Professional Documents
Culture Documents
NCP Pedro Flores Day 1
NCP Pedro Flores Day 1
Uploaded by
vanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Pedro Flores Day 1
NCP Pedro Flores Day 1
Uploaded by
vanCopyright:
Available Formats
Republic of the Philippines
Cebu Normal University
Osmeña Blvd. Cebu City, 6000 Philippines
College of Nursing
Center of Excellence (COE) | Level IV Re-Accredited (AACCUP)
Telephone No.: (032) 254 4837
Email: cn@cnu.edu.ph/secretary@cnunursing.org
Website: www.cnu.edu.ph
Theory-based (Betty Neuman)
NURSING CARE PLAN
Assessment 3 points Goals 2 points Interventions 4 points Bibliography
Diagnosis 3 points Theoretical Basis 2 points Evaluation 1 point 15 points
Name of Student: Lopez, Fritzie Vanbelle U,._______________
Client’s Initials:__P.F._____________________________________ Stressor Classification: (Please check)
Age:__74__Gender: _M___Civil Status:_Married_Religion:_N/A_ __/___ Physiological (body structure and functions)
Allergies: __none___________________________________________ ______ Psychological (mental processes and emotion)
Diet:__DAT________________________________________________ ______ Socio-cultural (relationships, social expectations)
Date of Admission:___November 8, 2020___________________ ______ Spiritual (influence of spiritual beliefs)
Diagnosis/Impression:__Chronic Bronchitis____________________ ______ Developmental (developmental processes over the lifespan)
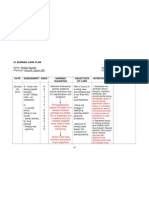
NURSING DIAGNOSIS NURSING GOALS NURSING OUTCOME
Assessment Diagnosis Mutual Planning Interventions Actual Evaluation
(Goal attainable within the shift) (with Rationale & Source)
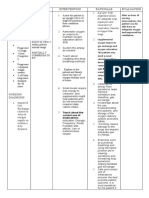
Subjective: SHORT TERM GOAL PRIMARY INTERVENTIONS Nursing Goals were
“Maglisod kog ginhawa Impaired gas exchange related After 8 hours, the patient will Promotive: almost met;
mam”, as verbalized by the to obstruction of airways as be able to: I: Assess and record respiratory rate, depth. Note the use
of accessory muscles, pursed-lip breathing, inability to
patient. evidenced by dyspnea, maintain optimal gas patient’s RR
speak or converse.
wheezing, restlessness, exchange as evidenced R: Useful in evaluating the degree of respiratory distress
reduced, but only to
As per wife, patient decreased oxygen saturation, by usual mental status, or chronicity of the disease process. 26cpm (still not
experiences shortness of and increased PCO2 unlabored respirations S: [ CITATION Mat195 \l 13321 ] within the desired
breath whenever he walks at 12-20 per minute, normal range); O2
more than 10 feet and oximetry results within I: Assess and routinely monitor skin and mucous sat raised to 95%;
membrane color. SOB still present,
usually has cough that gets normal range, blood
R: Cyanosis may be peripheral (noted in nail beds) or
worse in the morning with gases within normal central (noted around lips/or earlobes). Duskiness and
and patient agrees to
a gray colored sputum. range, and baseline HR central cyanosis indicate advanced hypoxemia.
History of smoking 30 Theoretical basis: for patient. S: [ CITATION Mat195 \l 13321 ]
Cebu Normal University Document
SDF-CON-NF-7002-034-00
sticks of cigarettes/day Gas is exchanged between the maintain clear lung
alveoli and the pulmonary I: Monitor changes in the level of consciousness and
fields and remain free
mental status.
capillaries via diffusion. of signs of respiratory R: Restlessness, agitation, and anxiety are common
Objective: Diffusion of oxygen and distress. manifestations of hypoxia. Worsening ABGs accompanied
dyspnea carbon dioxide occurs verbalize by confusion/ somnolence are indicative of cerebral
wheezing passively, according to their understanding of dysfunction due to hypoxemia.
concentration differences S: [ CITATION Mat195 \l 13321 ]
restlessness oxygen and other
coughing across the alveolar-capillary therapeutic I: Monitor oxygen saturation continuously, using pulse
nail clubbing barrier. These concentration interventions. oximeter.
ABG values: differences must be R: Pulse oximetry is a useful tool to detect changes in
pH = 7.236 maintained by ventilation oxygenation. An oxygen saturation of <90% (normal: 95%
PO2 = 4.7 (airflow) of the alveoli and LONG TERM GOAL to 100%) or a partial pressure of oxygen of <80 (normal:
perfusion (blood flow) of the 80 to 100) indicates significant oxygenation problems.
PCO2 = 8 After 3-5 days, the patient
pulmonary capillaries. S: [ CITATION Doe16 \l 13321 ]
vital signs: will:
T = 37.1 ͦC
[ CITATION Gil17 \l 13321 ] demonstrate improved I: Monitor arterial blood gasses values as ordered.
PR = 85 bpm ventilation and R: As the patient’s condition progresses, Pa02 usually
Chronic bronchitis is the adequate oxygenation decreases. For patient’s with chronic carbon dioxide
RR = 31 cpm
widespread inflammation of of tissues by ABGs retention may have chronically compensated respiratory
BP = 130/80 mmHg acidosis with a low normal pH and a PaCo2 higher than 50
airways with narrowing or within patient’s normal
02 Sat = 94% mm Hg.
blocking of airways and range and be free of
PS = 1/10 (upon S: [ CITATION Doe16 \l 13321 ]
increased production of symptoms of
inhalation)
mucoid sputum with marked respiratory distress. Preventive:
cyanosis. participate in treatment I: Assess the patient’s ability to cough out secretions. Take
regimen within the note of the quantity, color, and consistency of the sputum.
The quantity and viscosity of level of R: Retained secretions weaken gas exchange.
sputum can obstruct the S: [ CITATION Gil17 \l 13321 ]
ability/situation.
airway and impair pulmonary
I: Evaluate the level of activity tolerance. Limit patient’s
ventilation and gas exchange. activity or encourage bed or chair rest during the acute
[ CITATION Mat195 \l 13321 ] phase.
R: During severe, acute or refractory respiratory distress,
the patient may be totally unable to perform basic self-care
activities because of hypoxemia and dyspnea. Rest
interspersed with care activities remains an important part
of the treatment regimen.
S: [ CITATION Gil17 \l 13321 ]
I: Evaluate sleep patterns, note reports of difficulties and
whether patient feels well rested. Provide quiet
environment, group care or monitoring activities to allow
Cebu Normal University Document
SDF-CON-NF-7002-034-00
periods of uninterrupted sleep; limit stimulants such as
caffeine; encourage position of comfort
R: Multiple external stimuli and the presence of dyspnea
may prevent relaxation and inhibit sleep.
S: [ CITATION Gil17 \l 13321 ]
SECONDARY INTERVENTIONS
Curative
I: Position patient with head of bed elevated, in a semi-
Fowler’s position (head of bed at 45 degrees when supine)
as tolerated.
R: Upright position or semi-Fowler’s position allows
increased thoracic capacity, full descent of diaphragm, and
increased lung expansion preventing the abdominal
contents from crowding.
S: [ CITATION Gil17 \l 13321 ]
I: Maintain an oxygen administration device as ordered,
attempting to maintain oxygen saturation at 90% or
greater.
R: Supplemental oxygen may be required to maintain
PaO2 at an acceptable level.
S: [ CITATION Gil17 \l 13321 ]
I: Do chest physiotherapy.
R: Chest percussion helps loosen and mobilize secretions
in smaller airways that cannot be removed by coughing or
suctioning.
S: (Wayne, 2017)
I: Help patient deep breathe and perform controlled
coughing. Have patient inhale deeply, hold breath for
several seconds, and cough two to three times with mouth
open while tightening the upper abdominal muscles as
tolerated.
R: This technique can help increase sputum clearance and
decrease cough spasms. Controlled coughing uses the
diaphragmatic muscles, making the cough more forceful
and effective.
S: [ CITATION Gil17 \l 13321 ]
I: Administer medications as prescribed.
R: It depends on the etiological factors of the problem
Cebu Normal University Document
SDF-CON-NF-7002-034-00
(e.g., antibiotics for pneumonia, bronchodilators for
COPD, anticoagulants and thrombolytics for pulmonary
embolus, analgesics for thoracic pain).
S: [ CITATION Doe16 \l 13321 ]
TERTIARY INTERVENTIONS
Rehabilitative
I: Provide reassurance and reduce anxiety.
R: Anxiety increases dyspnea, respiratory rate, and work
of breathing.
S: [ CITATION Gil17 \l 13321 ]
I: Pace activities and schedule rest periods to prevent
fatigue. Assist with ADLs.
R: Activities will increase oxygen consumption and
should be planned so the patient does not become hypoxic.
S: [ CITATION Doe16 \l 13321 ]
I: Instruct family in complications of disease and
importance of maintaining medical regimen, including
when to call physician.
R: Knowledge of the family about the disease is very
important to prevent further complications.
S: [ CITATION Gil17 \l 13321 ]
Bibliography
Doenges, M. E., Moorhouse, M., & Murr, A. C. (2013). Nurse's Pocket Guide (13th ed.). Philadelphia: F.A. Davis Company.
Vera, M. (2019, September 28). 7 Chronic Obstructive Pulmonary Disease (COPD) Nursing Care Plans. Retrieved from Nurseslabs: https://nurseslabs.com/chronic-obstructive-pulmonary-
disease-copd-nursing-care-plans/2/
Wayne, G. (2017, September 4). Impaired Gas Exchange Nursing Care Plan. Retrieved from Nurseslabs: https://nurseslabs.com/impaired-gas-exchange/
Cebu Normal University Document
SDF-CON-NF-7002-034-00
You might also like
- Case Analysis March 11Document5 pagesCase Analysis March 11Nicole Villanueva, BSN - Level 3ANo ratings yet
- Urinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideDocument5 pagesUrinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideLaoMed plusNo ratings yet
- Clinical Reasoning Questions - CollaborationDocument4 pagesClinical Reasoning Questions - CollaborationMohammad OmarNo ratings yet
- Subjective Cues:: Nursing Care ProcessDocument8 pagesSubjective Cues:: Nursing Care ProcessBianca Marithè RejanoNo ratings yet
- NCPDocument2 pagesNCPAnne De VeraNo ratings yet
- PRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaDocument4 pagesPRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaElay Pedroso100% (1)
- Electrolyte Imbalance NCPDocument6 pagesElectrolyte Imbalance NCPjohnart jimenezNo ratings yet
- Nursing Care Plans: Blood Pleural EffusionDocument9 pagesNursing Care Plans: Blood Pleural Effusionjamil aldasriNo ratings yet
- NCP of CavDocument3 pagesNCP of CavHenry Roque TagalagNo ratings yet
- Nursing Care Plan (NCP) For SchizophreniformDocument8 pagesNursing Care Plan (NCP) For SchizophreniformRisa Sol AriasNo ratings yet
- Ursing ARE LAN: Short Term Goal: Independent Intervention: Independent InterventionDocument2 pagesUrsing ARE LAN: Short Term Goal: Independent Intervention: Independent InterventionGiselle EstoquiaNo ratings yet
- NCPDocument3 pagesNCPJanie StubbertNo ratings yet
- NCP AppendicitisDocument5 pagesNCP AppendicitisElbert Kay SerranoNo ratings yet
- NCPDocument2 pagesNCPJonathan LiscanoNo ratings yet
- Atropine SulfateDocument4 pagesAtropine SulfateSuraya_Mohamed_3281No ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputRenie SerranoNo ratings yet
- Cues Diagnosis Background Knowledge Planning Intervention Rationale EvaluationDocument2 pagesCues Diagnosis Background Knowledge Planning Intervention Rationale EvaluationhaniehaehaeNo ratings yet
- Assessment Planning Intervention Rationale EvaluationDocument2 pagesAssessment Planning Intervention Rationale EvaluationIrish Jane GalloNo ratings yet
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafeNo ratings yet
- Exercise No.009Document2 pagesExercise No.009bea pegadNo ratings yet
- Simple Schematic Diagram of PneumoniaDocument1 pageSimple Schematic Diagram of PneumoniaTyrel LozanoNo ratings yet
- NCP 6-10Document4 pagesNCP 6-10Junabel EmNo ratings yet
- Group 3 Culminating Activity Week 2Document7 pagesGroup 3 Culminating Activity Week 2Anna mae OcampoNo ratings yet
- NCP ProperDocument9 pagesNCP Properstephanie eduarteNo ratings yet
- NCP Imbalanced NutritionDocument7 pagesNCP Imbalanced NutritionNora VarshavskiNo ratings yet
- NCMHDocument2 pagesNCMHLucas MaximusNo ratings yet
- Drug StudyDocument8 pagesDrug StudyJohn Ronald P. RamosNo ratings yet
- TPN NCPDocument10 pagesTPN NCPArabylle Maranca AbuelNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocument3 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationTedd CamilingNo ratings yet
- NCP DisturbedDocument2 pagesNCP DisturbedTrixie Anne GamotinNo ratings yet
- NCP Activity IntoleranceDocument3 pagesNCP Activity IntoleranceJopaii TanakaNo ratings yet
- NCP On DyspneaDocument5 pagesNCP On DyspneaDizzy BualanNo ratings yet
- Growth and DevelopmentDocument5 pagesGrowth and DevelopmentGabrielLopezNo ratings yet
- Impaired Gas ExchangeDocument1 pageImpaired Gas ExchangeLyka Mae Imbat - PacnisNo ratings yet
- SOAPIE - Decreased Cardiac Output Related To Altered Heart RateDocument1 pageSOAPIE - Decreased Cardiac Output Related To Altered Heart RateKian Herrera100% (1)
- Ineffective Tissue PerfusionDocument5 pagesIneffective Tissue PerfusionApryll Kristin Villaluna ZafeNo ratings yet
- NCP For DRDocument1 pageNCP For DRvalencia222No ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Kardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313Document2 pagesKardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313kuro hanabusaNo ratings yet
- Nursing Care PlanDocument13 pagesNursing Care Planyumiko0% (1)
- NCPDocument9 pagesNCPHendy Hency YunusNo ratings yet
- NCP RevisedDocument7 pagesNCP RevisedJessa BorreNo ratings yet
- Acute Head InjuryDocument5 pagesAcute Head InjuryRitesh KumarNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- NCP GeriaDocument6 pagesNCP GeriaKeanu ArcillaNo ratings yet
- E. Nursing DiagnosisDocument2 pagesE. Nursing DiagnosisAle SandraNo ratings yet
- Viii NCPDocument6 pagesViii NCPAdrian MangahasNo ratings yet
- Risk For AspirationDocument1 pageRisk For Aspirationmmcgee01No ratings yet
- NCP UreteroDocument1 pageNCP UreteroCerie Anne OlayNo ratings yet
- NRes1 Course Unit 4Document5 pagesNRes1 Course Unit 4Giselle EstoquiaNo ratings yet
- Cues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationMiggy SikatNo ratings yet
- Guillain Barre Case StudyDocument18 pagesGuillain Barre Case Studymydnyt02No ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocument2 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNo ratings yet
- Nursing Care Plan AnemiaDocument3 pagesNursing Care Plan AnemiaNat B. AntipoloNo ratings yet
- Philippine Health AgendaDocument9 pagesPhilippine Health AgendaCzeazarNo ratings yet
- NURSING RESEARCH-21 CorrectedDocument163 pagesNURSING RESEARCH-21 Correctedcoosa liquorsNo ratings yet
- NCPDocument17 pagesNCPbalongetzNo ratings yet
- Vitamin K (Phytomenadione) 2016: Indication Action Drug Type Trade Name Presentation Dosage / IntervalDocument3 pagesVitamin K (Phytomenadione) 2016: Indication Action Drug Type Trade Name Presentation Dosage / IntervalDeni Yuda Adi SaputraNo ratings yet
- NCPDocument7 pagesNCPRonel ResurricionNo ratings yet
- Go NCP IneffectivebreathingpatDocument7 pagesGo NCP IneffectivebreathingpatSAMANTHA T. MODESTONo ratings yet
- CARE PLAN For BRONCHIECTASISDocument8 pagesCARE PLAN For BRONCHIECTASISCecil MonteroNo ratings yet
- Lee, Rocky 54, M/M, CAP Other Data For Charting: 5.ignazio, Amor, 54, F/MDocument3 pagesLee, Rocky 54, M/M, CAP Other Data For Charting: 5.ignazio, Amor, 54, F/MvanNo ratings yet
- FluticasoneDocument4 pagesFluticasonevanNo ratings yet
- Sodium Bicarbonate Drug StudyDocument5 pagesSodium Bicarbonate Drug Studyvan0% (1)
- Nurses Progress NotesDocument2 pagesNurses Progress Notesvan100% (1)
- Nurses Progress NotesDocument2 pagesNurses Progress Notesvan100% (1)
- Protists FungiDocument77 pagesProtists FungiEgga AndiniNo ratings yet
- Board Basics An Enhancement To MKSAP 19 (Patrick Craig Alguire (Editor) )Document410 pagesBoard Basics An Enhancement To MKSAP 19 (Patrick Craig Alguire (Editor) )Emin bojec100% (1)
- Anatomy and Physiology: Key FeaturesDocument4 pagesAnatomy and Physiology: Key Featuresorchitarosadila haryonoNo ratings yet
- Amyloidosis SkinDocument6 pagesAmyloidosis SkinGoran MaliNo ratings yet
- Chapter 6 Thermal Injuries or DeathsDocument15 pagesChapter 6 Thermal Injuries or DeathsJm Lanaban100% (1)
- NMC CBT - Sample Exam Practice 2 AnswersDocument7 pagesNMC CBT - Sample Exam Practice 2 AnswersSupremo Manuel M Deluao75% (4)
- 3 Year Paediatric Assignment One: Department NursingDocument12 pages3 Year Paediatric Assignment One: Department NursingmekdesNo ratings yet
- Backpain NCPDocument3 pagesBackpain NCPxxarrowloverzxxdes23No ratings yet
- Case Study - BronchopneumoniaDocument108 pagesCase Study - BronchopneumoniaAnthony WallNo ratings yet
- Gastric Outlet Obstruction (Soltan Aiman NeazyDocument49 pagesGastric Outlet Obstruction (Soltan Aiman NeazyMohammed ElhashimiNo ratings yet
- Advantages of Covid19Document1 pageAdvantages of Covid19Sarah Jane MenilNo ratings yet
- Inborne Error of Amino Acid MetabolismDocument44 pagesInborne Error of Amino Acid MetabolismPrincewill SeiyefaNo ratings yet
- Biodiversity and Human HealthDocument32 pagesBiodiversity and Human HealthMarygrace BroñolaNo ratings yet
- Flashcards MicrobiologiaDocument50 pagesFlashcards MicrobiologiaBenjamin BarcelóNo ratings yet
- Gastroenterology - DiverticulaDocument1 pageGastroenterology - DiverticulaEugen MNo ratings yet
- ASHISH KESHRI (1) Detailed ReportDocument1 pageASHISH KESHRI (1) Detailed ReportShatabdi VermaNo ratings yet
- Janet Carr - Down's Syndrome - Children Growing Up (1995, Cambridge University Press)Document217 pagesJanet Carr - Down's Syndrome - Children Growing Up (1995, Cambridge University Press)EMI URSANNo ratings yet
- Grade 8 Tle Quarter ExamDocument3 pagesGrade 8 Tle Quarter ExamJovelyn TakilidNo ratings yet
- WHO COVID-19 Report April 28, 2020Document12 pagesWHO COVID-19 Report April 28, 2020CityNewsToronto100% (1)
- Unit X - Abnormalities During Postnatal Period Assessment and Management of Women With Postnatal Complications Total: 4 HoursDocument73 pagesUnit X - Abnormalities During Postnatal Period Assessment and Management of Women With Postnatal Complications Total: 4 Hourssoumya satheshNo ratings yet
- 220 Nursing Bullets Fundamentals of Nursing Reviewer 1Document23 pages220 Nursing Bullets Fundamentals of Nursing Reviewer 1Kyles JumaritoNo ratings yet
- Clinical Application of The EchocardiogtamDocument39 pagesClinical Application of The EchocardiogtamStella CooKeyNo ratings yet
- Mr. Jones Case StudyDocument4 pagesMr. Jones Case StudyDiane JaravataNo ratings yet
- IL1 AntagonistaDocument13 pagesIL1 AntagonistaZitlal-lin VictoriaNo ratings yet
- Candida Vulvovaginitis - Clinical Manifestations and Diagnosis - UpToDateDocument18 pagesCandida Vulvovaginitis - Clinical Manifestations and Diagnosis - UpToDateCindyNo ratings yet
- A1.Fundamentals - 25item With Rationale (NCLEX)Document5 pagesA1.Fundamentals - 25item With Rationale (NCLEX)Blardy Falking You Benchod BlardyNo ratings yet
- What Causes Gastritis?Document3 pagesWhat Causes Gastritis?TANYANo ratings yet
- NCP JaundiceDocument9 pagesNCP JaundiceMeena Koushal100% (1)