Professional Documents
Culture Documents
Letters: Naproxen Excretion in Milk and Its Uptake by The Infant
Uploaded by
sasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Letters: Naproxen Excretion in Milk and Its Uptake by The Infant
Uploaded by
sasCopyright:
Available Formats
plasma creatinine. Clin Chem 1981;27:1953-4. subjects. J Antimicrob Chemother 1981;8(suppl E):131-40.
7. Saah AJ, Koch TR, Drusano GL. Cefoxitin falsely elevates 14. Foord RN. Cephaloridine and the kidney. In: Progress in anti-
creatinine levels. JAMA 1982;247:205-6. microbial and anticancer chemotherapy: proceedings of the 6th Inter-
8. Henry RJ. Clinical chemistry: principles and technics. New national Congress of Chemotherapy. Vol I. Tokyo: University of
York: Hoeber, 1964:287. Tokyo Press, 1970:597-604.
9. Neu HC, Srinivasan S. Pharmacology of ceftizoxime compared 15. McKendrick MW, Legg EF. In vivo and in vitro interference
with that of cefamandole. Antimicrob Agents Chemother due to cefotaxime on the assay of creatinine. J Clin Pathol
1981;21:366-9. 1981;34:224-5.
10. Stoeckel K. Pharmacokinetics of Rocephin, a highly active new 16. Kroll M, Koch T, Drusano GL, et al. Moxalactam, cefotax-
cephalosporin with an exceptionally long biological half-life. Chemo- ime, cefoperazone and ceftazidime do not interfere with creatinine
therapy 1981;27(suppl 1):42-6. determinations in serum or urine. 22nd Interscience Conference on
II. Harding SM, Monro AJ, Thornton JE, et al. The comparative Antimicrobial Agents and Chemotherapy, Oct 4-6, 1982, Miami Beach
pharmacokinetics of ceftazidime and cefotaxime in healthy volunteers. (abstract 525).
J Antimicrob Chemother 1981;8(suppl B):263-72. 17. Guay DRP, Meatherall RC, Macaulay PA. Interference of
12. Brogden RN, Carmine A, Heel RC, et al. Cefoperazone: a selected second- and third-generation cephalosporins with creatinine
review of its in vitro antimicrobial activity, pharmacological prop- determination. Am J Hosp Pharm 1983;40:435-8.
erties and therapeutic efficacy. Drugs 1981;22:423-60. 18. Polk RE, Stephens GH. Effects of cefazolin and moxalactam
13. Swabb EA, Leitz MA, Pilkiewicz FG, et al. Pharmacokinetics on serum chemistry values determined by autoanalyzer. Am J Hosp
of the monobactam SQ 26,776 after single intravenous doses in healthy Pharm 1981;38:866-8.
LETTERS
••••••••••••
Naproxen Excretion in Milk and its Uptake by the Infant alkaline hydrolysis were 100.6 and 120.6 mg for the first and second
TO THE EDITOR: The possible presence of drugs in breast milk fre- 250-mg doses, which constitute 40.3 percent and 48.2 percent of the
quently prompts questions by nursing mothers concerned about the administered dose, respectively. The observed EXu following inges-
safety of the suckling infant when the mother is under drug therapy. tion of the 375-mg dose was 179.4 mg, or 47.8 percent of the dose.
This information is crucial particularly when a mother is suffering These EXu values agree with the 43-65 percent reported by others!
from a chronic disease, such as rheumatoid arthritis. Naproxen is an Maximum milk naproxen concentrations appeared four hours postdos-
antiinflammatory acid commonly used in the treatment of rheumatoid ing and were 0.125 mg 0J0 and 0.114 mgOJo; lines through the terminal
arthritis. It elicits its therapeutic effects after daily administration of points had half-lives of 22.8 hand 23.8 h after administration of the
500-3000 mg, with infrequent significant side effects. I However, no first and second 250-mg doses, respectively (Figure I). The peak mam-
information as to the disposition of naproxen in breast milk and its mary concentration after the 375-mg dose was 0.237 mgOJo. Breast
uptake by the infant is available. We have investigated naproxen mam- milk pH ranged from 6.5-6.8 throughout the experiment.
mary excretion in a nursing mother and the uptake of the drug by The infant excreted 0.47 mg total intact and conjugated naproxen
the suckling infant. during the mother's 375-mg dosing interval (Figure 2). This consti-
A nursing mother with rheumatoid arthritis was referred to us for tutes 0.26 percent of the EXu observed in the mother. Assuming that
measurement of naproxen in her breast milk. She was 23-years-old, a 5-month-old infant exhibits the same pattern of naproxen metab-
weighed 59 kg, and had been under therapy with naproxen (Naprosyn, olism as an adult, the ratio of EXu of the infant over that of the mother
Syntex, Inc.) 250 mg bid for eight months. The infant, a healthy provides a measure of the ingested dose of the drug by the infant.
5-month-old, 8-kg boy, was breast fed regularly. The purpose of the Only 0.26 percent of the mother's dose was recovered from the infant.
drug analysis was to investigate the amount of naproxen in the milk
and the feasibility of increasing the mother's dose to 375 mg bid
without exposing the infant to large quantities of the drug through
feeding. The mother was taking no other medication.
To ascertain the attainment of the steady-state drug level, urine and
milk samples were collected over two consecutive periods of dosing
intervals. Following ingestion of the first routine daily 250-mg dose,
milk (5-10 ml) and urine (total output) were collected from the mother
,)
~
s
~lO
~
•
• •
•
•
•
•
•
at 0,2,4,8, and 12 h, and during the second daily dose interval at 4,8,
i • •
" 5
and 12 h postdosing. After analysis of the drug in the specimens, the
dosage regimen was increased to 375 mg bid and, three weeks later, O,l)-
milk and urine samples were taken from the mother at 0,2,4, and
\10.20
12 h following the first daily dose. Using disposable plastic bags, urine o
(total output) of the infant also was collected during the same dosing
interval at 0, 2.8, 5, 10, and 12 h. The infant went to the breast at .:':0.10
1.2 and 5.5 h postdosing. Naproxen concentrations in milk and urine •~
(after alkaline hydrolysis of conjugates) were determined, using the iii
~O.(E
high performance liquid chromatography method of Upton et al.'
10 15 20 25 10
Regression lines passing through the declining terminal phase of
fbco,
the mother's urinary excretion rate curves (Figure 1) indicate half-
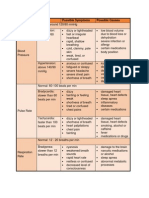
lives (tYz) of 8.75 hand 7.75 h for the first and second daily doses, Figure 1. Steady-state urinary excretion rate of naproxen after alkaline hydrolysis
respectively, of 250 mg. This value was 8.50 h for the 375-mg dose and corresponding milk naproxen concentrations during oral administration of 250
curve. Total cumulative urinary excretions (EXu) of naproxen after rng bid ( . ,0) and 375 mg bid (_,0), respectively. to a nursing mother.
910 Drug Intelligence and Clinical Pharmacy VOL17 DEC 83
Downloaded from aop.sagepub.com at DALHOUSIE UNIV on June 4, 2016
0.5 mined by dividing the MD (maintenance dose) by the duration of
. fusi
In usion (K0 = MD
-t-)'
Sawchuk and Zaske originally described this equation using the term
K O • 1 The use of K o in describing the dose administered also should
be considered when using the Appendix Equations 7 and 8 of this
article.
The authors also provide guidelines for establishing a dosing regimen
in patients receiving hemodialysis and peritoneal dialysis. They describe
6
f1,,,,,
10 12 a method of predicting the K el of these patients. However, no men-
tion is made of the in vivo inactivation of aminoglycosides by
Figure 2. Cumulative urinary excretion of naproxen after alkaline hydrolysis in an penicillins and semisynthetic penicillins. This can shorten the amino-
infant nursed regularly by his mother who was ingesting naproxen 375 mg bid. glycoside half-life significantly in patients with severe renal
insufficiency.i' This factor should be taken into account in dosing
Very low milk naproxen concentrations are consistent with this renal-failure patients when penicillins or semisynthetic penicillins are
observation. Other acidic drugs such as salicylate," ibuprofen,' and added to or deleted from the dosing regimen.'
flufenamic acid" also have limited mammary excretion, due, perhaps, DIANE E. BECK, Pharm.D.
to the more acidic nature of milk as compared with plasma.' To draw Assistant Professor
a definite conclusion as to the safety of naproxen therapy during Department of Clinical Pharmacy Practice
different stages of lactating period, more subjects must be examined. School of Pharmacy
Nevertheless, based on these observations, one may conclude that the Auburn University
extent of naproxen ingestion from breast milk of mothers under Auburn University, Alabama 36849
chronic therapy with this drug is limited and unlikely to cause signifi-
cant consequences in the suckling infant. References
FAKHREDDIN JAMALI, Ph.D. 1. Sawchuk RJ, Zaske DE. Pharmacokinetics of dosing regimens
Assistant Professor of Pharmacokinetics which utilize multiple intravenous infusions: gentamicin in burn pa-
DOUGLAS R.S. STEVENS tients. J Pharmacokinet Biopharm 1976;4: 183-95.
Pharmacy Student 2. Kradjan WA, Burger R. In vivo inactivation of gentamicin by
Faculty of Pharmacy and Pharmaceutical Sciences carbenicillin and ticarcillin. Arch Intern Med 1980;1l0:1668-70.
The University of Alberta 3. Russo ME, Thor EA. Gentamicin and ticarcillin in subjects with
Edmonton, Alberta T6G 2N8, Canada end-stage renal disease. Comparison of two assay methods and evalua-
tion of inactivation rate. Clin NephroI1981;15:175-80.
References 4. Chow MS, Quintiliani R, Nightingale CH. In vivo inactiva-
1. Day RO, Furst DE, Dromgoole SH, Kamm B, Roe R, Paulus tion of tobramycin by ticarcillin-a case report. JAMA
HE. Relationship of serum naproxen concentration to efficacy in 1982;247:658-9.
rheumatoid arthritis. Clin Pharmacol Ther 1982;31:733-40.
2. Upton RA, Buskin IN, Guentert TW, Williams RL, Riegelman
S. Convenient and sensitive high-performance liquid chromatography TOTHEEDITOR: Clarification should be made in the use of equations
assay for ketoprofen, naproxen and other allied drugs in plasma or that appeared in the article "Gentamicin and Tobramycin Dosing
urine. J Chromatogr 1980;190:119-28. Guidelines: An Evaluation." Equation I, on page 427, defines the
3. Segre EJ. Naproxen metabolism in man. J Clin Pharmacol steady-state peak (CPmax) as follows:
1975;15:316-23. MD (l-e-Kel t)
4. Jamali F, Keshavarz E. Salicylate excretion in breast milk. Int YdK d • (l-e- K elT)
J Pharm 1981;8:285,290.
5. Weibert RT, Townsend RJ, Kaiser DG, Naylor AJ. Lack of The term K d is, of course, supposed to be K el . However, of greater
ibuprofen secretion into human milk. Clin Pharm 1982;1:457-8. importance is the missing infusion time (t) factor in the denominator.
Equation 1 should be written as:
6. Buchanan RA, Eaton CJ, Koeff ST, Kinkel AW. The breast
milk excretion of flufenamic acid. CUff Ther Res 1969;1l:533-8. MD • (l-e- K elt )
CPmax = -Y--=-d"'K=-e-It- (1 - e - KelT)
7. Rasmussen F. Mammary excretion of sulphonamides. Acta
Pharmacol ToxicoI1958;15:139-48.
Some authors define maintenancedose as dosage (mg)/infusion time
(h). However, it is clear from the use of the equation on page 430
(Eq, 7) that MD is intended to be a dosage in milligrams, rather than
Comments and Corrections on Dosing Guidelines a dosage rate.
TOTHEEDITOR: In the article entitled "Gentamicin and Tobramycin Infusion time (t) should be added to Equation I and subsequent
Dosing Guidelines: An Evaluation" (DICP 1983;17:425-32), the equations, to prevent major errors in maintenance dose and concen-
authors present guidelines that they have developed to standardize tration calculations.
their pharmacokinetic dosing service in which a number of pharmacists PHILLIP HANN, Pharm.D.
participate. These guidelines are expected to promote consistent inter- Director
pretation and application of clinical and kirietic data. Education and Professional Services
Some readers may attempt to adopt these guidelines for applica- AMI Pharmacy Management Services
tion in their institutions. However, they should be cautioned to apply Encino, California 91436
the intermittent infusion equations in this article carefully (Eq. I,
Appendix Eq. 7 and 8). These equations assume the duration of amino- NOTE: This same error was brought to our attention by L.J. Coglan,
glycoside infusion to be one hour. However, in many institutions, pharmacist, Mesa Lutheran Hospital, Mesa, AZ.-ED.
the duration of infusion often varies, from 15 to 60 minutes. In this
situation, if the maintenance dose (administered in < 60 min) is in-
corporated into Equation 1 without conversion to mg/h, CPmax will
AUTHOR'S REPL v: It has been brought to my attention that there are
be underestimated.
two errors in our article "Gentamicin and Tobramycin Dosing Guide-
This potential error can be prevented by rewriting Equation 1 in
lines: An Evaluation." The errors are on page 431 and involve Equa-
the article as follows:
K o.(I- e- Kelt) tions 11 and 12. The errors in the mathematical statement should be
CPmax= K corrected as follows:
KelYd (l-e- elT) _ dose
Yd- Eq. 11
where K o is the zero-order infusion rate in mg/h; K o can be deter- KelPt
Drug Intelligence and Clinical Pharmacy VOL 17 DEC 83 911
Downloaded from aop.sagepub.com at DALHOUSIE UNIV on June 4, 2016
You might also like
- A Comprehensive Book on Experimental PharmaceuticsFrom EverandA Comprehensive Book on Experimental PharmaceuticsRating: 5 out of 5 stars5/5 (1)
- Bioequivalence Study of Carbamazepine Tablets: in Vitro/in Vivo CorrelationDocument8 pagesBioequivalence Study of Carbamazepine Tablets: in Vitro/in Vivo CorrelationFahmy SanjayaNo ratings yet
- Toxicology in Drug Discovery: Presented By: Pranita Potbhare Guided By: Dr. Manoj UpadhyayDocument27 pagesToxicology in Drug Discovery: Presented By: Pranita Potbhare Guided By: Dr. Manoj UpadhyaynikuNo ratings yet
- Interactiune BZD-mancareDocument9 pagesInteractiune BZD-mancareAndrei BombardieruNo ratings yet
- Ritalin ADocument8 pagesRitalin ALeonardo David Dearo SimonettiNo ratings yet
- Anderson Et Al - 1987 - Pharmacokinetics of A Single Dose of Rimantadine in Young Adults and ChildrenDocument3 pagesAnderson Et Al - 1987 - Pharmacokinetics of A Single Dose of Rimantadine in Young Adults and ChildrenМихаил РайцисNo ratings yet
- Ivivc: in Vitro-In Vivo CorrelationDocument46 pagesIvivc: in Vitro-In Vivo CorrelationMubammad Mursaleen100% (1)
- Bioavailability - and - Bioequivalence - 2 PDFDocument18 pagesBioavailability - and - Bioequivalence - 2 PDFdilka dariyaNo ratings yet
- ZocorDocument3 pagesZocorENo ratings yet
- Research ArticleDocument12 pagesResearch ArticleIbrahim Al SharabiNo ratings yet
- Bioavailability & Bioequivalence StudiesDocument45 pagesBioavailability & Bioequivalence StudiesHussein Talal Kenaan100% (2)
- PHARDOSEDocument26 pagesPHARDOSEZelica SantosNo ratings yet
- KJBVGGVVVDocument10 pagesKJBVGGVVVSuvojit BasakNo ratings yet
- ECAM2015 324369 PDFDocument6 pagesECAM2015 324369 PDFLuiz Otavio CostaNo ratings yet
- IV InfusionDocument1 pageIV InfusionSurampalliGuruNo ratings yet
- BF03258422Document6 pagesBF03258422Dini BerlianaNo ratings yet
- ClinicalresearchDocument49 pagesClinicalresearchNikhil PatilNo ratings yet
- Gauthier 1992Document6 pagesGauthier 1992hectorNo ratings yet
- 7.1 Basic Care During Postpartum Period 2017 2Document49 pages7.1 Basic Care During Postpartum Period 2017 2Abdella KesimNo ratings yet
- Esomeprazol Vs RabeprazolDocument7 pagesEsomeprazol Vs RabeprazolpabloNo ratings yet
- Final ResultsDocument9 pagesFinal ResultsAjie Wahyu Saputra MirzaNo ratings yet
- PharmacodynamicsDocument28 pagesPharmacodynamicsAbdishakur AdanNo ratings yet
- Crystalloid For The Management of Burn Shock.: A Right Choice?Document15 pagesCrystalloid For The Management of Burn Shock.: A Right Choice?syedsahibNo ratings yet
- Farklin 1 2021 Ppds Fkunsri 16 JuliDocument134 pagesFarklin 1 2021 Ppds Fkunsri 16 JuliBayu WisnuNo ratings yet
- Therapeutic Drug Monitoring of Levetiracetam in Daily Clinical Practice: High-Performance Liquid Chromatography Versus ImmunoassayDocument5 pagesTherapeutic Drug Monitoring of Levetiracetam in Daily Clinical Practice: High-Performance Liquid Chromatography Versus ImmunoassayMaria MendozaNo ratings yet
- Pharmacodynamics and Pharmacokinetics of The.29Document4 pagesPharmacodynamics and Pharmacokinetics of The.29Ama KireidesuNo ratings yet
- IVIVCDocument20 pagesIVIVCJafer DetamoNo ratings yet
- Food Interaction and Steady-State Pharmacokinetics of Itraconazole Capsules in Healthy Male VolunteersDocument7 pagesFood Interaction and Steady-State Pharmacokinetics of Itraconazole Capsules in Healthy Male VolunteersarchikaNo ratings yet
- Effects of Menstrual Cycle and Oral Contraceptive Use On Serum Levels of Lipid-Soluble AntioxidantsDocument4 pagesEffects of Menstrual Cycle and Oral Contraceptive Use On Serum Levels of Lipid-Soluble Antioxidantsdesy.armalina699No ratings yet
- Admin,+journal+manager,+20 AJPCR 5619 RADocument8 pagesAdmin,+journal+manager,+20 AJPCR 5619 RAAmol Amritkar NASIKNo ratings yet
- 06 Oa Comparison of Spot PDFDocument5 pages06 Oa Comparison of Spot PDFrositaputriagustiniNo ratings yet
- Bio As Say TechniquesDocument39 pagesBio As Say TechniquesGayatri LodhiNo ratings yet
- Laboratorios Valores EndocrinoDocument88 pagesLaboratorios Valores EndocrinoS ONo ratings yet
- Single-Dose and Multiple-Dose Pharmacokinetics of Zaltoprofen After Oral Administration in Healthy Chinese VolunteersDocument7 pagesSingle-Dose and Multiple-Dose Pharmacokinetics of Zaltoprofen After Oral Administration in Healthy Chinese VolunteersSonia BaruaNo ratings yet
- Singh. NMP Better Result VS DYDDocument2 pagesSingh. NMP Better Result VS DYDRuth RachmawatyNo ratings yet
- Lepidium Meyenii (Maca), A Root With Aphrodisiac andDocument6 pagesLepidium Meyenii (Maca), A Root With Aphrodisiac anda303111No ratings yet
- Bioavailability and Bioequivalence: By: Kris May Lyn A. RamosDocument77 pagesBioavailability and Bioequivalence: By: Kris May Lyn A. RamosValar Morghulis100% (1)
- RelativeBioavailabilityofRifampicin Id enDocument8 pagesRelativeBioavailabilityofRifampicin Id enHealthy SeptianaNo ratings yet
- Bahan Translate Biofar Pak OpikDocument1 pageBahan Translate Biofar Pak OpikPuty Prianti Novira100% (1)
- Pharmaceutics-I - Practical Record - 1st Sem-M.pharmDocument44 pagesPharmaceutics-I - Practical Record - 1st Sem-M.pharmVenkatesh VenkateshNo ratings yet
- Literature Review of OmeprazoleDocument5 pagesLiterature Review of Omeprazoleaflsbegdo100% (1)
- 15 - Ema - Epar - H389 - 2005Document55 pages15 - Ema - Epar - H389 - 2005Bin Chen MálagaNo ratings yet
- Tmp117e TMPDocument6 pagesTmp117e TMPFrontiersNo ratings yet
- Asian-Australasian Journal of Animal Sciences: TitleDocument13 pagesAsian-Australasian Journal of Animal Sciences: TitlecitraNo ratings yet
- Relationship Serum and Saliva Chloramphenicol ConcentrationsDocument4 pagesRelationship Serum and Saliva Chloramphenicol Concentrationsmonarch01No ratings yet
- Lopinavir Ritonavir Pharmacokinetic Profile Impact of Sex and Other CovariatesDocument9 pagesLopinavir Ritonavir Pharmacokinetic Profile Impact of Sex and Other CovariatesLuciana OliveiraNo ratings yet
- Pengaruh Makanan Pada CaptoprilDocument5 pagesPengaruh Makanan Pada CaptoprilNiluh putu Satria maharaniNo ratings yet
- Antimicrobial Agents and Chemotherapy 1978 Ginsburg 845.fullDocument4 pagesAntimicrobial Agents and Chemotherapy 1978 Ginsburg 845.fullnelisaNo ratings yet
- IUB 401 Ch3 DisinDossoBDocument55 pagesIUB 401 Ch3 DisinDossoBJubayer Al MahmudNo ratings yet
- To Assess The Effectiveness of Application of Aloe Vera Gel On Pressure Ulcers Among Patients Admitted in Selected HospitalsDocument4 pagesTo Assess The Effectiveness of Application of Aloe Vera Gel On Pressure Ulcers Among Patients Admitted in Selected HospitalsIJAR JOURNALNo ratings yet
- Formulaiton and Pharmacokinetic Evaluation of Naproxen Sodium Modified Release TabletDocument8 pagesFormulaiton and Pharmacokinetic Evaluation of Naproxen Sodium Modified Release TabletiajpsNo ratings yet
- 634268337552295000Document20 pages634268337552295000Uma MaheswararaoNo ratings yet
- Bioequivalence Study of Two Loperamide HydrochloriDocument5 pagesBioequivalence Study of Two Loperamide HydrochloriLoRna Nu'aNo ratings yet
- Chapter IIIDocument6 pagesChapter IIIprickybiikNo ratings yet
- Pharmacokinetics and Bioavailability of Montelukast Sodium (Mk-0476) in Healthy Young and Elderly VolunteersDocument9 pagesPharmacokinetics and Bioavailability of Montelukast Sodium (Mk-0476) in Healthy Young and Elderly VolunteersRahat ShamimNo ratings yet
- PIII-74 Pro-76: Society For Clinical Pharmacology and TherapeuticsDocument1 pagePIII-74 Pro-76: Society For Clinical Pharmacology and Therapeuticsdev darma karinggaNo ratings yet
- 5 PharmacologyDocument4 pages5 Pharmacologyshiv_prhNo ratings yet
- PH166 JournalCritique Julio (Wilmore)Document11 pagesPH166 JournalCritique Julio (Wilmore)Wilmore JulioNo ratings yet
- Practice ProblemsDocument7 pagesPractice ProblemsApril Mergelle LapuzNo ratings yet
- Development and Validation of New Analytical Methods For The Quantification of Clofarabine in Bulk and Pharmaceutical Dosage FormDocument10 pagesDevelopment and Validation of New Analytical Methods For The Quantification of Clofarabine in Bulk and Pharmaceutical Dosage FormImpact JournalsNo ratings yet
- 62 - Xenobiotics and BFDocument20 pages62 - Xenobiotics and BFsasNo ratings yet
- 45 - Breast Developement and AnatomyDocument5 pages45 - Breast Developement and AnatomysasNo ratings yet
- 57 - Adverse Drug Reactions in Breastfed Less Than ImaginedDocument16 pages57 - Adverse Drug Reactions in Breastfed Less Than ImaginedsasNo ratings yet
- 55 - Medication in BF WomenDocument8 pages55 - Medication in BF WomensasNo ratings yet
- It's Alive: Microbes and Cells in Human Milk and Their Potential Benefits To Mother and InfantDocument3 pagesIt's Alive: Microbes and Cells in Human Milk and Their Potential Benefits To Mother and InfantsasNo ratings yet
- 32-Acute Otitis MediaDocument11 pages32-Acute Otitis MediasasNo ratings yet
- 41-Intro Anatomy Immunity-NutritionDocument20 pages41-Intro Anatomy Immunity-NutritionsasNo ratings yet
- 31 - OMS Diarrhée Et Pneumonie PDFDocument54 pages31 - OMS Diarrhée Et Pneumonie PDFsasNo ratings yet
- 17-Evaluation of The Safety of Drugs WorkshopDocument9 pages17-Evaluation of The Safety of Drugs WorkshopsasNo ratings yet
- 18 - The Nuts and Bolts of BF Anatomy and PhysiologyDocument6 pages18 - The Nuts and Bolts of BF Anatomy and PhysiologysasNo ratings yet
- Vital Signs Assessment TableDocument2 pagesVital Signs Assessment Tableapi-250869701No ratings yet
- Performance Appraisal of Intensive Care Unit NursesDocument5 pagesPerformance Appraisal of Intensive Care Unit NursesJoyce Albaladejo100% (1)
- Ien Application Package: Type Text HereDocument23 pagesIen Application Package: Type Text Herejyselle domingoNo ratings yet
- AcknowledgementDocument4 pagesAcknowledgementArnie Mae ZorillaNo ratings yet
- Hepatitis Case Notification Message Mapping GuideDocument74 pagesHepatitis Case Notification Message Mapping Guideas d-fNo ratings yet
- Evidence Based-How To Ask An Answerable QuestionsDocument62 pagesEvidence Based-How To Ask An Answerable QuestionsFeniNo ratings yet
- SealBio: A Novel, Non-Obturation Endodontic Treatment Based On Concept of RegenerationDocument3 pagesSealBio: A Novel, Non-Obturation Endodontic Treatment Based On Concept of RegenerationPressInitiativeNo ratings yet
- Chapter 002Document5 pagesChapter 002Lisa Szyszka100% (1)
- RISK ASSESSMENT QUIZ ANSWERS (Confer)Document1 pageRISK ASSESSMENT QUIZ ANSWERS (Confer)Roh Young songNo ratings yet
- Phlebitis Score: Early Stage of Phlebitis Resite CannulaDocument1 pagePhlebitis Score: Early Stage of Phlebitis Resite CannulaelisaNo ratings yet
- Wilms TumorDocument6 pagesWilms TumorJennyDanielNo ratings yet
- Stafford y Colom (2013) - Purpose and of Psychoeducation Inpatients With Bipolar Disorder in A Bipolar ClinicsettingDocument9 pagesStafford y Colom (2013) - Purpose and of Psychoeducation Inpatients With Bipolar Disorder in A Bipolar ClinicsettingAbrahán OrellanaNo ratings yet
- FinalpaperDocument16 pagesFinalpaperapi-249847133No ratings yet
- Indent FormDocument2 pagesIndent FormDheeraj Bhatt0% (1)
- Acute Postpartum Paraplegia Caused by Spinal Extradural Capillary HemangiomaDocument2 pagesAcute Postpartum Paraplegia Caused by Spinal Extradural Capillary HemangiomaRabin SitumorangNo ratings yet
- Ihcanapril17 PDFDocument48 pagesIhcanapril17 PDFMommyx44100% (2)
- Barcoding InformaticsDocument10 pagesBarcoding Informaticsapi-650274498No ratings yet
- Week 5 VceDocument4 pagesWeek 5 VceRayanne JonesNo ratings yet
- Palliative CareDocument160 pagesPalliative CareReni PurwoNo ratings yet
- STATUS PSIKIATRI Kaplan Mental State Hari SelasaDocument82 pagesSTATUS PSIKIATRI Kaplan Mental State Hari SelasaendahwmNo ratings yet
- Civ 1Document5 pagesCiv 1waseem555No ratings yet
- Topics On Prosthetics & Orthotics - PDF CreDocument4 pagesTopics On Prosthetics & Orthotics - PDF CreSuprit MahakudNo ratings yet
- HemiparesisDocument35 pagesHemiparesisIsabela IacobNo ratings yet
- Physical Health CheckDocument9 pagesPhysical Health CheckDivya ThanlaeNo ratings yet
- Current Trends and Principles of Pediatric in NursingDocument15 pagesCurrent Trends and Principles of Pediatric in Nursingrubinarashmi16No ratings yet
- RadioterapiDocument11 pagesRadioterapiSaifuddin SuhriNo ratings yet
- Health, Safety, and Nutrition OER TextbookDocument505 pagesHealth, Safety, and Nutrition OER Textbookmiracle mae caparasNo ratings yet
- Nutrisi Pada KankerDocument8 pagesNutrisi Pada KankerRenny AnggreniNo ratings yet
- Bacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceDocument18 pagesBacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceZarwo Black UstadzNo ratings yet
- Sífilis Ocular 2021 Super CompletoDocument69 pagesSífilis Ocular 2021 Super CompletoouranpisNo ratings yet