Professional Documents
Culture Documents
Group Fdar Hemophilia A
Uploaded by
Mika Saldaña0 ratings0% found this document useful (0 votes)
206 views2 pagesOriginal Title
GROUP-FDAR-HEMOPHILIA-A
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
206 views2 pagesGroup Fdar Hemophilia A
Uploaded by
Mika SaldañaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
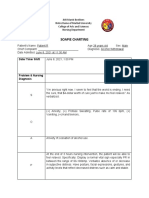
DATE/TIME FOCUS D = DATA A = ACTION R= RESPONSE
October 24, Initial Assessment D - Arrived at ER, a 40-year-old female, awake,
2020 restless but coherent accompanied by sister via
8:00 AM wheelchair with chief complaints of body weakness,
abdominal pain, hematochezia, odynophagia and
purple spots inside the mouth.
A - Ushered to bed; Assisted to comfortable
position. Raised and locked siderails. Vital signs
taken and recorded as follows - BP: 80/60mmHg, PR:
65 bpm, RR: 20cpm, Temp: 36.2 C, and O2 Sat of 90%.
Seen and examined by ER ROD with orders carried
out. Secured consent for admission signed by
patient. Referred/ Facilitated CBC plt, blood typing,
APTT, PT, bleeding time, & One-stage factor Assay:
Intrinsic Coagulation System determination laboratory
and diagnostic exams STAT.
8:05 AM Started IVF of D5LR IL regulated at 20gtts/min, infusing
well with IV cannula gauge 20 at right metacarpal vein.
8:10 AM Administered Tranexamic Acid 500 mg via IV. ----------------
8:20 AM Fluid Volume Deficit D – “Nagiinuro ako hin dugo ngan nanhahagkot na
gad ako baga ako hiton mahihimatay di nala
maiha.” As verbalized. BP: 80/60 mmHg, PR: 65
bpm, Temperature: 36.2 C, O2 saturation: 90%
room air. Restless, reports of fatigue, dizziness and
light headedness. Cold, clammy skin. Capillary refill
more than 3 < seconds. Hemoglobin: 6 g/dl, Weight
65 kg. VIII inhibitor level of 59.7 bethesda units.
A - Monitored vital signs particulary BP ,HR and
Temperature; Asessed for any alteration in mental
status; provided monitoring sheet & calibrated bottle for
urine collection; Documented color and amount of urine
and noting especially for urine output less than 30
mL/hour; Identified the possible cause of the fluid
disturbance or imbalance; Monitored closely for signs of
circulatory overload; Monitored for the existence of
factors causing deficient fluid volume; Urged the patient
to increase fluid intake to at least 10 – 12 glasses or 1-2
liters per day; Encouraged SO to assist with feedings, as
necessary; Emphasized importance of oral hygiene;
Provided comfortable environment and light sheets;
8:30 AM Started Methylprednisolone 60 mg IV as ordered. ----------
8:45 AM Started Iron sucrose 200mg IV diluted to 100 mL PNSS. ---
9: 00 AM R – “Mas mauru-upay na po it akon inaabat yana.” As
verbalized. Reported decrease in restlessness, dizziness
and light headedness.
-----------------------------------------------
9: 10 AM Post transfer D - Received from ER via wheelchair. Awake and
assessment slightly restless but coherent with an ongoing IVF of
D5LR IL regulated at 20gtts/min, infusing well with IV
cannula gauge 20 at right metacarpal vein. -------------------
A - Transferred to bed accompanied by sister and
placed in a comfortable position. Vitals signs taken
and recorded as follows: BP: 80/60 mmHg, PR: 65
bpm, Temp: 36.2 °C, and O2 Sat of 90%. Secured with
side rails up and locked. Oriented with regards to
hospital and ward policies. Encouraged verbalization
of feelings and concerns. ------------------------------------
9:20 AM Acute pain D - “Kanina pa ini nagsisinakit na akon tiyan, baga
hin diri nawawara” as verbalized. Dull, aching pain
on the umbilical region of the abdominal area, 9/10
on Pain Rating Scale (with 10 being the highest and
1 being the lowest), Guarding behaviors, Facial
grimace and restlessness, BP of 80/60 mmHg, HR of
65 bpm, and RR of 20 cpm, Hgb of 6 g/dL, Hct of
33%, bleeding time of 11 minutes, aPTT of 35-48
seconds, PT of 12 seconds. -------------------------------
A - Performed a comprehensive assessment of pain.
Determined the characteristics, onset, location,
duration, severity, pattern, and associated factors;
Observed for nonverbal pain cues, such as body
positioning, reluctance to move, facial expressions,
and physiological manifestations of acute pain-
elevated BP, tachycardia, and increased respiratory
rate; Explored alternative pain relief measures, such
as relaxation techniques, biofeedback, meditation,
and distraction- visual, auditory, tactile, kinaesthetic,
guided imagery, and breathing techniques; Provided
support for and careful positioning; Established a
quiet environment; Applied cold compress to
umbilical region, Monitored cardiovascular and
respiratory status prior to administration of tramadol,
a opiate analgesic; -----------------------------------------
9:35 AM Administered Tramadol 50 mg IV. ----------------------
You might also like
- 9 Yoga Class Sequences for Different TargetsDocument20 pages9 Yoga Class Sequences for Different TargetsLaerteNo ratings yet
- Nursing Care Plan (Compartment Sydnrome)Document6 pagesNursing Care Plan (Compartment Sydnrome)Zyiv BalogalNo ratings yet
- Aakash Zoology Study Package 3 SolutionsssssssDocument104 pagesAakash Zoology Study Package 3 SolutionsssssssRishika PaulNo ratings yet
- Lotus Notes Bleeding Letting For ClinicalDocument26 pagesLotus Notes Bleeding Letting For ClinicalMatthieu Decalf100% (2)
- Basal Metabolic RateDocument6 pagesBasal Metabolic RateDeborah Bravian Tairas0% (1)
- Fdar 008Document4 pagesFdar 008Kae MacalinaoNo ratings yet
- Lack of Knowledge On Diabetes Management or Blood Glucose ManagementDocument2 pagesLack of Knowledge On Diabetes Management or Blood Glucose ManagementDanica Kate GalleonNo ratings yet
- FDARDocument2 pagesFDARRajenne Blanche C. KHONo ratings yet
- Anaphy TransesDocument21 pagesAnaphy Transesfaith A.No ratings yet
- LIM NursesNotesDocument2 pagesLIM NursesNotesSophia limNo ratings yet
- Pathology For The Health Professions 5th Edition Damjanov Solutions ManualDocument25 pagesPathology For The Health Professions 5th Edition Damjanov Solutions ManualKevinRobertsbfak98% (56)
- Grand Case Pres FDARDocument11 pagesGrand Case Pres FDARMika SaldañaNo ratings yet
- Grand Case Pres FDARDocument11 pagesGrand Case Pres FDARMika SaldañaNo ratings yet
- Nurses Notes ExampleDocument3 pagesNurses Notes Exampleleo100% (1)
- Vital Signs Taking - Procedures-Rationale-Checklist (New)Document8 pagesVital Signs Taking - Procedures-Rationale-Checklist (New)Davi ciiNo ratings yet
- IAS Biology Student Book 1 (2018) AnswersDocument74 pagesIAS Biology Student Book 1 (2018) AnswersGazar76% (33)
- Pathfast PresepsinDocument6 pagesPathfast PresepsinWulan Ervinna SimanjuntakNo ratings yet
- General ObjectivesDocument1 pageGeneral ObjectivesErwin DegraciaNo ratings yet
- GROUP 2 FDAR RevisedDocument2 pagesGROUP 2 FDAR RevisedReysiela Mae ValinoNo ratings yet
- Nurses Notes: Student Nurse: Casas, Jannen A. Patient's Name: - N.T.M - Doctor: Bed No.Document2 pagesNurses Notes: Student Nurse: Casas, Jannen A. Patient's Name: - N.T.M - Doctor: Bed No.Jannen CasasNo ratings yet
- Philippine Health Agenda - Dec1 - 1 PDFDocument26 pagesPhilippine Health Agenda - Dec1 - 1 PDFreyalene gallegosNo ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- 5 Senses Detailed Lesson PlanDocument4 pages5 Senses Detailed Lesson PlanErica MonferoNo ratings yet
- University of Negros Occidental Student Clinical Training ReportDocument3 pagesUniversity of Negros Occidental Student Clinical Training ReportAzhly AntenorNo ratings yet
- How to prevent common breastfeeding difficultiesDocument2 pagesHow to prevent common breastfeeding difficultiesEmman Acosta Domingcil100% (1)
- Acute hypoxemia with suspected CAPDocument2 pagesAcute hypoxemia with suspected CAPCaitlyn100% (1)
- Drug StudyDocument20 pagesDrug StudydjanindNo ratings yet
- Lifestyle Modification: Asterlyn T. Coniendo Bsn-IvDocument4 pagesLifestyle Modification: Asterlyn T. Coniendo Bsn-IvAsterlyn ConiendoNo ratings yet
- Nursing Diagnosis Analysis Goal/Objectives Intervention Rationale EvaluationDocument3 pagesNursing Diagnosis Analysis Goal/Objectives Intervention Rationale EvaluationLorraine Punla PanganNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument14 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationJennifer ArdeNo ratings yet
- BSN 215 Reflection Essay - LagoDocument2 pagesBSN 215 Reflection Essay - LagoAlliahkherzteen LagoNo ratings yet
- ENT Patient Timeline and CareDocument6 pagesENT Patient Timeline and CareSj Eclipse100% (2)
- Post-Thyroidectomy FdarDocument1 pagePost-Thyroidectomy FdarKim Glaidyl BontuyanNo ratings yet
- Manage Bronchiectasis Nursing Care PlanDocument5 pagesManage Bronchiectasis Nursing Care PlanPaola Marie VenusNo ratings yet
- Final Course in The WardDocument4 pagesFinal Course in The WardMichael Boado100% (1)
- Nursing Diagnosis, Planning, Implementation and EvaluationDocument1 pageNursing Diagnosis, Planning, Implementation and EvaluationErjohn Vincent Lim100% (1)
- Kardex for Jose Rizal University Medical CenterDocument2 pagesKardex for Jose Rizal University Medical CenterMichael SarmientoNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Nursing Care Plan Pr/Annex: Saint Louis University Baguio City, Philippines School of NursingDocument7 pagesNursing Care Plan Pr/Annex: Saint Louis University Baguio City, Philippines School of NursingKAREN DAOAYNo ratings yet
- Fatigue Care Plan HIVDocument2 pagesFatigue Care Plan HIVDaryl Paglinawan100% (1)
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Choledolithiasis Cs 103 1Document34 pagesCholedolithiasis Cs 103 1Merlene Sarmiento SalungaNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- NCP For Ulnar SurgeryDocument5 pagesNCP For Ulnar SurgeryjiloNo ratings yet
- Fdar-Pedia WardDocument1 pageFdar-Pedia WardSyrelle GomezNo ratings yet
- DuphalacDocument2 pagesDuphalacianecunarNo ratings yet
- Impaired Physical Mobility: Date/ Time Focus DARDocument1 pageImpaired Physical Mobility: Date/ Time Focus DARMaria Chrislyn Marcos GenorgaNo ratings yet
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDocument3 pagesAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelNo ratings yet
- NCP (Postpartum Hemmorhage)Document3 pagesNCP (Postpartum Hemmorhage)Anne DyNo ratings yet
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Document20 pagesSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizNo ratings yet
- NCP2 - DengueDocument4 pagesNCP2 - DengueSummer SuarezNo ratings yet
- Drug mechanism indication contraindication side effects nursingDocument1 pageDrug mechanism indication contraindication side effects nursinghahahahaaaaaaaNo ratings yet
- Nursing Care of Uremic SyndromeDocument11 pagesNursing Care of Uremic Syndromeyoedha_banditozz50% (2)
- AnxietyDocument3 pagesAnxietyJenny Pearl Pasal100% (1)
- Sulfamethoxazole-trimethoprim drug cardDocument1 pageSulfamethoxazole-trimethoprim drug carderica2323No ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument2 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Coreg (Carvedilol) 6.25mgDocument3 pagesCoreg (Carvedilol) 6.25mgE100% (2)
- Week 3. COURSE TASK - Acute PancreatitisDocument3 pagesWeek 3. COURSE TASK - Acute PancreatitisqwertNo ratings yet
- NCM 114 - NCPDocument3 pagesNCM 114 - NCPReysiela Mae ValinoNo ratings yet
- Subjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentDocument2 pagesSubjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentCorinneNo ratings yet
- Urinary Tract Infection Nursing-Care-PlanDocument3 pagesUrinary Tract Infection Nursing-Care-PlanRnspeakcomNo ratings yet
- Sample CHN Teaching Learning GuideDocument3 pagesSample CHN Teaching Learning GuideSUREEN MAY ANG REGULARNo ratings yet
- Course in The WardDocument1 pageCourse in The WardGeevee Naganag VentulaNo ratings yet
- Self Task For English Lesson Part 2THDocument1 pageSelf Task For English Lesson Part 2THistiningrum0% (1)
- Leukemias: Care SettingDocument11 pagesLeukemias: Care SettingTinNo ratings yet
- NCPDocument14 pagesNCPRaidis Pangilinan0% (1)
- Generic Name: Classification Indication:: Hema KDocument2 pagesGeneric Name: Classification Indication:: Hema KKristine YoungNo ratings yet
- NCP Con ConstipationDocument2 pagesNCP Con ConstipationChristine Marie Bucio OraizNo ratings yet
- Soapie Charting: Date/ Time/ ShiftDocument2 pagesSoapie Charting: Date/ Time/ Shiftspain michaelisNo ratings yet
- Thromboangiitis Obliterans (Buerger's Disease): A Case PresentationDocument16 pagesThromboangiitis Obliterans (Buerger's Disease): A Case PresentationYan VencerNo ratings yet
- Emj Cases : Questions For Case 1Document8 pagesEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- History of Present Illness of Acute Parenchymal BleedingDocument2 pagesHistory of Present Illness of Acute Parenchymal BleedingHanna SeNo ratings yet
- Adolescent Growth & DeveleopmentDocument8 pagesAdolescent Growth & DeveleopmentMika SaldañaNo ratings yet
- Nursing care for children with cardiovascular diseasesDocument4 pagesNursing care for children with cardiovascular diseasesMika SaldañaNo ratings yet
- Pre-Scholler Growth and DevelopmentDocument4 pagesPre-Scholler Growth and DevelopmentMika SaldañaNo ratings yet
- The Skeletal SystemDocument5 pagesThe Skeletal SystemMika SaldañaNo ratings yet
- Essential Intrapartal Newborn Care (Einc) Notes By: Yzobelle RedondoDocument11 pagesEssential Intrapartal Newborn Care (Einc) Notes By: Yzobelle RedondoKriztian BorromeoNo ratings yet
- Chapter 20: Nursing Care of A Family Experiencing A Pregnancy Complication By: Yzobelle RedondoDocument8 pagesChapter 20: Nursing Care of A Family Experiencing A Pregnancy Complication By: Yzobelle RedondoMika SaldañaNo ratings yet
- CHN NCP - Lec - Maam VIVDocument39 pagesCHN NCP - Lec - Maam VIVMika SaldañaNo ratings yet
- CHN Priorities Health DeficitsDocument6 pagesCHN Priorities Health DeficitsMika SaldañaNo ratings yet
- Complications of Labor and BirthDocument8 pagesComplications of Labor and BirthMika SaldañaNo ratings yet
- For VS NEWDocument4 pagesFor VS NEWMika SaldañaNo ratings yet
- Chapter 18 MCN EditedDocument6 pagesChapter 18 MCN EditedMika SaldañaNo ratings yet
- CHN Priorities Health DeficitsDocument6 pagesCHN Priorities Health DeficitsMika SaldañaNo ratings yet
- CHN - HE Plan (Dengue & Leptospirosis)Document2 pagesCHN - HE Plan (Dengue & Leptospirosis)Mika SaldañaNo ratings yet
- Concept MappingDocument2 pagesConcept MappingMika SaldañaNo ratings yet
- CriteriaDocument6 pagesCriteriaMika SaldañaNo ratings yet
- CriteriaDocument6 pagesCriteriaMika SaldañaNo ratings yet
- SENIOR CITIZENS - Mika's ReportDocument5 pagesSENIOR CITIZENS - Mika's ReportMika SaldañaNo ratings yet
- HISTORY AND IMPORTANCE OF NEWBORN SCREENINGDocument35 pagesHISTORY AND IMPORTANCE OF NEWBORN SCREENINGMika SaldañaNo ratings yet
- Control of Communicable Diseases: (Doh Philippines)Document4 pagesControl of Communicable Diseases: (Doh Philippines)Mika SaldañaNo ratings yet
- Concept MappingDocument2 pagesConcept MappingMika SaldañaNo ratings yet
- Control of Communicable Diseases: (Doh Philippines)Document4 pagesControl of Communicable Diseases: (Doh Philippines)Mika SaldañaNo ratings yet
- Control of Communicable Diseases: (Doh Philippines)Document4 pagesControl of Communicable Diseases: (Doh Philippines)Mika SaldañaNo ratings yet
- Chapter 18 MCN EditedDocument6 pagesChapter 18 MCN EditedMika SaldañaNo ratings yet
- Presence of Risk Factor For Schistosomiasis Criteria Computation Actual Score JustificationDocument25 pagesPresence of Risk Factor For Schistosomiasis Criteria Computation Actual Score JustificationMika SaldañaNo ratings yet
- CHN - HE Plan (Dengue & Leptospirosis)Document2 pagesCHN - HE Plan (Dengue & Leptospirosis)Mika SaldañaNo ratings yet
- Parents Consent LetterDocument2 pagesParents Consent LetterMika SaldañaNo ratings yet
- Nres - 3 - Chapter 4 & 5 (Latest)Document63 pagesNres - 3 - Chapter 4 & 5 (Latest)Mika SaldañaNo ratings yet
- Enzymes: Indian Institute of Technology PatnaDocument22 pagesEnzymes: Indian Institute of Technology PatnaHritik KumarNo ratings yet
- Neurotrauma Rural Guidelines 2edDocument27 pagesNeurotrauma Rural Guidelines 2edAldion ZericoNo ratings yet
- ID Validitas Pengukuran Lemak Tubuh Yang MeDocument12 pagesID Validitas Pengukuran Lemak Tubuh Yang MeVante Lestya100% (1)
- Brochure GE Versamed Ivent 201 VentilatorDocument2 pagesBrochure GE Versamed Ivent 201 Ventilatoreslam MansourNo ratings yet
- Optical IllusionsDocument37 pagesOptical IllusionsAnshu Singh100% (1)
- Blood: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeDocument73 pagesBlood: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical Collegelourd nabNo ratings yet
- Prepare and RepairDocument38 pagesPrepare and RepairPete PuzaNo ratings yet
- BL 26Document1 pageBL 26ray72roNo ratings yet
- Article in Press: Neuroscience and Biobehavioral ReviewsDocument12 pagesArticle in Press: Neuroscience and Biobehavioral ReviewsDanilo NiroNo ratings yet
- 3 - Rasa DhatuDocument25 pages3 - Rasa DhatuChethan.H ChethuNo ratings yet
- College of Engineering Pune: Marathwada Mitra Mandal'sDocument3 pagesCollege of Engineering Pune: Marathwada Mitra Mandal'sTejas TaleleNo ratings yet
- Bioenergetics and Lipid MetabolismDocument34 pagesBioenergetics and Lipid MetabolismM Daffa Abhista ReviansyahNo ratings yet
- Novel Metabolic and Physiological Functions of Branched Chain Amino Acids: A ReviewDocument12 pagesNovel Metabolic and Physiological Functions of Branched Chain Amino Acids: A ReviewThiago Franco GuimarãesNo ratings yet
- Amorsen Elsa AnimalsDocument9 pagesAmorsen Elsa Animalsapi-267874252No ratings yet
- Culture of Organisation: Culture Is The Common Shared Values Within An OrganisationDocument27 pagesCulture of Organisation: Culture Is The Common Shared Values Within An OrganisationSiva BhandaruNo ratings yet
- The Anatomy of the Gastrointestinal TractDocument6 pagesThe Anatomy of the Gastrointestinal TractstuffNo ratings yet
- 269 - Embryology Physiology) Development of The Heart  - ÏDocument11 pages269 - Embryology Physiology) Development of The Heart  - ÏFood Safety CommunityNo ratings yet
- Transport in AnimalsDocument81 pagesTransport in AnimalsIbrahim NOORZADNo ratings yet
- Lipids (Mcmurry Ch. 27)Document15 pagesLipids (Mcmurry Ch. 27)Meisy RadhistaNo ratings yet
- Essentials of Medical Language 3rd Edition Allan Test BankDocument143 pagesEssentials of Medical Language 3rd Edition Allan Test BankDebbieCollinsokpzd100% (14)