Professional Documents
Culture Documents
UST Department of Pediatrics Pediatrics 2-Module 1 Gastroenterology-Hematology-Cardiology Module Student's Guide On Bleeding
Uploaded by
Jolaine ValloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
UST Department of Pediatrics Pediatrics 2-Module 1 Gastroenterology-Hematology-Cardiology Module Student's Guide On Bleeding
Uploaded by
Jolaine ValloCopyright:
Available Formats
UST Department of Pediatrics
Pediatrics 2-Module 1
Gastroenterology-Hematology-Cardiology module
Student’s guide on bleeding
#commonyetuncommon
Anna, an 11-year old female, Filipino, Roman Catholic from Sampaloc Manila was brought to the
Emergency Room due to profuse nosebleeding.
History of the Present Illness:
Two days prior to consult, Anna developed cough and colds. Few hours prior to consult, Anna
picked her nose removing the nasal discharge that dried up (booger). She pinched her nose and
put cold compress on her forehead. Bleeding was quite profuse. An hour later, she vomited
previously ingested food admixed with blood. She panicked and turned pale. However, she
remained conscious. She was immediately brought to UST Hospital Emergency Department for
consult.
PE: awake, anxious, ambulatory
BP= 100/60, CR= 110/min, RR=24/min, T= 37.0oC, Wt= 33 kg. Lt = 135 cm
Skin: with greenish discoloraYon on right thigh measuring 3 cm in widest diameter
Pink palpebral conjuncYvae, anicteric sclerae, intact tympanic membrane, (+) blood clot in
right nostril, with pale boggy turbinates in the right nostril, pinkish buccal mucosa, Grade
1 slightly hyperemic tonsils without exudates,
No enlarged cervical lymph nodes
Symmetrical chest expansion, no retracYons, resonant, clear breath sounds
Adynamic precordium, apex beat at 5th LICS MCL, normal heart sounds, no murmurs
Abdomen flat, bowel sounds 12 click/minute, tympaniYc on all quadrants, liver span 6.5 cm,
Traube’s space not obliterated, soa, non-tender
ExtremiYes; no gross deformiYes, no edema, pulses full and equal, CRT < 2 seconds
GUIDE QUESTIONS:
1. What historical data will you gather from the informant?
a. History of mucocutaneous bleeding or deep muscle and joint bleeding
b. Underlying medical condiYons that can cause hemostaYc derangement like liver disease,
malabsorpYon syndrome, Vitamin K deficiency, etc.
c. Intake of drugs like aspirin, NSADS, anYbioYcs, anYconvulsants
d. Family history of the same symptoms especially among the male relaYves
2. What are the salient features of the case?
3. Discuss the importance and clinical implicaYon of your physical examinaYon findings? How
will you correlate these physical findings with the possible cause/s of bleeding in this paYent?
4. What clinical condiYon/s would you consider given the above informaYon?
5. What laboratory examinaYons will you request for? Give the principles of each. Correlate the
expected results with the clinical condiYon of this paYent.
6. Interpret the results
7. What laboratory tests should be further requested if a primary bleeding disorder is highly
suspected?
9. How would you manage this paYent?
Please refer to Nelson’s textbook of Pediatrics 21th ed. Chapter 504, pp2589-2618
You might also like
- Vasculitis Syndromes: Kawasaki Disease, Henoch-Schonlein Purpura, and Localized SclerodermaDocument54 pagesVasculitis Syndromes: Kawasaki Disease, Henoch-Schonlein Purpura, and Localized SclerodermaMiguel M. Melchor RodríguezNo ratings yet
- Data Management 'Birth Certificate'Document22 pagesData Management 'Birth Certificate'Jolaine Vallo100% (1)
- Advocacy Proposal - Group 3-3Document6 pagesAdvocacy Proposal - Group 3-3Jolaine ValloNo ratings yet
- Nbme 1 Block 1-4Document75 pagesNbme 1 Block 1-4Eimad Atif100% (1)
- Mora Solvendi (Delay of The Debtor)Document11 pagesMora Solvendi (Delay of The Debtor)John Paul100% (1)
- Data Management MCCODDocument48 pagesData Management MCCODJolaine ValloNo ratings yet
- Pedia 1Document8 pagesPedia 1Jani MisterioNo ratings yet
- Nbme 1Document77 pagesNbme 1Rezo BagashviliNo ratings yet
- Mock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsFrom EverandMock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsNo ratings yet
- NBME 1 RatioDocument87 pagesNBME 1 RatioBugs Caslib100% (1)
- Sept Recall PlabDocument19 pagesSept Recall PlabDr-Jahanzaib GondalNo ratings yet
- MSc Thesis on VAW in PhilippinesDocument100 pagesMSc Thesis on VAW in Philippineselma cutamoraNo ratings yet
- 'Batangas Medical Center Case Report by PGI Carlos H. AcuñaDocument7 pages'Batangas Medical Center Case Report by PGI Carlos H. AcuñaCarlos H. AcuñaNo ratings yet
- Liver Abscess Risk FactorsDocument7 pagesLiver Abscess Risk FactorsJoan junioNo ratings yet
- Form 1Document108 pagesForm 1Asim MohamedNo ratings yet
- Acute Respiratory Distress SyndromeDocument14 pagesAcute Respiratory Distress SyndromeAila BarbaNo ratings yet
- CPC 1 For PrintingDocument3 pagesCPC 1 For Printingapi-257172337100% (2)
- NBME 10 Unsolved QuestionsDocument88 pagesNBME 10 Unsolved QuestionsMisbah Kaleem100% (3)
- Sample POMRDocument4 pagesSample POMRJeffrey RamosNo ratings yet
- UST FMS Department of Pediatrics Pediatrics 2, Module 1 AY 2020-2021Document1 pageUST FMS Department of Pediatrics Pediatrics 2, Module 1 AY 2020-2021Jolaine ValloNo ratings yet
- CPC-Patho Version 6Document20 pagesCPC-Patho Version 6Bea SamonteNo ratings yet
- Case Management NICU July 2020 Sam WibowoDocument6 pagesCase Management NICU July 2020 Sam WibowoSamuel WibowoNo ratings yet
- Urinary Tract Infection Presenting With Nonspecific Complaints and Normal Urinalysis in 84-Year-Old WomanDocument3 pagesUrinary Tract Infection Presenting With Nonspecific Complaints and Normal Urinalysis in 84-Year-Old WomanAmeldaNo ratings yet
- TBL PaedsDocument10 pagesTBL PaedsHo Yong WaiNo ratings yet
- 12b Clinical Update Example 2018Document9 pages12b Clinical Update Example 2018Ana BienneNo ratings yet
- Primary SurveyDocument13 pagesPrimary SurveyNurul FadliNo ratings yet
- ASD Internship ReportingDocument14 pagesASD Internship ReportingPernel Jose Alam MicuboNo ratings yet
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- PCC CaseDocument9 pagesPCC CaseKaila AbeledaNo ratings yet
- Case 5: Tutor GuideDocument18 pagesCase 5: Tutor GuidelubnaNo ratings yet
- Pediatric Sepsis from Occult Dental AbscessDocument5 pagesPediatric Sepsis from Occult Dental Abscessdelfi simatupangNo ratings yet
- CASE PRESENTATION IMPROVES NURSING SKILLSDocument7 pagesCASE PRESENTATION IMPROVES NURSING SKILLSAnjali NaudiyalNo ratings yet
- E92t15 2015EDocument24 pagesE92t15 2015EDr-Mohammad AlfawazNo ratings yet
- NCMB312 - : Bachelor of Science in Nursing: Communicable Disease NursingDocument7 pagesNCMB312 - : Bachelor of Science in Nursing: Communicable Disease NursingMichelle Gliselle Guinto MallareNo ratings yet
- ROSIMO - AUG 2021 NB VomitingDocument5 pagesROSIMO - AUG 2021 NB VomitingcarlosNo ratings yet
- Sample Medical ReportsDocument6 pagesSample Medical ReportsMayNo ratings yet
- Major Case 3Document3 pagesMajor Case 3Christine Evan HoNo ratings yet
- Partial of PathophysiologyDocument56 pagesPartial of Pathophysiologytoolsdesk1No ratings yet
- NIICU Clinical Database #1Document10 pagesNIICU Clinical Database #1angela0289No ratings yet
- Case 7-2021: A 19-Year-Old Man With Shock, Multiple Organ Failure, and RashDocument11 pagesCase 7-2021: A 19-Year-Old Man With Shock, Multiple Organ Failure, and RashBruno ConteNo ratings yet
- Acute Cholangitis: Our Lady of Fatima UniversityDocument23 pagesAcute Cholangitis: Our Lady of Fatima UniversityMaria Paula Bungay100% (1)
- UntitledDocument5 pagesUntitledVincent ChristiantoNo ratings yet
- PP CaseDocument48 pagesPP CaseDany PrabowoNo ratings yet
- B2 FLORES, NIÑA - Paper Case 3Document10 pagesB2 FLORES, NIÑA - Paper Case 3Niña Therese FloresNo ratings yet
- Sample POMRDocument4 pagesSample POMRJeffrey RamosNo ratings yet
- 1) An Infant With Vomiting, Lethargy, Hypoglycemia and No Ketones in Urine Should Be Evaluated For Which Metabolic Defect?Document22 pages1) An Infant With Vomiting, Lethargy, Hypoglycemia and No Ketones in Urine Should Be Evaluated For Which Metabolic Defect?arti kandekarNo ratings yet
- CC 10 NOv 2017 ITPDocument32 pagesCC 10 NOv 2017 ITPLilik NatasubrataNo ratings yet
- M.D Pediatrics PH.D Pediatric Special Need and Nutrition Consultant Mansoura National Hospital Insurance H Fever H and Egyptian Liver HDocument49 pagesM.D Pediatrics PH.D Pediatric Special Need and Nutrition Consultant Mansoura National Hospital Insurance H Fever H and Egyptian Liver HMona MostafaNo ratings yet
- Boy presents with pink urine after boxing matchDocument27 pagesBoy presents with pink urine after boxing matchMateen ShukriNo ratings yet
- Melbourne 14 May 2005: Case 1: Rotator Cuff InjuryDocument9 pagesMelbourne 14 May 2005: Case 1: Rotator Cuff InjuryZweNo ratings yet
- Fatal Toxic Shock Syndrome From An Intrauterine DeviceDocument3 pagesFatal Toxic Shock Syndrome From An Intrauterine DeviceSiti Ro'AinunNo ratings yet
- 36 THDocument2 pages36 THPeter Francis RaguindinNo ratings yet
- 15yo With Lethargy and FeverDocument7 pages15yo With Lethargy and FeverdakewtwontonNo ratings yet
- Pediatric Round PneumoniaDocument4 pagesPediatric Round PneumoniaSalwa Zahra TsamaraNo ratings yet
- Крок-2 - студ - 18 - англDocument8 pagesКрок-2 - студ - 18 - англAimeeNo ratings yet
- Acute Pancreatitis Case PresDocument29 pagesAcute Pancreatitis Case Preskristine keen buanNo ratings yet
- Nej M CPC 1900142Document11 pagesNej M CPC 1900142arthur andreNo ratings yet
- Case Report SamplesDocument3 pagesCase Report SampleszQuang HuyNo ratings yet
- A Pain in The NeckDocument6 pagesA Pain in The NeckBudi IstriawanNo ratings yet
- San Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityDocument5 pagesSan Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityNiña AmatNo ratings yet
- Krok2 - Medicine - 2016Document25 pagesKrok2 - Medicine - 2016ashighaNo ratings yet
- (GYN) 05 Pelvic PainDocument5 pages(GYN) 05 Pelvic PainJolaine ValloNo ratings yet
- Pathoma RuntimesDocument6 pagesPathoma RuntimesaloverofdanceNo ratings yet
- February 2024 NewsletterDocument1 pageFebruary 2024 NewsletterJolaine ValloNo ratings yet
- PhysicianDocument204 pagesPhysicianTrisNo ratings yet
- (ANES) Fri Asynchronous Discussion - Basic Principles of Palliative Care and End of Life Care (Group 3) 10-23-2020Document12 pages(ANES) Fri Asynchronous Discussion - Basic Principles of Palliative Care and End of Life Care (Group 3) 10-23-2020Jolaine ValloNo ratings yet
- Structure-Function Correlation of Juxtapapillary Choroidal Thickness With Visual Field Analysis of Patients Suspected With GlaucomaDocument9 pagesStructure-Function Correlation of Juxtapapillary Choroidal Thickness With Visual Field Analysis of Patients Suspected With GlaucomaJolaine ValloNo ratings yet
- Effects of Music As An Adjunctive Therapy On Severity of Symptoms in Patients With Obsessive-Compulsive Disorder: Randomized Controlled TrialDocument15 pagesEffects of Music As An Adjunctive Therapy On Severity of Symptoms in Patients With Obsessive-Compulsive Disorder: Randomized Controlled TrialJolaine ValloNo ratings yet
- Effect of Internet-Based Vs Face-to-Face Cognitive Behavioral Therapy For Adults With Obsessive-Compulsive Disorder A Randomized Clinical TrialDocument15 pagesEffect of Internet-Based Vs Face-to-Face Cognitive Behavioral Therapy For Adults With Obsessive-Compulsive Disorder A Randomized Clinical TrialJolaine ValloNo ratings yet
- (ANES) Fri Asynchronous - Discussion - Principles of Palliative Care and End of Life CareDocument8 pages(ANES) Fri Asynchronous - Discussion - Principles of Palliative Care and End of Life CareJolaine ValloNo ratings yet
- CL Psychiatry Case Vignettes, 2022: July 1Document2 pagesCL Psychiatry Case Vignettes, 2022: July 1Jolaine ValloNo ratings yet
- Student Guide Clerkship Revised AY2021-2022 Sept - OctDocument12 pagesStudent Guide Clerkship Revised AY2021-2022 Sept - OctJolaine ValloNo ratings yet
- Preoperative Evaluation and PreparationDocument7 pagesPreoperative Evaluation and PreparationJolaine ValloNo ratings yet
- (DERMA) 03 TineasDocument9 pages(DERMA) 03 TineasJolaine ValloNo ratings yet
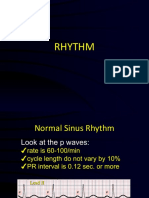
- RhythmsDocument59 pagesRhythmsJolaine ValloNo ratings yet
- Derma Quiz 5 NotesDocument6 pagesDerma Quiz 5 NotesJolaine ValloNo ratings yet
- Hema Pretests CompiledDocument6 pagesHema Pretests CompiledJolaine ValloNo ratings yet
- (DERMA) 06 Asymptomatic Skin Colored PapulesDocument12 pages(DERMA) 06 Asymptomatic Skin Colored PapulesJolaine ValloNo ratings yet
- Pgi To Do List: As of October 22, 2020 - Please Do Steps 1-3:)Document2 pagesPgi To Do List: As of October 22, 2020 - Please Do Steps 1-3:)Jolaine ValloNo ratings yet
- Med-Rheuma-Patient Write Up - Valeriano and ValloDocument10 pagesMed-Rheuma-Patient Write Up - Valeriano and ValloJolaine ValloNo ratings yet
- (DERMA) 01 Introduction To Dermatology (History and PE)Document8 pages(DERMA) 01 Introduction To Dermatology (History and PE)Jolaine ValloNo ratings yet
- Onco Pretests CompiledDocument6 pagesOnco Pretests CompiledJolaine ValloNo ratings yet
- 12 Clin Path Exocrine and Endocrine Functions of The PancreasDocument13 pages12 Clin Path Exocrine and Endocrine Functions of The PancreasJolaine ValloNo ratings yet
- 01 CLIN PTH S01 T01 Red Blood Cell DisordersDocument8 pages01 CLIN PTH S01 T01 Red Blood Cell DisordersJolaine ValloNo ratings yet
- Gi Pretests CompiledDocument7 pagesGi Pretests CompiledJolaine ValloNo ratings yet
- Rheuma Prestests CompiledDocument13 pagesRheuma Prestests CompiledJolaine ValloNo ratings yet
- D2 Grp1 CLIN PATH Case Discussion 1Document11 pagesD2 Grp1 CLIN PATH Case Discussion 1Jolaine ValloNo ratings yet
- 03 C2022 ClinPath 1.03 Hemostasis and ThrombosisDocument7 pages03 C2022 ClinPath 1.03 Hemostasis and ThrombosisJolaine ValloNo ratings yet
- Emotion-WPS OfficeDocument2 pagesEmotion-WPS OfficemikaNo ratings yet
- What Is MotivationDocument6 pagesWhat Is MotivationJohn Paul De GuzmanNo ratings yet
- Edited General English Question Paper Part 1Document12 pagesEdited General English Question Paper Part 1Utkarsh R MishraNo ratings yet
- Processing, Handling and Storage of Agricultural Product 2Document6 pagesProcessing, Handling and Storage of Agricultural Product 2LittleagleNo ratings yet
- Israel Film FundDocument1 pageIsrael Film FundgodardsfanNo ratings yet
- OUM Human Anatomy Final Exam QuestionsDocument5 pagesOUM Human Anatomy Final Exam QuestionsAnandNo ratings yet
- Test Bank For American Pageant Volume 1 16th EditionDocument36 pagesTest Bank For American Pageant Volume 1 16th Editionzoonwinkfoxyj8100% (48)
- IN SUNNY SPAIN, 1882-85: "My Country, My Love, My People, I Leave You Now, You Disappear, I Lose Sight of You"Document4 pagesIN SUNNY SPAIN, 1882-85: "My Country, My Love, My People, I Leave You Now, You Disappear, I Lose Sight of You"Mary Claire ComalaNo ratings yet
- NASA: 181330main Jun29colorDocument8 pagesNASA: 181330main Jun29colorNASAdocumentsNo ratings yet
- Coleção Bernoulli Ensino Médio 2020 - 100% BNCC by Bernoulli Sistema de Ensino - IssuuDocument1 pageColeção Bernoulli Ensino Médio 2020 - 100% BNCC by Bernoulli Sistema de Ensino - IssuuVitor OliveiraNo ratings yet
- Obessive Compulsive Disorder (OCD)Document10 pagesObessive Compulsive Disorder (OCD)marketingmoneyindiaNo ratings yet
- Villariba - Document Analysis - Jose RizalDocument2 pagesVillariba - Document Analysis - Jose RizalkrishaNo ratings yet
- Sec 4 RA 6713 & Sec 3 RA 3019 OutlineDocument4 pagesSec 4 RA 6713 & Sec 3 RA 3019 OutlineAivan Charles TorresNo ratings yet
- Surveying 2 Practical 3Document15 pagesSurveying 2 Practical 3Huzefa AliNo ratings yet
- Dell in India Targeting SMB Markets - The Differentiation Strategy PDFDocument16 pagesDell in India Targeting SMB Markets - The Differentiation Strategy PDFJatinNo ratings yet
- Student (Mechanical Engineering), JECRC FOUNDATION, Jaipur (2) Assistant Professor, Department of Mechanical Engineering, JECRC FOUNDATION, JaipurDocument7 pagesStudent (Mechanical Engineering), JECRC FOUNDATION, Jaipur (2) Assistant Professor, Department of Mechanical Engineering, JECRC FOUNDATION, JaipurAkash yadavNo ratings yet
- Global Internship for Language TeachersDocument5 pagesGlobal Internship for Language TeachersCarlos ChamorroNo ratings yet
- ACCT250-Auditing Course OutlineDocument7 pagesACCT250-Auditing Course OutlineammadNo ratings yet
- Petroleum Research: Khalil Shahbazi, Amir Hossein Zarei, Alireza Shahbazi, Abbas Ayatizadeh TanhaDocument15 pagesPetroleum Research: Khalil Shahbazi, Amir Hossein Zarei, Alireza Shahbazi, Abbas Ayatizadeh TanhaLibya TripoliNo ratings yet
- Row and Cluster Housing Building Codes and Bye LawsDocument1 pageRow and Cluster Housing Building Codes and Bye Lawssadhana illaNo ratings yet
- Emerson Field Tools Quick Start GuideDocument48 pagesEmerson Field Tools Quick Start Guidepks_2410No ratings yet
- Organization Structure in SAP Plant Maintenance: CommentsDocument3 pagesOrganization Structure in SAP Plant Maintenance: CommentsMarco Antônio Claret TeixeiraNo ratings yet
- Macroeconomics QuestionnaireDocument5 pagesMacroeconomics Questionnairevikrant vardhanNo ratings yet
- USD - DPF Cleaning Machine - POSEYDON1000 - PolDocument8 pagesUSD - DPF Cleaning Machine - POSEYDON1000 - PolAbaidi RabieNo ratings yet
- Target products to meet 20% demandDocument12 pagesTarget products to meet 20% demandAlma Dela PeñaNo ratings yet
- CartridgeDocument26 pagesCartridgeMnavya SaiNo ratings yet
- L.G.B.T. Fiction: Book ReviewDocument4 pagesL.G.B.T. Fiction: Book ReviewDejana KosticNo ratings yet
- The Oz DietDocument5 pagesThe Oz Dietkaren_wilkesNo ratings yet