Professional Documents
Culture Documents
Diagnosis and Management of Acute Encephalitis: A Practical Approach
Diagnosis and Management of Acute Encephalitis: A Practical Approach
Uploaded by
Daanni SolisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnosis and Management of Acute Encephalitis: A Practical Approach
Diagnosis and Management of Acute Encephalitis: A Practical Approach
Uploaded by
Daanni SolisCopyright:
Available Formats
Neurology® Clinical Practice
Diagnosis and
management of acute
encephalitis
A practical approach
Arun Venkatesan, MD, PhD
Romergryko G. Geocadin, MD
Summary
Encephalitis results in considerable morbidity and mor-
tality in the United States and worldwide. Neurologists
are often consulted or directly care for patients with en-
cephalitis admitted to the hospital and must be able to
discriminate between encephalitis and the many condi-
tions that mimic it. Moreover, neurologists must be
familiar with the myriad causes of encephalitis in order
to develop a practical approach to diagnostic testing
and treatment. An understanding of recent advances
in management, particularly with respect to autoim-
mune etiologies and critical care approaches, is equally
important. Here, we summarize a general approach to
the care of adult patients with encephalitis.
E
ncephalitis results from inflammation of the brain parenchyma, and may be caused
by infections or autoimmune conditions. Diagnosis is typically made by a combina-
tion of clinical, laboratory, neuroimaging, and electrophysiologic findings. A num-
ber of case definitions have been developed,1–7 which generally require
encephalopathy, as characterized by alteration in consciousness or personality change lasting
for a sustained period of time (typically greater than 24 hours). To distinguish encephalitis
from other causes of encephalopathy, key features include presence of fever, CSF pleocytosis,
or MRI or EEG changes compatible with encephalitis (table 1). Although such definitions
likely capture most patients with clinically significant encephalitis, some will be missed. For
example, localized forms of brain inflammation (i.e., a unilateral brainstem process) may
cause focal neurologic deficits without affecting consciousness or behavior.8
Neurologists must be aware of the numerous conditions that may mimic encephalitis.
Some examples include vascular disease, systemic infection (with no direct CNS infection)
Johns Hopkins Encephalitis Center, Department of Neurology (AV, RG), and the Departments of Anaesthesiology–
Critical Care Medicine, Neurosurgery, and Medicine (RG), Johns Hopkins University School of Medicine,
Baltimore, MD.
Funding information and disclosures are provided at the end of the article. Full disclosure form information
provided by the authors is available with the full text of this article at Neurology.org/cp.
Correspondence to: avenkat2@jhmi.edu
206 © 2014 American Academy of Neurology
Diagnosis and management of acute encephalitis
Table 1 Diagnostic criteria for encephalitisa
Major criterion (required)
Patients presenting to medical attention with altered mental status (defined as decreased or
altered level of consciousness, lethargy, or personality change) lasting $24 hours with no
alternative cause identified
Minor criteria (2 required for possible encephalitis; $3 required for probable or confirmed
encephalitis)
Documented fever $38°C (100.4°F) within the 72 hours before or after presentation
Generalized or partial seizures not fully attributable to a preexisting seizure disorder
New onset of focal neurologic findings
CSF leukocyte count $5/mm3
Abnormality of brain parenchyma on neuroimaging suggestive of encephalitis that is either new
from prior studies or appears acute in onset
Abnormality on EEG that is consistent with encephalitis and not attributable to another cause.
a
Adapted from reference 7 (Venkatesan et al. Clinical Infectious Diseases 2013;57:1114–1128)
by permission of Oxford University Press on behalf of the Infectious Diseases Society of America.
or inflammation, toxic exposures, or metabolic derangements (table e-1 at Neurology.org/cp).
Such conditions need to be aggressively investigated in all patients with suspected encepha-
litis. Given the range of conditions that cause and mimic encephalitis, obtaining a thorough
history is crucial. Important historical points include the presence of recent illness, ill con-
tacts, unusual exposures (including occupational, vector, and animal), outdoor activities, and
ingestions. It is critical to elicit travel history, both recent and remote, since agents such as
rabies or malaria can become symptomatic long after initial exposure.
A practical approach to diagnosis in adults is presented in table 2. In addition to routine studies
to investigate for causes of encephalopathy, all patients with suspected encephalitis should undergo
blood cultures and HIV testing. Extra serum should be drawn during the acute phase of illness and
held for later serologic studies, and if the diagnosis is still uncertain, a convalescent serum should be
collected 10–21 days later. Lumbar puncture (LP) is recommended in all individuals unless
contraindicated (i.e., significant mass effect/edema or effacement of basal cisterns on neuroimaging,
or suspected skin or soft tissue abscess in the path of the puncture needle).9
Since herpes simplex virus (HSV), varicella-zoster virus (VZV), and enterovirus are 3 of the
most commonly identified etiologic agents in acute encephalitis,1,4,6 these should be routinely
screened for in the CSF. With respect to neuroimaging, MRI is preferred to CT given the
increased sensitivity and specificity for evaluation of encephalitis.10–12 Chest imaging should
also be performed as focal infiltrates may be suggestive of certain pathogens (e.g., fungal or
mycobacterial infections).
In addition to travel, exposure, and medical history, specific signs and symptoms as well as
laboratory and neuroimaging features can help to guide further testing (table 2). For example,
prominent psychosis or movement disorders should prompt testing for anti-NMDA receptor
(NMDAR) encephalitis, those with limbic symptoms should undergo testing for anti–voltage-gated
potassium channel [VGKC] and other paraneoplastic encephalitides, and brainstem lesions should
prompt further testing for a range of additional pathogens. Notably, the field of autoimmune
encephalitis is rapidly advancing, and testing algorithms are likely to continue to evolve.
Diagnostic testing: practical considerations and caveats
During LP, CSF opening pressure should be obtained in all individuals, since abnormalities in
intracranial pressure (ICP) may contribute to the neurologic dysfunction in encephalitis or, al-
ternatively, suggest a different diagnosis. Although the typical CSF profile of viral encephalitis
demonstrates a mononuclear pleocytosis with cell counts up to 200 cells/mm3, with more
Neurology: Clinical Practice ||| June 2014 Neurology.org/cp 207
Arun Venkatesan and Romergryko G. Geocadin
Table 2 Initial evaluation of encephalitis in adultsa
Routine studies
CSF (unless contraindicatedb)
Opening pressure, leukocyte count with differential, erythrocyte count, protein, glucose
Gram stain and bacterial culture
HSV-1/2 PCR (if test available, consider HSV CSF IgG and IgM in addition)
VZV PCR (sensitivity may be low; if test available, consider VZV CSF IgG and IgM in addition)
Enterovirus PCR
Cryptococcal antigen or India ink staining
Oligoclonal bands and IgG index
Venereal Disease Research Laboratory
Serum
Routine blood cultures
HIV serology (consider RNA)
Treponemal testing (rapid plasma reagin, specific treponemal test)
Imaging
Neuroimaging (MRI preferred to CT, if available)
Chest imaging (chest x-ray or CT)
Neurophysiology
EEG
Other tissues/fluids
When clinical features of extra-CNS involvement are present, we recommend additional
testing (e.g., biopsy of skin lesions; bronchoalveolar lavage or endobronchial biopsy in those
with pneumonia/pulmonary lesions; throat swab PCR/culture in those with upper respiratory
illness; stool culture in those with diarrhea); also see below
Conditional studies
Host factors
Immunocompromised—CMV PCR, HHV6/7 PCR, Toxoplasma gondii; MTB, fungal infections,
WNV
Geographic factors
Africa—malaria, trypanosomiasias, dengue
Asia—Japanese encephalitis virus, dengue, malaria, Nipah virus
Australia—Murray Valley encephalitis, Kunjin virus, Australian bat lyssavirus
Europe—tick-borne encephalitis virus; if Southern Europe, consider WNV testing, Toscana
virus testing
Central and South America—dengue, malaria, WNV, Venezuelan equine encephalitis
North America—geographically appropriate arboviruses (e.g., WNV, Powassan, LaCrosse,
Eastern equine encephalitis virus, St. Louis encephalitis, dengue, Lyme)
Season and exposure
Summer/fall: WNV and other arboviruses, tick-borne disease
Cat (particularly if with seizures, paucicellular CSF)—Bartonella
Tick exposure—tick-borne disease
Animal bite/bat exposure—rabies
Swimming or diving in warm freshwater or nasal/sinus irrigation—Naegleria fowleri
Continued
208 © 2014 American Academy of Neurology
Diagnosis and management of acute encephalitis
Table 2 Continued
Specific signs and symptoms
Psychotic features or movement disorder—anti-NMDAR encephalitis, rabies, Creutzfeldt-
Jakob disease
Prominent limbic symptoms—autoimmune limbic encephalitis, HHV6/7
Rapid decompensation (particularly with animal bite history or prior travel to rabies-endemic
areas)—rabies
Respiratory symptoms—Mycoplasma pneumoniae, respiratory viruses
Acute flaccid paralysis—WNV and other arboviruses, rabies
Parkinsonism—Arbovirus, Toxoplasma
Nonhealing skin lesions—Balamuthia mandrillaris, Acanthamoeba
Laboratory features
Elevated transaminases—rickettsia, tick-borne diseases
CSF protein .100 mg/dL, or CSF glucose ,2/3 peripheral glucose, or lymphocytic
pleocytosis with subacute symptom onset—MTB and fungal testing
CSF protein .100 mg/dL or CSF glucose ,2/3 peripheral glucose and neutrophilic
predominance with acute symptom onset and recent antibiotic use—S pneumoniae and
Neisseria meningiditis
CSF eosinophilia—MTB and fungal testing, Baylisascaris procyonis, Angiostrongylus
cantonensis, Gnathostoma sp.
Erythrocytes in CSF—N fowleri
Hyponatremia—anti-VGKC; MTB
Neuroimaging features
Frontal lobe—N fowleri
Temporal lobe—anti-VGKC basal ganglia or thalamus, Arbovirus, MTB
Brainstem—Arbovirus, listeria, Brucella, MTB
Cerebellum—Epstein-Barr virus
Diffuse cerebral edema—respiratory virus testing
Space-occupying or ring-enhancing lesions—MTB and fungal infections, B mandrillaris and
Acanthamoeba, toxoplasma serology
Hydrocephalus or basilar meningeal enhancement—MTB and fungal infections
Infarction or hemorrhage—MTB and fungal infections; respiratory virus testing
Incomplete ring-enhancing lesions—ADEM
Abbreviations: ADEM 5 acute disseminated encephalomyelitis; CMV 5 cytomegalovirus; HHV 5
human herpesvirus; HSV 5 herpes simplex virus; IgG 5 immunoglobulin G; IgM 5 immunoglobulin
M; NMDAR 5 NMDA receptor; VZV 5 varicella-zoster virus; WNV 5 West Nile virus.
a
Adapted from reference 7 (Venkatesan et al. Clinical Infectious Diseases 2013;57:1114–1128)
by permission of Oxford University Press on behalf of the Infectious Diseases Society of America.
This table is not intended to encompass all causes of encephalitis, nor all epidemiologic or labo-
ratory-based risk factors. We recommend utilizing this table as a guideline for initial management
of acute encephalitis in adults.
b
Lumbar puncture is recommended in all individuals with suspected encephalitis unless contra-
indicated (i.e., significant mass effect/edema, effacement of basal cisterns on imaging; skin or soft
tissue infection in needle path; see reference 9).
substantial pleocytosis typically suggesting a bacterial infection, some viruses can be associated
with CSF leukocyte counts greater than 1,000 cells/mm3 (i.e., mumps, lymphocytic chori-
omeningitis virus). Moreover, neutrophils, which are generally accepted to be present in the
first 24 hours after viral infection, may persist beyond 24 hours.13
Neurology: Clinical Practice ||| June 2014 Neurology.org/cp 209
Arun Venkatesan and Romergryko G. Geocadin
It is critical to elicit travel history, both recent
and remote, since agents such as rabies or
malaria can become symptomatic long after
initial exposure.
Selected viral etiologies The 2 most common human herpesviruses identified in the setting
of encephalitis are HSV-1 and VZV. The HSV PCR test can result in false-negatives, partic-
ularly among children and early in the course of disease.14–16 If herpes simplex encephalitis is
still suspected despite negative testing from the first LP, a second CSF examination should be
repeated within 3 to 7 days.17 Since VZV reactivation may occur without demonstrable skin
lesions (zoster sine herpete), testing for VZV in all individuals with suspected encephalitis is
recommended regardless of whether vesicular lesions are present.18 Notably, testing of the
CSF for VZV PCR, though recommended, appears to have suboptimal sensitivity. Indeed,
detection of CSF antibodies to VZV may be a more sensitive approach to diagnosing VZV
encephalitis.19
Diagnosis of arboviral encephalitis presents a unique set of challenges. In general, serologic test-
ing of serum and CSF is preferable to PCR, since the peak viral load typically occurs before the
onset of symptoms. This has been well described in West Nile virus (WNV) neuroinvasive dis-
ease, for example, where the sensitivity of CSF PCR is low compared with CSF WNV immu-
noglobulin M (IgM).20 Since the percentage of seropositive patients increases over the first
week of illness, repeat testing can be useful if the suspicion for disease is high despite initial
negative results.21,22 Following acute infection, IgM antibodies may persist for months, and
thus their presence does not necessarily indicate current or active infection.23,24 Seroconver-
sion of the IgM antibody or a 4-fold or greater rise in titer, or both, can substantiate the
diagnosis.
Selected autoimmune etiologies Cardinal clinical features of anti-NMDAR encephalitis in-
clude changes in behavior or cognition, seizures, orofacial dyskinesias, and autonomic instabil-
ity.25,e1 In a large series of patients in whom both CSF and serum were tested for NMDAR
antibodies, approximately 15% of individuals had positive CSF antibodies in the absence of
serum antibodies.e2 Thus, CSF testing is recommended in those with a compatible clinical
Neurology.org/cp picture and negative serum antibodies. Recent evidence has linked the development of anti-
bodies to NMDAR to preceding or concurrent herpes simplex encephalitis. In a study of
patients with PCR-proven herpes simplex encephalitis (HSE), NMDAR antibodies were
detected in one-third of patients (13 of 44),e3 while more recently, some pediatric cases with
neurologic relapse (movement disorders or new cognitive dysfunction, or both) following
herpes encephalitis have been found to have NMDAR antibodies and responded to immu-
notherapy.e4,e5 These reports suggest that patients who experience a neurologic decline fol-
lowing treatment for HSE should be tested for NMDAR antibodies.
Autoimmune limbic encephalitis results in a combination of acute or subacute onset of
short-term memory deficits, behavioral changes, and seizures. It occurs in association with sev-
eral types of antibodies, including those associated with cancer (onconeuronal antibodies to
antigens such as Hu, CV2, and Ma2) and those directed against synaptic or neuronal cell sur-
face antigens (i.e., VGKC, glutamic acid decarboxylase, and AMPA receptor, among others). In
general, serum testing may be sufficient.e6
Management
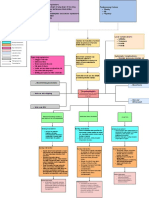
The management of acute encephalitis can be guided by a practical approach involving 3 “Es”:
emergent issues, epilepsy, and etiology. An overview of acute management of patients is
provided in the figure, and typical doses of therapeutic agents are listed in table 3.
210 © 2014 American Academy of Neurology
Diagnosis and management of acute encephalitis
Figure Approach to management of patients with suspected encephalitis
HSV 5 herpes simplex virus; ICU 5 intensive care unit; VZV 5 varicella-zoster virus.
Emergent issues
Upon presentation, a careful evaluation is important to quickly identify and address all evolving
and impending emergent neurologic and systemic issues. The immediate goal is to ensure pa-
tient safety while efficient and effective diagnosis and management are undertaken. Assessing
the ABCs is an essential first step. Is the patient’s airway protected? Reduced level of con-
sciousness, which can result from metabolic encephalopathy, seizures, or cerebral edema, can
lead to impaired airway reflexes that may necessitate endotracheal intubation. Is breathing
adequate? Similar neurologic conditions that impair airway reflexes can also impair respiratory
drive, while systemic conditions such as pneumonia may impair oxygenation. Hypoxemia or
hypercarbia may necessitate mechanical ventilatory support after endotracheal intubation.
Is circulation sufficient? A number of etiologies of encephalitis, including anti-NMDAR
encephalitis and HSE, have been associated with autonomic dysfunction, and hemodynamic
stability must be ensured.
Where should the patient be admitted? In one series of patients with encephalitis, approx-
imately 25% of cases were admitted to the intensive care unit (ICU).e7 Factors involved in
making the decision to admit to the ICU include level of consciousness, impairment in the
ABCs, comorbid conditions, and specific etiologic concerns. The clinical needs of patients
with encephalitis in the ICU are complex and a multidisciplinary team is essential. While no
dedicated data exist, the complexities of the neurologic issues, along with critical care con-
cerns, are reasons to favor admission in a dedicated neurologic critical care unit. In the
absence of one, it is key that neurologic consultants work closely and in real time with the
ICU team to ensure the best outcome of patients.
Acute reduction or alteration of consciousness The acute reduction or alteration of con-
sciousness is an emergent neurologic issue. In the setting of encephalitis, the top concerns in-
clude ICP and mass effect, direct and global effect of inflammation or infection to the brain,
and systemic issues that affect brain function (i.e., hypoglycemia, fever, electrolyte abnormality,
O2 and CO2, and systemic infections). Here, we focus on management of increased ICP and
mass effect. Seizures will be addressed separately.
Concerns for ICP abnormalities and mass effect should prompt rapid bedside assessment
and immediate neurologic imaging (a head CT typically suffices). A reduction in level of
Neurology: Clinical Practice ||| June 2014 Neurology.org/cp 211
Arun Venkatesan and Romergryko G. Geocadin
Table 3 Therapeutics agents commonly used in encephalitis
Indication Typical dosing/administrationa
Cerebral edemae8 Mannitol 0.25 to 1 g/kg bolus every 4–6 hours
Hypertonic saline
Active brain herniation, 23% saline (30 mL bolus via central venous access)
Maintenance, 2%–3% saline (250–500 mL boluses or continuous venous infusion; 3% saline via
central venous access)
Seizures and status
epilepticuse12
First line, initial dosing Lorazepam 0.1 mg/kg IV up to 4 mg per dose
Midazolam 0.25 mg/kg IM up to 10 mg maximum
Diazepam 0.15 mg/kg IV up to 10 mg per dose
Second line, initial dosing Fosphenytoin 20 mg PE/kg IV
Levetiracetam 1,000–3,000 mg IV
Valproate sodium, 20–40 mg/kg IV
Third line, loading dose Propofol 1–2 mg/kg
Phenobarbital 20 mg/kg IV
Pentobarbital 5–15 mg/kg IV
Herpes simplex Acyclovir, 10 mg/kg IV q 8 hrs 3 14–21 days
encephalitis17
Autoimmune encephalitis,
acutee16,e17
First line Methylprednisolone 1,000 mg IV q day 3 5 days
IV immunoglobulin, 0.4 g/kg IV q day 3 5 days
Plasma exchange, 5–7 exchanges administered every other day
Second line Cyclophosphamide, body surface area 3 800 mg IV
Rituximab, 1,000 mg IV 3 1, followed by second dose in 2 weeks
a
Drugs and dosing recommendations are provided only as guide; clinical conditions and drug effects must be carefully considered
prior to drug administration.
consciousness (LOC) associated with unilateral or bilateral pupillary dilation and nonreactivity
to light may indicate transtentorial brain herniation. A recent review addressed the reversal of
brain herniation.e8 Normal oxygenation (O2 sats .90%) and hyperventilation to pCO2 30 6
2 mm Hg and mean arterial pressure to at least 60 mm Hg are reasonable initial targets. If
mass effect from significant cerebral edema is noted, hyperosmolar therapy with the use of
mannitol or hypertonic saline may be necessary. IV mannitol at 0.25 to 1 g/kg bolus every 4–
6 hours can be given via a peripheral line, though it is important to correct the diuresis
associated with mannitol with normal saline solution in order to avoid dehydration. Our
preference has been the use of hypertonic saline rather than mannitol; we typically use
concentrations of 2% Na via a peripheral line, and 3% or 23.4% Na via a central line.
We administer 2% or 3% Na as boluses of 250–500 cc to attain a serum Na of 150–155;
maintenance infusion may be necessary over several days. The administration of a 30-cc bolus
of 23.4% Na is reserved for active brain herniation. One important caveat in the use of saline
solutions is in the setting of hyponatremia, as can occur in CNS infection. Long-term hy-
ponatremia needs to be corrected slowly over several days to avoid myelin injury, and there-
fore mannitol may be preferred in such settings. However, for those with normal Na,
hypertonic saline is typically safe and may be used aggressively as needed. Mass effect
212 © 2014 American Academy of Neurology
Diagnosis and management of acute encephalitis
The clinical needs of patients with encephalitis in
the ICU are complex and a multidisciplinary team
is essential.
associated with vasogenic edema may benefit from high doses of corticosteroids, the use of
which is described later (Etiology). Fevers may increase ICP and worsen neurologic injury,
and should be treated.e9 Rapidly evolving hydrocephalus typically requires placement of a
ventriculostomy for CSF drainage and ICP monitoring. In some case, cerebral edema and
ICP elevation may progress despite the above interventions, and initiation of barbiturate
coma or hemicraniectomy to relieve global pressure may be necessary.
While issues of increased ICP are being addressed, other factors that may contribute to en-
cephalopathy need to be continually evaluated. The list can be exhaustive but some entities to
consider include septic encephalopathy due to an extraneural infection; endocrine pathology
(i.e., thyroid, adrenals); metabolic issues (i.e., hyperammonemia, electrolyte disorder, syn-
drome of inappropriate antidiuretic hormone secretion); and cerebral hypoperfusion states.
Seizures and status epilepticus
The occurrence of seizures is common and status epilepticus in critically ill patients with enceph-
alitis is noted in 15%.e7 In encephalitic patients with reduced or altered LOC, seizures represent
a potentially treatable entity and should be treated immediately if diagnosed. Emergent EEG is
crucial and prolonged continuous EEG is recommended to improve diagnostic ability and to
monitor treatment effects of antiepileptic agents in real time. The clinical approach to seizures
and status epilepticus highlights the need for close collaboration between the neurologist and
the intensivist. The goal of treatment is to control epileptic activity, but in many cases it is
necessary to induce a burst-suppression pattern on EEG.
In patients suspected or diagnosed with seizures, concurrent with the ABCs is the need to ad-
minister first-line agents such as lorazepam IVe10 or midazolam IM.e11 For definite or continued
seizure activity, choices for second-line antiepileptic drugs (AEDs) can be tailored to the clinical
situation with IV agents such as fosphenytoin, levetiracetam, and valproic acid. It is not uncom-
mon for encephalitic patients to progress to more refractory epileptic states that typically require a
third-line AED with anesthetic properties, such as barbiturates (i.e., pentobarbital or high-dose
phenobarbital), propofol, and ketamine. As the aggressiveness of epilepsy treatment increases, so
does the need for increasing ICU support due to potential adverse effects such as hypotension,
loss of protective airway reflex, and respiratory drive. Other potential systemic complications
include pneumonia and sepsis. Continuous monitoring for seizures and their resolution is im-
portant to optimize AED therapy while minimizing duration of drug exposure and attendant
complications. A guideline to the management of status epilepticus has recently been published.e12
Etiology
The diagnostic approach provided above may require days to weeks to ascertain a specific eti-
ologic basis for treatment. At the time of presentation, it is important to consider empiric man-
agement for common etiologies of encephalitis. Foremost is HSV and the need to start IV
acyclovir as early as possible. Delay in acyclovir treatment in those suspected with HSV infec-
tion resulted in increased risk of death and severe disability.e13 Depending on the CSF profile,
any suspicion of bacterial infection may necessitate broader coverage with appropriate anti-
biotics and corticosteroids as necessary.e14 In addition, results of the diagnostic evaluation may
prompt administration of other appropriate antiviral, antibacterial, or antifungal agents.
In patients with autoimmune etiology, appropriate strategies for immune modulation must be
initiated. First-line immunotherapies for acute immune-mediated encephalitis generally include
corticosteroids (i.e., IV methylprednisolone, 1,000 mg daily for 5 days), IV immunoglobulin
Neurology: Clinical Practice ||| June 2014 Neurology.org/cp 213
Arun Venkatesan and Romergryko G. Geocadin
(typically 2 g/kg body weight given over 5 days), and plasmapheresis (typically 5 exchanges,
administered every other day), either alone or in combination. Response to these agents is typically
monitored over several weeks and, if suboptimal, then second-line treatments, including cyclo-
phosphamide (i.e., 1,000 mg/kg body weight, given once) or rituximab (i.e., 1,000 mg IV given
once, then repeated in 2 weeks), are recommended.e2 In the case of paraneoplastic syndromes, the
resection of the offending tumor (i.e., oophorectomy in NMDAR encephalitis) is often critical
for achieving control of neuroinflammation.e15 Notably, empiric immunosuppressive therapy
may be considered in those with encephalitis of unknown etiology, although clinical or radio-
logic deterioration in such patients should prompt a brain biopsy.8
REFERENCES
1. Granerod J, Ambrose HE, Davies NW, et al. Causes of encephalitis and differences in their clinical
presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 2010;
10:835–844.
2. Kolski H, Ford-Jones EL, Richardson S, et al. Etiology of acute childhood encephalitis at The Hos-
pital for Sick Children, Toronto, 1994–1995. Clin Infect Dis 1998;26:398–409.
3. Ball R, Halsey N, Braun MM, et al. Development of case definitions for acute encephalopathy,
encephalitis, and multiple sclerosis reports to the vaccine: adverse event reporting system. J Clin
Epidemiol 2002;55:819–824.
4. Glaser CA, Honarmand S, Anderson LJ, et al. Beyond viruses: clinical profiles and etiologies associ-
ated with encephalitis. Clin Infect Dis 2006;43:1565–1577.
5. Sejvar JJ, Kohl KS, Bilynsky R, et al. Encephalitis, myelitis, and acute disseminated encephalomyelitis
(ADEM): case definitions and guidelines for collection, analysis, and presentation of immunization
safety data. Vaccine 2007;25:5771–5792.
6. Mailles A, Stahl JP. Infectious encephalitis in France in 2007: a national prospective study. Clin Infect
Dis 2009;49:1838–1847.
7. Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions, diagnostic algorithms, and priorities in
encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis 2013;
57:1114–1128.
8. Tan IL, Mowry EM, Steele SU, et al. Brainstem encephalitis: etiologies, treatment, and predictors of
outcome. J Neurol 2013;260:2312–2319.
9. Roos KL. Lumbar puncture. Semin Neurol 2003;23:105–114.
10. Steiner I, Budka H, Chaudhuri A, et al. Viral encephalitis: a review of diagnostic methods and
guidelines for management. Eur J Neurol 2005;12:331–343.
11. Schroth G, Kretzschmar K, Gawehn J, Voigt K. Advantage of magnetic resonance imaging in the
diagnosis of cerebral infections. Neuroradiology 1987;29:120–126.
12. Marchbank ND, Howlett DC, Sallomi DF, Hughes DV. Magnetic resonance imaging is preferred in
diagnosing suspected cerebral infections. BMJ 2000;320:187–188.
13. Negrini B, Kelleher KJ, Wald ER. Cerebrospinal fluid findings in aseptic versus bacterial meningitis.
Pediatrics 2000;105:316–319.
14. De Tiège X, Héron B, Lebon P, Ponsot G, Rozenberg F. Limits of early diagnosis of herpes simplex
encephalitis in children: a retrospective study of 38 cases. Clin Infect Dis 2003;36:1335–1339.
15. Weil AA, Glaser CA, Amad Z, Forghani B. Patients with suspected herpes simplex encephalitis:
rethinking an initial negative polymerase chain reaction result. Clin Infect Dis 2002;34:1154–1157.
16. Elbers JM, Bitnun A, Richardson SE, et al. A 12-year prospective study of childhood herpes simplex
encephalitis: is there a broader spectrum of disease? Pediatrics 2007;119:e399–e407.
17. Tunkel AR, Glaser CA, Bloch KC, et al. The management of encephalitis: clinical practice guidelines
by the Infectious Diseases Society of America. Clin Infect Dis 2008;47:303–327.
18. Gregoire SM, van Pesch V, Goffette S, Peeters A, Sindic CJ. Polymerase chain reaction analysis and
oligoclonal antibody in the cerebrospinal fluid from 34 patients with varicella-zoster virus infection of
the nervous system. J Neurol Neurosurg Psychiatry 2006;77:938–942.
19. Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Varicella zoster virus vasculopathies: diverse clinical
manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol 2009;8:731–740.
20. Lanciotti RS, Kerst AJ, Nasci RS, et al. Rapid detection of West Nile virus from human clinical
specimens, field-collected mosquitoes, and avian samples by a TaqMan reverse transcriptase-PCR
assay. J Clin Microbiol 2000;38:4066–4071.
21. Tardei G, Ruta S, Chitu V, Rossi C, Tsai TF, Cernescu C. Evaluation of immunoglobulin M (IgM)
and IgG enzyme immunoassays in serologic diagnosis of West Nile Virus infection. J Clin Microbiol
2000;38:2232–2239.
214 © 2014 American Academy of Neurology
Diagnosis and management of acute encephalitis
22. Davis LE, DeBiasi R, Goade DE, et al. West Nile virus neuroinvasive disease. Ann Neurol 2006;60:
286–300.
23. Kapoor H, Signs K, Somsel P, Downes FP, Clark PA, Massey JP. Persistence of West Nile virus (WNV)
IgM antibodies in cerebrospinal fluid from patients with CNS disease. J Clin Virol 2004;31:289–291.
24. Prince HE, Tobler LH, Lapé-Nixon M, Foster GA, Stramer SL, Busch MP. Development and
persistence of West Nile virus-specific immunoglobulin M (IgM), IgA, and IgG in viremic blood
donors. J Clin Microbiol 2005;43:4316–4320.
25. Irani SR, Bera K, Waters P, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression
of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes.
Brain 2010;133:1655–1667.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
A. Venkatesan serves a Medical Expert for the US Government Vaccine Injury Compensation Program and
has received/receives research support from the NIH, Maryland Stem Cell Research Foundation, Howard
Hughes Medical Institute, and the National MS Society. R. Geocadin has received funding for travel from
the American Heart Association and the Neurocritical Care Society; receives research support from the
NIH; and has served as a medico-legal consultant. Full disclosure form information provided by the authors
is available with the full text of this article at Neurology.org/cp.
Related articles from other AAN physician and patient resources
Neurologyw C Neurology.org
Burden of encephalitis-associated hospitalizations in the United States, 1998–2010
February 4, 2014;82:443–451.
Predictors of outcome in acute encephalitis
August 27, 2013;81:793–800.
Continuumw C ContinuumJournal.com
Encephalitis and postinfectious encephalitis
December 2012;1271–1289.
Meningitis and encephalitis
October 2011;1010–1023.
Neurology Noww C Neurologynow.com
Ask the Experts: Flu and neurologic disease
November/December 2010;6:33.
Neurology Todayw C Neurotodayonline.com
BOOKSHELF: Through the Lens of a Journalist—A Personal Journey with Acute
Autoimmune Encephalitis
March 7, 2013;13:22.
West Nile Virus Spreads Rapidly Across the Nation—What Have Neurologists Learned?
October 4, 2012;12:1,11–16.
Children with the H1N1 Influenza Reportedly Suffered Serious Neurological Complications—
Renewing Call for Routine Influenza Vaccines
October 4, 2012;12:18–19.
Neurology: Clinical Practice ||| June 2014 Neurology.org/cp 215
You might also like
- NURS - FPX 5005 - Brendan Madden - Assessment - 2-1Document9 pagesNURS - FPX 5005 - Brendan Madden - Assessment - 2-1SohaibNo ratings yet
- CH 5Document153 pagesCH 5sojithesouljaNo ratings yet
- Adina Radulescu - ENGLISH IN KINETOTHERAPYDocument5 pagesAdina Radulescu - ENGLISH IN KINETOTHERAPYCosmina CorbeanuNo ratings yet
- Acquired NeuropathiesDocument106 pagesAcquired NeuropathiesDanny J. BrouillardNo ratings yet
- A Short History of Transfusion MedicineDocument14 pagesA Short History of Transfusion MedicinePatriciaNo ratings yet
- Manual Training Program Wvmc-Im Revised June 2018Document61 pagesManual Training Program Wvmc-Im Revised June 2018CARES Martin Federic Palco100% (1)
- A Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsDocument9 pagesA Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsarmankoassracunNo ratings yet
- Peripheral Neuropathy Diff Diagnosis and Management AafpDocument6 pagesPeripheral Neuropathy Diff Diagnosis and Management Aafpgus_lions100% (1)
- Seizure in SLE PatientDocument7 pagesSeizure in SLE PatientdivisiimunNo ratings yet
- Autoimmune EncephalitisDocument10 pagesAutoimmune EncephalitisMagda CabralesNo ratings yet
- Encephalitis: - Gunaseelan KumarDocument30 pagesEncephalitis: - Gunaseelan KumarGunaseelan Kumar100% (1)
- Britton Et Al-2015-Internal Medicine JournalDocument14 pagesBritton Et Al-2015-Internal Medicine JournalfrizkapfNo ratings yet
- Infectious Dan Autoantibody Associated EncephalitisDocument13 pagesInfectious Dan Autoantibody Associated EncephalitisAyudiah ParamitaNo ratings yet
- Pid 1 86Document9 pagesPid 1 86SandraNo ratings yet
- ENCEPHALITISDocument104 pagesENCEPHALITISAsogaa MeteranNo ratings yet
- Encefalitis Aguda en InmunocompetentesDocument15 pagesEncefalitis Aguda en InmunocompetentesNicolas de la cruz floresNo ratings yet
- Dengue Meningoencephalitis: Case ReportDocument3 pagesDengue Meningoencephalitis: Case ReportOleOhhNo ratings yet
- 72 - Progressive Multifocal Leukoencephalopathy in An Immunocompetent PatientDocument7 pages72 - Progressive Multifocal Leukoencephalopathy in An Immunocompetent PatientFaras ArinalNo ratings yet
- Management of EncephalitisDocument25 pagesManagement of EncephalitisOWintero OWarmoNo ratings yet
- Acute Viral Encephalitis - NEJMDocument17 pagesAcute Viral Encephalitis - NEJMFredghcNo ratings yet
- The NORSE (New-Onset Refractory Status Epileptic Us) SyndromeDocument4 pagesThe NORSE (New-Onset Refractory Status Epileptic Us) Syndromebenghooi75No ratings yet
- Discoveries 08 110Document19 pagesDiscoveries 08 110Riki AntoNo ratings yet
- Initial Evaluation VertigoDocument8 pagesInitial Evaluation VertigoTanri Hadinata WiranegaraNo ratings yet
- Holanda Et Al - J Neurovirol 2022Document4 pagesHolanda Et Al - J Neurovirol 2022jtd9h2xp5hNo ratings yet
- Translate Fira IngDocument6 pagesTranslate Fira IngRio Taruna JatiNo ratings yet
- Autoimmune Causes of Encephalitis Syndrome in Thailand: Prospective Study of 103 PatientsDocument9 pagesAutoimmune Causes of Encephalitis Syndrome in Thailand: Prospective Study of 103 PatientsLily Dian AgungNo ratings yet
- SNM America PsikiatriDocument7 pagesSNM America PsikiatriMuhammad Abdul RahmanNo ratings yet
- Case Report: A Case of Herpes Simplex Virus-1 Encephalitis From A Medicolegal Point of ViewDocument4 pagesCase Report: A Case of Herpes Simplex Virus-1 Encephalitis From A Medicolegal Point of Viewzefri suhendarNo ratings yet
- Rolul (A) EEG SI NIRS in Diagnosticul, Managmentul Si Prognosticul Convulsiilor NeonataleDocument10 pagesRolul (A) EEG SI NIRS in Diagnosticul, Managmentul Si Prognosticul Convulsiilor Neonataleandreea sfirnaciucNo ratings yet
- Acute Viral Encephalitis in ChildrenDocument16 pagesAcute Viral Encephalitis in ChildrenCF PonceNo ratings yet
- The Diagnosis and Treatment of Autoimmune Encephalitis: Open AccessDocument13 pagesThe Diagnosis and Treatment of Autoimmune Encephalitis: Open AccessFransiska OktavianiNo ratings yet
- tmpD6CD TMPDocument8 pagestmpD6CD TMPFrontiersNo ratings yet
- Ene 12372Document7 pagesEne 12372Andres Rojas JerezNo ratings yet
- The Management of Encephalitis Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis Clinical Practice Guidelines by The Infectious Diseases Society of AmericaNana ShkodinaNo ratings yet
- Paraneoplastic Neurologic Syndromes Are Defined and Characterized by An Inappropriate Immune Response Targeting Native Nervous System Antigens That Are Ectopically Expressed by A Systemic TumorDocument11 pagesParaneoplastic Neurologic Syndromes Are Defined and Characterized by An Inappropriate Immune Response Targeting Native Nervous System Antigens That Are Ectopically Expressed by A Systemic TumorAnonymous ZUaUz1wwNo ratings yet
- Clin Infect Dis.-2008-Tunkel-ENCEFALITISDocument25 pagesClin Infect Dis.-2008-Tunkel-ENCEFALITISJizus GonzalezNo ratings yet
- Appi Neuropsych 18010005Document6 pagesAppi Neuropsych 18010005sarahNo ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- Acute Symptomatic Seizures A Clinically Oriented Review: Pedro Beleza, MDDocument36 pagesAcute Symptomatic Seizures A Clinically Oriented Review: Pedro Beleza, MDHabib BaNo ratings yet
- Practical Neurology (Cerebellar Ataxia)Document11 pagesPractical Neurology (Cerebellar Ataxia)idno1008No ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaVictor Euclides Briones MoralesNo ratings yet
- Epilepsy Update Diagnosis, Classification and ManagementDocument7 pagesEpilepsy Update Diagnosis, Classification and ManagementfelipeNo ratings yet
- Clinical Guideline: Management of The First Unprovoked Epileptic Seizure in Adults and ChildrenDocument6 pagesClinical Guideline: Management of The First Unprovoked Epileptic Seizure in Adults and Childrennaili nsnNo ratings yet
- Part 2diagnostic of NPH PDFDocument13 pagesPart 2diagnostic of NPH PDFrys239No ratings yet
- Diagnosis and Treatment of Autoimmune EncephalitisDocument26 pagesDiagnosis and Treatment of Autoimmune EncephalitisSylvia TrianaNo ratings yet
- Armangue2014Document8 pagesArmangue2014etiyaNo ratings yet
- EncephalitisDocument30 pagesEncephalitisHITIPHYSIO100% (1)
- Management and Outcome Predictors During Herpes Simplex Virus EncephalitisDocument9 pagesManagement and Outcome Predictors During Herpes Simplex Virus Encephalitiscarmen rosa secce pedrazaNo ratings yet
- Encefalitis 2022Document10 pagesEncefalitis 2022SMIBA MedicinaNo ratings yet
- A Case of Male Sle: An Unusual PresentationDocument4 pagesA Case of Male Sle: An Unusual PresentationIJAR JOURNALNo ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaomartorigalNo ratings yet
- Encefalitis AutoinmuneDocument8 pagesEncefalitis AutoinmuneRoosevelt Santibañez Dla TorreNo ratings yet
- Precis of Lancet Neurology Autoimmune Encephalitis Paper Corregido Por Dalmau2 Editora 5 63 1Document10 pagesPrecis of Lancet Neurology Autoimmune Encephalitis Paper Corregido Por Dalmau2 Editora 5 63 1Anonymous S3wsIptcONo ratings yet
- Encephalitis: Diagnosis, Management and Recent Advances in The Field of EncephalitidesDocument10 pagesEncephalitis: Diagnosis, Management and Recent Advances in The Field of EncephalitidesPerlaNo ratings yet
- Diagnosis and Treatment of Rapidly Progressive DementiasDocument16 pagesDiagnosis and Treatment of Rapidly Progressive DementiasAndrea Cayufilo CarmonaNo ratings yet
- Diagnostic Approach To Viral Acute Encephalitis Syndrome (AES) in Paediartric Age Group - A Study From New DelhiDocument5 pagesDiagnostic Approach To Viral Acute Encephalitis Syndrome (AES) in Paediartric Age Group - A Study From New DelhiAkila SwaminathanNo ratings yet
- Epidemiology PDFDocument6 pagesEpidemiology PDFNia ElisaNo ratings yet
- A Case of Sporadic Creutzfeldt-JakobDocument5 pagesA Case of Sporadic Creutzfeldt-JakobVlad PopescuNo ratings yet
- Diagnosis and Treatment of Viral Encephalitis: ReviewDocument10 pagesDiagnosis and Treatment of Viral Encephalitis: ReviewnataliaNo ratings yet
- Epileptic Disorders - 2021 - Leibetseder - How To Distinguish Seizures From Non Epileptic ManifestationsDocument23 pagesEpileptic Disorders - 2021 - Leibetseder - How To Distinguish Seizures From Non Epileptic ManifestationsFranklin SierraNo ratings yet
- CNS Infection: Nurcahaya Sinaga Haji Pemprovsu Hospital, Faculty of Medicine Universitas Muhammadiyah Sumatera UtaraDocument34 pagesCNS Infection: Nurcahaya Sinaga Haji Pemprovsu Hospital, Faculty of Medicine Universitas Muhammadiyah Sumatera Utaramuhammad alqoriNo ratings yet
- Viral EncephalitisDocument19 pagesViral Encephalitishappinesel100% (1)
- Autoimmune EncephalitisDocument39 pagesAutoimmune EncephalitisnurulmaulidyahidayatNo ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Lilavati V/s KEMDocument35 pagesLilavati V/s KEMAshita Doshi100% (1)
- Offshore Pre Asses FormDocument8 pagesOffshore Pre Asses Formwendyphan09No ratings yet
- HbA1c OdtDocument2 pagesHbA1c OdtAhmed Assaf100% (1)
- Annals of Clinical Case ReportsDocument3 pagesAnnals of Clinical Case ReportssheilaNo ratings yet
- Cost Analysis of Mirwais and Nangarhar Regional Hospitals in AfghanistanDocument12 pagesCost Analysis of Mirwais and Nangarhar Regional Hospitals in AfghanistanNational Graduate ConferenceNo ratings yet
- Functions of Different Categories of BSF - BS, BB, Etc. FinalDocument21 pagesFunctions of Different Categories of BSF - BS, BB, Etc. Finalnorth genNo ratings yet
- Bài tập của Trí 19032022Document6 pagesBài tập của Trí 19032022Minh TríNo ratings yet
- Oet Medicine Official Oet Practice Book 1 Cambridge TEST 1 FDocument42 pagesOet Medicine Official Oet Practice Book 1 Cambridge TEST 1 FP.K.No ratings yet
- Fundamentals of NursingDocument51 pagesFundamentals of NursingKimTot OctavianoNo ratings yet
- FICADocument3 pagesFICAIsmi Jihan MidianiNo ratings yet
- Atropine Sulphate 1mg/1ml Emergency MedicationDocument2 pagesAtropine Sulphate 1mg/1ml Emergency MedicationRafiq EsufzaeNo ratings yet
- Tuberculin Skin Test. Prevention of Tuberculosis.: 2. The Department of Tuberculosis of KSMA. Doc. Fydorova S.VDocument46 pagesTuberculin Skin Test. Prevention of Tuberculosis.: 2. The Department of Tuberculosis of KSMA. Doc. Fydorova S.VMadabout MusicNo ratings yet
- Role of Medicinal Herbs in Management of Oral Diseases - A ReviewDocument5 pagesRole of Medicinal Herbs in Management of Oral Diseases - A ReviewIOSRjournalNo ratings yet
- 224 Closed Manipulation Casting of Distal Radius Fractures Fernandez DL 2005 Hand Clin p307-316 PDFDocument10 pages224 Closed Manipulation Casting of Distal Radius Fractures Fernandez DL 2005 Hand Clin p307-316 PDFanindyadputriNo ratings yet
- Clinico Radiological ConferenceDocument67 pagesClinico Radiological ConferenceSharmaine Margaret LeeNo ratings yet
- MCNP Integrated Concepts NP 4Document11 pagesMCNP Integrated Concepts NP 4Karen Mae Santiago AlcantaraNo ratings yet
- Worldwide History of PedodonticsDocument3 pagesWorldwide History of PedodonticsewretrdfNo ratings yet
- Arizona Burncenter Guidelines PDFDocument20 pagesArizona Burncenter Guidelines PDFBuyungNo ratings yet
- Interview: Patient HistoryDocument8 pagesInterview: Patient HistoryquelspectacleNo ratings yet
- Precipitating Factors Predisposing Factors: Sitting Down or Lying Down For Too Long ObesityDocument1 pagePrecipitating Factors Predisposing Factors: Sitting Down or Lying Down For Too Long ObesitySureen RegularNo ratings yet
- Aruna Ramchandra Shanbaug VDocument9 pagesAruna Ramchandra Shanbaug VjaishreeNo ratings yet
- Cheryl Ann Stohler CV by JdsDocument3 pagesCheryl Ann Stohler CV by Jdsapi-236756953No ratings yet
- Pone 0210716Document12 pagesPone 0210716Gemala AdillawatyNo ratings yet
- Benefit Guide AllianzDocument50 pagesBenefit Guide AllianzAbstractSoftNo ratings yet
- Assessment - 3A - Case - Study - of - Mary - With - ADD (1) - 2Document17 pagesAssessment - 3A - Case - Study - of - Mary - With - ADD (1) - 2ericNo ratings yet