Professional Documents
Culture Documents
Management of Infants at Risk of GBS Disease. AAP 2019 Guidelines PDF
Management of Infants at Risk of GBS Disease. AAP 2019 Guidelines PDF
Uploaded by
Eider LeonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Infants at Risk of GBS Disease. AAP 2019 Guidelines PDF
Management of Infants at Risk of GBS Disease. AAP 2019 Guidelines PDF
Uploaded by
Eider LeonCopyright:
Available Formats
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care
Management of Infants at Risk for
Group B Streptococcal Disease
Karen M. Puopolo, MD, PhD, FAAP,a,b Ruth Lynfield, MD, FAAP,c James J. Cummings, MD, MS, FAAP,d COMMITTEE ON FETUS AND
NEWBORN, COMMITTEE ON INFECTIOUS DISEASES
Group B streptococcal (GBS) infection remains the most common cause of abstract
neonatal early-onset sepsis and a significant cause of late-onset sepsis among
young infants. Administration of intrapartum antibiotic prophylaxis is the only
a
currently available effective strategy for the prevention of perinatal GBS early- Department of Pediatrics, Perelman School of Medicine, University of
Pennsylvania, Philadelphia, Pennsylvania; bChildren’s Hospital of
onset disease, and there is no effective approach for the prevention of late-onset Philadelphia, Philadelphia, Pennsylvania; cMinnesota Department of
disease. The American Academy of Pediatrics joins with the American College of Health, St Paul, Minnesota; and dDepartments of Pediatrics and
Bioethics, Alden March Bioethics Institute, Albany Medical College,
Obstetricians and Gynecologists to reaffirm the use of universal antenatal Albany, New York
microbiologic-based testing for the detection of maternal GBS colonization to
This document is copyrighted and is property of the American
facilitate appropriate administration of intrapartum antibiotic prophylaxis. The Academy of Pediatrics and its Board of Directors. All authors have filed
purpose of this clinical report is to provide neonatal clinicians with updated conflict of interest statements with the American Academy of
Pediatrics. Any conflicts have been resolved through a process
information regarding the epidemiology of GBS disease as well current approved by the Board of Directors. The American Academy of
Pediatrics has neither solicited nor accepted any commercial
recommendations for the evaluation of newborn infants at risk for GBS disease involvement in the development of the content of this publication.
and for treatment of those with confirmed GBS infection.
Clinical reports from the American Academy of Pediatrics benefit from
expertise and resources of liaisons and internal (AAP) and external
reviewers. However, clinical reports from the American Academy of
Pediatrics may not reflect the views of the liaisons or the
organizations or government agencies that they represent.
The Centers for Disease Control and Prevention (CDC) first published The guidance in this report does not indicate an exclusive course of
consensus guidelines on the prevention of perinatal group B streptococcal treatment or serve as a standard of medical care. Variations, taking
into account individual circumstances, may be appropriate.
(GBS) disease in 1996. These guidelines were developed in collaboration
with the American Academy of Pediatrics (AAP), the American College of All clinical reports from the American Academy of Pediatrics
automatically expire 5 years after publication unless reaffirmed,
Obstetricians and Gynecologists (ACOG), the American College of Nurse- revised, or retired at or before that time.
Midwives, the American Academy of Family Physicians, and other
DOI: https://doi.org/10.1542/peds.2019-1881
stakeholder organizations1 on the basis of available evidence as well as
expert opinion. The 1996 consensus guidelines recommended either an Address correspondence to Karen M. Puopolo, MD, PhD. E-mail:
puopolok@email.chop.edu
antenatal culture–based or risk factor–based approach for the
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
administration of intrapartum antibiotic prophylaxis (IAP) to prevent
invasive neonatal GBS early-onset disease (EOD).1 The guidelines were Copyright © 2019 by the American Academy of Pediatrics
updated in 2002 primarily on the basis of new data from a CDC multistate
retrospective cohort study in which authors found universal screening for To cite: Puopolo KM, Lynfield R, Cummings JJ, AAP
group B streptococci (Streptococcus agalactiae) was .50% more effective COMMITTEE ON FETUS AND NEWBORN, AAP COMMITTEE ON
at preventing the disease compared to a risk-based approach.2,3 In 2010, INFECTIOUS DISEASES. Management of Infants at Risk for
Group B Streptococcal Disease. Pediatrics. 2019;144(2):
the CDC once again revised the GBS perinatal prevention guidelines and
e20191881
continued to endorse the universal antenatal culture–based approach to
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019:e20191881 FROM THE AMERICAN ACADEMY OF PEDIATRICS
identify women who would receive from blood, cerebrospinal fluid (CSF), hospital discharge with culture-
IAP to prevent GBS EOD.4 Notable or another normally sterile site from confirmed infection attributable to
changes in the 2010 revision birth through 6 days of age.8 Active any bacteria to be approximately 5
addressed the use of IAP for women Bacterial Core surveillance (ABCs), cases per 100 000 live births.14
in preterm labor and those with performed in collaboration with the Globally, outside the United States, an
preterm prelabor rupture of CDC in 10 states from 2006 to 2015, estimated 200 000 cases of GBS EOD
membranes (PROM), the choice of found that the overall incidence of occurred in 2015. Stillbirth, GBS EOD,
specific antibiotics for IAP, and the GBS EOD declined from 0.37 cases and late-onset GBS cases combined
use of nucleic acid amplification tests per 1000 live births in 2006 to 0.23 contribute to an estimated 150 000
(NAATs) to identify maternal GBS cases per 1000 live births in 2015.6 fetal and neonatal deaths throughout
colonization. The 2010 revision Meningitis was diagnosed in 9.5% of the world, with the largest
included a neonatal management infants with GBS EOD. CSF culture- concentration of GBS perinatal deaths
algorithm for secondary prevention of positive GBS EOD occurred in the occurring in Africa.15
GBS EOD that was widely adopted by absence of bacteremia in 9.1% of
neonatal physicians as a means of early-onset meningitis cases Late-Onset GBS Disease
managing risk of all bacterial causes (incidence: approximately 2.5 cases GBS late-onset disease (LOD) is
of early-onset sepsis (EOS).5 With per 1 million live births).6 Infants defined as isolation of GBS from
implementation of universal maternal born at ,37 weeks’ gestation account a normally sterile site from 7 to
antenatal screening and IAP, the for 28% of all GBS cases; 89 days of age.8 Rarely, very–late-
national incidence of GBS EOD has approximately 15% of cases occur onset GBS disease may occur after
declined from 1.8 cases per 1000 live among preterm infants with very low 3 months of age, primarily among
births in 1990 to 0.23 cases per 1000 birth weight (,1500 g).6,9 Overall, infants born very preterm or infants
live births in 2015.6 GBS infection accounts for with immunodeficiency syndromes.16,
17
Evolving epidemiology, newly approximately 45% of all cases of GBS LOD rates have not changed
published data, and changing practice culture-confirmed EOS among term with widespread use of IAP. GBS LOD
standards inform periodic review infants and approximately 25% of all incidence was stable over the
of practice guidelines. In 2017, EOS cases that occur among infants 2006–2015 ABCs study period, with
representatives from the CDC, AAP, with very low birth weight.9,10 Death an average incidence of 0.31 cases
ACOG, and other stakeholder attributable to GBS EOD occurs per 1000 live births.6 The median age
organizations agreed to review and primarily among preterm infants: the at presentation with GBS LOD was
revise the 2010 GBS guidelines. A current case fatality ratio is 2.1% 34 days (interquartile range: 20–49
consensus was reached that the among term infants and 19.2% days). Bacteremia was identified in
AAP would revise neonatal care among those born at ,37 weeks’ approximately 93% of GBS LOD, and
recommendations and ACOG would gestation.6 bacteremia without focus was the
revise obstetric care guidelines. These most common form of disease. Group
GBS EOD primarily presents clinically B streptococci were isolated from CSF
separate but aligned publications
at or shortly after birth. The majority in 20.7% of cases, and meningitis was
replace the CDC 2010 GBS perinatal
of infants become symptomatic by 12 diagnosed in 31.4% of cases. Cultures
guidance.
to 24 hours of age11–13; during the of bone and joint and peritoneal fluid
This clinical report addresses the 2006–2015 period of ABCs, 94.7% of yielded group B streptococci in
epidemiology, microbiology, disease GBS EOD cases were diagnosed #48 1.8% of cases. CSF culture-positive
pathogenesis, and management hours after birth.6 The incidence of GBS LOD occurred in the absence
strategies for neonatal early- and late- newborn infants discharged from of bacteremia in approximately
onset GBS infection. Maternal a birth hospital and readmitted to 20% of late-onset meningitis cases
management is addressed in ACOG a hospital with GBS EOD within (incidence: 1.9 cases per 100 000 live
Committee Opinion No. 782, 6 days of age was approximately 0.3 births). Infants born at ,37 weeks’
“Prevention of Group B Streptococcal cases per 100 000 live births in the gestation account for approximately
Early-Onset Disease in Newborns.”7 ABCs. Although potentially an 42% of all GBS LOD cases, and death
underestimate, this finding was attributable to GBS LOD occurs in
CURRENT EPIDEMIOLOGY OF NEONATAL consistent with data from the preterm infants at roughly twice the
GBS INFECTION Northern California Kaiser rate of term infants (7.8% vs 3.4%,
Permanente health care system, respectively).6 GBS LOD complicated
Early-Onset GBS Infection which found the incidence of by meningitis has a higher patient
GBS EOD is defined as isolation of newborn infants readmitted to the fatality rate than those with other
group B Streptococcus organisms hospital within the first week after syndromes.
Downloaded from www.aappublications.org/news by guest on July 24, 2019
2 FROM THE AMERICAN ACADEMY OF PEDIATRICS
PATHOGENESIS OF AND RISK FACTORS Multiple clinical characteristics appropriate use of these procedures
FOR GBS INFECTION associated with greater risk of among GBS-colonized women.7
maternal GBS colonization and with Administration of IAP in women with
EOD
the pathogenesis of GBS EOD are GBS colonization minimizes the impact
Group B Streptococcus emerged as the predictive of neonatal disease.20,21,34–43 of intrapartum obstetric procedures on
primary bacterial cause of EOS in the Lower gestational age is associated the risk of neonatal GBS EOD.
1970s, and subsequent studies with less effective opsonic, neutrophil-
identified maternal GBS colonization LOD
mediated defenses in the infant as well
as the primary risk factor for GBS- as lower levels of protective maternally A positive GBS screen result in the
specific EOS.18–20 The most common derived antibody.44–46 Increased mother at the time of birth and at the
pathogenesis of GBS EOD is that of duration of rupture of membranes time of LOD diagnosis is significantly
ascending colonization of the uterine (ROM) promotes the process of associated with LOD.48,49 Maternal
compartment with group B ascending colonization and infection of colonization is not universally present
streptococci that are present in the the uterine compartment and fetus. in LOD cases, however, suggesting that
maternal gastrointestinal and Maternal intrapartum fever may reflect horizontal acquisition of group B
genitourinary flora. Infection occurs the maternal inflammatory response to streptococci from nonmaternal
with subsequent colonization and evolving intraamniotic bacterial caregivers may also be part of the
invasive infection of the fetus and/or infection and is an important predictor pathogenesis of GBS LOD. GBS LOD is
fetal aspiration of infected amniotic of neonatal early-onset infection. strongly associated with preterm
fluid. This pathogenesis primarily African American race and, less birth.6,48–53 In studies from
occurs during labor for term infants, Washington in 1992 to 2011 and
consistently, a maternal age ,20 years
but the timing is less certain among Houston in 1995 to 2000, it was found
have been associated with a higher risk
preterm infants for whom that the risk for LOD increased for
of GBS EOD.10,34,37,39 The independent
intraamniotic infection may be the each week of decreasing gestation and
contribution of these factors remains
cause of PROM and/or preterm 40% to 50% of all LOD occurs among
unclear because maternal age and race
labor.21 Rarely, GBS EOD may develop infants born ,37 weeks’ gestation.48,
are also associated with higher rates of
at or near term before the onset of 50
Maternal age ,20 years and African
GBS colonization, preterm birth, and
labor, potentially because of group B American race are variably associated
socioeconomic disadvantage, and
streptococci traversing exposed but with neonatal GBS LOD in United
African American race has been
intact membranes. GBS EOD also is States studies.10,48,50,51 Other clinical
associated with a greater likelihood of
associated with stillbirth.22,23 intrapartum factors predictive of GBS
missed antenatal screening.37,41 The
EOD (maternal intrapartum fever,
Maternal colonization is delivery of a previous infant with GBS
duration of ROM) are not predictive of
a prerequisite for GBS EOD. Authors EOD is associated with increased risk
LOD. Authors of a population-based
of a recent meta-analysis estimated in a subsequent delivery,3 a factor that study in Italy found that group B
that globally, GBS colonization was may be related to poor maternal streptococci could be cultured from
detected at vaginal and/or rectal sites antibody responses to colonizing a mother’s milk in approximately 25%
in 18% of pregnant women, with strains or other immune- or strain- of cases that occurred in breastfed
regional variation of 11% to 35%.24 specific factors.42 GBS bacteriuria is infants,49 and authors of case reports
Authors of most clinical studies in the associated with a high level of maternal associate colonized human milk with
United States have found colonization colonization and increased risk of GBS LOD.54 However, human
rates of 20% to 30% among pregnant neonatal colonization and disease.41,47 milk–associated GBS antibody is
women,14,25–28 with variation by Finally, obstetric practices that may protective against GBS LOD,55 and it
maternal age and race. Colonization promote ascending bacterial infection, remains unclear whether human milk
can be ongoing or intermittent among such as the frequency of intrapartum is simply a marker of heavy maternal
pregnant and nonpregnant women.28, vaginal examinations, invasive fetal and infant colonization or a source of
29 monitoring, and membrane sweeping,
Transmission of group B infection.
streptococci from mother to infant have been associated with GBS EOD in
usually occurs shortly before or some observational studies.39,44 Such GBS Virulence
during delivery. In the absence of IAP, studies are difficult to interpret Bacterial factors promote invasive
approximately 50% of newborn because of confounding; available data GBS infection. Group B streptococci
infants born to mothers positive for are not sufficient to determine if these are characterized by immunologically
GBS become colonized with group B procedures are associated with an distinct surface polysaccharide
streptococci, and of those, 1% to 2% increased risk for GBS EOD. Current capsules that define 10 serotypes
will develop GBS EOD.30–33 ACOG guidance addresses the (types I, Ia, and II–IX). Worldwide,
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 3
serotypes I–V account for 98% of delivery interrupts vertical isolates among women with
carriage and 97% of infant invasive transmission of group B streptococci a penicillin allergy.
strains; serotype III accounts for and decreases the incidence of
approximately 25% of colonizing invasive GBS EOD.30–32,63 IAP is Updated ACOG recommendations
strains and approximately 62% of hypothesized to prevent neonatal GBS address the indications for IAP.7 IAP at
invasive infant strains, with regional disease in 3 ways: (1) by temporarily the time of presentation for delivery is
variation.24,56 Surveillance data in the indicated for all women with GBS
decreasing maternal vaginal GBS
United States for invasive strains colonization identified by antenatal
colonization burden; (2) by preventing
from 2006 to 2015 revealed that vaginal-rectal culture, for women with
surface and mucus membrane
93.1% of GBS EOD cases were GBS bacteriuria identified at any point
colonization of the fetus or newborn;
attributable to serotypes Ia (27.3%), during pregnancy, for women with
and (3) by reaching levels in newborn
III (27.3%), II (15.6%), V (14.2%), a history of a previous infant with GBS
bloodstream above the minimum
and Ib (8.8%); the proportion disease, and for women who present
inhibitory concentration (MIC) of the
attributable to the emerging serotype in preterm labor and/or with PROM at
antibiotic for killing group B
,37 0/7 weeks’ gestation. Women
IV ranged from 3.4% to 11.3% over streptococci.30,31 Current clinical
the study period.6 Serotype III who present in labor at $37 0/7
practices are focused on the
accounted for approximately 56.2% weeks’ gestation with unknown GBS
identification of women at highest risk
of 1387 GBS LOD cases during status should receive IAP if risk factors
of GBS colonization and/or of
2006–2015, with serotypes Ia (20%), develop during labor (maternal
transmission of group B streptococci
V (8.3%), IV (6.2%), and Ib (6.1%) intrapartum temperature $100.4°F
to the newborn infant to facilitate
making up most of the remaining [38°C] or duration of ROM $18 hours)
targeted administration of IAP.
serotypes. The capsular or if the result of an available point-of-
polysaccharide of all GBS serotypes The ACOG currently recommends care NAAT is positive for group B
resists complement deposition and universal antenatal testing of streptococci. If a woman with
inhibits opsonophagocytosis. pregnant women for GBS colonization unknown status has a negative point-
Maternally derived, serotype-specific by using vaginal-rectal cultures of-care NAAT test result but develops
antibody to maternal colonizing GBS obtained at 36 0/7 to 37 6/7 weeks’ intrapartum risk factors, IAP should be
isolates is protective against newborn gestation.7 GBS testing is also administered because the sensitivity of
infection.44,45 Group B streptococci recommended for pregnant women the NAAT may be decreased without
express multiple additional virulence who present in preterm labor and/or an enrichment incubation step.
factors, including surface proteins with PROM before 37 0/7 weeks’ Women with GBS colonization in one
such as the a and b C-proteins that gestation. If maternal GBS pregnancy have an estimated 50% risk
promote adherence and immune colonization is identified by antenatal of colonization in a subsequent
evasion, pore-forming toxins such as urine culture, it does not need to be pregnancy.64 Therefore, current ACOG
b-hemolysin and CAMP factor, and reconfirmed by vaginal-rectal culture. recommendations state that if
secreted proteases such as the C5a GBS vaginal-rectal culture is a woman with unknown GBS status
peptidase that cleaves complement.57 optimally performed by using a broth presents in labor and is known to have
Strains vary in their expression of enrichment step, followed by GBS had GBS colonization in a previous
virulence factors, many of which are identification by using traditional pregnancy, IAP may be considered.
highly regulated by 2-component microbiologic methods or by NAAT-
regulatory systems.58–62 The based methods. At some centers, Recommended Antibiotics for GBS
hypervirulent serotype III multilocus NAATs may be used to perform real- IAP to Prevent Neonatal GBS EOD
sequence type 17 (ST17), for time, point-of-care screening of Group B streptococci remain
example, is commonly found in cases women who present in labor with susceptible to b-lactam antibiotics,
of GBS meningitis.6,23 unknown GBS status. Point-of care and penicillin G and ampicillin are the
NAAT-based screening is not the antibiotics best studied for
primary recommended approach to prevention of neonatal infection.
IAP FOR THE PREVENTION OF determine maternal colonization Penicillin G administered to the
EARLY-ONSET GBS INFECTION status, both because of variable mother readily crosses the placenta,
reported sensitivity of the point-of- reaching peak cord blood
Prevention of Perinatal GBS Infection care NAAT as compared to concentrations by 1 hour and rapidly
Multiple observational studies and 1 traditional culture and because most declining by 4 hours, reflecting
randomized controlled trial have NAAT-based testing cannot be used elimination of the antibiotic by the
revealed that the administration of to determine the antibiotic fetal kidney into amniotic fluid.65
intrapartum antibiotics before susceptibility of colonizing GBS Ampicillin has been detected in cord
Downloaded from www.aappublications.org/news by guest on July 24, 2019
4 FROM THE AMERICAN ACADEMY OF PEDIATRICS
blood within 30 minutes and in of clindamycin prophylaxis.72–75 alternative medications for GBS IAP
amniotic fluid within 45 minutes of Authors of 1 study of 21 women when maternal allergy precludes the
administration to the mother.30 colonized with clindamycin-susceptible use of b-lactam antibiotics. These
Ampicillin concentrations measured GBS isolates found vaginal GBS colony medications are likely to provide
in 115 newborn infants at 4 hours of counts declined with administration of some protection against GBS infection
age were found to be greater than the clindamycin IAP.72 Clindamycin for both mother and newborn infant
GBS MIC if maternal IAP dosing administered intravenously to 23 when antimicrobial susceptibility
occurred at least 15 minutes before women for high-risk penicillin allergy testing supports the use of these
delivery.66 Ampicillin IAP decreases resulted in cord blood concentrations second-line agents. In addition, new
maternal vaginal colonization and that were 37% to 160% of maternal ACOG recommendations encouraging
prevents neonatal surface concentrations and within therapeutic the use of penicillin allergy testing in
colonization in 97% of cases if IAP is ranges in 22 of the 23.75 However, pregnant women with uncertain or
administered at least 2 hours before clindamycin undergoes hepatic undocumented histories of penicillin
delivery.30,32 Penicillin G has metabolism and is poorly excreted in reactions are intended to increase the
a narrower antimicrobial spectrum fetal urine and, therefore, does not number of pregnant women who can
compared to ampicillin and therefore reach significant concentrations in safely receive b-lactam–based
remains the preferred agent, but amniotic fluid until multiple doses are regimens for GBS IAP.7
ampicillin is acceptable. administered.73,74 The clinical
effectiveness of clindamycin as IAP IAP and GBS EOD
Alternative Antibiotics for GBS IAP administered a median of 6 hours The pharmacokinetics and
before delivery was only 22% pharmacodynamics of ampicillin,
Cefazolin is recommended for GBS
compared to no IAP in an ABCs study penicillin, and cefazolin suggest that
IAP for women with a penicillin
that included women treated with effective GBS EOD prophylaxis may be
allergy who are at low risk for
clindamycin during the time periods of achieved within 2 to 4 hours of
anaphylaxis7 and has similar
1998–1999 and 2003–2004.76 maternal administration. The clinical
pharmacokinetics and mechanisms of
effectiveness of different durations of
action as ampicillin. Cefazolin rapidly Vancomycin is recommended for use
GBS IAP was evaluated by using
crosses the placenta and is detected as GBS IAP for women with
a data set including 7691 births
in cord blood and amniotic fluid at a penicillin allergy who are at high
collected as part of the ABCs system
levels above the GBS MIC within risk for anaphylaxis if colonized with
from 2003 to 2004. In this study, the
20 minutes after maternal clindamycin-resistant GBS isolates.
administration of different durations
administration.67–70 Although authors of older studies
of penicillin or ampicillin ($4; 2–,4;
using ex vivo perfusion models with
Clindamycin is recommended for GBS or ,2 hours before delivery) were
placental lobules suggested that
IAP for women with a penicillin compared to no administration to
vancomycin crosses the placental
allergy who are at high risk for evaluate the effectiveness of each in
poorly, authors of a subsequent study
anaphylaxis and who are colonized preventing GBS EOD. Although all
of 13 women undergoing elective
with GBS known to be susceptible to regimens were effective compared to
cesarean delivery found cord blood
clindamycin.7 Group B streptococci no IAP, administration of IAP at $4
concentrations of vancomycin greater
are increasingly resistant to hours before delivery was most
than the GBS MIC within 30 minutes
clindamycin as well as to macrolide effective in preventing GBS EOD.76
of maternal drug administration.77,78
antibiotics such as erythromycin. In This study was limited by the fact that
Authors of recent studies compared
reports from the ABCs from 2016, 85% of the cases occurred among
cord blood vancomycin
authors found that 42% of GBS infants born to women who screened
concentrations after vancomycin was
isolates were resistant to clindamycin negative for GBS or whose GBS status
administered to pregnant women
and 54% were resistant to was unknown, meaning that in most
using standard dosing and maternal
erythromycin.71 Because of both poor cases, GBS IAP was administered in
weight-based dosing.79,80 Therapeutic
placental kinetics and high levels of response to risk factors and not as
maternal and cord blood vancomycin
resistance, erythromycin is no longer prophylaxis for known maternal GBS
concentrations were achieved in most
recommended for GBS IAP.7 colonization. Despite this limitation,
cases with weight-based dosing. The
Antibiotic susceptibility data for the this study, combined with the time-
ACOG currently recommends weight-
maternal colonizing GBS isolate dependent bactericidal mechanism of
based dosing for vancomycin when
should be available to support the use action of b-lactam antibiotics,
this agent is indicated for IAP.
of clindamycin for IAP in women who supports the effectiveness of
report a penicillin allergy. Several Current data support the use of ampicillin and penicillin administered
studies inform the potential efficacy clindamycin and vancomycin as at least 4 hours before delivery. No
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 5
data specifically inform the clinical RISK ASSESSMENT FOR EARLY-ONSET fluid Gram-stain and/or culture or
effectiveness of cefazolin IAP, but the GBS INFECTION by placental histopathologic testing.
pharmacokinetics and mechanism of Because the pathogenesis of GBS EOD Such clear diagnostic information
bacterial killing action for cefazolin are begins with vertical transmission of will rarely be available at the time of
similar enough to those of penicillin group B streptococci from mother to delivery for infants born at or near
and ampicillin that the administration fetus and newborn infant, the term. Suspected intraamniotic
of cefazolin can be considered to strongest predictor of GBS EOD is infection is defined as a single
provide adequate prophylaxis against maternal GBS colonization. Other maternal intrapartum temperature
GBS EOD. Although data regarding the factors that are important to the $39.0°C or maternal temperature of
pharmacokinetics of clindamycin and pathogenesis of GBS EOD, such as the 38.0°C to 38.9°C in combination with
vancomycin have been published, virulence of the maternal colonizing 1 or more of maternal leukocytosis,
evidence regarding their clinical isolate and the presence of maternal purulent cervical drainage, or fetal
efficacy is more limited. Therefore, for serotype-specific protective antibody, tachycardia. Recognizing the
the purpose of newborn GBS EOD risk cannot be known to the physician at uncertainties surrounding the
assessment, when non–b-lactam the time of neonatal risk assessment. diagnosis of intraamniotic infection,
antibiotics of any duration are The remaining clinical risk factors for the ACOG recommends that
administered for GBS IAP, such GBS EOD are the same as those for intrapartum antibiotic therapy be
treatment should be considered as not EOS caused by other common administered whenever intra-
fully adequate in neonatal risk bacterial causes of EOS, including amniotic infection is diagnosed or
calculation. gestational age at birth, intraamniotic suspected and should be considered
infection, and duration of ROM. The when otherwise unexplained
IAP and GBS LOD isolated maternal temperature 38.0°
administration of GBS IAP and the
There is no epidemiological evidence administration of intrapartum C to 38.9°C is present.85
to suggest a protective effect of GBS antibiotics in response to obstetric • The routine measurement of
IAP for the prevention of GBS LOD. concern for intraamniotic infection complete blood cell counts or
This observation is likely attributable both decrease this risk. The newborn inflammatory markers such as
to the dynamic nature of GBS infant’s condition at birth and C-reactive protein alone in
colonization. Early studies of IAP evolving condition over the first 12 to newborn infants to determine risk
demonstrated initial maternal vaginal 24 hours after birth are strong of GBS EOD is not justified given
and/or rectal GBS clearance with IAP, predictors of early-onset infection the poor test performance of these
followed by recolonization with group attributable to any pathogen.12,13 in predicting what is currently
B streptococci within 24 to 48 hours a low-incidence disease.86–89
after birth.30 Authors of a study in Previous guidance on GBS EOD risk
assessment presented challenges to • Newborn clinical illness consisting
Italy found that approximately 25% of
physicians because of practical of abnormal vital signs (eg,
infants born to mothers with GBS
difficulties in establishing the tachycardia, tachypnea, and/or
colonization who received GBS IAP
obstetric diagnosis of maternal temperature instability),
were colonized by 1 month of age.
chorioamnionitis or intraamniotic supplemental oxygen requirement
Molecular analysis revealed the infant
infection, absence of guidance on what and/or need for continuous
colonization was attributable to the
defines abnormal laboratory test positive airway pressure,
same strain colonizing the mother
results in the newborn infant, and mechanical ventilation, or blood
antepartum.81 Similarly, authors of
a lack of clear definitions for newborn pressure support can be used to
a longitudinal cohort study conducted
clinical illness. Each of these concerns predict early-onset infection.13
in Japan from 2014 to 2015 observed
are addressed in detail in the current There is no evidence that
that among neonates born to mothers
AAP clinical reports on management hypoglycemia occurring in isolation
with GBS colonization who received
of neonates with suspected or proven in otherwise well-appearing infants
IAP, approximately 20% were
colonized with group B streptococci at early-onset bacterial sepsis.83,84 In is a risk factor for GBS EOD or EOS.
summary, at this time, evidence A newborn’s clinical condition often
1 week and/or 1 month of age.82 The
supports the following: evolves in the hours after birth, and
authors also observed that 6.5% of
physicians must exercise judgment
infants born to mothers who screened • The ACOG provides guidance
to distinguish transitional instability
negative for GBS were colonized at regarding intraamniotic infection85;
from signs of clinical illness.
1 week and/or 1 month of age, likely neonatal risk assessment can be
as a result of horizontal transmission informed by this guidance. The Clinicians should recognize that GBS
from newly colonized mothers as well definitive diagnosis of intraamniotic EOD can occur among term infants
as from other contacts. infection is that made by amniotic born to mothers who have screened
Downloaded from www.aappublications.org/news by guest on July 24, 2019
6 FROM THE AMERICAN ACADEMY OF PEDIATRICS
negative for GBS. Authors of 1 single- molecular identification techniques born at or near term ($35 weeks’
center study with policies mandating reveal that approximately 7% to 8% gestation) and those preterm (#34
universal screening-based GBS IAP of women who screen negative for 6/7 weeks’ gestation). A summary of
found that over an 8-year period, 17 GBS will be identified as positive for the management strategies provided
GBS EOD cases occurred among term GBS at the time of delivery.27,91 In in the previous AAP reports are
infants and 14 of 17 (82.4%) of the some proportion of these cases, provided here.
mothers had screened negative for additional risk factors for EOS were
GBS.90 Multistate ABCs data in present, but GBS EOD can develop in There Are 3 Current Approaches to
2003–2004 identified 189 cases of newborn infants without additional Risk Assessment Among Infants Born
GBS EOD among term infants and risk, and these will only be identified at ‡35 Weeks’ Gestation
determined that 116 of 189 (61.4%) when they develop signs of illness. • Categorical risk assessment:
occurred among infants born to Nonetheless, most infants who Categorical risk factor assessment
women who screened negative for develop GBS EOD will do so in the uses risk factor threshold values to
GBS.37 GBS EOD may occur in infants setting of specific risk factors. In the identify infants at increased risk for
of mothers who screened negative for current era of widespread use of GBS GBS EOD (Fig 1A). Different
GBS because of changes in maternal IAP, the clinical approach to risk of versions of this approach have been
colonization status during the GBS EOD should be the same as that published since 1996 and are based
interval from screening to for all bacterial causes of early-onset on infection epidemiology and
presentation for delivery or because infection. As addressed in the AAP expert opinion. For the purpose of
of an incorrect technique in obtaining clinical reports on management of categorical risk assessment,
vaginal and rectal screening cultures neonates with suspected or proven maternal intrapartum temperature
or in laboratory processing. Studies early-onset bacterial sepsis,83,84 risk $38.0°C is used as a surrogate for
comparing antepartum culture to of early-onset infection should be intraamniotic infection. The
intrapartum culture or intrapartum considered separately for infants administration of penicillin G,
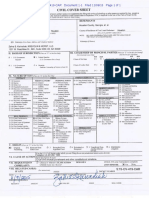
FIGURE 1
Options for EOS risk assessment among infants born $35 weeks’ gestation. A, Categorical risk assessment. B, Neonatal Early-Onset Sepsis Calculator. The
screenshot of the Neonatal Early-Onset Sepsis Calculator (https://neonatalsepsiscalculator.kaiserpermanente.org/) was used with permission from
Kaiser-Permanente Division of Research. C, Enhanced observation. a Consider lumbar puncture and CSF culture before initiation of empiric antibiotics for
infants who are at the highest risk of infection, especially those with critical illness. Lumbar puncture should not be performed if the infant’s clinical
condition would be compromised, and antibiotics should be administered promptly and not deferred because of procedure delays. b Adequate GBS IAP is
defined as the administration of penicillin G, ampicillin, or cefazolin $4 hours before delivery.
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 7
ampicillin, or cefazolin $4 hours probability of 0.5/1000, unless local those who develop signs of illness
before delivery is considered incidence of EOS is known to differ over the first 48 hours after birth
adequate GBS IAP; other antibiotics from the national incidence of EOS are treated empirically with
or other durations of treatment ,4 among term infants. The models do antibiotics.93–95 One center
hours are considered inadequate account for the content and timing reported the use of clinical
when using this approach. of GBS-specific IAP. When using observation for initially well-
Substantial data have been these models, only penicillin, appearing infants born at $34 to
reported on the impact of using ampicillin, or cefazolin should be 35 weeks’ gestation to mothers
categorical risk factors to manage considered as “GBS-specific with the obstetric diagnosis of
the risk of GBS EOD.3,14,36,40 antibiotics.” The administration of chorioamnionitis. Whether
However, the risk is highly variable clindamycin or vancomycin alone observed in a setting with
among the newborn infants for IAP for any duration is currently continuous monitoring or with
recommended to receive empirical recommended to be entered as “no serial examinations during
treatment in this approach, ranging antibiotics.” Because the models maternal-infant couplet care, this
from slightly lower than the were developed to predict risk of all center ultimately administered
baseline population risk to bacterial causes of EOS (and not just empirical antibiotics to 5% to 12%
significantly higher, depending on GBS EOD), and because these of such infants.94,95 Centers that
the gestational age, duration of models account for other antibiotic adopt this approach will need to
ROM, and timing and content of types and indications for establish processes to ensure serial,
intrapartum antibiotic structured, documented physical
administered intrapartum
administration, “GBS specific assessments and develop clear
antibiotics. Consequently,
antibiotics .2 hours prior to birth” criteria for additional evaluation
a limitation of this approach is that
is 1 of the calculator variables. The and empirical antibiotic
categorical management will result
2-hour timing is used because administration. Physicians and
in empirical treatment of many
multiple factors in addition to GBS families must understand that the
relatively low-risk newborn infants.
IAP are considered when using the identification of initially well-
• Multivariate risk assessment (the multivariate models in the Neonatal appearing infants who develop
Neonatal Early-Onset Sepsis Early-Onset Sepsis Calculator. Used clinical illness is not a failure of
Calculator): Multivariate risk in this manner, threshold risk care, but rather an anticipated
assessment integrates the individual estimates prompting enhanced outcome of this approach to GBS
infant’s combination of risk factors clinical observation or blood culture EOD risk management.
and the newborn infant’s clinical and empirical antibiotic therapy
condition to estimate an individual For Infants Born at £34 Weeks’
have been prospectively validated in
Gestation, the Optimal Approach to
infant’s risk of EOS, including GBS large newborn cohorts.14,92 Centers
Risk Assessment for All EOS Should
EOD. Predictive models based on that opt for this approach to risk Be Applied to Risk of GBS EOD
gestational age at birth, highest assessment should develop methods
maternal intrapartum temperature, to calculate the risk estimate for all The circumstances of preterm birth
maternal GBS colonization status, newborn infants born at $35 may provide the best current
duration of ROM, and type and weeks’ gestation and will need to approach to GBS EOD management for
duration of intrapartum antibiotic develop a structured approach to preterm infants (Fig 2). Clinicians may
therapies have been developed and close clinical observation of infants adopt one of the following strategies
validated.13,38 These models are to develop institutional approaches
at specific levels of estimated risk.
available as a Web-based Neonatal best suited to their local resources and
• Risk assessment based on newborn structure of care (Fig 1).
Early-Onset Sepsis Calculator clinical condition: A final approach
(Fig 1B) (https:// • Preterm infants at highest risk for
to GBS EOD risk assessment is to
neonatalsepsiscalculator. EOS: Infants born preterm because
rely on clinical signs of illness to
kaiserpermanente.org) that includes of cervical insufficiency, preterm
identify infants who may be at
recommended clinical actions to be labor, PROM, intraamniotic infection,
taken at specific levels of predicted increased risk of infection. Among and/or acute and otherwise
risk. The models begin with the term infants, good clinical unexplained onset of nonreassuring
previous probability of infection, condition at birth is associated with fetal status are at the highest risk of
and because they predict all an approximately 60% to 70% EOS and GBS EOD. The
bacterial causes of EOS and not only reduction in risk for early-onset administration of GBS IAP may
GBS EOD, physicians in the United infection.13 Under this approach, decrease the risk of infection among
States should enter a previous infants who appear ill at birth and these infants, but the most
Downloaded from www.aappublications.org/news by guest on July 24, 2019
8 FROM THE AMERICAN ACADEMY OF PEDIATRICS
reasonable approach to these blood culture and clinical those infants who are well
infants is to obtain a blood culture monitoring. For infants who do not appearing at birth and to obtain
and start empirical antibiotic improve after initial stabilization a blood culture and to initiate
treatment. A lumbar puncture for and/or those who have severe antibiotic therapy for infants with
culture and analysis of CSF should systemic instability, the respiratory and/or cardiovascular
be considered in clinically ill infants administration of empirical instability after birth.
when there is a high suspicion for antibiotics may be reasonable but
GBS EOD, unless the procedure will is not mandatory. CLINICAL PRESENTATION AND
compromise the neonate’s clinical • Infants delivered for maternal and/ TREATMENT OF GBS INFECTION
condition. or fetal indications but who are Newborn infants with GBS EOD may
• Preterm infants at lower risk for ultimately born by vaginal or present with signs of illness ranging
EOS: Preterm infants at lowest risk cesarean delivery after efforts to from tachycardia, tachypnea, or
for all EOS and for GBS EOD are induce labor and/or with ROM lethargy to severe cardiorespiratory
those born under circumstances before delivery are subject to failure, persistent pulmonary
that include all of these criteria96, factors associated with the hypertension of the newborn, and
97
: (1) maternal and/or fetal pathogenesis of GBS EOD. If the perinatal encephalopathy. GBS LOD
indications for preterm birth (such mother has an indication for GBS most commonly occurs as bacteremia
as maternal preeclampsia or other IAP and adequate IAP (penicillin, without a focus and is often
noninfectious medical illness, ampicillin, or cefazolin $4 hours characterized by fever ($38°C) as
placental insufficiency, or fetal before delivery) is not given or if well as lethargy, poor feeding,
growth restriction), (2) birth by any other concern for infection irritability, tachypnea, grunting, or
cesarean delivery, and (3) absence arises during the process of apnea. Infants with LOD meningitis
of labor, attempts to induce labor, delivery, the infant should be can also have nonspecific signs such
or any ROM before delivery. managed as recommended above as irritability, poor feeding, vomiting,
Acceptable initial approaches to for preterm infants at higher risk and temperature instability as well as
these infants include (1) no for GBS EOD. Otherwise, an signs suggestive of central nervous
laboratory evaluation and no acceptable approach to these systems involvement such as bulging
empirical antibiotic therapy or (2) infants is close observation for fontanelle or seizures. Focal
FIGURE 2
EOS risk assessment among infants born #34 weeks’ gestation. a Intraamniotic infection should be considered when a pregnant woman presents with
unexplained decreased fetal movement and/or there is sudden and unexplained poor fetal testing. b Lumbar puncture and CSF culture should be
performed before initiation of empiric antibiotics for infants who are at the highest risk of infection unless the procedure would compromise the infant’s
clinical condition. Antibiotics should be administered promptly and not deferred because of procedural delays. c Adequate GBS IAP is defined as the
administration of penicillin G, ampicillin, or cefazolin $4 hours before delivery. d For infants who do not improve after initial stabilization and/or those
who have severe systemic instability, the administration of empiric antibiotics may be reasonable but is not mandatory.
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 9
syndromes such as pneumonia, bone has identified rare isolates of group B a b-lactam, cephalosporin, or
or joint infection, cellulitis, or adenitis streptococci with mutations in vancomycin. When group B
often have findings that point to the penicillin-binding proteins leading to streptococci are identified in culture,
site of infection. Osteomyelitis elevated MICs (nonsusceptibility) to penicillin G is the drug of choice, with
frequently is insidious and may not b-lactam antibiotics.99 Ampicillin, ampicillin as an acceptable
be associated with fever. together with an aminoglycoside, is alternative therapy.
Complications are common for the primary recommended therapy
See Table 1 for dose and interval
meningitis and can include for infants up to 7 days of age. The
guidance. The length of antibiotic
neurodevelopment impairment, empirical addition of broader-
treatment is generally 10 days for
hearing loss, persistent seizure spectrum therapy should be
bacteremia without focus and 14 days
disorders, or cerebrovascular considered if there is strong clinical
for uncomplicated meningitis;
disease.98 concern for ampicillin-resistant
antibiotics should be given
infection in a critically ill newborn,
Evaluation for GBS disease is the intravenously for the entire course.
particularly among neonates with
same as that for all forms of sepsis in Longer therapy is used when there is
very low birth weight.100–102 Among
the newborn and young infant.83,84 a prolonged or complicated course.
previously healthy infants in the
Blood culture, lumbar puncture for Some experts recommend a second
community, if the infant is not
culture and analysis of CSF, and lumbar puncture for CSF culture 24
critically ill and there is no evidence
markers of inflammation are to 48 hours after the start of
of meningitis, ampicillin and
discussed in detail in the AAP clinical antibiotics. Additional lumbar
ceftazidime together are
reports on management of neonates punctures and intracranial imaging
recommended as empirical therapy
with suspected or proven early-onset are advised if there is not resolution
for those 8 to 28 days of age;
bacterial sepsis. The evaluation for of CSF infection, if neurologic
ceftriaxone therapy is recommended
GBS LOD should also include urine abnormalities persist, or if focal
under these circumstances for infants
culture. If bone or joint infection is deficits develop. Osteoarticular
29 to 90 days of age. For all
suspected, additional studies can infection should be treated for 3 to
previously healthy infants in the
include radiographs, MRI, and bone 4 weeks and ventriculitis should be
community from 8 to 90 days of age,
or joint fluid culture. When treated for at least 4 weeks.
vancomycin should be added to
meningitis is diagnosed, cranial Consultation with a pediatric
recommended empirical therapy if
imaging is often useful to assess for infectious disease specialist should be
there is evidence of meningitis or
complications such as ventriculitis or considered for meningitis and for
critical illness to expand coverage,
brain abscess. Cultures should cases with site-specific infection.
including for b-lactam–resistant
include testing for antibiotic Audiology testing and ongoing
Streptococcus pneumoniae. The choice
susceptibility. audiologic monitoring, if indicated,
of empirical therapy among
should be arranged before discharge.
continuously hospitalized preterm
Empirical and Definitive Treatment infants beyond 72 hours of age is
Antibiotics initiated because of guided by multiple factors, including Multiple Births
concern for GBS EOD are the same as the presence of central venous When invasive GBS infection occurs
those for all bacterial causes of EOS catheters and local hospital in an infant who is 1 of multiple
until the results of cultures are microbiology. The empirical choice births, the birth siblings should be
available. GBS neonatal disease for such infants should include an observed carefully for signs of
isolates remain susceptible to antibiotic to which group B infection and treated empirically if
b-lactam antibiotics, although ABCs streptococci are susceptible, such as signs of illness occur. There is no
TABLE 1 Recommended Intravenous Antibiotic Treatment Regimens for Confirmed Early- and Late-Onset GBS Bacteremia and Meningitis
GA #34 wk GA .34 wk
PNA #7 d PNA .7 d PNA #7 d PNA .7 d
Bacteremia
Ampicillin 50 mg/kg every 12 h 75 mg/kg every 12 h 50 mg/kg every 8 h 50 mg/kg every 8 h
Penicillin G 50 000 U/kg every 12 h 50 000 U/kg every 8 h 50 000 U/kg every 12 h 50 000 U/kg every 8 h
Meningitis
Ampicillin 100 mg/kg every 8 h 75 mg/kg every 6 h 100 mg/kg every 8 h 75 mg/kg q 6 h
Penicillin G 150 000 U/kg every 8 h 125 000 U/kg every 6 h 150 000 U/kg every 8 h 125 U/kg every 6 h
Adapted from Table 4.2. Antibacterial Drugs for Neonates (,28 Postnatal Days of Age). In: Kimberlin DW, Brady MT, Jackson MA, Long SS, eds. Red Book: 2018 Report of the Committee on
Infectious Diseases. 31st ed. Itasca, IL: American Academy of Pediatrics; 2018:915-919. GA, gestational age; PNA, postnatal age.
Downloaded from www.aappublications.org/news by guest on July 24, 2019
10 FROM THE AMERICAN ACADEMY OF PEDIATRICS
evidence to support full antibiotic associated early infant antibiotic at-risk nonpregnant adults could
treatment courses in the absence of exposures with increased risks of potentially prevent many of these
confirmed GBS disease. atopic and allergic disorders as well issues. Preclinical and human phase I
as increases in early childhood weight and II studies have been completed
Recurrent GBS Disease gain.109–112 Several human studies revealing the safety and
Recurrent neonatal and young infant report differences in the composition immunogenicity of glycoconjugate
GBS disease can occur after of the maternal vaginal113 and infant GBS vaccines.121–123 Current ABCs
completed appropriate treatment of gut microbiome associated with the reveals that 99% of infections are
the primary infection.103,104 Authors use of IAP, with effects on both the caused by 6 GBS serotypes,
of a population-based study diversity and richness of identified suggesting that a hexavalent vaccine
conducted in Japan53 during 2011 to species.114–119 The differences could be widely effective.6
2015 found that recurrence occurred observed vary with the mode of
in 2.8% of cases of neonatal GBS delivery and duration of
breastfeeding; differences were
SUMMARY OF RECOMMENDATIONS
infection. Recurrent cases were
detected as long as 12 months after 1. The AAP supports the maternal
identified 3 to 54 days after
completion of the therapy for the first birth in 1 study.115 Changes in the policies and procedures for the
initial constitution of neonatal gut prevention of perinatal GBS
occurrence. Recurrent cases are
microbiota in response to IAP are not disease as recommended by
generally caused by the same GBS
unexpected; GBS IAP is administered the ACOG.
serotype that caused the primary
infection, and persistent mucosal with the intent of altering the content 2. For the purpose of neonatal
colonization and poor neonatal of the newborn infant’s initial management, the administration
antibody responses to the first microflora exposure at delivery to of intrapartum penicillin G,
infection likely contribute to the decrease colonization with ampicillin, or cefazolin can provide
pathogenesis of recurrent infection. a significant neonatal pathogen. adequate IAP against neonatal
Recurrent disease is not preventable Whether the secondary effects of IAP early-onset GBS disease. For
by extension of recommended on the microbiome influence short- women at high risk of anaphylaxis
antibiotic courses nor by the addition and long-term childhood health to b-lactam antibiotics,
of rifampin to eradicate mucosal outcomes is unknown and an area of clindamycin and vancomycin
colonization.105 Parents should be active investigation. should be administered as
counseled about the possibility of recommended by the ACOG and
GBS Vaccine Development
recurrent GBS disease after treatment will likely provide some protection
of both GBS EOD and LOD. Multiple gaps remain in GBS disease against GBS EOD in exposed
prevention. Neonatal EOD continues newborn infants. However, there is
to occur in the United States, currently insufficient clinical
FUTURE DIRECTIONS primarily among preterm infants, efficacy evidence to consider the
term infants born to women with administration of these antibiotics
Intrapartum Antibiotics, the cultures negative for antenatal GBS, equivalent to b-lactam antibiotics
Microbiome, and Childhood Health and infants born to mothers with for the purpose of neonatal risk
GBS IAP and the administration of reported b-lactam allergy that assessment.
intrapartum antibiotics because of precludes maximally effective IAP.
3. Risk assessment for early-onset
concern for maternal intraamniotic The incidence of GBS LOD has not
GBS disease should follow the
infection combined result in been affected by IAP. In addition,
general principles established in
approximately 30% of pregnant group B Streptococcus is a cause of
the AAP clinical reports on
women receiving antibiotics around stillbirth and of invasive infection
management of neonates with
the time of delivery. The composition among pregnant and postpartum
suspected or proven early-onset
of the gut microbiota develops and women as well as among the elderly
bacterial sepsis.83,84 These
diversifies from birth through early and those whose health is
principles include the following:
childhood, and disruption of the compromised by diabetes or
○ separate consideration of infants
microbiota during this critical malignancy.15,120 Furthermore, GBS
period may have enduring health disease is a worldwide problem, born at $35 0/7 weeks’
consequences. Perinatal antibiotic particularly among resource-limited gestation and those born at #34
administration is associated with countries where IAP is not a readily 6/7 weeks’ gestation;
abnormal host development in available preventive strategy. ○ infants born at $35 0/7 weeks’
animal models.106–108 Human Effective, multivalent vaccines gestation may be assessed for risk
epidemiological studies have administered to pregnant women and of early-onset GBS infection with
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 11
a categorical algorithm by using Susan W. Aucott, MD, FAAP Marc Fischer, MD, FAAP – Centers for Disease
multivariate models such as the Karen M. Puopolo, MD, PhD, FAAP Control and Prevention
Jay P. Goldsmith, MD, FAAP Natasha B. Halasa, MD, MPH, FAAP –
Neonatal Early-Onset Sepsis
Meredith Mowitz, MD, FAAP Pediatric Infectious Diseases Society
Calculator or with enhanced Kristi Watterberg, MD, FAAP, Immediate Past Nicole Le Saux, MD, FRCP(C) – Canadian
clinical observation; and Chairperson Paediatric Society
○ infants born at #34 6/7 weeks’ Scot B. Moore, MD, FAAP – Committee on
Practice Ambulatory Medicine
gestation are at highest risk for LIAISONS Neil S. Silverman, MD – American College of
early-onset infection from all Obstetricians and Gynecologists
Timothy Jancelewicz, MD – American
causes, including group B Jeffrey R. Starke, MD – FAAP, American
Academy of Pediatrics Section on Surgery
streptococci, and may be best Thoracic Society
Michael Narvey, MD – Canadian Pediatric
approached by using the James J. Stevermer, MD, MSPH, FAAFP –
Society
American Academy of Family Physicians
circumstances of preterm birth Russell Miller, MD – American College of
Kay M. Tomashek, MD, MPH, DTM – National
to determine management. Obstetricians and Gynecologists
Institutes of Health
RADM Wanda Barfield, MD, MPH – Centers
4. Early-onset GBS infection is for Disease Control and Prevention
diagnosed by blood or CSF culture. Erin Keels, DNP, APRN, NNP-BC – National STAFF
Common laboratory tests such as Association of Neonatal Nurses
Jennifer M. Frantz, MPH
the complete blood cell count and
C-reactive protein do not perform STAFF
well in predicting early-onset ACKNOWLEDGMENTS
Jim Couto, MA
infection, particularly among well- The American Academy of Pediatrics thanks
appearing infants at lowest Stephanie Schrag, DPhil, Epidemiology Team
Lead, Respiratory Diseases Branch, Centers
baseline risk of infection. COMMITTEE ON INFECTIOUS DISEASES,
for Disease Control and Prevention, and
5. Evaluation for late-onset GBS 2018–2019 Carol Baker, MD, McGovern Medical School,
disease should be based on clinical Yvonne A. Maldonado, MD, FAAP, University of Texas-Houston, for their
Chairperson partnership and contributions to the
signs of illness in the infant.
Theoklis E. Zaoutis, MD, MSCE, FAAP, Vice development of this clinical report.
Diagnosis is based on the isolation Chairperson
of group B streptococci from Ritu Banerjee, MD, PhD, FAAP
blood, CSF, or other normally Elizabeth D. Barnett MD, FAAP
sterile sites. Late-onset GBS James D. Campbell, MD, MS, FAAP ABBREVIATIONS
Jeffrey S. Gerber, MD, PhD, FAAP AAP: American Academy of
disease occurs among infants born
Athena P. Kourtis, MD, PhD, MPH, FAAP
to mothers who had positive GBS Ruth Lynfield, MD, FAAP
Pediatrics
screen results as well as those who Flor M. Munoz, MD, MSc, FAAP ABCs: Active Bacterial Core
had negative screen results during Dawn Nolt, MD, MPH, FAAP surveillance
pregnancy. Adequate IAP does not Ann-Christine Nyquist, MD, MSPH, FAAP ACOG: American College of
Sean T. O’Leary, MD, MPH, FAAP Obstetricians and
protect infants from late-onset
Mark H. Sawyer, MD, FAAP
GBS disease. William J. Steinbach, MD, FAAP
Gynecologists
6. Empirical antibiotic therapy for Ken Zangwill, MD, FAAP CDC: Centers for Disease Control
early-onset and late-onset GBS and Prevention
disease differs by postnatal age at CSF: cerebrospinal fluid
EX OFFICIO EOD: early-onset disease
the time of evaluation. Penicillin G
David W. Kimberlin, MD, FAAP – Red Book EOS: early-onset sepsis
is the preferred antibiotic for
Editor GBS: group B streptococcal
definitive treatment of GBS disease Henry H. Bernstein, DO, MHCM, FAAP – Red
in infants; ampicillin is an IAP: intrapartum antibiotic
Book Online Associate Editor
acceptable alternative. H. Cody Meissner, MD, FAAP – Visual Red prophylaxis
Book Associate Editor LOD: late-onset disease
MIC: minimum inhibitory
COMMITTEE ON FETUS AND NEWBORN, concentration
2018–2019 LIAISONS
NAAT: nucleic acid
James Cummings, MD, MS, FAAP, Amanda C. Cohn, MD, FAAP – Centers for amplification test
Chairperson Disease Control and Prevention
PROM: prelabor rupture of
Ivan Hand, MD, FAAP Jamie Deseda-Tous, MD – Sociedad
Ira Adams-Chapman, MD, FAAP Latinoamericana de Infectología Pediátrica membranes
Brenda Poindexter, MD, FAAP Karen M. Farizo, MD – US Food and Drug ROM: rupture of membranes
Dan L. Stewart, MD, FAAP Administration
Downloaded from www.aappublications.org/news by guest on July 24, 2019
12 FROM THE AMERICAN ACADEMY OF PEDIATRICS
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
1. Centers for Disease Control and Kimberlin DW, Brady MT, Jackson MA, 6 years in France. Acta Paediatr. 2010;
Prevention. Prevention of perinatal Long SS, eds. Red Book: 2018 99(1):47–51
group B streptococcal disease: Report of the Committee on
18. Boyer KM, Gadzala CA, Burd LI, Fisher
a public health perspective [published Infectious Diseases. 31st ed. Itasca,
DE, Paton JB, Gotoff SP. Selective
correction appears in MMWR Morb IL: American Academy of Pediatrics;
intrapartum chemoprophylaxis of
Mortal Wkly Rep. 1996;45(31):679]. 2018:762–768
neonatal group B streptococcal early-
MMWR Recomm Rep. 1996;45(RR-7):
9. Schrag SJ, Farley MM, Petit S, et al. onset disease. I. Epidemiologic
1–24
Epidemiology of invasive early-onset rationale. J Infect Dis. 1983;148(5):
2. Schrag S, Gorwitz R, Fultz-Butts K, neonatal sepsis, 2005 to 2014. 795–801
Schuchat A. Prevention of perinatal Pediatrics. 2016;138(6):e20162013
19. Baker CJ, Barrett FF. Transmission of
group B streptococcal disease.
10. Weston EJ, Pondo T, Lewis MM, et al. The group B streptococci among parturient
Revised guidelines from CDC. MMWR
burden of invasive early-onset neonatal women and their neonates. J Pediatr.
Recomm Rep. 2002;51(RR-11):1–22
sepsis in the United States, 2005-2008. 1973;83(6):919–925
3. Schrag SJ, Zell ER, Lynfield R, et al; Pediatr Infect Dis J. 2011;30(11):
Active Bacterial Core Surveillance 937–941 20. Benitz WE, Gould JB, Druzin ML. Risk
Team. A population-based comparison factors for early-onset group B
11. Baker CJ. Early onset group B streptococcal sepsis: estimation of
of strategies to prevent early-onset
streptococcal disease. J Pediatr. 1978; odds ratios by critical literature review.
group B streptococcal disease in
93(1):124–125 Pediatrics. 1999;103(6). Available at:
neonates. N Engl J Med. 2002;347(4):
233–239 12. Escobar GJ, Li DK, Armstrong MA, et al. www.pediatrics.org/cgi/content/full/
Neonatal sepsis workups in infants 103/6/e77
4. Verani JR, McGee L, Schrag SJ; Division
./=2000 grams at birth: a population- 21. Goldenberg RL, Hauth JC, Andrews WW.
of Bacterial Diseases, National Center
based study. Pediatrics. 2000;106(2 pt Intrauterine infection and preterm
for Immunization and Respiratory
1):256–263 delivery. N Engl J Med. 2000;342(20):
Diseases, Centers for Disease Control
and Prevention (CDC). Prevention of 13. Escobar GJ, Puopolo KM, Wi S, et al. 1500–1507
perinatal group B streptococcal Stratification of risk of early-onset 22. Gibbs RS, Roberts DJ. Case records of
disease--revised guidelines from CDC, sepsis in newborns $ 34 weeks’ the Massachusetts General Hospital.
2010. MMWR Recomm Rep. 2010;59(RR- gestation. Pediatrics. 2014;133(1):30–36 Case 27-2007. A 30-year-old pregnant
10):1–36 14. Kuzniewicz MW, Puopolo KM, Fischer A, woman with intrauterine fetal
5. Mukhopadhyay S, Taylor JA, Von et al. A quantitative, risk-based death. N Engl J Med. 2007;357(9):
Kohorn I, et al. Variation in sepsis approach to the management of 918–925
evaluation across a national network neonatal early-onset sepsis. JAMA 23. Nan C, Dangor Z, Cutland CL, Edwards
of nurseries. Pediatrics. 2017;139(3): Pediatr. 2017;171(4):365–371 MS, Madhi SA, Cunnington MC. Maternal
e0162845 15. Seale AC, Bianchi-Jassir F, Russell NJ, group B Streptococcus-related
6. Nanduri SA, Petit S, Smelser C, et al. et al. Estimates of the burden of group stillbirth: a systematic review. BJOG.
Epidemiology of invasive early-onset B streptococcal disease worldwide for 2015;122(11):1437–1445
and late-onset group B streptococcal pregnant women, stillbirths, and 24. Russell NJ, Seale AC, O’Driscoll M, et al;
disease in the United States, 2006 to children. Clin Infect Dis. 2017;65(suppl_ GBS Maternal Colonization Investigator
2015: multistate laboratory and 2):S200–S219 Group. Maternal colonization with
population-based surveillance. JAMA group B Streptococcus and serotype
16. Hussain SM, Luedtke GS, Baker CJ,
Pediatr. 2019;173(3):224–233 distribution worldwide: systematic
Schlievert PM, Leggiadro RJ. Invasive
7. American College of Obstetricians and group B streptococcal disease in review and meta-analyses. Clin Infect
Gynecologists. Prevention of group B children beyond early infancy. Pediatr Dis. 2017;65(suppl_2):S100–S111
streptococcal early-onset disease in Infect Dis J. 1995;14(4):278–281
25. Campbell JR, Hillier SL, Krohn MA,
newborns: ACOG Committee Opinion,
17. Guilbert J, Levy C, Cohen R, Delacourt C, Ferrieri P, Zaleznik DF, Baker CJ. Group
Number 782. Obstet Gynecol. 2019;
Renolleau S, Flamant C; Bacterial B streptococcal colonization and
134(1):e19–e40
meningitis group. Late and ultra late serotype-specific immunity in pregnant
8. American Academy of Pediatrics. onset Streptococcus B meningitis: women at delivery. Obstet Gynecol.
Group B streptococcal infections. In: clinical and bacteriological data over 2000;96(4):498–503
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 13
26. Buchan BW, Faron ML, Fuller D, Davis TE, Study Group. Multistate case-control streptococcal disease. J Infect Dis.
Mayne D, Ledeboer NA. Multicenter study of maternal risk factors for 2014;209(5):781–788
clinical evaluation of the Xpert GBS LB neonatal group B streptococcal
46. Collins A, Weitkamp JH, Wynn JL. Why
assay for detection of group B disease. Pediatr Infect Dis J. 1994;13(7):
are preterm newborns at increased
Streptococcus in prenatal screening 623–629
risk of infection? Arch Dis Child Fetal
specimens. J Clin Microbiol. 2015;53(2):
36. Schuchat A, Zywicki SS, Dinsmoor MJ, Neonatal Ed. 2018;103(4):F391–F394
443–448
et al. Risk factors and opportunities for
27. Young BC, Dodge LE, Gupta M, Rhee JS, prevention of early-onset neonatal 47. Adair CE, Kowalsky L, Quon H, et al. Risk
Hacker MR. Evaluation of a rapid, real- sepsis: a multicenter case-control factors for early-onset group B
time intrapartum group B study. Pediatrics. 2000;105(1 pt 1):21–26 streptococcal disease in neonates:
streptococcus assay. Am J Obstet a population-based case-control study.
37. Van Dyke MK, Phares CR, Lynfield R, CMAJ. 2003;169(3):198–203
Gynecol. 2011;205(4):372.e1–372.e6
et al. Evaluation of universal antenatal
28. Hansen SM, Uldbjerg N, Kilian M, screening for group B streptococcus. 48. Pintye J, Saltzman B, Wolf E, Crowell CS.
Sørensen UB. Dynamics of N Engl J Med. 2009;360(25):2626–2636 Risk factors for late-onset group B
Streptococcus agalactiae colonization streptococcal disease before and after
in women during and after pregnancy 38. Puopolo KM, Draper D, Wi S, et al. implementation of universal screening
and in their infants. J Clin Microbiol. Estimating the probability of neonatal and intrapartum antibiotic prophylaxis.
2004;42(1):83–89 early-onset infection on the basis of J Pediatric Infect Dis Soc. 2016;5(4):
maternal risk factors. Pediatrics. 2011; 431–438
29. Meyn LA, Moore DM, Hillier SL, Krohn 128(5). Available at: www.pediatrics.
MA. Association of sexual activity with org/cgi/content/full/128/5/e1155 49. Berardi A, Rossi C, Lugli L, et al; GBS
colonization and vaginal acquisition of Prevention Working Group, Emilia-
group B Streptococcus in nonpregnant 39. Zaleznik DF, Rench MA, Hillier S, et al. Romagna. Group B streptococcus late-
women. Am J Epidemiol. 2002;155(10): Invasive disease due to group B onset disease: 2003-2010. Pediatrics.
949–957 Streptococcus in pregnant women and 2013;131(2). Available at: www.
neonates from diverse population pediatrics.org/cgi/content/full/131/2/
30. Yow MD, Mason EO, Leeds LJ, Thompson groups. Clin Infect Dis. 2000;30(2): e361
PK, Clark DJ, Gardner SE. Ampicillin 276–281
prevents intrapartum transmission of 50. Lin FY, Weisman LE, Troendle J, Adams K.
group B streptococcus. JAMA. 1979; 40. Mukhopadhyay S, Dukhovny D, Mao W, Prematurity is the major risk factor for
241(12):1245–1247 Eichenwald EC, Puopolo KM. 2010 late-onset group B streptococcus
perinatal GBS prevention guideline and disease. J Infect Dis. 2003;188(2):
31. Boyer KM, Gadzala CA, Kelly PD, Gotoff SP. resource utilization. Pediatrics. 2014; 267–271
Selective intrapartum chemoprophylaxis 133(2):196–203
of neonatal group B streptococcal 51. Jordan HT, Farley MM, Craig A, et al;
early-onset disease. III. Interruption of 41. Heath PT, Balfour GF, Tighe H, Verlander Active Bacterial Core Surveillance
mother-to-infant transmission. J Infect NQ, Lamagni TL, Efstratiou A; HPA GBS (ABCs)/Emerging Infections Program
Dis. 1983;148(5):810–816 Working Group. Group B streptococcal Network, CDC. Revisiting the need for
disease in infants: a case control study. vaccine prevention of late-onset
32. de Cueto M, Sanchez MJ, Sampedro A, Arch Dis Child. 2009;94(9):674–680
Miranda JA, Herruzo AJ, Rosa-Fraile M. neonatal group B streptococcal
Timing of intrapartum ampicillin and 42. Carstensen H, Christensen KK, Grennert disease: a multistate, population-based
prevention of vertical transmission of L, Persson K, Polberger S. Early-onset analysis. Pediatr Infect Dis J. 2008;
group B streptococcus. Obstet Gynecol. neonatal group B streptococcal 27(12):1057–1064
1998;91(1):112–114 septicaemia in siblings. J Infect. 1988; 52. Bartlett AW, Smith B, George CR, et al.
17(3):201–204 Epidemiology of late and very late onset
33. Russell NJ, Seale AC, O’Sullivan C, et al.
Risk of early-onset neonatal group B 43. Persson K, Bjerre B, Elfström L, group B streptococcal disease: fifteen-
streptococcal disease with maternal Polberger S, Forsgren A. Group B year experience from two Australian
colonization worldwide: systematic streptococci at delivery: high count in tertiary pediatric facilities. Pediatr
review and meta-analyses. Clin Infect urine increases risk for neonatal Infect Dis J. 2017;36(1):20–24
Dis. 2017;65(suppl_2):S152–S159 colonization. Scand J Infect Dis. 1986; 53. Matsubara K, Hoshina K, Kondo M, et al.
18(6):525–531
34. Schuchat A, Oxtoby M, Cochi S, et al. Group B streptococcal disease in
Population-based risk factors for 44. Baker CJ, Kasper DL. Correlation of infants in the first year of life:
neonatal group B streptococcal maternal antibody deficiency with a nationwide surveillance study in
disease: results of a cohort study in susceptibility to neonatal group B Japan, 2011-2015. Infection. 2017;45(4):
metropolitan Atlanta. J Infect Dis. 1990; streptococcal infection. N Engl J Med. 449–458
162(3):672–677 1976;294(14):753–756
54. Zimmermann P, Gwee A, Curtis N. The
35. Schuchat A, Deaver-Robinson K, 45. Baker CJ, Carey VJ, Rench MA, et al. controversial role of breast milk in GBS
Plikaytis BD, Zangwill KM, Mohle-Boetani Maternal antibody at delivery protects late-onset disease. J Infect. 2017;
J, Wenger JD; The Active Surveillance neonates from early onset group B 74(suppl 1):S34–S40
Downloaded from www.aappublications.org/news by guest on July 24, 2019
14 FROM THE AMERICAN ACADEMY OF PEDIATRICS
55. Le Doare K, Kampmann B. Breast milk independent patient data. Am 75. Wear CD, Towers CV, Brown MS, Weitz B,
and Group B streptococcal infection: J Perinatol. 2016;33(5):510–517 Porter S, Wolfe L. Transplacental
vector of transmission or vehicle for 65. Barber EL, Zhao G, Buhimschi IA, Illuzzi passage of clindamycin from mother to
protection? Vaccine. 2014;32(26): JL. Duration of intrapartum prophylaxis neonate. J Perinatol. 2016;36(11):
3128–3132 and concentration of penicillin G in fetal 960–961
56. Madrid L, Seale AC, Kohli-Lynch M, et al; serum at delivery. Obstet Gynecol. 2008; 76. Fairlie T, Zell ER, Schrag S. Effectiveness
Infant GBS Disease Investigator Group. 112(2 pt 1):265–270 of intrapartum antibiotic prophylaxis
Infant group B streptococcal disease 66. Berardi A, Pietrangiolillo Z, Bacchi for prevention of early-onset group B
incidence and serotypes worldwide: Reggiani ML, et al. Are postnatal streptococcal disease. Obstet Gynecol.
systematic review and meta-analyses. ampicillin levels actually related to the 2013;121(3):570–577
Clin Infect Dis. 2017;65(suppl_2): duration of intrapartum antibiotic 77. Nanovskaya T, Patrikeeva S, Zhan Y,
S160–S172 prophylaxis prior to delivery? A Fokina V, Hankins GD, Ahmed MS.
57. Patras KA, Nizet V. Group B pharmacokinetic study in 120 neonates. Transplacental transfer of vancomycin
streptococcal maternal colonization Arch Dis Child Fetal Neonatal Ed. 2018; and telavancin. Am J Obstet Gynecol.
and neonatal disease: molecular 103(2):F152–F156 2012;207(4):331.e1–331.e6
mechanisms and preventative 67. Brown CEL, Christmas JT, Bawdon RE.
approaches. Front Pediatr. 2018;6:27 78. Laiprasert J, Klein K, Mueller BA,
Placental transfer of cefazolin and Pearlman MD. Transplacental passage
58. Jiang SM, Cieslewicz MJ, Kasper DL, piperacillin in pregnancies remote from of vancomycin in noninfected term
Wessels MR. Regulation of virulence by term complicated by Rh pregnant women. Obstet Gynecol. 2007;
a two-component system in group B isoimmunization. Am J Obstet Gynecol. 109(5):1105–1110
streptococcus. J Bacteriol. 2005;187(3): 1990;163(3):938–943
1105–1113 79. Towers CV, Weitz B. Transplacental
68. Groff SM, Fallatah W, Yang S, et al. Effect passage of vancomycin. J Matern Fetal
59. Tazi A, Bellais S, Tardieux I, Dramsi S, of maternal obesity on maternal-fetal Neonatal Med. 2018;31(8):1021–1024
Trieu-Cuot P, Poyart C. Group B transfer of preoperative cefazolin at
Streptococcus surface proteins as cesarean section. J Pediatr Pharmacol 80. Onwuchuruba CN, Towers CV, Howard
major determinants for meningeal Ther. 2017;22(3):227–232 BC, Hennessy MD, Wolfe L, Brown MS.
tropism. Curr Opin Microbiol. 2012; Transplacental passage of vancomycin
69. Fiore Mitchell T, Pearlman MD,
15(1):44–49 from mother to neonate. Am J Obstet
Chapman RL, Bhatt-Mehta V, Faix RG.
Gynecol. 2014;210(4):352.e1–352.e4
60. Klinzing DC, Ishmael N, Dunning Hotopp Maternal and transplacental
JC, et al. The two-component response pharmacokinetics of cefazolin. Obstet 81. Berardi A, Rossi C, Creti R, et al. Group B
regulator LiaR regulates cell wall stress Gynecol. 2001;98(6):1075–1079 streptococcal colonization in 160 mother-
responses, pili expression and 70. Allegaert K, van Mieghem T, Verbesselt baby pairs: a prospective cohort study.
virulence in group B Streptococcus. R, et al. Cefazolin pharmacokinetics in J Pediatr. 2013;163(4):1099–104.e1
Microbiology. 2013;159(pt 7):1521–1534 maternal plasma and amniotic fluid 82. Toyofuku M, Morozumi M, Hida M, et al.
61. Mu R, Cutting AS, Del Rosario Y, et al. during pregnancy. Am J Obstet Gynecol. Effects of intrapartum antibiotic
Identification of CiaR regulated genes 2009;200(2):170.e1–170.e7 prophylaxis on neonatal acquisition of
that promote group B streptococcal 71. Centers for Disease Control and group B streptococci. J Pediatr. 2017;
virulence and interaction with brain Prevention. Active bacterial core 190:169–173.e1
endothelial cells. PLoS One. 2016;11(4): surveillance (ABCs): bact facts 83. Puopolo KM, Benitz WE, Zaoutis TE;
e0153891 interactive. Available at: https://wwwn. Committee on Fetus and Newborn;
62. Périchon B, Szili N, du Merle L, et al. cdc.gov/BactFacts/index.html. Accessed Committee on Infectious Diseases.
Regulation of PI-2b pilus expression in February 20, 2019 Management of neonates born at $35
hypervirulent Streptococcus agalactiae 72. Knight KM, Thornburg LL, McNanley AR, 0/7 weeks’ gestation with suspected or
ST-17 BM110. PLoS One. 2017;12(1): Hardy DJ, Vicino D, Glantz JC. The effect proven early-onset bacterial sepsis.
e0169840 of intrapartum clindamycin on vaginal Pediatrics. 2018;142(6):e20182894
63. Boyer KM, Gotoff SP. Prevention of early- group B streptococcus colony counts. 84. Puopolo KM, Benitz WE, Zaoutis TE;
onset neonatal group B streptococcal J Matern Fetal Neonatal Med. 2012; Committee on Fetus and Newborn;
disease with selective intrapartum 25(6):747–749 Committee on Infectious Diseases.
chemoprophylaxis. N Engl J Med. 1986; 73. Weinstein AJ, Gibbs RS, Gallagher M. Management of neonates born at #34
314(26):1665–1669 Placental transfer of clindamycin and 6/7 weeks’ gestation with suspected or
gentamicin in term pregnancy. Am proven early-onset bacterial sepsis.
64. Turrentine MA, Colicchia LC, Hirsch E,
J Obstet Gynecol. 1976;124(7):688–691 Pediatrics. 2018;142(6):e20182896
et al. Efficiency of screening for the
recurrence of antenatal group B 74. Philipson A, Sabath LD, Charles D. 85. Committee on Obstetric Practice.
Streptococcus colonization in Transplacental passage of Committee opinion no. 712: intrapartum
a subsequent pregnancy: a systematic erythromycin and clindamycin. N Engl management of intraamniotic infection.
review and meta-analysis with J Med. 1973;288(23):1219–1221 Obstet Gynecol. 2017;130(2):e95–e101
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 15
86. Newman TB, Puopolo KM, Wi S, Draper birth weight infants: opportunities for 106. Cox LM, Yamanishi S, Sohn J, et al.
D, Escobar GJ. Interpreting complete antibiotic stewardship. Pediatr Infect Altering the intestinal microbiota
blood counts soon after birth in Dis J. 2017;36(5):477–481 during a critical developmental window
newborns at risk for sepsis. Pediatrics. has lasting metabolic consequences.
97. Puopolo KM, Mukhopadhyay S, Hansen
2010;126(5):903–909 Cell. 2014;158(4):705–721
NI, et al; NICHD Neonatal Research
87. Hornik CP, Benjamin DK, Becker KC, Network. Identification of extremely 107. Cho I, Yamanishi S, Cox L, et al.
et al. Use of the complete blood cell premature infants at low risk for early- Antibiotics in early life alter the murine
count in early-onset neonatal sepsis. onset sepsis. Pediatrics. 2017;140(5): colonic microbiome and adiposity.
Pediatr Infect Dis J. 2012;31(8):799–802 e20170925 Nature. 2012;488(7413):621–626
88. Newman TB, Draper D, Puopolo KM, Wi 98. Tibussek D, Sinclair A, Yau I, et al. Late- 108. Leclercq S, Mian FM, Stanisz AM, et al.
S, Escobar GJ. Combining immature and onset group B streptococcal meningitis Low-dose penicillin in early life induces
total neutrophil counts to predict early has cerebrovascular complications. long-term changes in murine gut
onset sepsis in term and late preterm J Pediatr. 2015;166(5):1187–1192.e1 microbiota, brain cytokines and
newborns: use of the I/T2. Pediatr Infect behavior. Nat Commun. 2017;8:15062
99. Metcalf BJ, Chochua S, Gertz RE Jr, et al;
Dis J. 2014;33(8):798–802
Active Bacterial Core surveillance team. 109. Kummeling I, Stelma FF, Dagnelie PC,
89. Benitz WE. Adjunct laboratory tests in Short-read whole genome sequencing et al. Early life exposure to antibiotics
the diagnosis of early-onset neonatal for determination of antimicrobial and the subsequent development of
sepsis. Clin Perinatol. 2010;37(2): resistance mechanisms and capsular eczema, wheeze, and allergic
421–438 serotypes of current invasive sensitization in the first 2 years of life:
90. Puopolo KM, Madoff LC, Eichenwald EC. Streptococcus agalactiae recovered in the KOALA Birth Cohort Study.
Early-onset group B streptococcal the USA. Clin Microbiol Infect. 2017; Pediatrics. 2007;119(1). Available at:
disease in the era of maternal 23(8):574.e7–574.e14 www.pediatrics.org/cgi/content/full/
screening. Pediatrics. 2005;115(5): 119/1/e225
100. Schrag SJ, Hadler JL, Arnold KE,
1240–1246 Martell-Cleary P, Reingold A, Schuchat 110. Risnes KR, Belanger K, Murk W, Bracken
91. El Helali N, Nguyen JC, Ly A, A. Risk factors for invasive, early-onset MB. Antibiotic exposure by 6 months
Giovangrandi Y, Trinquart L. Diagnostic Escherichia coli infections in the era of and asthma and allergy at 6 years:
accuracy of a rapid real-time widespread intrapartum antibiotic use. findings in a cohort of 1,401 US
polymerase chain reaction assay for Pediatrics. 2006;118(2):570–576 children. Am J Epidemiol. 2011;173(3):
universal intrapartum group B 310–318
101. Puopolo KM, Eichenwald EC. No change
streptococcus screening. Clin Infect Dis. in the incidence of ampicillin-resistant, 111. Metsälä J, Lundqvist A, Virta LJ, Kaila M,
2009;49(3):417–423 neonatal, early-onset sepsis over Gissler M, Virtanen SM. Mother’s and
92. Dhudasia MB, Mukhopadhyay S, 18 years. Pediatrics. 2010;125(5). offspring’s use of antibiotics and infant
Puopolo KM. Implementation of the Available at: www.pediatrics.org/cgi/ allergy to cow’s milk. Epidemiology.
sepsis risk calculator at an academic content/full/125/5/e1031 2013;24(2):303–309
birth hospital. Hosp Pediatr. 2018;8(5): 102. Moore MR, Schrag SJ, Schuchat A. 112. Saari A, Virta LJ, Sankilampi U, Dunkel
243–250 Effects of intrapartum antimicrobial L, Saxen H. Antibiotic exposure in
93. Berardi A, Fornaciari S, Rossi C, et al. prophylaxis for prevention of group-B- infancy and risk of being overweight in
Safety of physical examination alone for streptococcal disease on the incidence the first 24 months of life. Pediatrics.
managing well-appearing neonates $ and ecology of early-onset neonatal 2015;135(4):617–626
35 weeks’ gestation at risk for early- sepsis. Lancet Infect Dis. 2003;3(4):
113. Roesch LF, Silveira RC, Corso AL, et al.
onset sepsis. J Matern Fetal Neonatal 201–213
Diversity and composition of vaginal
Med. 2015;28(10):1123–1127 103. Green PA, Singh KV, Murray BE, Baker microbiota of pregnant women at risk
94. Joshi NS, Gupta A, Allan JM, et al. CJ. Recurrent group B streptococcal for transmitting Group B Streptococcus
Clinical monitoring of well-appearing infections in infants: clinical and treated with intrapartum penicillin.
infants born to mothers with microbiologic aspects. J Pediatr. 1994; PLoS One. 2017;12(2):e0169916
chorioamnionitis. Pediatrics. 2018; 125(6 pt 1):931–938
114. Aloisio I, Mazzola G, Corvaglia LT, et al.
141(4):e20172056 104. Moylett EH, Fernandez M, Rench MA, Influence of intrapartum antibiotic
95. Joshi NS, Gupta A, Allan JM, et al. Hickman ME, Baker CJ. A 5-year review prophylaxis against group B
Management of chorioamnionitis- of recurrent group B streptococcal Streptococcus on the early newborn
exposed infants in the newborn nursery disease: lessons from twin infants. Clin gut composition and evaluation of the
using a clinical examination-based Infect Dis. 2000;30(2):282–287 anti-Streptococcus activity of
approach. Hosp Pediatr. 2019;9(4): Bifidobacterium strains. Appl Microbiol
105. Fernandez M, Rench MA, Albanyan EA,
227–233 Biotechnol. 2014;98(13):6051–6060
Edwards MS, Baker CJ. Failure of
96. Mukhopadhyay S, Puopolo KM. Clinical rifampin to eradicate group B 115. Azad MB, Konya T, Persaud RR, et al;
and microbiologic characteristics of streptococcal colonization in infants. CHILD Study Investigators. Impact of
early-onset sepsis among very low Pediatr Infect Dis J. 2001;20(4):371–376 maternal intrapartum antibiotics,
Downloaded from www.aappublications.org/news by guest on July 24, 2019
16 FROM THE AMERICAN ACADEMY OF PEDIATRICS
method of birth and breastfeeding on prophylaxis upon the intestinal B streptococcus vaccine in healthy
gut microbiota during the first year of microbiota and the prevalence of women and their infants: a randomised
life: a prospective cohort study. BJOG. antibiotic resistance genes in vaginally phase 1b/2 trial. Lancet Infect Dis. 2016;
2016;123(6):983–993 delivered full-term neonates. 16(8):923–934
116. Corvaglia L, Tonti G, Martini S, et al. Microbiome. 2017;5(1):93
122. Hillier SL, Ferrieri P, Edwards MS, et al.
Influence of intrapartum antibiotic 119. Pärnänen K, Karkman A, Hultman J, A phase 2, randomized, control trial of
prophylaxis for group B streptococcus et al. Maternal gut and breast milk group B streptococcus (GBS) type III
on gut microbiota in the first month of microbiota affect infant gut antibiotic capsular polysaccharide-tetanus toxoid
life. J Pediatr Gastroenterol Nutr. 2016; resistome and mobile genetic elements. (GBS III-TT) vaccine to prevent vaginal
62(2):304–308 Nat Commun. 2018;9(1):3891 colonization with GBS III. Clin Infect Dis.
117. Stearns JC, Simioni J, Gunn E, et al. 120. Edwards MS, Baker CJ. Group B 2019;68(12):2079–2086
Intrapartum antibiotics for GBS streptococcal infections in elderly 123. Dzanibe S, Madhi SA. Systematic review
prophylaxis alter colonization patterns adults. Clin Infect Dis. 2005;41(6): of the clinical development of group B
in the early infant gut microbiome of low 839–847 streptococcus serotype-specific
risk infants. Sci Rep. 2017;7(1):16527 121. Madhi SA, Cutland CL, Jose L, et al. capsular polysaccharide-based
118. Nogacka A, Salazar N, Suárez M, et al. Safety and immunogenicity of an vaccines. Expert Rev Vaccines. 2018;
Impact of intrapartum antimicrobial investigational maternal trivalent group 17(7):635–651
Downloaded from www.aappublications.org/news by guest on July 24, 2019
PEDIATRICS Volume 144, number 2, August 2019 17
Management of Infants at Risk for Group B Streptococcal Disease
Karen M. Puopolo, Ruth Lynfield, James J. Cummings, COMMITTEE ON FETUS
AND NEWBORN and COMMITTEE ON INFECTIOUS DISEASES
Pediatrics originally published online July 8, 2019;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/early/2019/07/04/peds.2
019-1881
References This article cites 121 articles, 28 of which you can access for free at:
http://pediatrics.aappublications.org/content/early/2019/07/04/peds.2
019-1881#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Fetus/Newborn Infant
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
sub
Infectious Disease
http://www.aappublications.org/cgi/collection/infectious_diseases_su
b
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news by guest on July 24, 2019
Management of Infants at Risk for Group B Streptococcal Disease
Karen M. Puopolo, Ruth Lynfield, James J. Cummings, COMMITTEE ON FETUS
AND NEWBORN and COMMITTEE ON INFECTIOUS DISEASES
Pediatrics originally published online July 8, 2019;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/early/2019/07/04/peds.2019-1881
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,
60007. Copyright © 2019 by the American Academy of Pediatrics. All rights reserved. Print
ISSN: 1073-0397.
Downloaded from www.aappublications.org/news by guest on July 24, 2019
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CE195 Case StudyDocument7 pagesCE195 Case StudyRold BaldsNo ratings yet
- Pestel Grameen BankDocument11 pagesPestel Grameen BankS.M.HILAL50% (2)
- Western Home Elevator Design Guide 2011 PDFDocument21 pagesWestern Home Elevator Design Guide 2011 PDFTuấn NamNo ratings yet
- Essc-Pwg Report Agusan Marsh Development Alliance Agusan Del Sur1Document9 pagesEssc-Pwg Report Agusan Marsh Development Alliance Agusan Del Sur1Princess VistalNo ratings yet
- Catalog BB Type HDocument2 pagesCatalog BB Type HdioalfanandaNo ratings yet
- Mode D'emploi Behringer Xenyx X1832USB (Français - 21 Des Pages)Document2 pagesMode D'emploi Behringer Xenyx X1832USB (Français - 21 Des Pages)Badang EloiNo ratings yet
- Auto Loan: Application FormDocument10 pagesAuto Loan: Application Formabhijit majarkhedeNo ratings yet
- Anexo 1. PararrayosDocument24 pagesAnexo 1. PararrayosJHONATAN ALEXANDER YANEZ CHANCUSIGNo ratings yet
- 1-Mole & RedoxDocument3 pages1-Mole & RedoxArnab DasNo ratings yet
- Mental Health PracticeDocument3 pagesMental Health Practicerose angelaNo ratings yet
- S1062359022700030 PDFDocument7 pagesS1062359022700030 PDFVengateshwaran TDNo ratings yet
- Carbon and Its Compound Important QuestionsDocument4 pagesCarbon and Its Compound Important QuestionsAnuradha KushwahaNo ratings yet
- Set 7 QnaDocument13 pagesSet 7 QnaRebornNgNo ratings yet
- Color by Number: Biomolecules Edition: Name: - PeriodDocument5 pagesColor by Number: Biomolecules Edition: Name: - PeriodCecilia Enriquez-MenesesNo ratings yet
- Timothy Johnson DocumentDocument1 pageTimothy Johnson Document13WMAZNo ratings yet
- Spe 23930 MsDocument8 pagesSpe 23930 MsIskander KasimovNo ratings yet
- Mobilfluid 426Document2 pagesMobilfluid 426tribolasNo ratings yet
- Development of Adolescent Problem BehaviorDocument11 pagesDevelopment of Adolescent Problem BehaviorVisvendra SinghNo ratings yet
- Biography: Ruined by Her 35m Jackpot: Britain's Biggest Lottery WinnerDocument9 pagesBiography: Ruined by Her 35m Jackpot: Britain's Biggest Lottery WinnerBalbina Alicja PędziwiatrNo ratings yet
- T4 PRO TH4110U2005 Guia InstalacionDocument36 pagesT4 PRO TH4110U2005 Guia Instalacionhugo renzo chavez bernuyNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationJulliza Joy PandiNo ratings yet
- 1 Mechanical Behavior of MaterialsDocument7 pages1 Mechanical Behavior of MaterialsMohammed Rashik B CNo ratings yet
- Blossoms of The Savannah SummaryDocument34 pagesBlossoms of The Savannah SummaryMAGOMU DAN DAVIDNo ratings yet
- Semiconductor PhysicsDocument54 pagesSemiconductor PhysicsGod KillerNo ratings yet
- Project Proposal ExampleDocument8 pagesProject Proposal ExampleplayerNo ratings yet
- Primary Water SystemDocument15 pagesPrimary Water SystemSantoshkumar GuptaNo ratings yet
- Datasheet of ACS730Document25 pagesDatasheet of ACS730Nguyên NghĩaNo ratings yet
- Safety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingDocument10 pagesSafety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingJake VergaraNo ratings yet
- Air Pressure Science Form 2 Chapter 6Document18 pagesAir Pressure Science Form 2 Chapter 6nwahidawomar100% (3)
- Full Catalogue 2008Document58 pagesFull Catalogue 2008Anonymous 1aHRPIIFfINo ratings yet