if the two methods
were equal regarding graft take as primary outcome and as secondary
outcomes complications and number of outpatient visits/ number of
days from surgery until the last outpatient visit for the recipient site
(as a proxy for time to healing), hypothesizing that they were.
METHODS
The present retrospective single-center case series reported our
experience using the two types of skin grafts after scalp surgery
in the inclusion period from 1.1.2014 to 30.09.2015. Data were
analyzed according to graft type with a full-thickness skin graft
(FTSG-group) or a split-thickness skin graft (STSG-group).
RESULTS
In the inclusion period, 106 patients had surgery (28 with a FTSG
and 78 with a STSG). Irrespectively of which skin graft that was
used, we found no statistically significant difference regarding
percentage of adherence, complications or number of outpatient
visits and time from operation until last outpatient visit regarding
the recipient site (p>0.05).
CONCLUSION
Our findings supported that use of either FTSG or STSG in scalp
lesions were equal choices.
KEYWORDS
Full thickness; Split thickness; Scalp surgery; Skin; graft;
*Corresponding Author: Transplant
Carolina Maria Helena Hilton, MD,
Department of Plastic Surgery Herlev Please cite this paper as:
Gentofte University Hospital, Hilton CMH, Hölmich LR. Full- or Split-Thickness Skin Grafting
Copenhagen University, in Scalp Surgery? Retrospective Case Series. World J Plast Surg
Herlev Ringvej 75, 2730, 2019;8(3):331-337. doi: 10.29252/wjps.8.3.331.
Herlev, Denmark.
Department of Oncology,
INTRODUCTION
Rigshospitalet, Blegdamsvej 9,
2100 København Ø, Denmark (New Scalp surgery for skin tumors often produces defects larger than
affiliation) what can be closed directly and therefore, reconstructive surgery
Tel: +4581197044
is necessary. Multiple methods of reconstruction are available,
Email: carro_hilton@hotmail.com
Received: July 4, 2018 including free flaps, local advancement flaps and skin grafting.1–4
Revised: June 8, 2019 Either a full-thickness skin graft (FTSG) or a split-thickness skin
Accepted: June 14, 2019 graft (STSG) may be employed. FTSGs are usually harvested
www.wjps.ir /Vol.8/No.3/September 2019
332 Skin grafting in scalp surgery
from the groin, the upper inner arm and the The possibility to mesh (to make holes in)
supraclavicular fossa or, for scalp surgery, the this type of graft makes it able to cover larger
adjacent scalp.5 areas than the size of the graft first harvested.
STSGs are usually harvested from the upper Skin graft contraction occur in two stages;
anterior or lateral thighs, but almost any body primary and secondary contraction. Primary
region can be used if necessary. After harvest at contraction, which is greater in a FTSG, refers
the donor site, the graft is applied to the defect to the immediate reduction in size after harvest
and a dressing is placed over to secure contact and secondary contraction, which is greater in a
with the wound bed and prevent bleeding and STSG, refers to wound bed contraction.10
formation of hematoma by providing slight This contraction can work in advantage for
compression. The dressing is held in place the patient over the long term by decreasing the
using either sutures or staples, and remains grafted area over time. A relative contraindication
until the patient arrives for the first outpatient exists for the use of a STSG over joints or where
visit, typically on the fourth-seventh day after contractures must be avoided. However, it
surgery.5 remains a necessary tool for larger defects, for
For scalp-surgery, including region-parietalis, example burn-wounds.10 Both types of grafts
region-occipitalis and the postauricular area, leave a difference in skin level, which is slightly
surgeons use either a STSG or a FTSG as more in STSG, and this graft is also more prone
opposed to the facial area or the hand where a to dryness afterwards, since sebaceous glands
FTSG is most commonly used due to cosmetic are not transferred with the graft.10
and functional reasons.5 Limited donor areas for There are no recommendations regarding
FTSG can be a reason for using STSG. There are which method is the most optimal to use on
a number of advantages and disadvantages with the scalp, and both are used in Denmark. The
the two types of grafts. The usage of a FTSG present study reported our experience with
leaves the donor area to be closed by suturing, patients receiving the two types of skin grafts
stapling or in rare cases with a split-thickness after scalp-surgery with excision of a skin tumor.
skin graft.6-9 The hypothesis was that the two methods were
FTSGs heal with a better cosmetic and equal regarding graft take and complications.
functional result, give better coverage and
have less secondary contraction, but require MATERIALS AND METHODS
substantial nourishment, which leaves them
vulnerable to insufficient vascularization.6–9 The present study is a retrospective single-center
An inadequate wound bed is a major factor case series including patients undergoing full-
affecting especially FTSG take, which with thickness or split-thickness skin grafting after
its added thickness places higher demands scalp surgery for skin tumors during the period
regarding nourishment and revascularisation.10 of 01.01.2014 and 30.09.2015. Patients were
STSGs have better initial take, larger donor site identified through the local hospital database
availability, and, in the scalp, contraction can be using treatment codes for excision of a tumor on
useful to decrease the size of the scar /alopecia.10 the head or neck, full thickness skin graft and
A STSG is harvested from the donor area split thickness skin graft. The study complies
with a dermatome (a surgical instrument used with the declaration of Helsinki.
to produce thin slices of skin) and the donor area The primary outcome was percentage of
is left for re-epithelialization. A reason for using skin graft adherence. Secondary outcomes were
this type of graft for skin cancer patients is that complications and number of outpatient visits/
they often present with recurring skin cancer, number of days from surgery until the last
requiring more surgery and therefore it could be outpatient visit for the recipient site (as a proxy
argued to leave their full skin graft reserves for for time to healing). Results were analyzed
tumors located in the face. In this study we did according to FTSGs and STSGs. Inclusion
not consider the cosmetic aspect of what graft criteria were surgery for a skin tumor in region-
to use.10 parietalis, region-occipitalis, the postauricular-
The scalp is an area where the cosmetic or scalp-area leaving a defect that was either
and functional result is often of not as great covered with a split-thickness or a full-thickness
importance as other areas, e.g. the face or hands. skin graft.
www.wjps.ir /Vol.8/No.3/September 2019
Hilton and Hölmich 333
If the patient had more than one surgery a full-thickness skin graft (FTSG-group) or a
during the period, we only included the initial split-thickness skin graft (STSG-group). Data
one, and in case of simultaneous tumors, the are presented as number of patients and median
largest was included. A diversity of tumors was (ranges). Fisher´s exact test and Chi-Square test
represented among the patients screened for were used for categorical data, Mann-Whitney
inclusion. The diagnosis was not considered to U for ordinal or continuous data, and 95%
influence what type of skin graft was used, nor confidence intervals as appropriate. A p value
the course of healing after excision of the tumor. <0.05 was considered significant. All statistics
We did not include region-frontalis in this study were done using SPSS software (Version 21.0,
since this in many cases could be located in the IBM, New York, USA).
face area rather than on the scalp, and a FTSG
is almost always used in the facial area, if not a RESULTS
local flap.
Exclusion criteria were missing description The medical records of 106 patients were
of the primary lesion, missing follow-up to last reviewed. There were 28 patients receiving a
planned outpatient visit or if the patient had a full-thickness (FTSG-group) and 78 a split-
chronic wound after previous surgery in the thickness skin graft (STSG-group). Patient
area. Data on demographics, site of pathology, demographics were shown in Table 1. There
skin tumor diagnosis, ulceration or infection were no differences with statistical significance
before surgery, longest excision diameter (as a between the two study groups. There was a trend
proxy for excision area, since this was not always towards more men getting FTSGs, smokers were
known), donor site location, length of hospital more likely to get a STSG, people with previous
stay, complications, number of outpatient visits, radiation or recent chemotherapy got exclusively
time from operation until the last outpatient STSGs and larger defects were treated with
visit at the plastic surgery department, previous STSG.
radiation therapy to the recipient area or Preoperative data, surgical information and
chemotherapy within a month prior to surgery tumor diagnosis are shown in Table 2. There was
were obtained from hospital files. no significant difference in preoperative status of
Infection before surgery was defined as cases the patients with regard to infection or ulceration
where antibiotics were prescribed preoperatively. of the tumor before surgery. The FTSG-group
Data were analyzed according to grafting with had a median excision of 3.0 (1.5-5.0) cm and
Table 1: Patient demographics
FTSG-group STSG-group p value
(n=28) (%) (n=78) (%)
Age (years, range) 81 (59-93) 78 (37-104) 0.69
Gender
- Female 5 (17.9) 19 (24.4) 0.60
- Male 23 (82.1) 59 (75.6)
Smoking
- Yes 1 (3.6) 9 (11.5) 0.32
- No 20 (71.4) 45 (57.7)
- Previously 7 (25.0) 24 (30.8)
Alcohol abuse 5 (17.9) 12 (15.4) 0.77
Chronic Obstructive Lung Disease 2 (7.1) 4 (5.1) 0.65
Hypertension 21 (75.0) 43 (55.1) 0.08
Heart disease 9 (32.1) 21 (26.9) 0.63
Diabetes mellitus 2 (7.1) 3 (3.8) 0.61
Hypothyroidism 0 (0) 5 (6.4) 0.32
Immunosuppression 3 (10.7) 10 (12.8) 1.00
Radiation therapy 0 (0) 5 (6.4) 0.32
Chemotherapy 0 (0) 1 (1.3) 1.00
Patient demographics in the full thickness skin graft group (FTSG-group) and the split thickness skin graft group
(STSG-group)
www.wjps.ir /Vol.8/No.3/September 2019
334 Skin grafting in scalp surgery
Table 2: Preoperative data, surgical information and diagnosis
FTSG-group STSG-group p value
(n=28) (%) (n=78) (%)
Tumor with ulceration 14 (50.0) 47 (60.3) 0.38
Tumor region
- Regio-parietalis 5 (17.9) 9 (11.5) 0.01
- Regio-occipitalis 3 (10.7) 2 (2.6)
- Post-auricular area 5 (17.9) 3 (3.8)
- Scalpa 15 (53.6) 64 (82.1)
Longest excision (cm, range) 3.0 (1.5-5.0) 4.0 (2.0-17.5) 0.001
Excision to
- Galea fascia 16 (57.1) 24 (31.6) 0.02
- Pericranium 12 (42.9) 52 (68.4)
- Missing information 2
Donor site
- Split thickness, thigh 19 (67.9) 78 (100.0)
- Full thickness, clavicular area 2 (7.1)
- Full thickness, ear-area 7 (25)
- Full thickness, arm
Transplant fixation
- Stapled 0 (0) 2 (2.6) 1.00
- Sutures 28 (100) 76 (97.4)
Inner dressing
- Euflavine 4 (14.3) 7 (9.0) 0.75
- Nitrofuranzoin 22 (78.6) 64 (82.1)
- Jelonet 24 (85.7) 67 (85.9)
Outer dressing
- Foam cloth 11 (40.7) 27 (35.1) 0.01
- Absorbent foam 16 (59.3) 50 (64.9)
- Missing information 1 1
Fixation of dressing
- Sutured 27 (96.4) 58 (74.4) 0.19
- Stapled 1 (3.6) 20 (25.6)
Diagnosis
Basal cell carcinoma 14 (50) 23 (29.9)
Squamos cell carcinoma 10 (35.7) 30 (39.0)
Malignant melanoma 1 (3.6) 9 (11.7)
Other tumors 3 (10.7) 15 (19.5)
Missing information 1
Preoperative data, surgical information and diagnosis from the full thickness skin graft group (FTSG-group) and
the split thickness skin graft group (STSG-group).
a: scalp region, not otherwise specified
the STSG-group had a median excision of 4.0 dressing-materials. Data regarding healing
(2.0-17.5) cm (p=0.001). There was a significant and complications are shown in Table 3. In the
difference between the two groups regarding FTSG-group, 22 (78.6%) of the patients had a
excision to galea fascia or pericranium. In the graft take of 90-100% at the date of unpacking
FTSG-group, 16 (57.1%) of the patients had an of the dressing, 4 (14.3%) of 60-90%, 1 (3.6%)
excision to the galea fascia and 12 (42.9%) to of 30-60% and 1 (3.6%) of <30%. Two patients
the pericranium as opposed to 24 (31.6%) and (7.1%) had full necrosis of the skin graft with
52 (68.4%) patients in the STSG-group. For 84 one of them undergoing a second skin grafting
(79.2%) of the patients, two of the following and the other one was left to secondary healing
materials were used as inner layers in the (Table 3).
dressing; euflavine, jelonet and nitrofuranzoin. Two patients (7.1%) were treated with
There was no difference between the two antibiotics due to postoperative infection. One
groups regarding distribution of the different patient developed a hematoma. In the STSG-
www.wjps.ir /Vol.8/No.3/September 2019
Hilton and Hölmich 335
Table 3: Healing and complications
FTSG-group STSG-group p value
(n=28) (%) (n=78) (%)
Recipient site
- % of adherence
• 90-100 22 (78.6) 64 (82.1) 0.75
• 60-90 4 (14.3) 6 (7.7)
• 30-60 1 (3.6) 4 (5.1)
• <30 1 (3.6) 4 (5.1)
Surgical complications
- Full loss of skin transplant 2 (7.1) 2 (2.6) 0.28
• Retransplantation 1 (3.6) 1 (1.3) 0.46
• Secondary healing 1 (3.6) 1 (1.3) 0.46
- Reoperation (not full loss) 0 (0) 1 (1.3) 1.00
- Infection treated with antibiotics 2 (7.1) 8 (10.3) 1.00
- Hematoma 1 (3.6) 2 (2.6) 1.00
- Seroma 0 (0) 5 (6.4) 0.32
- Overall complication rate 5 (17.9) 18 (23.1) 0.79
Donor site
- Checked by a general practitioner or 19 (67.9) 49 (62.8) 0.82
nurse health visitor
Surgical complications
- Necrosis 0 (0) 1 (1.3) 1.00
- Wound rupture 1 (3.6) 0 (0) 1.00
- Infection treated with antibiotics/ 1 (3.6) 4 (5.1) 1.00
flamazine/biatain Ag
- Hematoma 0 (0) 1 (1.3) 1.00
Hospital stay (days, range) 0 (0-2) 0 (0-4) 0.10
Re-hospitalization (days, range) 0 (0-0) 0 (0-11) 0.55
- Missing information 1
Number of outpatient visits (no, range) 1 (1-14) 2 (1-14) 0.43
- Missing information 1 2
Time from operation until last outpatient visit, 7 (4-191) 10.5 (4-330) 0.97
recipient site/”healing” (days, range)
- Missing information 1 2
Time from operation until last outpatient 6 (4-16) 14 (11-56) 0.001
visit/”healing”, donor site (days, range)
- Missing information 21 55
Healing and complications for the full thickness skin graft group (FTSG-group) and the split thickness skin graft
group (STSG-group) after scalp surgery
group, 64 (82.1%) of the patients had a graft Overall complication rate was 5 (17.9%) in
take of 90-100%, 6 (7.7%) of 60-90%, 4 (5.1%) the FTSG-group and 18 (23.1%) in the STSG-
of 30-60% and 4 (5.1%) of <30%. Two (2.6%) of group (p=0.79). At the donor site, one patient
the patients had a full necrosis of the skin graft in the FTSG-group had wound dehiscence. One
with 1 (1.3%) of them undergoing a second skin (3.6%) in the FTSG-group had infection of the
grafting and 1 (1.3%) left to secondary healing. donor site treated with antibiotics as opposed to
Eight (10.3%) of the patients were treated with 4 (5.1%) in the STSG-group, who were treated
antibiotics due to postoperative infection. with Flamazine or Biatain Ag dressing.
Two (2.6%) patients developed a hematoma In the STSG-group, there was registered
and 5 (6.4%) a seroma. There was no significant that one patient (1.3%) developed a hematoma
difference between the two groups regarding and one had partial necrosis of the donor site.
graft adherence and surgical complications. There was no statistically significant difference
www.wjps.ir /Vol.8/No.3/September 2019
336 Skin grafting in scalp surgery
in donor site complications between the two significant advantage regarding graft failure,
groups. Duration of hospital stay had a median graft contraction, hyperpigmentation, altered
of 0 (0-2) days in the FTSG-group and 0 (0-4) sensation, infection rate and hospital stay.
in the STSG-group (p=0.10). Duration of re- In the process of deciding what graft to
hospitalization had a median of 0 (0-0) days in use potential complications, cosmetics of the
the FTSG-group and 0 (0-11) in the STSG-group donor and recipient site and patient satisfaction
(p=0.55). The number of outpatient visits was 1 should all be considered, where the last part
(1-14) and 2 (1-14) in the FTSG-group and the was not analyzed in this study. Hereafter,
STSG-group, respectively (p=0.43). Time from practical matters such as draping of the patient
surgery until the last outpatient visit for wound during surgery could also be determinant for
care was 7 days (4-191) in the FTSG-group and the chosen graft and at last, with no difference
10.5 days (4-330) in the STSG-group (p=0.97). in complications between the two groups,
recommendations of which skin graft to use
DISCUSSION could also be based on the economical aspect;
the costs of the surgery.
In the present study there were no significant Our main limitation is the retrospective nature
statistical difference regarding preoperative data, of our study, leaving it vulnerable to confounding
adherence of the skin graft, complications or by indication, i.e. the surgeons could have been
overall complication ratio. There was a significant choosing STSG for complicated cases. If that
difference concerning length and depth of the was the case, STSG could be superior to FTSG.
excision and also regarding the time from surgery However, this cannot be determined from
until the last outpatient visit of the donor site, but the present study. Furthermore, most patients
not for the recipient site. We found a significant were followed up at their General Practitioner
difference with the longest excision diameter in concerning their donor site, from where we do
the split-thickness group and a larger percentage not have data. However, we expect these cases to
with deeper excision, to the pericranium, in the be rather uncomplicated, otherwise they should
split-thickness skin graft group. have been referred back to the department.
This is most likely a matter of confounding by Finally, due to the small number of patients
indication: larger size defects call for larger skin in our case series, rare complications might
grafts and STSG would more often be chosen in not have been seen. Cosmetics and patient
such cases. Deeper defects can be at risk of more satisfaction could be analyzed retrospectively,
healing problems due to a less vascularized although, given the limitations of a retrospective
wound bed, and in such cases most surgeons study, only a randomized controlled study will
would probably chose STSG over FTSG. The be able to examine if the two procedures are
pericranium is though well vascularized, and no really equal. In conclusion we could not find any
real contraindication for using a STSG. significant difference regarding graft take with
The time from surgery until the last outpatient the use of either FTSG or STSG in scalp defects,
visit at the plastic surgery department could be which is reassuring.
seen as a proxy for the healing progress. We
found no difference regarding the recipient site, CONFLICT OF INTEREST
but a significant difference regarding the donor
site with a longer time for a split skin thickness The authors declare no conflict of interest.
graft. There were though missing data from
over 50% of the patients in each group and most REFERENCES
donor sites got controlled by the patients general
practitioner. 1 Eck DL, Koonce SL, Al Majed BM, Perdikis
Wellington et al.11 found in their analysis of G. Evaluation of options for large scalp defect
31 patients with STSG and 16 with FTSG for reconstruction: a 12-year experience. Eplasty
coverage after radial forearm free flap harvest, 2014;14:e10.
no significant difference in time to healing 2 Newman MI, Hanasono MM, Disa JJ, Cordeiro
at the donor site. Al Shlash et al.12 found in PG, Mehrara BJ. Scalp reconstruction:
their study with 85 burn patients who received a 15-year experience. Ann Plast Surg
STSG (56 cases) and FTSG (29 cases) no 2004;52:501-6; discussion 6. doi: 10.1097/01.
www.wjps.ir /Vol.8/No.3/September 2019
Hilton and Hölmich 337
sap.0000123346.58418.e6. 8 Kim TB, Moe KS, Eisele DW, Orloff LA,
3 Leedy JE, Janis JE, Rohrich RJ. Wang SJ. Full-thickness skin graft from the
Reconstruction of acquired scalp defects: groin for coverage of the radial forearm free
an algorithmic approach. Plast Reconstr flap donor site. Am J Otolaryngol 2007;28:325-
Surg 2005;116:54e-72e. doi: 10.1097/01. 9. doi: 10.1016/j.amjoto.2006.10.009.
prs.0000179188.25019.6c. 9 Lutz BS, Wei FC, Chang SC, Yang KH, Chen
4 Desai SC, Sand JP, Sharon JD, Branham G, IH. Donor site morbidity after suprafascial
Nussenbaum B. Scalp reconstruction: an elevation of the radial forearm flap: a
algorithmic approach and systematic review. prospective study in 95 consecutive cases.
JAMA Facial Plast Surg 2015;17:56-66. doi: Plast Reconstr Surg 1999;103:132-7. doi:
10.1001/jamafacial.2014.889. 10.1097/00006534-199901000-00021.
5 Schwanholt C, Greenhalgh DG, Warden 10 Landau AG, Hudson DA, Adams K,
GD. A comparison of full-thickness versus Geldenhuys S, Pienaar C. Full-thickness skin
split-thickness autografts for the coverage of grafts: maximizing graft take using negative
deep palm burns in the very young pediatric pressure dressings to prepare the graft bed.
patient. J Burn Care Rehabil 1993;14:29-33. Ann Plast Surg 2008;60:661-6. doi: 10.1097/
doi: 10.1097/00004630-199301000-00008 . SAP.0b013e318146c288.
6 Prasetyono TO, Sadikin PM, Saputra DK. 11 Davis WJ, 3rd, Wu C, Sieber D, Vandevender
The use of split-thickness versus full- DK. A comparison of full and split thickness
thickness skin graft to resurface volar aspect skin grafts in radial forearm donor sites. J
of pediatric burned hands: A systematic Hand Microsurg 2011;3:18-24. doi: 10.1007/
review. Burns 2015;41:890-906. doi: 10.1016/j. s12593-011-0036-9.
burns.2015.01.011. 12 Shlash SO, Madani JO, Deib JI, Alsubhi
7 Kim S, Chung SW, Cha IH. Full thickness skin FS, Saifi SS, Helmi AM, Al-Mutairi SK,
grafts from the groin: donor site morbidity and Khurram JA. Demographic characteristics
graft survival rate from 50 cases. J Korean and outcome of burn patients requiring skin
Assoc Oral Maxillofac Surg 2013;39:21-6. grafts: a tertiary hospital experience. Int J
doi: 10.5125/jkaoms.2013.39.1.21. Burns Trauma 2016;6:30-6.
www.wjps.ir /Vol.8/No.3/September 2019
You might also like
- Graft Selection: Full-Thickness Skin GraftDocument8 pagesGraft Selection: Full-Thickness Skin GraftIkhsanNo ratings yet
- Analyzing Contraction of Full Thickness Skin Grafts in Time: Choosing The Donor Site Does MatterDocument6 pagesAnalyzing Contraction of Full Thickness Skin Grafts in Time: Choosing The Donor Site Does MatterFelix Hadi NainggolanNo ratings yet
- Skin Graft: Technique, Indications and OutcomesDocument9 pagesSkin Graft: Technique, Indications and OutcomesIJAR JOURNALNo ratings yet
- Full-Thickness Skin Grafting in Nasal ReconstructionDocument6 pagesFull-Thickness Skin Grafting in Nasal ReconstructionMuhammad FaizalNo ratings yet
- Lee 2015Document7 pagesLee 2015AncaVerdesNo ratings yet
- Ijomi 15 415Document4 pagesIjomi 15 415Bagis Emre GulNo ratings yet
- 20SPIGCDocument3 pages20SPIGCscribullNo ratings yet
- Treatment of Extensive Postburn Deformities Using Extralarge Sheets of Full Thickness Skin GraftsDocument8 pagesTreatment of Extensive Postburn Deformities Using Extralarge Sheets of Full Thickness Skin GraftsIndah YulantariNo ratings yet
- Skin Graft Techniques Khan2020Document15 pagesSkin Graft Techniques Khan2020danielNo ratings yet
- 3 s2.0 B9781416003168500144 MainDocument10 pages3 s2.0 B9781416003168500144 MainRashmeeta ThadhaniNo ratings yet
- Flaps in Maxillofacial ReconstructionDocument29 pagesFlaps in Maxillofacial ReconstructionJaspreet Kaur33% (3)
- Tom Skin-Sparing Approach To Treatemen of NSTI 2016Document14 pagesTom Skin-Sparing Approach To Treatemen of NSTI 2016Sadaf Raisa KhanNo ratings yet
- Parotidectomy For Benign Parotid Tumors: An Aesthetic ApproachDocument6 pagesParotidectomy For Benign Parotid Tumors: An Aesthetic ApproachamelNo ratings yet
- 2015 - A New Technique For Increasing Keratinized Tisue Around Dental Implants. The Partialy Epithelialized Free Conective Tisue Graft. Retrospective Analysis of A Case Series - Eberhard FrischDocument7 pages2015 - A New Technique For Increasing Keratinized Tisue Around Dental Implants. The Partialy Epithelialized Free Conective Tisue Graft. Retrospective Analysis of A Case Series - Eberhard FrischJose LuisNo ratings yet
- PDF JTN 2170Document9 pagesPDF JTN 2170RathavishwarajNo ratings yet
- SKin GraftDocument19 pagesSKin GraftRinna Numberi,MDNo ratings yet
- Reconstructive Options For The Neck After Resection of Cutaneous MalignanciesDocument10 pagesReconstructive Options For The Neck After Resection of Cutaneous MalignanciesAlvaro Carlos Calvo ValenciaNo ratings yet
- Adams 2006Document13 pagesAdams 2006AncaVerdesNo ratings yet
- BEDAH (Skin Graft)Document7 pagesBEDAH (Skin Graft)Jose FoxNo ratings yet
- Dermal SubstitutesDocument9 pagesDermal SubstitutesEsq. Nelson OduorNo ratings yet
- Aps 39 118Document8 pagesAps 39 118isabelNo ratings yet
- Comparison of Incisional Delay Patterns On A Rat Random Flap ModelDocument8 pagesComparison of Incisional Delay Patterns On A Rat Random Flap ModelonderhuseyinbasNo ratings yet
- Direct-To-Implant Breast ReconstructionDocument3 pagesDirect-To-Implant Breast ReconstructionCarlos Javier SolorzaNo ratings yet
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumDocument6 pagesComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinNo ratings yet
- Hard Palate Dermis Fat Composite Graft For Reconstruction of Contracted Anophthalmic SocketDocument7 pagesHard Palate Dermis Fat Composite Graft For Reconstruction of Contracted Anophthalmic SocketSaraelsy MonterrosoNo ratings yet
- Gox 8 E2578Document12 pagesGox 8 E2578Ade Triansyah EmsilNo ratings yet
- Alogénico Vs AutoóogoDocument4 pagesAlogénico Vs AutoóogoMaximiliano Jara ContrerasNo ratings yet
- The Utility of Full-Thickness Skin Grafts (FTSGS) For Auricular ReconstructionDocument8 pagesThe Utility of Full-Thickness Skin Grafts (FTSGS) For Auricular ReconstructionAncaVerdesNo ratings yet
- Small Intestine Anastomosis by Full Thickness, Single Layer and Interrupted Suture Technique: Results of A Comparative StudyDocument4 pagesSmall Intestine Anastomosis by Full Thickness, Single Layer and Interrupted Suture Technique: Results of A Comparative StudyS3V4_9154No ratings yet
- Bone-Anchored Hearing Aid: A Comparison of Surgical TechniquesDocument7 pagesBone-Anchored Hearing Aid: A Comparison of Surgical TechniquesShanaz KanandaNo ratings yet
- JCM 11 03305Document8 pagesJCM 11 03305Vainatheya AnanthNo ratings yet
- Reupload Skin Graft ManagementDocument20 pagesReupload Skin Graft Managementhawaalia534100% (1)
- Comparison of Different Kinesio Taping Techniques Following Third Molar SurgeryDocument10 pagesComparison of Different Kinesio Taping Techniques Following Third Molar SurgerygreynerNo ratings yet
- Comparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumDocument6 pagesComparison of Hyperdry Amniotic Membrane Transplantation and Conjunctival Autografting For Primary PterygiumNazliah SyarbinNo ratings yet
- Types of Gingival GraftsDocument34 pagesTypes of Gingival GraftsAhmad KurukchiNo ratings yet
- Decision Algỏithm and Surgical Strategies For Managing Trachecutaneous FistulaDocument9 pagesDecision Algỏithm and Surgical Strategies For Managing Trachecutaneous Fistulahai1No ratings yet
- Resection of Localized Cheek Infantile HemangiomaDocument4 pagesResection of Localized Cheek Infantile HemangiomaindriNo ratings yet
- Ahonen-Siirtola2018 - Article - LaparoscopicVersusHybridApproa 1Document8 pagesAhonen-Siirtola2018 - Article - LaparoscopicVersusHybridApproa 1John NinNo ratings yet
- Skin GraftDocument7 pagesSkin GraftrchNo ratings yet
- Journal Homepage: - : IntroductionDocument22 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Clinical Evidence Series58Document28 pagesClinical Evidence Series58David DavidNo ratings yet
- Case Studies in Advanced Skin Cancer Management: An Osce Viva ResourceFrom EverandCase Studies in Advanced Skin Cancer Management: An Osce Viva ResourceNo ratings yet
- Clinical StudyDocument11 pagesClinical StudyandreeaNo ratings yet
- Archotol 1983 00800170041011Document3 pagesArchotol 1983 00800170041011abhishekjha0082No ratings yet
- Observation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsDocument10 pagesObservation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsAngelica SerbulNo ratings yet
- Suzuki K 2020. 3-6 MesesDocument11 pagesSuzuki K 2020. 3-6 MesesMARIA ANTONIETA RODRIGUEZ GALECIONo ratings yet
- Surgical Reconstruction in Scalp DefectsDocument4 pagesSurgical Reconstruction in Scalp Defectsmurdoko_boyNo ratings yet
- Cat Udn DDDocument12 pagesCat Udn DDThịnh LêNo ratings yet
- JURDING RCT PlastikDocument22 pagesJURDING RCT Plastikbrianto adhyNo ratings yet
- Modul Wound Bed Preparation DR Ardianto SucintaDocument37 pagesModul Wound Bed Preparation DR Ardianto SucintaArdianto SucintaNo ratings yet
- Invited Discussion On: Concentrated Growth Factors Extracted From Blood Plasma Used To Repair Nasal Septal Mucosal Defect After RhinoplastyDocument2 pagesInvited Discussion On: Concentrated Growth Factors Extracted From Blood Plasma Used To Repair Nasal Septal Mucosal Defect After RhinoplastyHiktor TomNo ratings yet
- TMP 8 B86Document5 pagesTMP 8 B86FrontiersNo ratings yet
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDocument11 pagesUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanNo ratings yet
- Classification and Pathophysiology of Skin GraftsDocument6 pagesClassification and Pathophysiology of Skin Graftsfaris nagibNo ratings yet
- Handout Advanced Course in Soft Tissue Surgery 2011Document64 pagesHandout Advanced Course in Soft Tissue Surgery 2011Mihaela AndreiNo ratings yet
- Full Thickness Skin Grafts in Periocular Reconstructions: Long-Term OutcomesDocument4 pagesFull Thickness Skin Grafts in Periocular Reconstructions: Long-Term OutcomesdrelvNo ratings yet
- Aesculap Ds Appendectomy ClipDocument12 pagesAesculap Ds Appendectomy ClipdoniNo ratings yet
- Qureshi 2019Document8 pagesQureshi 2019Jefferson RuizNo ratings yet
- Study On Surgical Management of Post Burn Hand Deformities: Abst TDocument5 pagesStudy On Surgical Management of Post Burn Hand Deformities: Abst TAmriansyah PranowoNo ratings yet
- Punzalan, Joshua Mitchell L. Case-Scenarios-NICUDocument2 pagesPunzalan, Joshua Mitchell L. Case-Scenarios-NICUJM PunzalanNo ratings yet
- Type 1 Diabetes MellitusDocument6 pagesType 1 Diabetes MellitusThina Cruz TorresNo ratings yet
- Tubercular Miasm: BY DR Krishnakumari 19HP05Document22 pagesTubercular Miasm: BY DR Krishnakumari 19HP05surabhiNo ratings yet
- Merin ClassificationDocument2 pagesMerin ClassificationPatphajong Limteerakul100% (11)
- LaQshya - Labour Room Quality Improvement Initiative GuidelineDocument60 pagesLaQshya - Labour Room Quality Improvement Initiative GuidelineKallol ChakrabortyNo ratings yet
- Søren Jepsen - Jack G. Caton - Jasim M. Albandar - Nabil F. BissadaDocument19 pagesSøren Jepsen - Jack G. Caton - Jasim M. Albandar - Nabil F. BissadaFelipeOyarceSalazarNo ratings yet
- Dialog InggrisDocument4 pagesDialog Inggrisبايو سيتياوانNo ratings yet
- Medicine: Sudden Seizure During Cesarean SectionDocument2 pagesMedicine: Sudden Seizure During Cesarean SectionDavid RefuncionNo ratings yet
- Louisa Oduro Animapauh CVDocument6 pagesLouisa Oduro Animapauh CVapi-426629371No ratings yet
- Introduction To Community Health and Environmental Sanitation PDFDocument44 pagesIntroduction To Community Health and Environmental Sanitation PDFKaty SanchezNo ratings yet
- Khawaja Ms Sialkot MbbsDocument5 pagesKhawaja Ms Sialkot MbbsRayan ArhamNo ratings yet
- LCD VLCDDocument18 pagesLCD VLCDRendy AndikaNo ratings yet
- Guidedboneregeneration Inalveolarbone Reconstruction: Istvan A. Urban,, Alberto MonjeDocument8 pagesGuidedboneregeneration Inalveolarbone Reconstruction: Istvan A. Urban,, Alberto MonjeVanessa Iñiguez ArmijosNo ratings yet
- VDRL Test and Its InterpretationDocument11 pagesVDRL Test and Its InterpretationSauZen SalaZarNo ratings yet
- Introduction To ParasitologyDocument3 pagesIntroduction To Parasitologydedi hartawanNo ratings yet
- Manila Tytana CollegesDocument1 pageManila Tytana CollegesSkyeNo ratings yet
- Titra SiDocument5 pagesTitra SiRizka Yuliasih KussantyNo ratings yet
- Prevalence of Birth Asphyxia and Associated Factors Among Neonates Delivered in Dilchora Referral Hospital in Dire Dawa Eastern Et 2090 7214 1000279 PDFDocument7 pagesPrevalence of Birth Asphyxia and Associated Factors Among Neonates Delivered in Dilchora Referral Hospital in Dire Dawa Eastern Et 2090 7214 1000279 PDFrikarikaNo ratings yet
- WHAT IS YOUR SEXUAL SELF? It Is A Part of Yourself Where You Learn Understand About SexualDocument14 pagesWHAT IS YOUR SEXUAL SELF? It Is A Part of Yourself Where You Learn Understand About SexualcyNo ratings yet
- The Drug Development Process Step 3 - Clinical ResearchDocument5 pagesThe Drug Development Process Step 3 - Clinical ResearchDavid ThaiNo ratings yet
- Victims of Sexual Offences: Medicolegal Examinations in Emergency SettingsDocument4 pagesVictims of Sexual Offences: Medicolegal Examinations in Emergency SettingsVidini Kusuma AjiNo ratings yet
- Dra. Michel Fernanda Girón Luna Cirujano DentistaDocument2 pagesDra. Michel Fernanda Girón Luna Cirujano DentistaMichelle GirónNo ratings yet
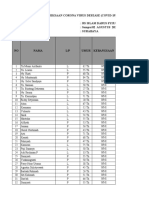
- Laporan Pasien Covid19 Ranap Dan Rajal RSI Darus Syifa SbyDocument61 pagesLaporan Pasien Covid19 Ranap Dan Rajal RSI Darus Syifa SbyNur HasanahNo ratings yet
- Heart Attack (Myocardial Infarction) - Symptoms and Causes - PatientDocument8 pagesHeart Attack (Myocardial Infarction) - Symptoms and Causes - Patientaasuman123No ratings yet
- ADMINDocument3 pagesADMINpia espanilloNo ratings yet
- TCM Case Work-Up: /conversion/tmp/activity - Task - Scratch/574230788Document12 pagesTCM Case Work-Up: /conversion/tmp/activity - Task - Scratch/574230788Hui YingNo ratings yet
- Development of The Infant and Young ChildDocument406 pagesDevelopment of The Infant and Young Childdarkorx100% (1)
- Intrapartum Fetal MonitoringDocument9 pagesIntrapartum Fetal MonitoringYwagar YwagarNo ratings yet
- Hospital & Non-Institutional DeliveriesDocument7 pagesHospital & Non-Institutional DeliveriesFritz MirandaNo ratings yet
- Pfizer Vaccine Near Romford Uk - Google SearchDocument1 pagePfizer Vaccine Near Romford Uk - Google SearchVISHAL BANSALNo ratings yet